Screening- Dysphagia
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
91 Terms
screening goal:
identify individuals at risk for swallowing difficulties so that
appropriate f/u assessments and interventions can be initiated to improve
their safety and quality of life, particularly in healthcare settings like hospitals or long-term care facilities
outcome of coordinated movements
If all movements are executed properly, then output would be accurate
reduced strength
reduced accuracy, tone and ROM
increased/variable tone
reduced/variable speed, ROM, steadiness, and accuracy
reduced ROM
variations in speed,tone, and accuracy
at rest our face should be:
grossly symmetric with normal tone and little spontaneous movement
things we should ask when assessing face
is their face symmetric?
is their face droopy?
how are the angles of their mouth?
is there flattening of nasolabial fold?
pt should be instructed to attempt a spontaneous smile
screening is defines as:
• Non-billable process
• Identify patients who may be candidates for
dysphagia evaluation and treatment
• “Hands-off”
• Do NOT touch patient!!
• Takes approximately 15 minutes
• No doctor’s orders are required
• Patients with risky diagnosis should be
screened
screening is completed for two reasons:
Exclude patients who do not need an evaluation
because:
• No swallowing problem or a risky diagnosis
(leg or arm fx)
OR
• Need to be NPO either temporarily or
permanently due to some other reason (long
hx of NPO)
red flag behaviors for screenings
recurrent pneumonia
unplanned weight loss
coughing with meds or at meals
ent consult with cord paralysis
labored breathing (especially after eating)
reporting of wet vocal quality (gurgly voice)- suggests pooling on surface of VF
difficulty with chewing
reported loss of appetite
dehydration- changes in skin integrity
recurrent temperature spikes w/ no known cause
history of gastrointestinal problems
recent changes in eating habits
non-oral feeding (or any Hx thereof)
abnormal oral feeding
diagnosis with high risk of dysphagia
cerebrovascular accident (CVA)
brainstem infarcts
intracerebral hemorrhage
multiple sclerosis
cerebral palsy
myasthenia gravis
alzheimers dementia
Hx of malnutrition
Parkinson’s Disease
Muscular Distrophy
Tardive dyskinesia
Spinal cord injury, esp in affected cervical or thoracic vertebrae
if patient has spinal injury on these cervical vertebrae can cause dysphagia
C3, c4, C5
enteral feeding
by way of gastrointestinal tract, through nose, mouth, or stomach via tube typically
parenteral feeding
other than gastrointestinal tract (vein or artery)
components of screening process
read chart
look for red flags
question staff and family on onset of illness, patent awareness, hadicapping etc
interview with patient staff and family
Sudden changes in patient’s food
preference
2. Documented difficulty chewing
3. Recent diet changes
4. Duration of patient’s mealtime
5. Necessity for assistance at mealtime
6. Choking, coughing, discomfort, drooling
7. Unusual posture at mealtime
8. Time between end of meal and sleep or nap
9. Refusal to eat
10.Evidence of pocketing
face to face screening with patient
Observe patient during mealtime to see how he/she
manages food and liquids
• Look for any red flags
• Observe rate and amounts of food presentation
• Is there coughing/choking?
• Is the patient pocketing?
• Does patient lose most food before it is masticated?
• All of these would warrant further evaluation
observe patients cognitive and awareness
Put all observational and anecdotal information
together to make professional judgment
• Is the patient a candidate for evaluation AND
treatment?
• If so, request doctor’s order for further evaluation –
Clinical or Bedside Evaluation
• If not, provide palliative recommendations to doctor
and family for patient’s well-being…
request doctor’s orders for eval and tx
This is a must for reimbursement!
•Many doctors will be angry if SLP begins
assessment and/or treatment without doctor
knowledge and consent
•Doctor’s order must contain:
•Diagnosis
•Issue to be evaluated
•Clarification order:
•After evaluation
•Indicates intensity of tx
screening does not
identify the nature of the problem
just identifies who is at risk
clinical/bedside evaluates ____ phase and can provide clues about ____- phase
oral; pharyngeal
bedside evaluation
initial step
sometimes all we can do if pt is agitates/combative/lethargis
patient only has oral phase issues
If pharyngeal phase is a concern:
Patient is at risk for aspiration
• Usually diet is modified or patient is made
NPO
aspiration cannot be confirmed or ruled out solely with a bedside exam
40-67% of patients may be silent aspirators with no signs/symptoms
purpose of clinical exam
Integrate info from interview, case history, medical records, and collaboration between SLP and Nursing (NSG)
• Determine need for
interview, case history,
instrumental exam
medical records, and
• Determine if patient is
collaboration between
candidate for therapy
SLP and Nursing
• Recommend route of
(NSG)
nutrition and hydration
• Observe and assess
• Recommend tx
oral motor function
• Counsel and educate
• Characteristics of
patient and family, along
dysphagia
with MD if necessary
components of clinical/beside exam
Chart Review
• Case History with a list of signs and
symptoms – chart/patient interview
• Nutrition history – chart
• Respiratory status - chart
• Nursing Assessment – chart/Nurse interview
• Bedside Exam/Clinical dysphagia eval:
• OM and Laryngeal exam
• Respiratory status and Cognition
• Swallowing
info to obtain from chart:
medical history
referral
signs of dysphagia
nutrition/hydration status
medication list
respiratory status
nursing assessment- to determine pts cognitive status
other evals/procedures patient has undergone
medical history
• Admitting diagnosis
• Functional problems observed
• Level of alertness (LOA)
• Previous diagnoses and treatment
• Advance directive (i.e., any interventions which can
be performed)
• Pre-morbid status (i.e., ADLs)
case history is affected by:
• Patient’s cognitive abilities
• Patient’s personality
• Whether patient perceives a problem
• What has already been established by other
professionals
• Severity of speech deficit (breathy=no or
inadequate VF adduction)
• History can be provided by someone close to patient
• History should be controlled by clinician not patient
case history
why are you here?
provide SLP more info about orientation, awareness abut speech and/or swallowing
ability to provide hx and depth and manner of hx provides info about language abilities
age/education, occupation, family ststua
Hx of childhood speech, language, or hearing deficit, any tx and if problem has resolved
signs
what the SLP observes, what we see while watching pt such as choking, gurgly voice, etc
symptoms
what patient reports is wrong/ family
signs of possible aspiration
• Increased temperature
• Drooling/increased secretions
• Weight loss
• Coughing/choking
• Pocketing food
• Pneumonia
• Self-imposed changes in diet
• Dehydration
symptoms of aspiration
• Pain (odynophagia)
• Globus
• Heartburn
• Bad taste in mouth
• Food “won’t go down”
• Nasal burning or dripping
• Takes too long to eat
• Vomiting-immediate or later?
• Voice has changed
• Other neurological symptoms
nutrition history
• Current diet
Amount eaten
Restrictions
• How long does it take to eat?
• Alternate method of feeding – Ensure or Boost
• Oral health/dentures affecting?
respiratory status
•Lung sounds
Rhonchi: coarse, dry rale in bronchial tubes
Rale: abnormal respiratory sound
Wheeze: whistling respiratory sound
Chest x-rays
•Infiltrates
•Does the lobe matter?
•Right Mid and Lower
•Oxygen therapy
•Mode of delivery
•Face mask
•Nasal cannula
nursing assessment
• Cognitive assessment
• Observations of patient
• Previous living situation
• Family support/involvement
• Sensory impairments
• Blind
• Hard of Hearing (HOH)
other evals we can do
oral motor exam
• Observe symmetry of structures, condition of
dentition, and oral hygiene
• Assess strength, coordination, and mobility of oral
structures
6 features in production of speech
Strength and Speed
• ROM and Steadiness
• Tone and Accuracy
strength
sufficient amount to function normally along with a reserve for periods of extended contraction without fatigue or against resistance
if the muscle is weak 3 patterns may emerge:
• No contraction (failure to move = no mvmt)
• Fatigue quickly with detrimental effects on
contraction (lessens with time)
• Unable to sustain contraction (lessens
immediately)
strength affects all three speech valves
• Articulation (i.e., at point of constriction)
• Velopharyngeal (i.e., VPI or nasal
regurgitation)
• Laryngeal (i.e., weak or breathy voice)
speed
• Muscle activity during speech is rapid
• Quick, unsustained, discrete mvmts are phasic
• Slow mvmt is common and has greater capacity for
sustained work
• Affects all valves and all aspects of production
• Produce 14 phones per second in conversation
• Single contraction or rep. of same contraction
• Contraction begins quickly, reaches target and relax
rapidly
ROM
• Distance traveled by speech structures is precise
• Excessive ROM is uncommon
• Restricted ROM is common in presence of slow,
normal, or rapid rate
• Affects prosody
• Illustrated in perceptual/acoustic analysis, visible in
speech and non-speech movement of articulators, and
measured physiologically
steadiness
• Normal movement typically has no interruption or
oscillation
• At rest, there is 8 to 12 Hz oscillation of muscles
• Amplitude can increase to visibly detectable levels in
healthy humans
• Physiologic tremor occurs during extreme fatigue,
emotional stress, and shivering
• Most common hyperkinesia is tremor, which consists
of alternating, repetitive, rhythmic oscillations of a
body part (3 to 12 Hz)
how does neurologic impairment affect steadiness?
steadiness breaks down and results in involuntary movement
4 types of tremor:
• Resting tremor = tremor at rest
• Action tremor = during movement
• Terminal tremor = end of a movement
• Postural tremor = when a structure is
maintained against gravity
Holding arms out from body for extended
period of time
4 types of hyperkinesia
dystonia, dyskinesia, chorea, athetosis
dystonia
a movement disorder characterized by sustained or intermittent involuntary muscle contractions that cause abnormal postures and movements
dyskinesia
involuntary, uncontrolled, and erratic muscle movements. These abnormal movements can affect a single part of the body, such as the head or a limb, or the entire body
chorea
a hyperkinetic movement disorder characterized by involuntary, unpredictable, and often restless movements that can affect the face, trunk, and limbs
athetosis
a movement disorder characterized by slow, writhing, involuntary movements of the limbs, face, neck, and trunk, often linked to damage to the brain's basal ganglia
tone
Gamma motor neurons indirect activation pathways are
crucial
• GMN keeps muscle spindles taut and adjusts
sensitivity to allow alpha neurons to fire
• Volitional movement is superimposed upon this
framework
• May be excessive or reduced
• Will affect all valves and all aspects of production
• Tone may be excessive or reduced, fluctuate in regular
fashion, wax or wane unpredictably, slowly or quickly
types of abnormal tone:
flaccid tone, spastic tone, hypokinetic tone, hyperkinetic tone
flaccid tone
tone is consistently reduced
spastic or hypokinetic tone
consistently increased
hyperkinetic tone
variable
modified tongue anchor test
having the pt puff cheeks and
protrude tongue simultaneously. Push on cheeks.
If their velopharyngeal functioning is within
normal limits, their cheeks will remain puffed up.
• Not valid if there is significant tongue or facial
weakness
• Rationale is that patients cannot use back of
tongue to aid in velopharyngeal closure
• Compensatory strategy
• Velopharyngeal closure can only be examined
through videofluoroscopy or nasoendoscopy
larynx adduction can be tested using two tasks:
cough- assesses cough sharpness, not loudness
weak/breathy cough can reflect adductor weakness/poor respiratory support
coup de glotte/glottal coup- sharp glottal stop or a grunt
does not require respiratory force or sustained airflow- assess sharpness
weak cough with strong glottal coup indicates:
respiratory weaknessw
weak coup/normal cough or equally weak coup/cough indicates:
laryngeal weakness or combined laryngeal respiratory weakness
vocal cord abduction

vocal cord adduction
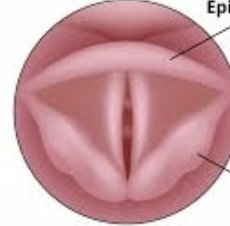
vocal cord abduction can be assessed through:
presence of inspiratory stridor (typically a sign of an obstructed or narowed upper airway)
laryngeal exams should be conducted when:
structural or LMN lesions are suspected
structural impairments to the vocal cords
polyps or nodules can alter mechanical properties of cords
weakness/paralysis can alter cord mobility
to assess inspiratory stridor
have the patient take a few quick breaths
normal reflex
occurs as a reflection of normal nervous system function
absence of normal reflex reflects PNS
release phenomena
reduction in cortical inhibitory influence on lower centers of brain and can reappear with age
gag/pharyngeal reflux
elicited by bottom of uvula, stroking back of tongue,
posterior pharyngeal wall or faucial pillars on both
sides
• Sensory = glossopharyngeal nerve (IX)
• Motor = vagus (X)
• Response is elevation of palate, retraction of tongue,
sphincteric contraction of pharyngeal walls
• Gag reflex is only significant if asymmetry is noted
• Ask if it feels different on the two sides- a lack of
sensation could be responsible for decreased gag
reflex
jaw jerk reflex
maxillary reflex
primitive deep muscle stretch reflex that may be pathologic in adults
patient should be relaxed with lips parted and jaw halfway open
tongue depressor is placed on chin and is tapped with other hand or a reflex hammer
response is pathologic if jaw closes quickly
present in approximately 10% of normal adults
may be a confirmatory sign of bilateral UMN lesions at a level above mid-pons (affecting motor/sensory branches of the trigeminal nerve)
sucking
primitive reflex
• Elicited by stroking lip from lateral aspect towards
philtrum on both sides
• Pathologic response is pursing of lips
• Can be a confirmatory sign of UMN damage,
especially to premotor cortex
• Frequently elicited in demented patients
• Rooting reflex occurs as an exaggerated reflex when an object approaches the mourh
snoit reflex
similar to sucking reflex
elicited by a light tqp of finger on philtrum or tip of nose or backwards pressure on midline of upper lip and philtrum
pathological snout reflex
puckering or protrusion, along with evaluation of lower lip and depression of the lateral angles of the mouth
cognitive-communicative ability can be measured with the following questions:
can pt follow simple directions?
oral motor and dysphagia exercises
can pt remember and restate a technique?
determine if pt can participate in treatment
can pt follow and remember directions independently for functional swallow?
what would a trial feeding look like?
present small amounts of variety of textures for both
liquids and solids
• Begin with ice chips, small sips of water, puree,
mechanical soft and regular consistencies
• Observe for any problems with specific consistency or
for oral phase issues
• If patient exhibits difficulty, attempt compensatory
technique
oral placement purpose
determine which placement facilitates the safest swallow
anterior oral placement
prone to aspirate but good bolus controlp
posterior oral placement
mastication/AP transit problem; no pharyngeal issues
left oral placement
R weakness
right oral placement
L weakness
midline oral placement
reduced sensitivity
3 oz water swallow test
A 3-ounce (approximately 90 milliliters) volume
of water is measured and poured into a cup.
• Patient is instructed to take small sips of the
water and swallow it in a controlled and
CONSECUTIVE manner.
• SLP observes the patient’s swallowing, looking
for signs of difficulty or abnormalities (coughing,
choking, throat clearing)
timed test of swallowing
1. A specific volume of liquid (typically water) is measured,
and patient is instructed to take a sip of the liquid and
swallow it as quickly and safely as possible.
2. The goal is to complete the swallow without coughing,
choking, or experiencing any other signs of aspiration
3. SLP uses a stopwatch or timer to measure the time it
takes for the individual to initiate and complete the
swallow, from the moment the liquid enters their mouth
to the moment they signal that the swallow is complete.
4. The test may be repeated several times with different
volumes of liquid to assess the individual's swallowing
abilities across different conditions.
cervical auscultation
a clinical procedure that involves listening to the sounds produced by swallowing in the neck region
pulse oximetry
monitors oxygen saturation levels
(the percentage of hemoglobin in the blood that is
carrying oxygen, compared to the total amount of
hemoglobin available).
reflex cough test
A small amount of a substance
known to induce coughing is applied to the back of
the patient's throat (often citric acid, tartaric acid,
distilled water, or a similar irritant). Individual's
response to the test substance is observed (i.e.,
coughing, throat clearing, or other signs of
discomfort).
non surgical enteral procedures
Oral nutrition – p.o. intake via diet
modification
• Enteral tube feeding – through tube or
catheter that delivers nutrients
bypassing oral intake
• NG tube (nasogastric tube) through
nose and inserted down esophagus
into stomach – usually for less than
30 days
• NJ tube (nasojejune) intestinal tract
– less than 30 days
surgical procedures
Gastrostomy – PEG (percutaneous endoscopic
gastrostomy)
• Tube inserted directly through a surgically
produced stoma in stomach
• Used for greater than 30 days duration
• Jejunostomy – PEJ (percutaneous endoscopic
jejunostomy)
• Tube inserted directly into intestines through
an incision
• Used for greater than 30 days duration
• Often used if PEG tube fails or becomes
infected
parenteral feeding
Provision of some or all
nutrients by means other than
gastrointestinal tract (usually
IV)
• Peripheral – delivered thorough a
peripheral vein (hand or forearm)
through IV
• Central – delivered through a
large diameter vein (superior
vena cava via the jugular vein)
• “Central line”