MODULE 3 OCR A level Biology
1/157
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
158 Terms
Features of exchange surfaces
Thin
Ability to maintain a steep concentration gradient
Large surface area to volume ratio
Moist lining
Features of the nasal cavity
Large surface area
Good blood supply - warms air to body temperature
Ciliated epithelium cells waft/move mucus back up to the trachea to be swallowed
Goblet cells secrete mucus to trap microbes and dust to prevent infection; also prevents dehydration.
Moist
Warms and moistens air before it enters the lungs
Trachea
Wide tube, main airway from nose to chest, supported by cartilage rings to prevent collapse
Lined with ciliated epithelium, walls contain smooth muscle and elastic fibres
Cartilage in the trachea
Strong and inflexible, strength to prevent collapse during inhalation.
Rings are incomplete to allow space for the food to pass down the oesophagus
Support larger bronchioles
Bronchi
The passages that direct air into the lungs
Features of bronchioles
Bronchioles contain smooth muscle walls - when this contracts, bronchioles dilate, and the volume of air changes; they also elastic fibres.
Bronchioles are lined with a thin layer of ciliated epithelium for gas exchange, but usually don't contain goblet cells
Not usually supported by cartilage; small bronchioles have no smooth muscles
Alveoli
Tiny air sacs, main gas exchange surfaces of the body, coming from bronchioles
Features of alveoli
Layer of thin, flattened epithelial cells
Elastic fibres which allow elastic expansion and returning to resting size
Large surface area due to there being many
Good blood supply from capillaries
Thin walls of alveoli and capillaries minimises diffusion distance
Good ventilation maintains concentration gradient
Inner surface covered by a thin layer of water, salts, and lung surfactant so it can remain inflated and assist oxygen diffusion
Ventilation
Movement of air in the lungs as a result of pressure changes in the thorax due to breathing
Thorax
Pleural cavity, chest
Pleural membranes
Thorax is lined by pleural membranes which surround the lungs
Space between is the pleural cavity, filled with lubricating fluid so that membranes slide easily over each other when breathing
Inhalation
External intercostal muscles contract. Ribs move outwards and upwards.
Diaphragm contracts, flattening and lowering.
Thorax volume increases, and pressure decreases lower than atmospheric air.
Air is drawn in to equalise pressure.
Moves into alveoli and elastic fibres stretch.
Exhalation
External intercostal muscles relax, returning to orginal shape, ribs move downwards and inwards.
Muscles of diaphragm relax, moves into resting dome shape.
Thorax volume decreases, pressure increases above atmospheric air.
Air leaves lungs to equalise pressure.
Elastic fibres in alveoli recoil to assist this.
Forced exhalation
Internal intercostal muscles contract to pull the ribs down and inwards hard and fast.
External intercostal muscles relax.
Abdominal muscles contract to force the diaphragm up, increasing lung pressure quickly.
Asthmatic attack
Cells lining bronchioles release histamines - become inflamed and swollen.
Excess mucus produced
Bronchiole walls contract
Airways narrow and fill with mucus, increasing difficulty of breathing.
Tidal volume
Amount of air exchanged in a single breath
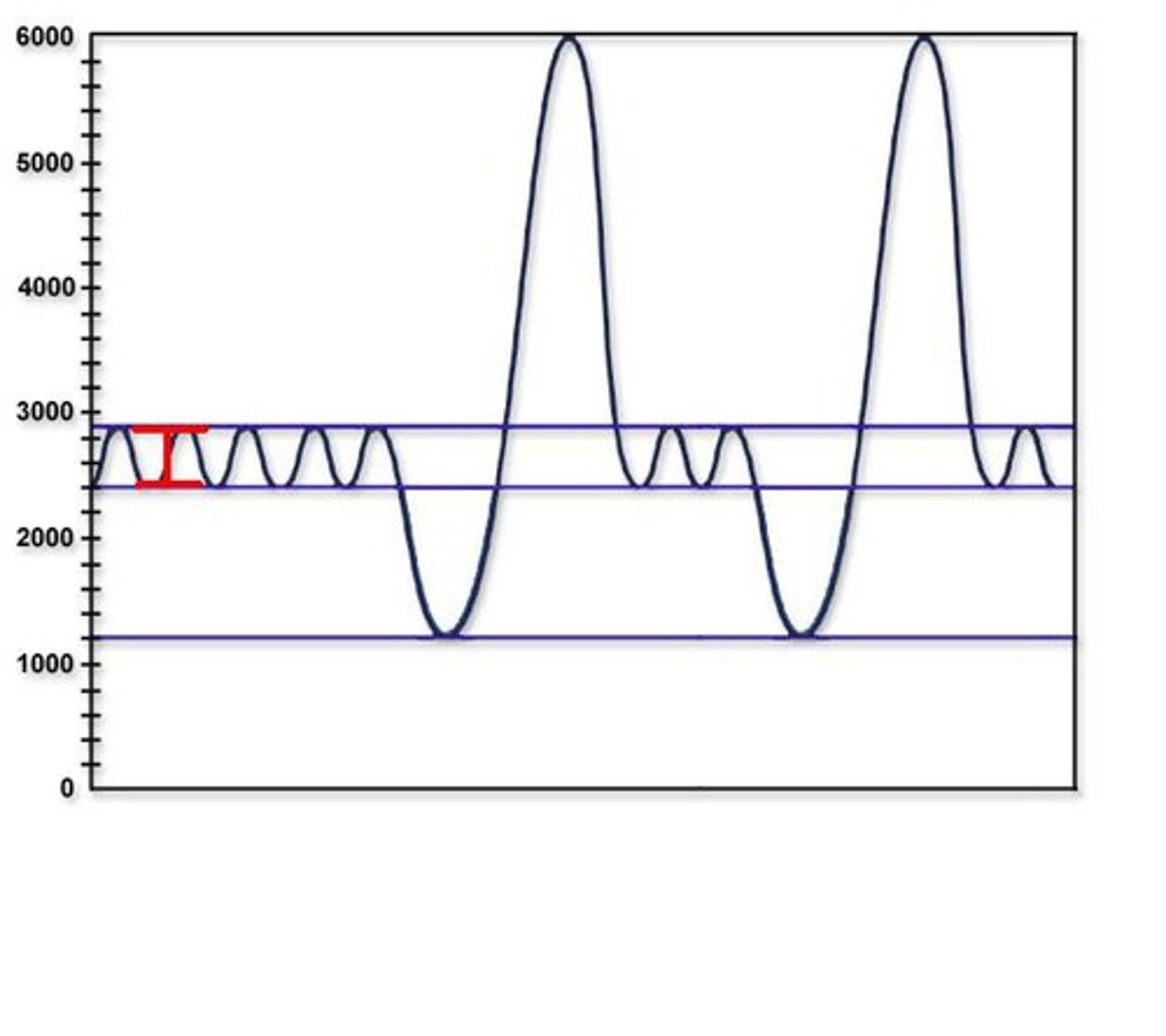
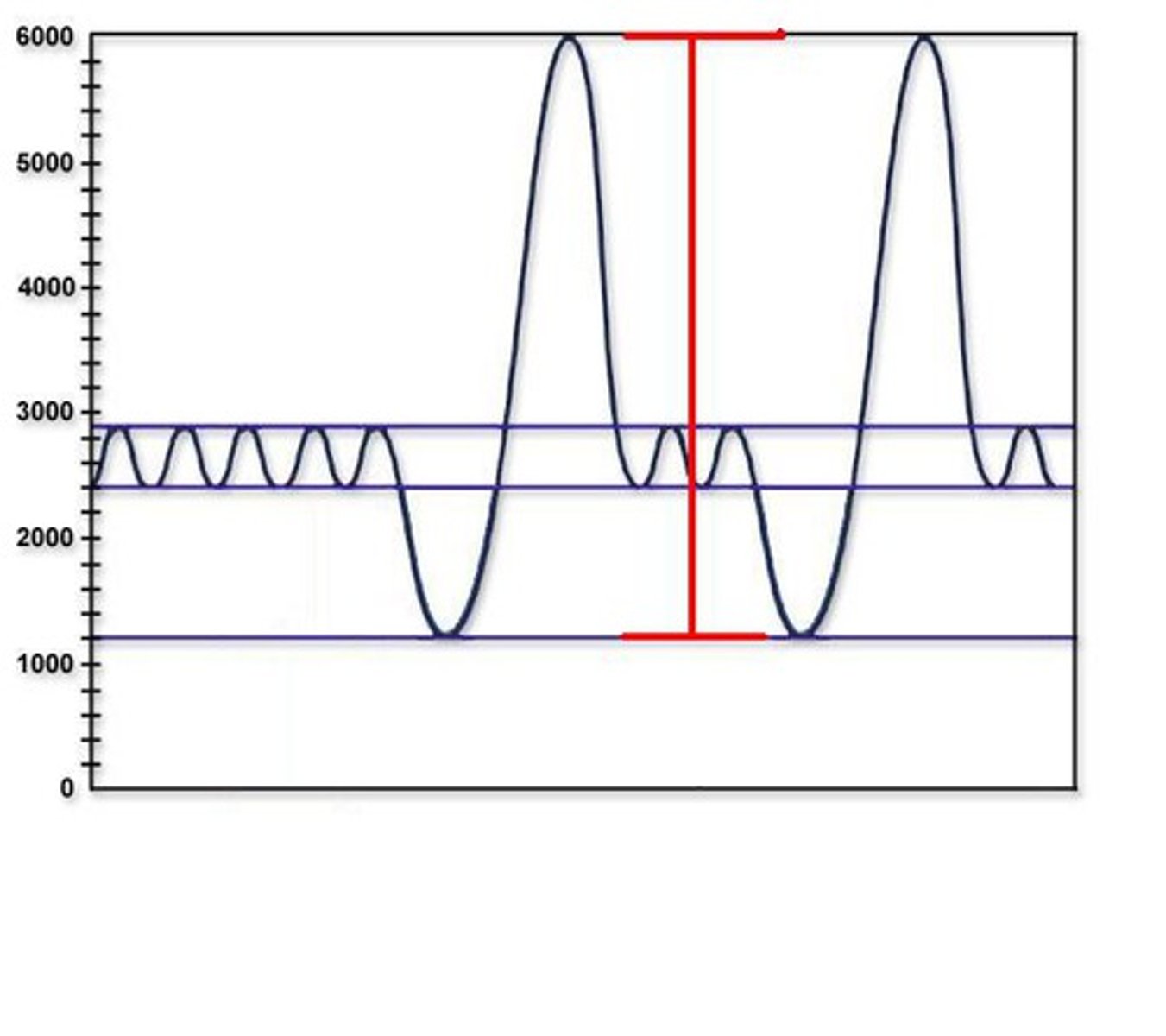
Vital capacity
Maximum volume of air exchanged in a single breath
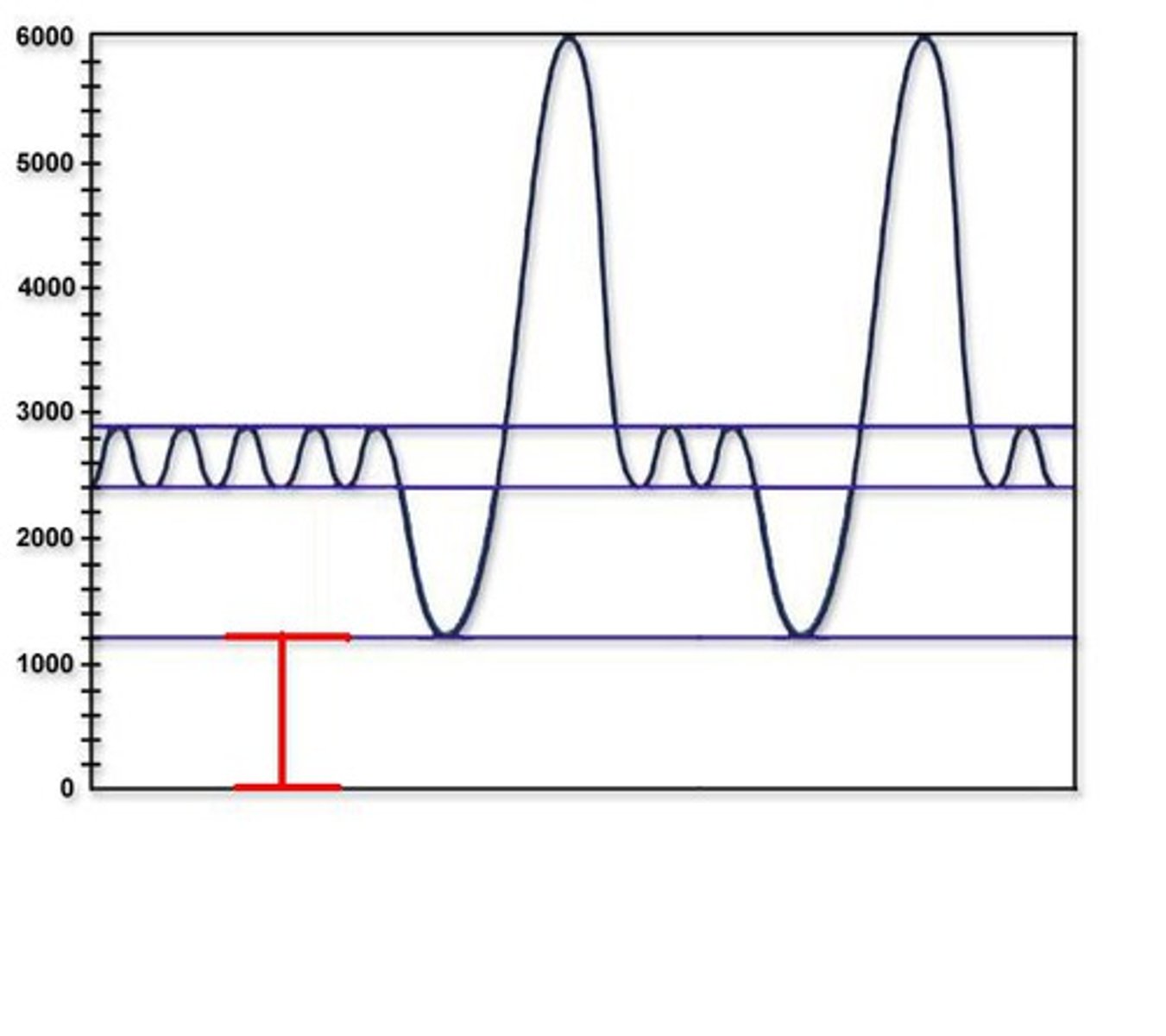
Residual volume
Volume leftover from exhaling
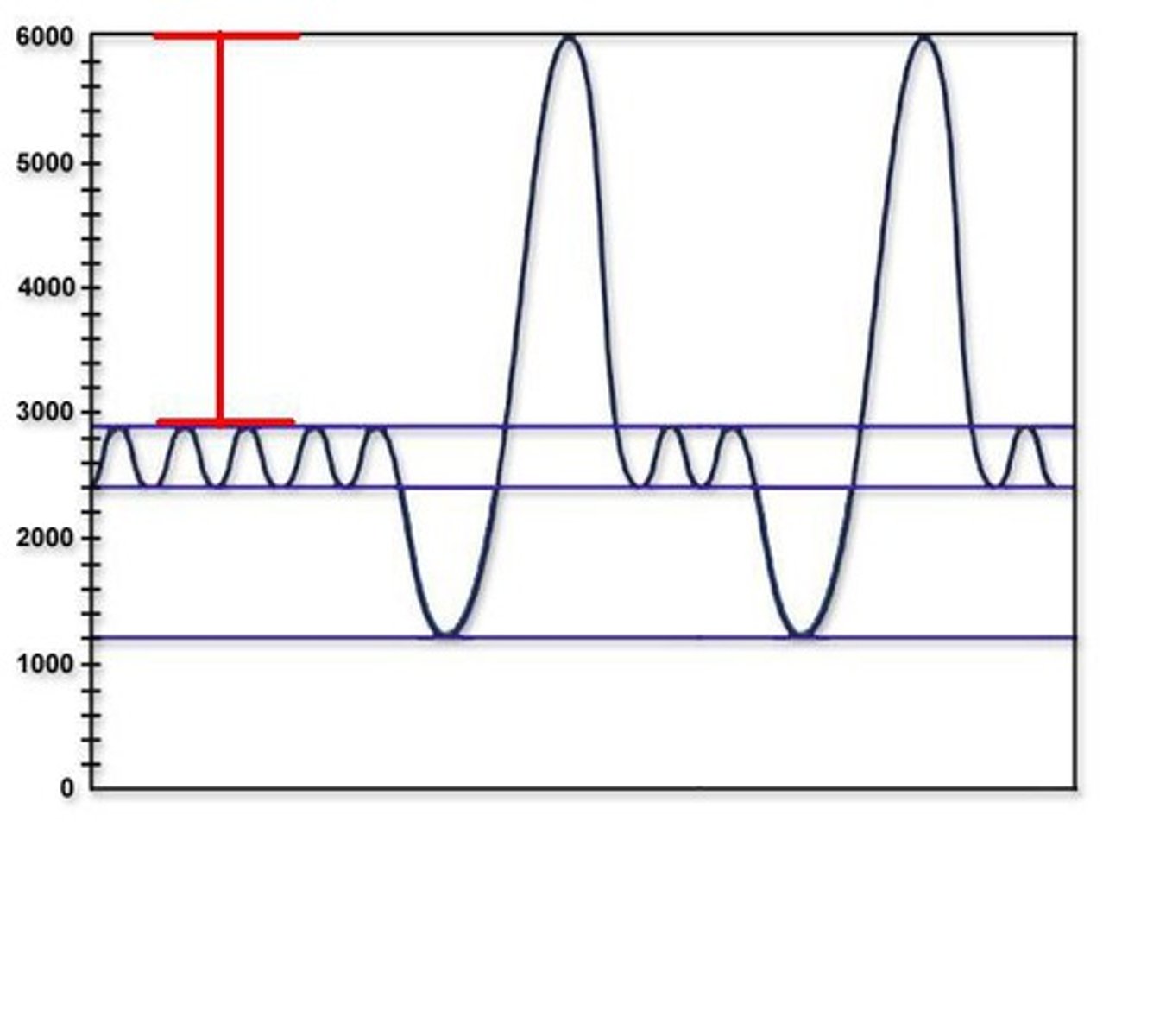
Inspiration reserve
Extra volume able to be filled from inhaling
Expiration reserve
Extra volume able to be released from exhaling
Ghost air
Air elsewhere in the ventilation system e.g. bronchi
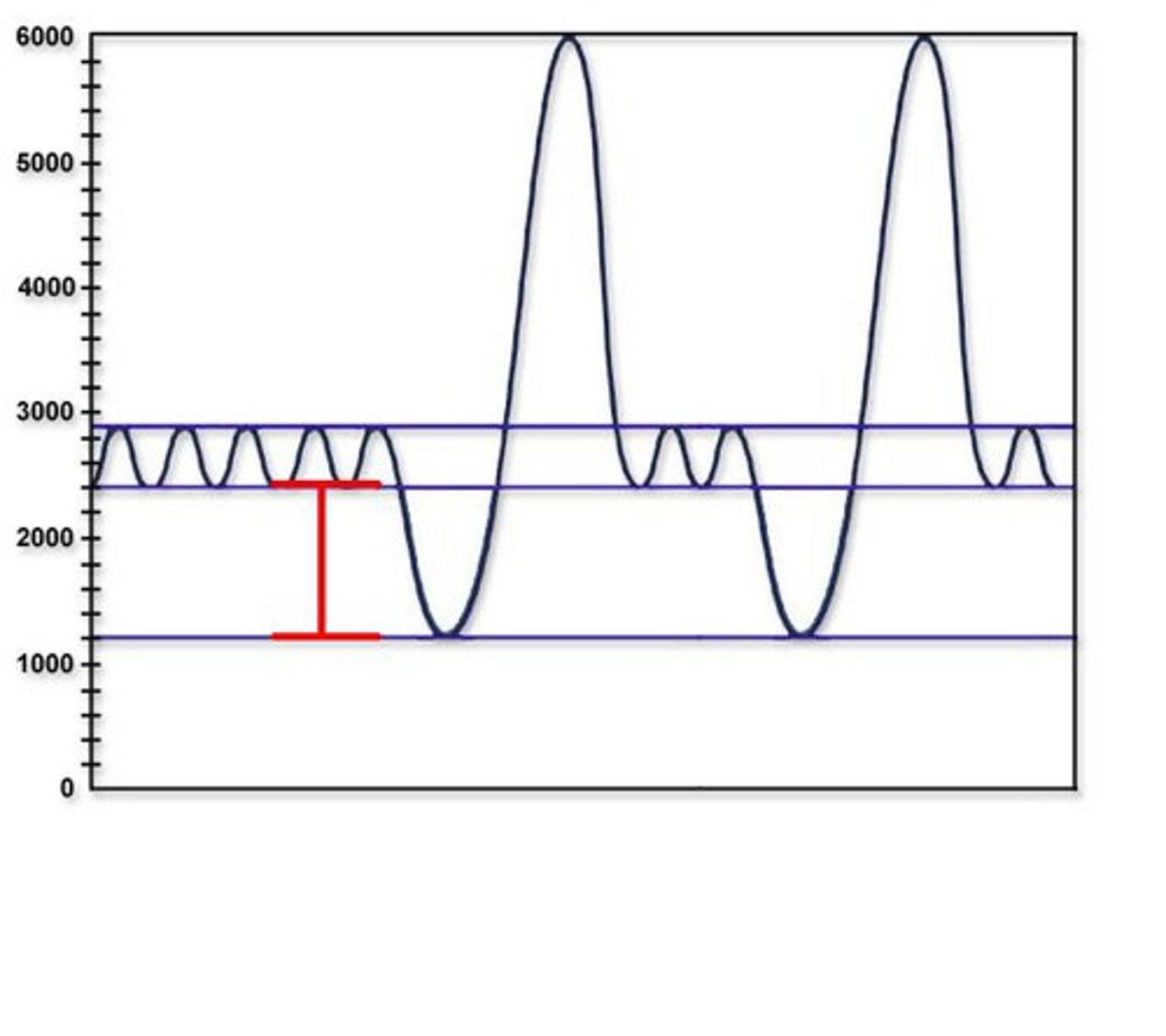
How is lung capacity measured?
Using a spirometer
How the spirometer works:
When you exhale, the chamber rises, and when you inhale, the chamber falls.
Attached to a pen, therefore a graph is drawn.
CO2 scrubber removes CO2 from recirculated air
Total air breathed per minute
Tidal volume x breathing rate
Breathing rate
number of breaths per minute
Oxygen consumption
Gradual removal of carbon dioxide, lowering the volume via a gradient
Common tidal volume
500cm^3
Common vital capacity
4-4.5dm^3
What is ventilation necessary for?
Gas exchange in the alveoli - CO2 into the alveoli from the blood, and O2 from the blood into the alveoli
What is involved in ventilation?
Intercostal muscles (lie between the ribs)
Diaphragm
Work together to change volume of the thorax, changing lung air pressure, inducing inspiration/expiration
Which breathing process requires energy?
Inhalation
Why do insects have specialised gas exchange?
Very low surface area to volume ratio compared to smaller organisms
Tough exoskeleton that largely inhibits gas exchange
Don't usually have haem groups in blood to carry oxygen.
Instead developed to deliver oxygen and remove CO2 directly from cells
What are spiracles?
External openings to the respiratory system along the exoskeleton, allowing for gas exchange
Sphincters open and close these spiracles
Spiracles lead to tracheae
What do sphincters do?
Open and close spiracles to prevent water loss due to vapour (produced from moist walls/tracheal fluid)
Usually closed during inactivity, but open due to increased CO2 levels or oxygen demand.
Tracheae (insects)
Direct air to tissues in insects
Moist walls for gas diffusion
Lined by spirals of chitin to prevent them from closing (like cartilage) which is relatively impermeable to gas
Branched into narrower tracheoles
Tracheoles (insects)
Narrow and abundant - large SA
Lack chitin - more permeable to gases
Tracheal fluid allows gases to dissolve before gas exchange.
Spread between cells for gas exchange and short diffusion system.
How do insect respiratory systems respond to oxygen demand increase?
Lactic acid is produced more in cells, lowering cell water potential
Water from tracheal fluid exits tracheoles
More surface area exposed for gas exchange/decrease of diffusion distance, drawing air into tracheoles via diffusion gradient
Mechanical ventilation of insects?
Bulk movement - Air is actively pumped into the system by muscular pumping movements of the thorax/abdomen
Changes volume of the body and pressure in tracheoles, drawing air in/out
Squeezes air from air sacs into tracheoles.
Collapsible enlarged trachea in insects?
Act as air reservoirs, increase the amount of air moved through the gas exchange system
Inflated/deflated by ventilating movements of the thorax and abdomen/movement of wings
Insect oxygen supply methods
Tracheal tubes - passive diffusion
Mechanical ventilation
Collapsible enlarged trachea
Operculum?
A bony flap that contains gills in an opercular cavity and covers these for protection
Adaptations of fish gills?
Lots of layers and lots of folded lamellae -> large surface area
Short diffusion path
ascularised and ventilated
Counter current blood flow in fish
Low oxygen blood enters the capillaries
Water passes over from the opposing direction of blood flow
Oxygen from water diffuses into the blood.
The concentration gradient is high because oxygenated blood is constantly removed
This high oxygen water than exits the gills
Tips of adjacent gill filaments overlap to increase resistance to water flow, and slow down movement
Stages of gill ventilation
The mouth opens to take water in
The buccal cavity floor is lowered, increasing the volume for water and decreasing pressure compared to outside
Water rushes in down pressure gradient. Mouth is shut
The opercular cavity expands, increasing volume and decreasing pressure
The buccal cavity floor is raised, increasing pressure compared to the opercular cavity, so water moves over the gills to the opercular cavity
The operculum opens and the sides of the opercular cavity move inwards to increase pressure.
Water rushes out through the operculum
Haemolymph?
Insect transport medium
Transports food, nitrogenous waste products, but NOT products of gas exchange
Haemocoel?
Insect body cavity
Why do multicellular organisms need specialised transport systems?
Increased metabolic demand
Smaller SA:V ratio, larger organisms
Hormones and enzymes are produced away from target cells
Removal of waste products
High oxygen demand
Open circulatory systems?
Low pressure
Haemolymph directly pumped into haemocoel, directly contacting tissues and cells.
Collected by drain-like open vessels to return fluid to heart
Seperate to gas exchange system
Closed circulatory systems?
Blood is pumped at high pressure that can be altered by vasodilation/constriction
Blood remains within the vessels and materials diffuse via capillaries
Veins carry blood to the heart; arteries carry from heart
The circulatory system also carries nutrients, gases, and waste products
Single circulatory system?
Blood only flows through the heart once for each circuit of the body
At the first capillary, O2 and CO2 are exchanged; at the second, substances are exchanged between blood and organ systems
Low pressure and low rate
Fish* and worms
Double circulatory system?
Greater pressure and flow rate
Four heart chambers
Elastic fibres?
Present in all lung tissues
Composed of elastin; stretch and recoil to allow flexible vessel walls
Recoil makes expiration a passive process
Smooth muscle?
Found throughotu the walls of the bronchi and bronchioles
Contract and relax to change lumen size therefore blood pressure/amount of air
Collagen?
Provides structural support to maintain vessel's shape and volume
Endothelium?
Smooth for easy flow
Features of arteries
Small lumen
Large muscular wall (more elastin than veins)
High pressure, pulse
No valves
Oxygenated blood from the heart*
Features of veins?
Wide lumen
Thin wall of muscles (less collagen and less elastic muscle than arteries)
Low pressure
Valves
Deoxygenated blood to the heart*
Found between big active body muscles - muscle contraction moves blood
Closer to the surface than arteries
Thin walls may distend/bulge
Features of capillaries?
Tiny lumen 1RBC thick
Thin wall of endothelium
Low pressure
No valves
Network supplies muscles with oxygen and nutrients for respiration; remove respiratory waste like CO2
Gaps between endothelial cells allow substances to leave in tissue fluid
Adaptations of capillaries
Large surface area
Larger total cross sectional area compared to arterioles means blood flow falls, allowing more time for diffusion of substances
Features of arterioles
Connect arteries and capillaries
More smooth muscle for vasoconstriction and vasodilation
Blood flow journey:
Lungs -> pulmonary veins -> left atrium -> left ventricle -> aorta -> body -> vena cava -> right atrium -> right ventricle -> pulmonary artery -> lungs
Oncotic pressure?
Tendency of water to move into blood from tissue fluid by osmosis
NEGATIVE
Hydrostatic pressure?
Pressure generated by a heart contracting to move water out of the plasma
POSITIVE
Tissue fluid?
Similar to plasma, lacks erythrocytes and plasma proteins
Vector for substances in blood to diffuse to cells
Lymph?
Similar to plasma, less oxygen and nutrients
Contains fatty acid
Tissue fluid that isn't reabsorbed (10%) drains into lymph capillaries to become lymph
Tissue fluid formation
Plasma proteins lower blood water potential, so water tends to move in by oncotic pressure. However, blood flow from the arterioles is under pressure for contraction - this is hydrostatic pressure - so this outweights oncotic pressure and forces plasma out to form tissue fluid.
Hydrostatic pressure falls at venule end, so oncotic pressure reabsorbs plasma.
Lymphatic system?
Lymph capillaries join up to form larger vessels - similar to veins, have valves and transport via muscle contraction.
Lymph returns to the blood via subclavian veins
Lymph nodes along lymph vessels are where lymphocytes build up.
Major in body's defence mechanism - enlarged lymph nodes are due to them intercepting bacteria
Positive cooperativity of haemoglobin
How the haemoglobin molecule changes shape each time to optimise bonding with oxygen molecules
Specialisation of erythrocytes
Transport oxygen around body. Flattened biconcave shape increases surface area to volume ratio optimising diffusion of oxygen into cell. Contain haemoglobin to carry oxygen. No nucleus or many other organelles increasing space for haemoglobin. Flexible so can squeeze through narrow capillaries.
Haemoglobin + oxygen ⇌
oxyhaemoglobin
Hb + 4O2 ⇌ Hb(O2)4
Forming Hb(O2)4 maintains a diffusion gradient of oxygen into the cell
Haemoglobin at low ppO2
Haemoglobin has a low affinity for oxygen
25% saturation at Kpa
Haemoglobin at higher ppO2
When an oxygen has binded, haemoglobin's quaternary structure changed to increase affinity of haem group for O2 - small increases in pp increases affinity.
At 7kpa, 75% saturation
Fourth oxygen (Hb)
Takes a large partial pressure to take up O2 due to the unlikeliness of collision
Often offloads in areas of significantly low pressure such as heavily respiring tissue
Haemoglobin oxygen affinity curve
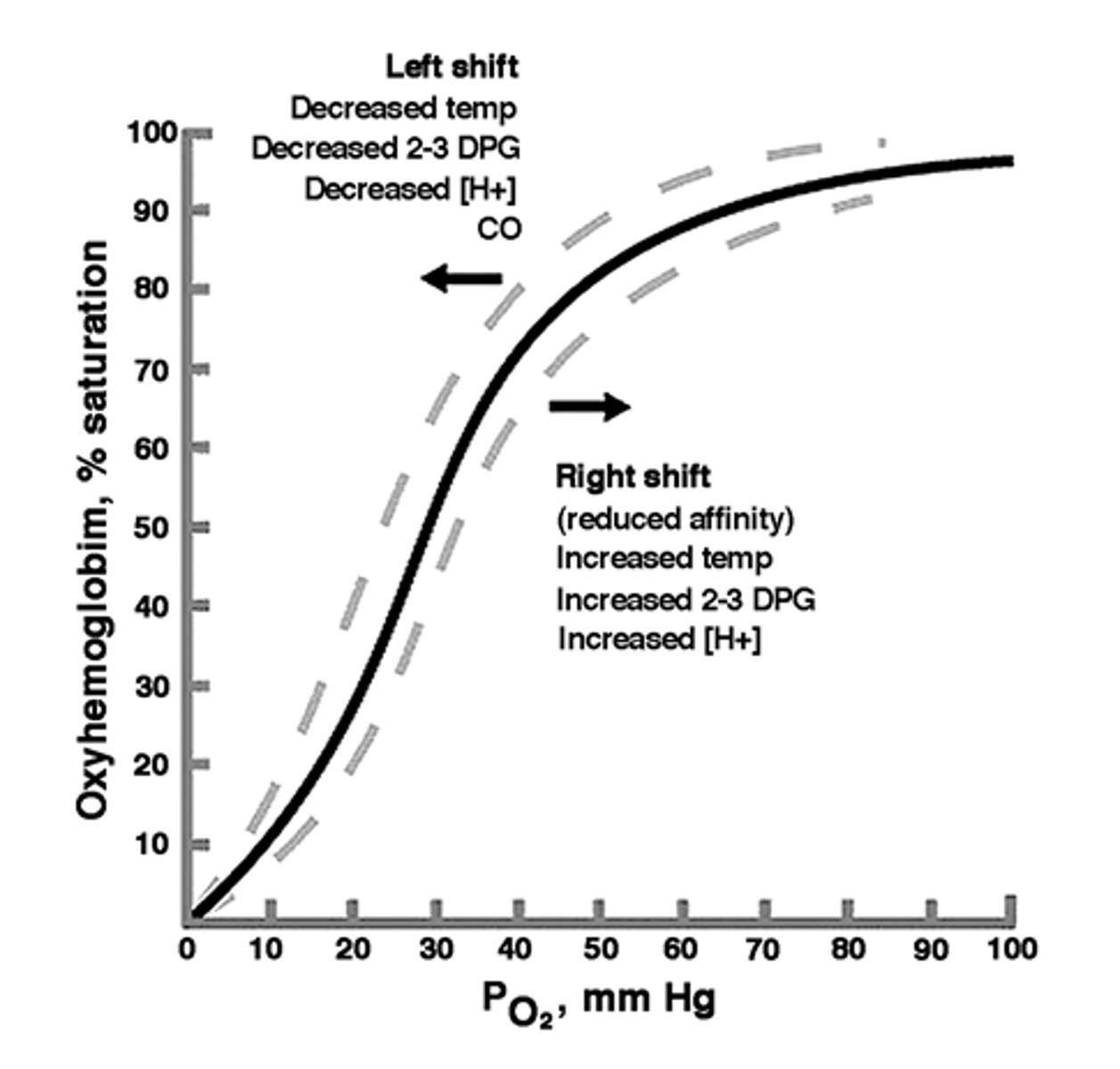
Where does haemoglobin unload and offload oxygen?
Haemoglobin takes in O2 at areas of high ppO2 - primarily the alveoli where it also offloads CO2
Haemoglobin unloads in areas of low ppO2 - high aerobic respiration such as tissues and cells
The Bohr Effect
At areas of high ppCO2, the oxygen dissociation curve shifts to the right, decreasing haemoglobin's affinity for oxygen. (this is due to the dissociation into H+ ions)
Hydrogen ions react to form haemoglobinic acid to prevent the build up of hydrogen ions and act as a buffer
It changes shape so that more oxygen is released when needed.
Chloride shift
The movement of chloride ions into erythrocytes while hydrogen carbonate ions move out into blood plasma, to maintain the cell's electrical balance
How can CO2 be transported in the blood?
5% dissolved in the plasma.
10-20% combined with amino groups in polypeptide chains of haemoglobin to form carbaminohaemoglobin.
75-85% converted into hydrogen carbonate ions in the cytoplasm of erythrocytes.
Carbon dioxide in the blood (equation)
Carbon dioxide + water ⇋ carbonic acid ⇋ hydrogen carbonate + hydrogen ions
CO2 + H2O ⇋ H2CO3 ⇋ H+ + HCO3-
What does haemoglobin form with H+?
Haemoglobinic acid, to act as a buffer and avoid changing haemoglobin pH
Erythrocytes at respiring cells (CO2)
Negative hydrogen carbonate ions diffuse out of the RBC via a gradient.
Chloride shift occurs to balance this.
Because CO2 is constantly converted to H2CO3, there is a diffusion gradient maintained into the cell. Carbon dioxide is able to be removed due to this
Erythrocytes at the lungs (CO2)
Hydrogen carbonate ions diffuse back into RBC and reform carbonic acid, this is then broken down into CO2 and water (and catalysed by carbonic anhydrase)
This releases CO2 which diffuses out of the lungs to be respired
Chloride ions also diffuse out.
How do fetus' gain O2?
The mother's oxygenated blood runs close to the deoxygenated fetal blood in the placenta.
Maternal blood has higher O2 concentration, so it diffuses into fetal blood.
How is efficiency of O2 diffusion into fetal blood increased?
Fetal haemoglobin has a slightly higher affinity for oxygen.
Fetal haemoglobin has two different polypeptide chains which cause O2 affinity to increase
Carbon dioxide from fetal blood diffuses into maternal blood, lowering the maternal haemoglobin's oxygen affinity
Vena cava?
Superior - receives blood from the upper body and head
Inferior - receives blood from the lower body
Tricuspid valve?
Between the right atrium and ventricle, preventing back flow
Bicuspid valve?
Between the left atrium and ventricle, preventing back flow
Semilunar valve?
Between the right ventricle and the pulmonary artery; also between the left ventricle and the aorta, preventing backflow
Septum?
Divides the left and right chambers of the heart, preventing mixing of deoxygenated and oxygenated blood
Cardiac cycle?
Events in a single heartbeat
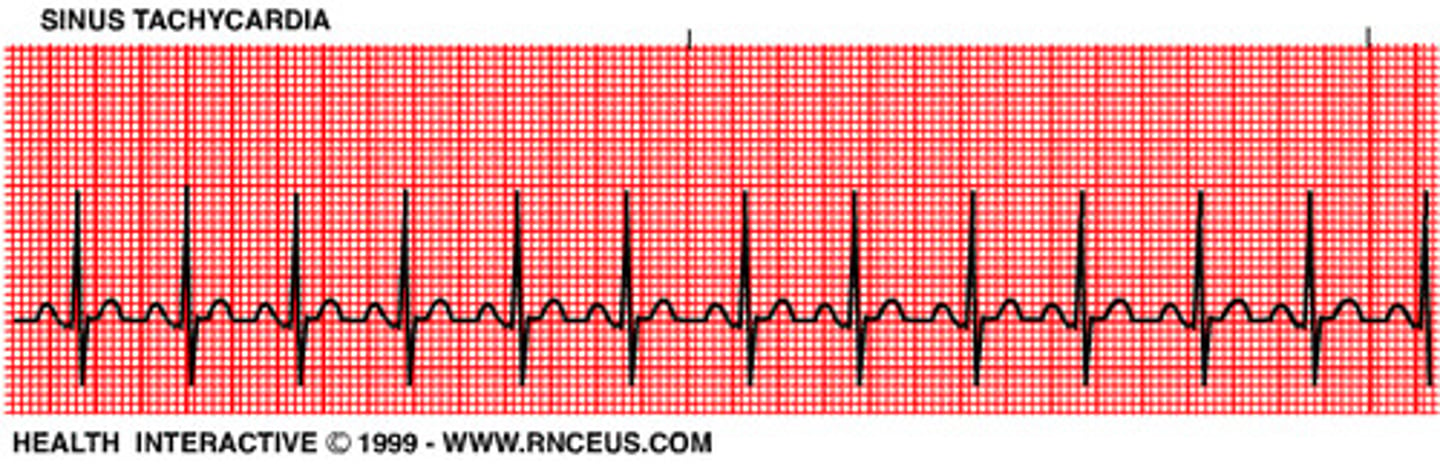
Tachycardia?
Overly rapid heartbeat
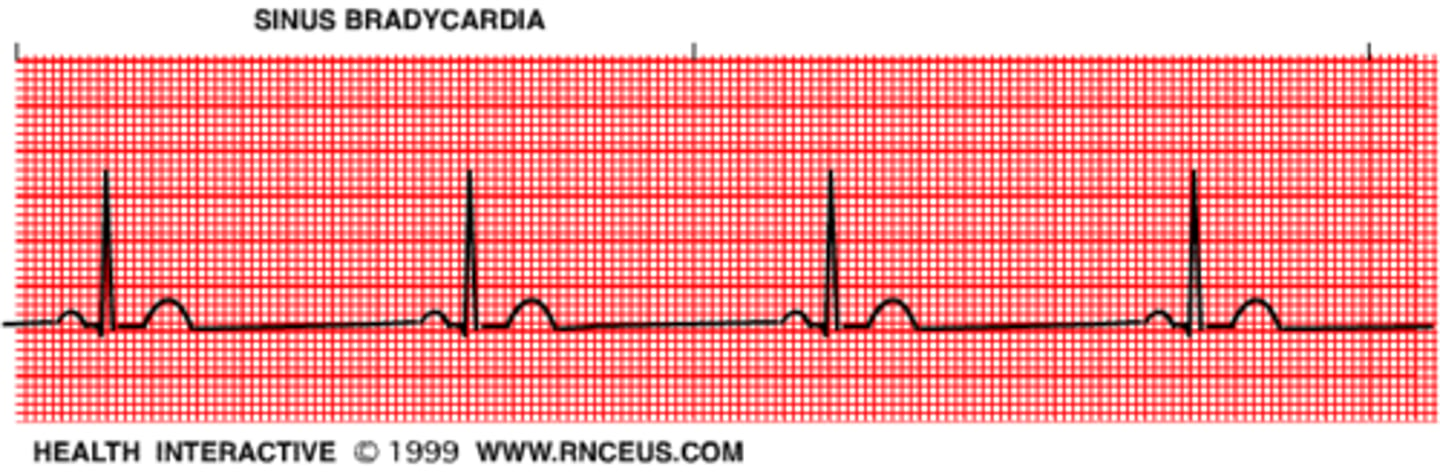
Bradycardia?
Abnormally slow heartbeat
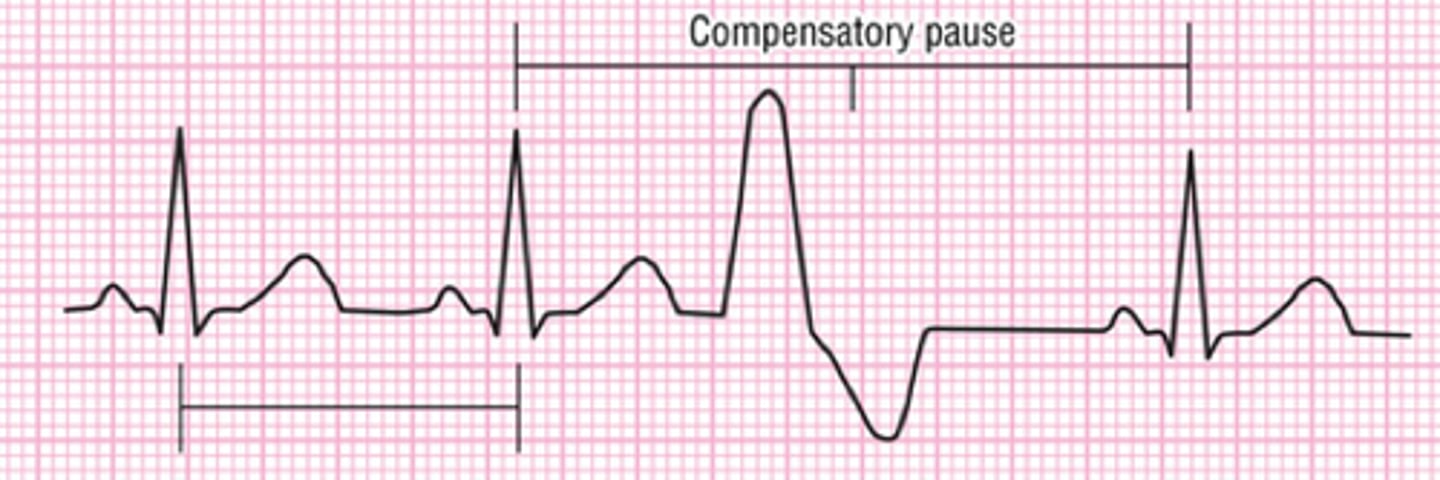
Ectopic heartbeat?
Extra heartbeats that are out of the normal rhythm.
Atrial fibrillation?
Rapid, random, ineffective contractions of the atrium

Coronary arteries?
Blood vessels that branch from the aorta and carry oxygen-rich blood to the heart muscle
Movement of deoxygenated blood?
Deoxygenated blood enters the right atrium from the vena cava at low pressure.
As blood flows in, pressure builds up until atrial pressure>ventricular pressure, so the tricuspid valve opens and blood enters the ventricle.
Atrial systole occurs to push remaining blood into ventricles.
This causes ventricular systole. Pressure in ventricles rises rapidly, when ventricular pressure>atrial pressure, the tricuspid valve closes to prevent backflow, but semi-lunar valve opens (atrial diastole happens)
The right ventricle contracts fully and pumps deoxygenated blood through semi-lunar valves into the pulmonary artery, which transports it to the capillary bed of the lungs.
Ventricular systole reduces ventricular pressure below that of the pulmonary artery, so semi-lunar valves shut.
Movement of oxygenated blood?
Oxygenated blood enters from the pulmonary vein at low pressure.
As blood flows in, pressure builds in the left atrium until atrial pressure>ventricular pressure. The bicuspid valve opens and atrial systole occurs to push all blood into the left ventricle.
This causes ventricular systole, and ventricular pressure rises rapidly. The bicuspid valve closes to prevent backflow, and semi-lunar valves open. (atrial diastole occurs)
The left ventricle contracts fully and pumps oxygenated blood through semi-lunar valves to aorta and the body.
Ventricular diastole occurs. When the ventricular pressure
SAN?
Site of pacemaker that iniates heartbeats
Found at the top of the right atrium
AVN?
Found near the semi-lunar valve, next to septum
Picks up SAN impulses and stimulates bundle of His
Bundle of His?
Bundle of conductive tissue made up of Purkyne fibres which penetrate through the septum between ventricles