Cardiovascular Physiology Overview and Key Concepts
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
129 Terms
What are the three main components of the cardiovascular (CV) system?
Pump, tubes, fluid.
Why is the cardiovascular system important?
It transports nutrients, gases, wastes, and hormones, and regulates temperature.
What occurs in the capillary beds of the lungs?
Gas exchange.
What do pulmonary arteries do?
Carry blood away from the heart to the lungs.
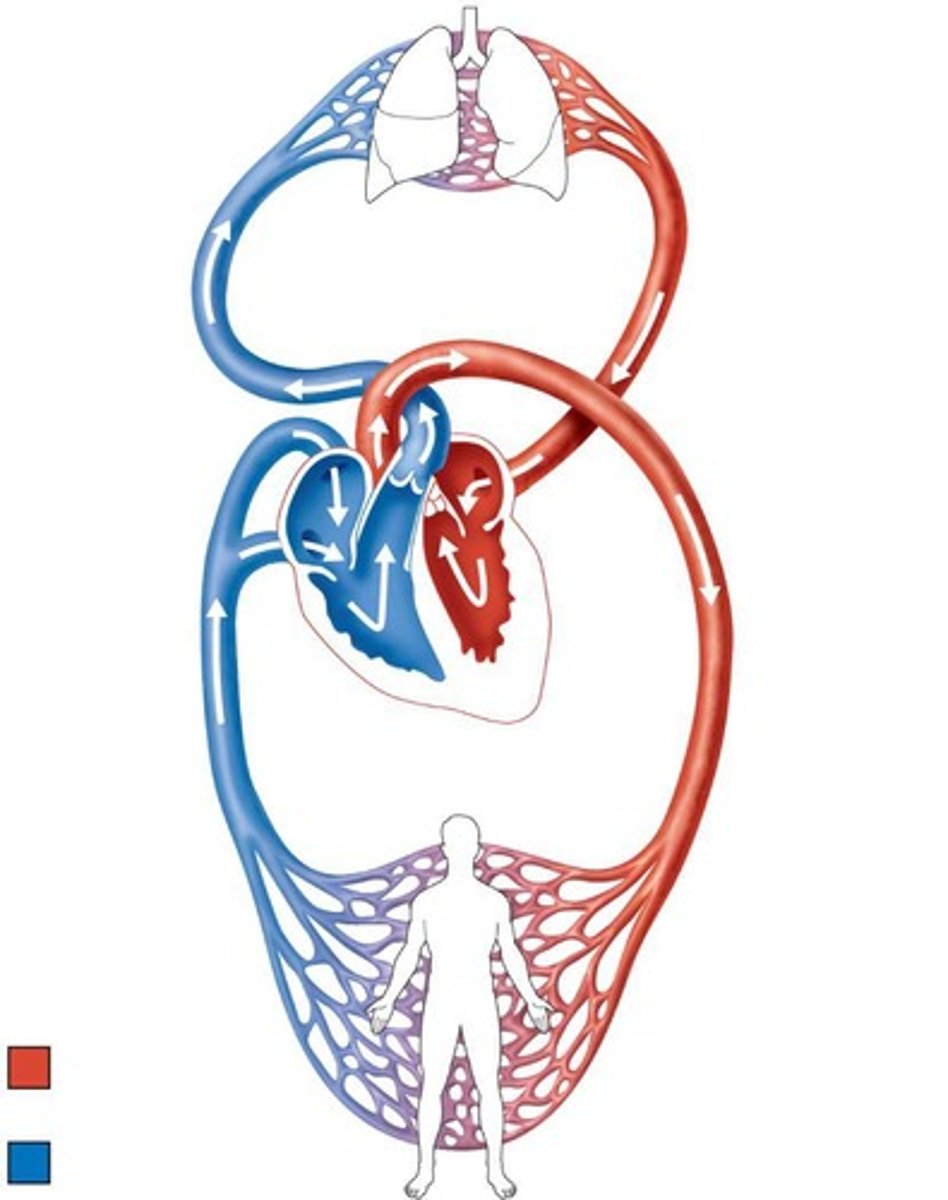
What do pulmonary veins do?
Carry oxygen-rich blood back to the heart from the lungs.
What is the function of the aorta?
It carries oxygen-rich blood from the heart to the body.
What is the role of veins in the cardiovascular system?
They carry oxygen-poor blood back to the heart.
What is the total blood volume in the human body?
4-6 liters.
What percentage of blood volume is found in veins?
70%.
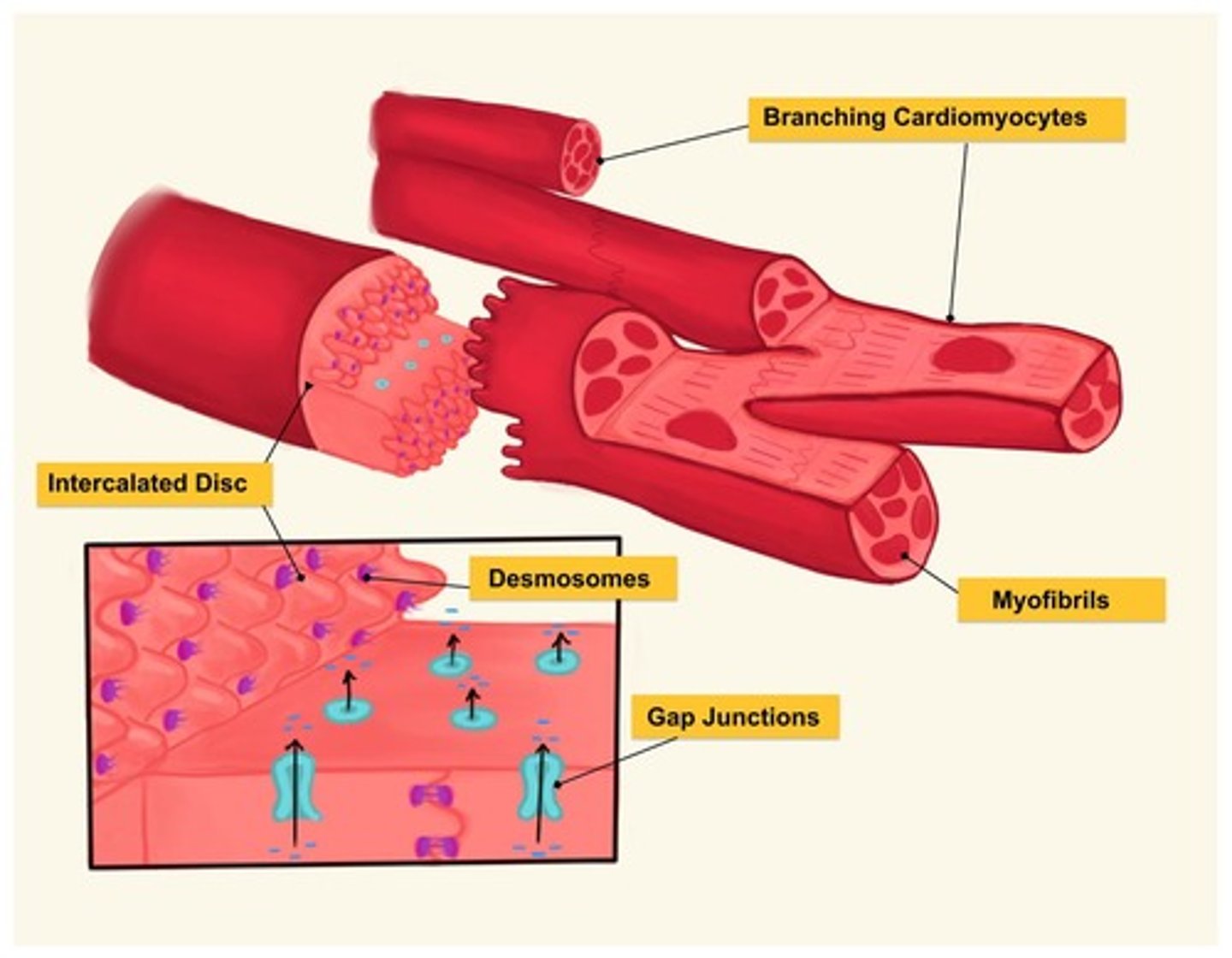
What are the two types of cardiomyocytes?
Contractile cells and nodal/conducting cells.
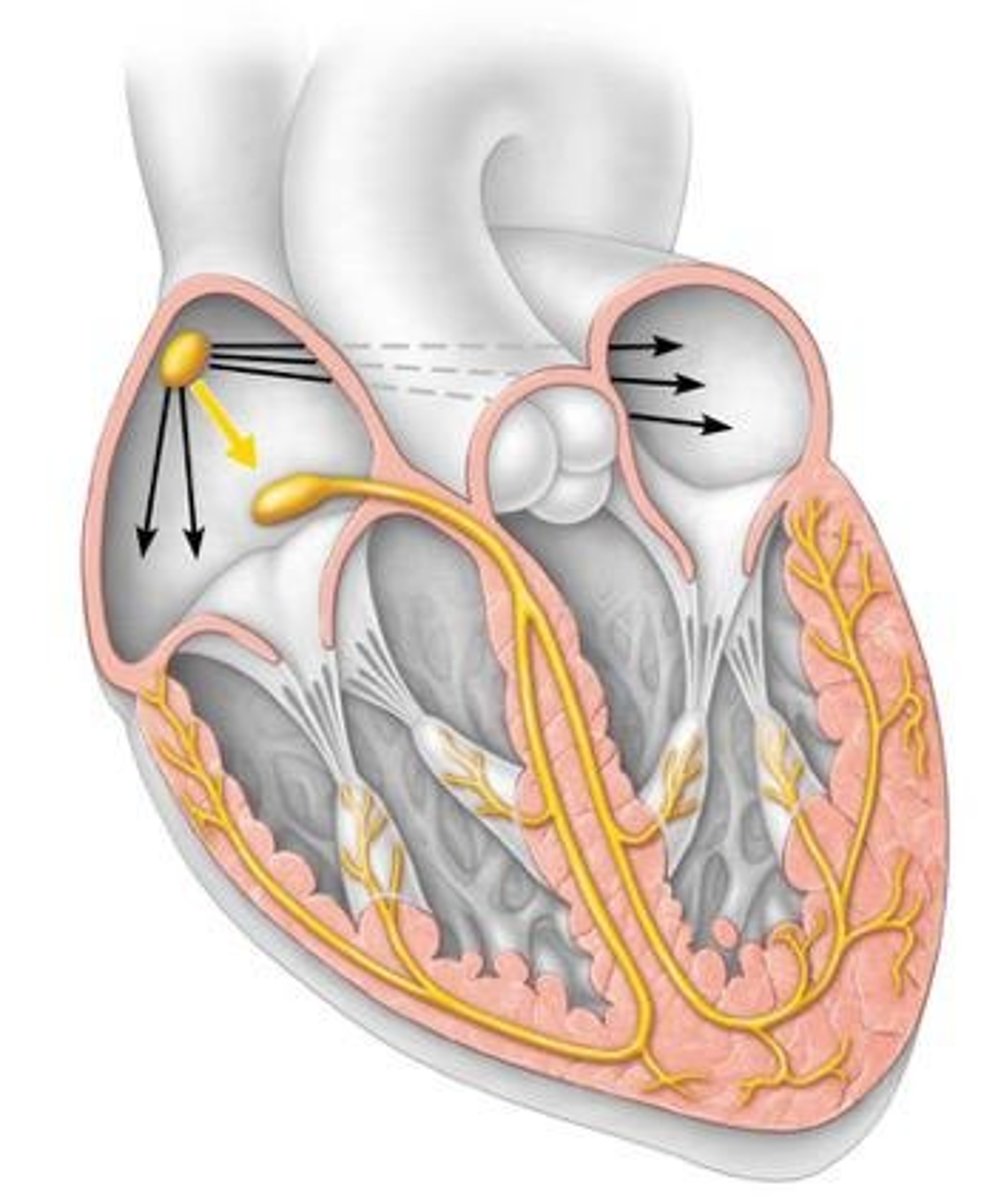
What is the primary function of nodal and conducting cells?
They are self-excitable and generate action potentials for heart contraction.
What is depolarization in cardiac cells?
It is when the cell becomes more positive than its resting membrane potential (RMP).
What is repolarization in cardiac cells?
It is when the positive cell returns to its resting membrane potential (RMP).
What is the threshold potential for a neuron to generate an action potential?
-55 mV.
What is the resting membrane potential (RMP) of a nodal cell?
No stable RMP, lowest at -60 mV.
What is the pacemaker potential in SA nodal cells?
It involves Na+, Ca2+, and K+ ions and leads to action potentials.
What is the sequence of the conducting system for action potential propagation?
1. Sinoatrial (SA) node, 2. Atrial muscle, 3. Atrioventricular (AV) node, 4. Atrioventricular bundle (Bundle of His), 5. Bundle branches (L & R), 6. Subendocardial branches (Purkinje fibers), 7. Ventricular muscle.
What is the significance of intercalated discs in myocardial cells?
They allow electrical connection through gap junctions.
What is the difference between skeletal myofibers and myocardial cells?
Skeletal myofibers are multinucleated and not electrically connected, while myocardial cells have a single nucleus and are electrically connected.
What is the role of calcium ions (Ca2+) in myocardial contraction?
Ca2+ is necessary for contraction in both contractile and nodal cells.
What happens during the action potential in nodal cells?
Ca2+ enters and K+ exits the cell, leading to depolarization and repolarization.
What is the sequence of events in the heart during an action potential?
Action potential occurs first, followed by contraction.
What does an electrocardiogram (ECG) measure?
It measures the sum of all electrical events in the heart.
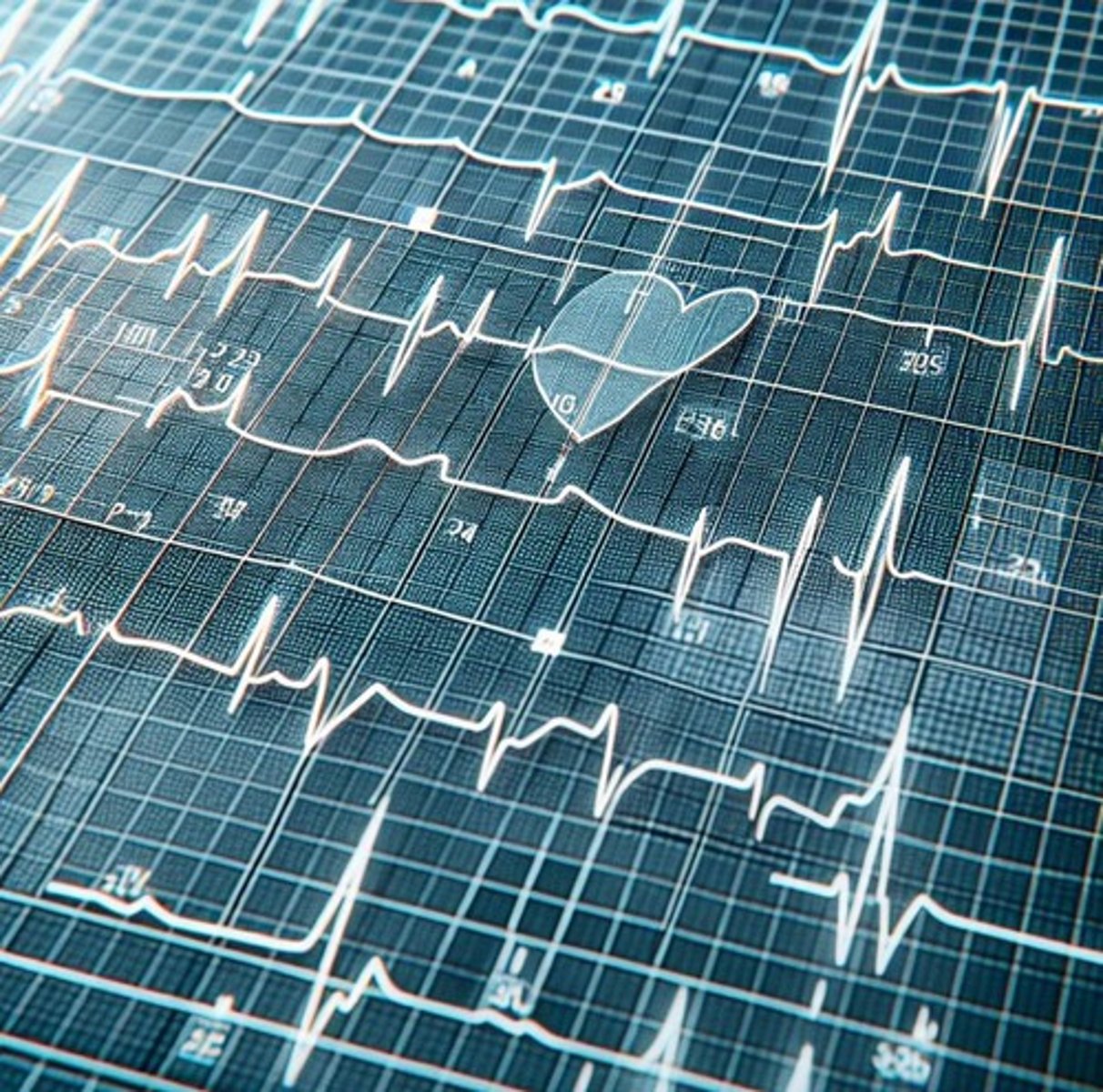
What can an ECG indicate about heart health?
It can indicate heart rate, heart damage (myocardial infarction), conduction issues, rhythm disturbances, and effects of drugs.
What is the resting heart rate for an average adult?
Approximately 70 beats per minute.
How do you calculate maximum heart rate?
220 minus your age in years.
What are the effects of parasympathetic stimulation on heart rate?
It decreases heart rate by increasing K+ permeability and decreasing Na+ and Ca2+ permeability.
What neurotransmitter is involved in parasympathetic innervation?
Acetylcholine (ACh).
What are the effects of sympathetic stimulation on heart rate?
It increases heart rate by increasing Na+ and Ca2+ permeability.
What neurotransmitter is involved in sympathetic innervation?
Norepinephrine (NE) or Epinephrine.
What are the phases of the cardiac cycle?
1. Atrial Systole 2. Isovolumetric Ventricular Systole 3. Ventricular Systole 4. Isovolumetric Ventricular Diastole 5. Late Ventricular Diastole.
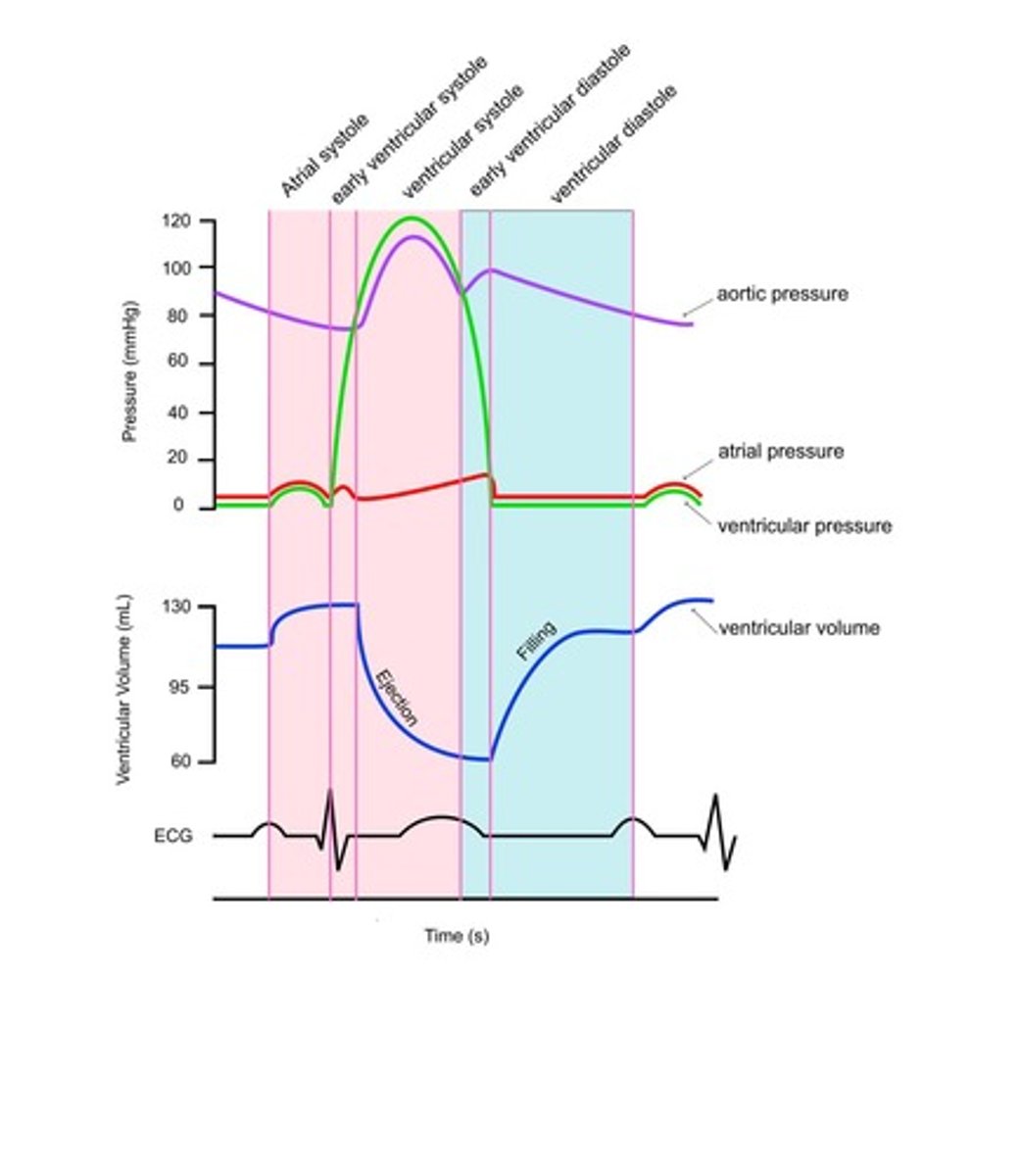
What happens during Atrial Systole?
The ECG shows a P wave, AV valves are open, and atrial pressure is higher than ventricular pressure.
What occurs during Isovolumetric Ventricular Systole?
The ECG shows a QRS wave, all valves are closed, and ventricular pressure is higher than atrial pressure but lower than aortic pressure.
What occurs during Ventricular Systole?
The aortic valve opens, ventricular pressure is higher than both atrial and aortic pressures.
What happens during Isovolumetric Ventricular Diastole?
The ECG shows a T wave, all valves are closed, and ventricular pressure drops below aortic pressure.
What occurs during Late Ventricular Diastole?
The AV valve opens, ventricular pressure drops below atrial pressure and is lower than aortic pressure.
What is stroke volume?
The amount of blood pumped per beat.
What is the relationship between pressure and blood flow in the heart?
Blood moves down a pressure gradient, from high to low pressure.
What occurs when pressure lines cross in the cardiac cycle?
Something happens to the heart valves, causing them to open or close.
What is the significance of the ECG event in relation to heart muscle contraction?
The ECG event occurs before heart muscle contraction or relaxation.
What is the intrinsic rate of the SA node?
Approximately 100 beats per minute.
What is the role of valves during the cardiac cycle?
Valves prevent backflow and must be open for blood to move.
What is the effect of sympathetic and parasympathetic stimulation on heart rate?
Sympathetic stimulation increases heart rate, while parasympathetic stimulation decreases it.
How does the heart rate change from rest to exercise?
Heart rate increases from approximately 70 beats/min at rest to 130 beats/min during exercise.
What is the definition of Stroke Volume?
The amount of blood ejected by the ventricle during one ventricular systole.
What is the formula for Cardiac Output?
Cardiac Output = Heart Rate x Stroke Volume.
What are the two main factors that control Stroke Volume?
1. Autonomic Nervous System Innervation 2. Preload on the heart.
What neurotransmitter is released by the parasympathetic nervous system and what effect does it have on Stroke Volume?
Acetylcholine is released, which decreases Ca2+ permeability, reducing the strength of contraction and thus minimally decreasing stroke volume.
How does the sympathetic nervous system affect Stroke Volume?
Norepinephrine/epinephrine increases Ca2+ permeability, enhancing the strength of contraction and thus increasing stroke volume.
What is End Diastolic Volume (EDV)?
The amount of blood in the ventricle after atrial systole.
What is End Systolic Volume (ESV)?
The amount of blood in the ventricle after ventricular systole.
What is the relationship between Stroke Volume, EDV, and ESV?
Stroke Volume = EDV - ESV.
What is Preload in the context of heart function?
Preload is the load on the heart prior to contraction, specifically the end diastolic volume (EDV).
How does an increase in EDV affect Stroke Volume?
An increase in EDV leads to greater stretch of the ventricles, resulting in a larger contraction and thus a bigger stroke volume.
What does the Frank-Starling Law state?
An increase in EDV will cause an increase in stroke volume.
What happens to the force of contraction when preload increases?
The force of contraction increases due to the increased stretch of the contractile cells of the ventricles.
How does Stroke Volume affect Cardiac Output?
An increase in Stroke Volume increases Cardiac Output, since Cardiac Output = Heart Rate x Stroke Volume.
What is the effect of larger EDV on ventricular contraction?
Larger EDV results in a larger contraction, leading to a bigger stroke volume.
What is the primary role of the Autonomic Nervous System in regulating Stroke Volume?
It modulates the strength of cardiac contractions through sympathetic and parasympathetic innervation.
What receptors do norepinephrine and epinephrine bind to in the heart?
They bind to adrenergic receptors on the ventricular muscle.
What is the significance of calcium permeability in cardiac muscle contraction?
Increased calcium permeability enhances the strength of contraction, thereby increasing stroke volume.
What is the relationship between preload and the stretch of contractile cells?
Increased preload leads to increased stretch of contractile cells, enhancing their force of contraction.
What is the physiological consequence of decreased stroke volume?
Decreased stroke volume can lead to reduced cardiac output, affecting overall blood circulation.
How can one increase End Diastolic Volume (EDV)?
By increasing venous return to the heart, which can be influenced by factors such as blood volume and body position.
What is the role of the autonomic nervous system in cardiac function?
It regulates heart rate and the strength of cardiac contractions through sympathetic and parasympathetic pathways.
What mechanism increases venous return to the heart?
The skeletal muscle pump, which squeezes blood in veins back to the heart.
What effect does increased venous return have on end-diastolic volume (EDV)?
It increases EDV.
What is the relationship between EDV and stroke volume (SV)?
An increase in EDV leads to an increase in stroke volume (SV).
What is the primary function of capillary beds in the lungs?
Gas exchange occurs in the capillary beds of the lungs.
What do arteries do in the cardiovascular system?
Arteries carry blood away from the heart.
What is the pathway of blood from the heart to the body tissues and back?
Blood is pumped from the heart through arteries to capillaries, where exchange occurs, then returns via veins.
What type of blood do pulmonary veins carry?
Oxygen-rich, carbon dioxide-poor blood.
What type of blood do venae cavae carry?
Oxygen-poor, carbon dioxide-rich blood.
What is the function of the tunica externa in blood vessels?
The tunica externa provides structural support and protection, made of fibrous connective tissue.
What is the role of the tunica media in blood vessels?
The tunica media contains smooth muscle and elastic fibers, allowing for vessel contraction and dilation.
What is the primary characteristic of arteries?
Arteries have a large diameter, thin walls compared to diameter, and lots of elastic fibers.
What is the blood pressure characteristic of arteries?
Arteries experience very high blood pressure, which is pulsatile.
What is the primary function of arterioles?
Arterioles are resistance vessels that control blood flow through vasoconstriction and vasodilation.
What happens to blood pressure as it moves through arterioles?
There is a large drop in pressure due to high resistance.
What is the purpose of regulating blood flow in the cardiovascular system?
To increase blood supply to active tissues and decrease it to inactive tissues, while maintaining supply to vital organs.
What is the relationship between pressure, blood flow, and resistance?
Blood flow is directly proportional to the pressure gradient and inversely proportional to resistance.
What is the formula for blood flow in relation to pressure and resistance?
Blood Flow = Pressure Gradient / Resistance.
What factors affect resistance in the circulatory system?
Resistance is affected by the length of the vessel, viscosity of the fluid, and the radius of the vessel.
What is the significance of the radius of a vessel in relation to resistance?
Resistance is proportional to the fourth power of the radius (r^4), meaning small changes in radius significantly affect resistance.
What is the purpose of the cardiovascular system's structure and tissue content?
The structure and tissue content of blood vessels determine their function.
What is the primary function of the systemic circuit?
The systemic circuit is responsible for delivering oxygen-rich blood to all body tissues.
What is the formula for blood flow?
Blood Flow = (P1 - P2) x r^4
What is the typical blood flow rate mentioned in the notes?
1.25 L/min
What are capillaries known as in the circulatory system?
Exchange vessels.
What is the structure of capillaries?
Capillaries are one endothelial cell thick with very thin walls, which is great for diffusion.
What are the blood characteristics of capillaries?
They have low blood pressure, a small drop in pressure, very low blood velocity, and a huge total cross-sectional area for diffusion.
What is the primary purpose of capillaries?
To exchange gases, wastes, nutrients, etc.
How does cross-sectional area affect blood velocity?
More cross-sectional area results in slower flow, which maximizes exchange.
What are the two types of capillaries mentioned?
Continuous capillaries and fenestrated capillaries.
What is the permeability of continuous capillaries compared to fenestrated capillaries?
Continuous capillaries are less permeable, while fenestrated capillaries are more permeable.
What is filtration in the context of capillaries?
Filtration is the movement of fluid out of a capillary.
What is reabsorption in the context of capillaries?
Reabsorption is the movement of fluid into a capillary.
What are the four Starling Forces?
1. Capillary Hydrostatic Pressure (Pc) 2. Interstitial Fluid Hydrostatic Pressure (PIF) 3. Capillary Plasma Osmotic Pressure (∏c) 4. Interstitial Fluid Osmotic Pressure (∏IF)
What is the capillary hydrostatic pressure range?
15 to 35 mmHg.
What is the typical capillary plasma osmotic pressure (∏c)?
25 mmHg.