HEMA 311: Hematopoiesis
1/135
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
136 Terms
Hematopoiesis
Continuous, regulated process of blood cell production that includes cell renewal, proliferation, differentiation, and maturation
Hematopoietic System
Serves as a functional model to study stem cell function
Hematopoietic Stem Cell (HSC)
Capable of self-renewal and directed differentiation into all required cell lineages
Mesoblastic Phase
When: 19th - 20th day of gestation
Where: blood islands of yolk sac (mesoderm)
What:
Primitive erythroblasts
Angioblasts
Embryonic HGBs (Gower I, Gower II, and Portland HGB)
8th - 12th Week
What stage of gestation does the production of cells lasts in mesoblastic phase?
Angioblasts
Product in mesoblastic phase that forms the blood vessels
3rd Month
The production of embryonic hemoglobin stops because blood islands disappear after what stage of gestation?
Aorta-Gonad-Mesonephros (AGM) Region
Where cells of mesodermal origin migrate to
Give rise to definitive erythroblasts and later into HSCs
Yolk Sac Phase
Other term for mesoblastic phase
Gower-I
Globin chains:
2 epsilon
2 zeta
Remember: 1 = EZ
Gower-II
Globin chains:
2 alpha
2 epsilon
Remember: 2 = TAE
Portland HGB
Globin chains:
2 zeta
2 gamma
Remember: ZiGa si Portland
Hepatic Phase
When: 5th - 7th week of gestation
Where: Fetal liver
What:
Development of lymphoid organs
Definitive erythroblasts
Granulocytes and Megakaryocytes
Lymphocytes
Monocytes
Fetal hemoglobin (Hgb F) and Adult hemoglobin (Hgb A)
Intravascular (within blood vessel)
Is hematopoiesis during the mesoblastic phase intravascular or extravascular?
Extravascular (outside of blood vessel)
Is hematopoiesis during the hepatic phase intravascular or extravascular?
6th Month
Hematopoiesis in the hepatic phase gradually declines after what stage of gestation?
Thymus
First fully developed organ in the fetus
T Cell production
Fetal Hemoglobin (Hgb F).
Predominant hemoglobin during the hepatic phase.
upto 1 year old
Spleen
Aside from the kidney, which organ produces B cells?
100 days
Minimum life span of RBCs
140 days
Maximum life span of RBCs
2nd Week
At what point in fetal development does the liver stop producing blood cells but remains capable of reactivation during severe blood loss?
Fetal Hemoglobin (Hgb F)
Globin chains:
2 alpha
2 gamma
Remember: F-A-G
120 days
Average life span of RBCs
Adult Hemoglobin (Hgb A1)
Globin chains:
2 alpha
2 beta
Adult Hemoglobin (Hgb A2)
Globin chains:
2 alpha
2 delta
Adult Hemoglobin (Hgb A)
Hemoglobin during the hepatic phase that is only in detectable levels
Erythropoiesis
What type of blood cell production is the mesoblastic phase confined to?
Extramedullary Hematopoiesis
Hematopoiesis that occurs outside the bone marrow
Medullary Phase
When: starts at 24th week of gestation (4th - 5th month of fetal development) until death
Where: Medulla / Bone Marrow Cavity (inner part of the bone)
What:
HSCs and Mesenchymal cells migrate into the medulla
Granulocytes and Megakaryocytes
Blood cells formed during the hepatic phase in the 3rd month of gestation
Lymphocytes
Blood cells formed during the hepatic phase in the 4th month of gestation
Monocytes
Blood cells formed during the hepatic phase in the 5th month of gestation
Mesenchymal Cells
A type of embryonic tissue that differentiate into structural elements to support developing blood cells
Myeloid Phase
Myeloid activity is apparent during this stage
Other term for medullary phase
3:1 - 4:1
Normal myeloid-to-erythroid (M:E) ratio in adults
Infection
6:1 (M:E ratio)
Leukemia
25:1 (M:E ratio)
Myeloid Hyperplasia
20:1 (M:E ratio)
Myeloid Hypoplasia
3:20 (M:E ratio)
Erythroid Hyperplasia
1:20 (M:E ratio)
Erythroid Hypoplasia
5:1 (M:E ratio)
Adult Hemoglobin (Hgb A).
Predominant Hgb after 1 year old.
Detectable Cytokines in Medullary Phase
Erythropoietin (EPO)
Granulocyte colony-stimulating factor (G-CSF)
Granulocyte-Macrophage colony-stimulating factor (GM-CSF)
Cytokines
What group of signaling proteins primarily regulates HSC’s production of blood cells during the medullary phase?
Lymphocytes.
What blood cell is mostly produced through extramedullary hematopoiesis?.
Primary Lymphoid Tissue
Where T and B lymphocytes are derived
Bone marrow
Thymus
Secondary Lymphoid Tissue
Where lymphoid cells respond to foreign Ag
Spleen
Lymph nodes
Mucosa-associated lymphoid tissue (MALT)
Gut-associated lymphoid tissue (GALT)
Infancy and Early Childhood
80 - 90% active marrow
Stage of life where all the bones in the body contain primarily red marrow
5 - 7 Yrs Old
60% active marrow
Stage of life where retrogression occurs (active marrow > adipocytes)
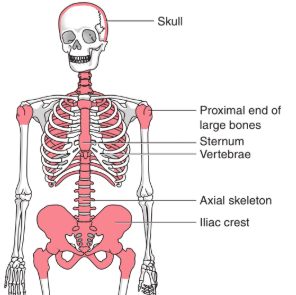
Adult
40% active marrow
Stage of life where active marrow is restricted to the:
Sternum
Vertebrae
Scapulae
Pelvis / Iliac crest
Ribs
Skull
Proximal portion of long bones
Marrow Cellularity
Ratio of red marrow to yellow marrow; usually decreases w/ age
Normocellular
Marrow has 30 - 70% HSCs
Hypocellular
Marrow has less than 30% HSCs
Hypercellular
Marrow has more than 70% HSCs
Aplastic
Marrow has few or no HSCs
Sternum
Main source of blood cell production in adults
Iliac Crest
Safest, most accessible site for bone marrow aspiration or biopsy
Iron 52
Iron 59
Technetium 99m-colloid
Dyes for identification of active hematopoietic tissue
Direct Aspirate Smears
Wedge-shaped smear
Avoid crushing the spicules
Anticoagulated Aspirate Smears
K3 EDTA
Crush Smears
Places additional glass slide directly over the specimen
Imprints
Closely replicate aspirate morphology
Concentrate Smears
Narrow-bore glass or a plastic tube such as “Wintrobe HCT tube”
Histologic Sections
10% Formalin
Zenker glacial acetic acid
B5 fixative
Marrow Smear Dyes
Wright’s stain
Wright-Giemsa stain
Stromal Cells
Cells in the bone marrow that secrete a semifluid extracellular matrix that serves to anchor developing hematopoietic cells in the bone cavity
Regulation of hematopoietic stem and progenitor cell survival and differentiation
Endothelial Cells
A stromal cell that regulates the flow of particles entering and leaving hematopoietic spaces
Adipocytes
A stromal cell that secretes steroids and regulates the volume of the marrow
Macrophages
A phagocytic stromal cell that secretes cytokines for regulation of hematopoiesis (together with LYMPHs)
Osteoblasts
Bone-forming stromal cells
Osteoclasts
Bone-resorbing stromal cells
Reticular Adventitial Cells
A stromal cell that forms a supporting lattice for the developing hematopoietic cells
Fibroblasts
Other term for reticular adventitial cells
Red Marrow
Composed of hematopoietic cells arranged in extravascular cords
Erythroblasts (in red marrow)
Develops in small clusters; located adjacent to the outer surfaces of vascular sinuses
Megakaryocytes (in red marrow)
Facilitates the release of platelets into the lumen of the sinus; located adjacent to the walls of vascular sinuses
Immature (myeloid) Granulocytic Cells (in red marrow)
Located deep w/n the cords but moves closer to the vascular sinuses as they mature along their differentiation pathway
Hematopoietic Microenvironment
Plays an important role in nurturing and protecting HSCs and regulating a balance among their quiescence, self-renewal, and differentiation
Niches
Other term for hematopoietic microenvironment
Spleen.
Largest lymphoid organ in the body.
350 mL
In a healthy individual, how much blood does the spleen contain?
Adenitis
Infection of the lymph node
6 Billion
2.5 B (erythrocytes)
2.5 B (platelets)
1 B (granulocytes)
How many blood cells per kg of body weight are produced each day?
Hematopoietic Stem Cell (HSC)
Differentiates into progenitor cells committed to either lymphoid or myeloid lineages when stimulated by cytokines
Monophyletic Theory
Suggests that all blood cells are derived from a single progenitor stem cell
Pluripotent Hematopoietic Stem Cell (PHSC)
The single progenitor stem cell in monophyletic theory is called a ________
Polyphyletic Theory
Suggests that each of the blood cell lineages is derived from its own unique stem cell
Apoptosis
Aside from self-renewal and differentiation, what is a possible fate for HSCs?
Stochastic Model of Hematopoiesis
Hematopoiesis is a random process whereby the HSC randomly commits to self-renewal or differentiation
Instructive Model of Hematopoiesis
The microenvironment in the bone marrow determines whether the HSC will self-renew or differentiate
Common Myeloid / Lymphoid Progenitor
Differentiates into lineage-specific progenitors (colony-forming units or CFU)
Lineage-specific Progenitors
Give rise to morphologically recognizable lineage-specific precursor cells
Megakaryocytes
Largest cells found in the bone marrow
Precursor Cells
Blast forms that undergo maturation
Differentiation
HSC > Common Myeloid / Lymphoid progenitors
Maturation
Precursor (blast) cells > mature cells
CFU-GEMM
Cell line:
Granulocyte
Erythrocyte
Megakaryocyte
Monocyte
CFU-E
Cell line:
Erythrocyte
CFU-Meg
Cell line:
Megakaryocyte