Circulatory system
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
.
.
Why do multicellular organisms eg: rabbit need a transport system, whereas unicellular organisms eg: bacterial cell does not
Multicellular organisms have a small surface area to volume ratio so have a high metabolic rate so diffusion rate is slow
what is the Formula for SA to Volume ratio
SA/Vol Vol is always = 1
mammals have what kind of circulatory system and what does that mean?
closed and double its a closed system because blood is carried in the vessels its a double circulatory system because blood passes through the heart twice
Benefits of double circulatory system
blood only passes through one capillary before returning to the heart
Increases speed of circulation
Oxygenated and deoxygenated blood are kept separate for efficiency
Increased pressure maintains a steeper concentration gradient which allows efficient exchange
What is a the difference between a closed and open system in circulatory system
Closed system is when blood stays within vessels Open system is when blood is not enclosed in the blood vessels
Open system has haemolymph as transport medium while in closed system its blood
An open system is good enough for insects because of small diffusion distances, closed system is more efficient to deliver gases and nutrients over a large distance
what circulatory system do fish have What does this mean
Single closed circulatory system Blood passes through heart once and is in blood vessels but has to be low pressure as it will damage gills and capillaries
Disadvantage of fish having a single circulatory system
Blood does not flow quickly to the rest of the body so limits rate of o2 delivered.
in the circulatory system insects dont have blood so what is the fluid in insects
haemolymph
What is diffusion?
The movement of atoms or molecules from an area of high concentration to an area of low concentration.
what circulatory system does an insect have
open (blood is not in vessels)
What pressure is blood at for insects and why
Low pressure so it flows slow It is at low pressure because they do simple movements and have a small simple heart
What are the 5 type of blood vessels And where do they carry blood
arteries away
Arterioles away
Veins towards
Venules towards
Capillaries
Arteries and veins have 3 layers name and describe them
Tunica externa (outermost layer made of collagen)
Tunica media (a layer of smooth muscle and elastic tissue)
Tunica intima (a layer of squamous eputhelial cells called endothelium )
What is the middle part of the blood vessel called
lumen (consists of blood)
What are the features of an artery
•Elastic fibres that stretch and recoil to maintain blood pressure •Thick tough outer collagen coat to withstand high pressure of blood •Thick layer of smooth muscle can contract and relax to alter diameter of lumen (this can alter blood flow)
Features of capillaries
•Made up of single squamous epithelial cells (one cell thick)
Carry low pressure blood
Thin walls to facilitate exchange of materials
Features of veins
•Large lumen to reduce friction and increase blood flow Thin tunica media as blood is at low pressure Thinner outer collagen layer (tunica externa) Has valves which prevent the backflow of blood
What layer is the endothelium found in What is its structure? What is its properties? What is its function?
•Tunica intima •Single layer of thin squamous cells •smooth (minimises friction)
What layer is the smooth muscle found in? What is its structure? What are its properties? What is its function?
•Tunica media •overlapping muscle cells •contracts or relaxes •adjusts blood flow through vasoconstriction and vasodilation
What layer is elastic fibres found in? What is its structure? What are its properties? What is its function?
•Tunica media •Made of elastic proteins •can stretch (coping with high blood pressure)
What layer are collagen fibres found in What is its structure? What are it's properties? What are its function?
Tunica externa •? •withstands high pressure
Tissue fluid is determined by what types of pressure
Oncotic pressure and hydrostatic pressure
What is oncotic pressure?
tendency of water to move into blood by osmosis Eg:
What is hydrostatic pressure
The pressure created by a fluid in an enclosed space
Where is tissue fluid formed
capillary beds
What is the composition of blood that is plasma
Composition of blood that is RBC, WBC, platelets etc
55%
45%
What things are inside the plasma
Water Solvent
Ions (blood
electrolytes)
Sodium, Potassium
Calcium, Magnesium
Plasma protein
Plasma functions
Contains electrolytes
Help maintain osmotic balance
Function in lipid transport, immunity and blood clotting
How does plasma leave capillary
Through tiny gaps (fenestrations) in capillary endothelial cells
As plasma proteins and blood cells are too large to be forced out of endothelium what happens
The plasma proteins remaining in the blood act as solutes and reduce water potential so create an osmotic pressure called oncotic pressure to cause the return of water (and solutes at venous end of capillary
How does the pressure at the arterial end of capillary affect movement of substances
Higher hydrostatic pressure than oncotic pressure so fluid is forced out capillary out of fenestrations (small gaps in capillary)
Proteins remain in the blood
increased proteins create a water potential gradient
Hydrostatic pressure is higher than oncotic pressure so so water moves out of capillaries into tissue fluid
where does the 10% of the fluid go
Lymphatic system
However the lymph eventually reenters the bloodstream along with any plasma proteins
Role of lymph and lymphatic system
Defending against infection
What are the problems with excess lymph
Can cause disorders eg: Kwashiorkor - malnutrition (severe protein deficiency in diet) •symptoms can be swollen stomach •lower concentrations of plasma proteins means lower oncotic pressure •Lower oncotic pressure means less tissue fluid reabsorbed into blood •more goes into lymphatic system causing swelling
What do the coronary arteries do?
Deliver oxygen and nutrients to the heart tissue
The muscle in the heart is the cardiac muscle and can contract on its own meaning it is what
Myogenic
Why does the heart create an increased blood pressure
The heart has to pump a large volume and blood around the body and this blood moves through narrow arteries causing blood pressure to be high.
Why do atria have thinner walls than ventricles
The atria don't have to pump blood very far
Why does the left ventricle have a thicker wall than the right ventricle
•The left ventricle pumps blood to all body tissues •This is a greater distance than the right ventricle •So it encounters more resistance •So it needs greater pressure to complete the circuit and return to the heart
Describe the direction of blood flow
Superior vena cava (blood starts deoxygenated) Right atrium Atrioventricular (tricuspid) valve Right ventricle Semi-lunar valve Pulmonary artery Capillaries in lungs (to become oxygenated) Pulmonary vein Left atrium Atrioventricular (bicuspid) valve Left ventricle Semi - lunar valve Aorta Body tissue Back to vena cavs
What is the cardiac cycle
Sequence of events in one heartbeat that pump blood around the body
What is systole? What is diastole?
When heart muscle is contracted When the heart muscle is relaxed
What happens in diastole
Ventricles and atria relax and atria fills with blood
this increases pressure so pressure is now higher in atria than ventricles
Blood starts to move from atria to ventricles by pushing open atrioventricular valve
What happens in atrial systole
Atria contract causing decrease in volume and an increase in pressure, pressure in atria rises above that in ventricles forcing AV valves open, blood is forced into the ventricles
What happens in ventricular systole
Ventricles contract Ventricle volume decreases as blood fills then, this causes an increase in pressure,
Atrioventricular valves are forced shut
Semi lunar valves are forced open as blood enters arteries this continues until pressure in arteries is less than ventricles
Blood falls back causing semi lunar valves to shut
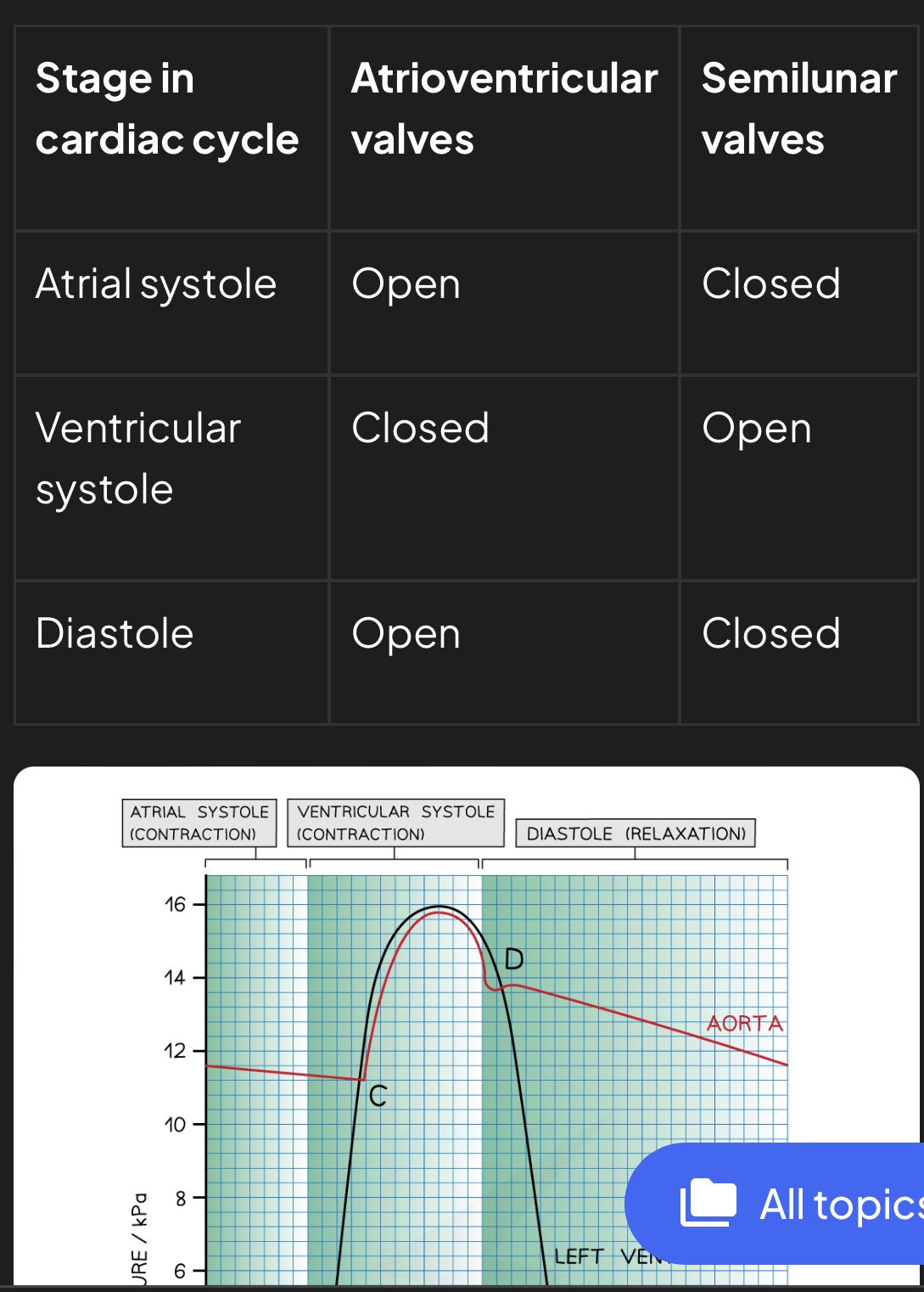
Which valves are open and closed during the stages of the cardiac cycle

What happens at point:
A
Between A and B
B
C
D
Between D and E
E
After E
Point A =End of diastole so atrium is filled with blood and pressure is higher than ventricles so AV valve opens
In between point A and B = Atrial systole - left atrium contracts increasing pressure and forcing blood into the left ventricle, pressure is higher in atrium than ventricle so AV is open
Point B = beginning of ventricular systole - left ventricle contracts causing pressure to increase, pressure in ventricle exceeds atrium pressure so AV valve shuts
Point C = end of ventricular systole - pressure exceeds that in aorta and aortic valve opens
Point D beginning of diastole - left ventricle has emptied all the blood and aortic valve closes
Point D to E = early diastole - ventricles are relaxed and blood veins to flow into relaxed atrium
Point E = diastole - left atrium fills with blood and AV valve opens
After E - ventricle expands and there is a decrease in ventricular pressure
What are the cells in the right atrium known as
Pacemaker cells
What do the sympathetic + parasympathetic division do to the pacemaker cell
Sympathetic division speeds up the pacemaker
Parasympathetic division slows down the pacemaker
What are pacemakers also known as
Sinoatrial node (SAN)
What does SAN do?
Initiates excitation (nerve impulse) without stimulation from nervous system meaning it's myogenic
Describe how heart contraction is initiated
•SAN initiates a wave of excitation that spreads over both atria causing them to contract simultaneously. This causes blood pressure to be higher in atria than in ventricles so blood is forced from atria to ventricles through AV valve
•Electrical excitation is sent to AVN where there is a short delay to allow atria to empty blood and force it to ventricles
•Wave of excitation spreads down bundle of his down to purkyne fibres and causes ventricles to contract from the apex upwards and forced blood through semi lunar valves to arteries
What would happen if there was no delay in excitation
Not enough time for blood to enter ventricles and pumping of blood around the heart would be less efficient
What is cardiac output
the total volume of blood pumped out the heart every minute
How do you calculate cardiac output?
stroke volume x heart rate Stroke volume = The amount of blood ejected from each ventricle per contraction/beat Heart rate = number of beats/contractions per minute
Convert into dm cubed
The units for cardiac output
ml min-1 or l min-1
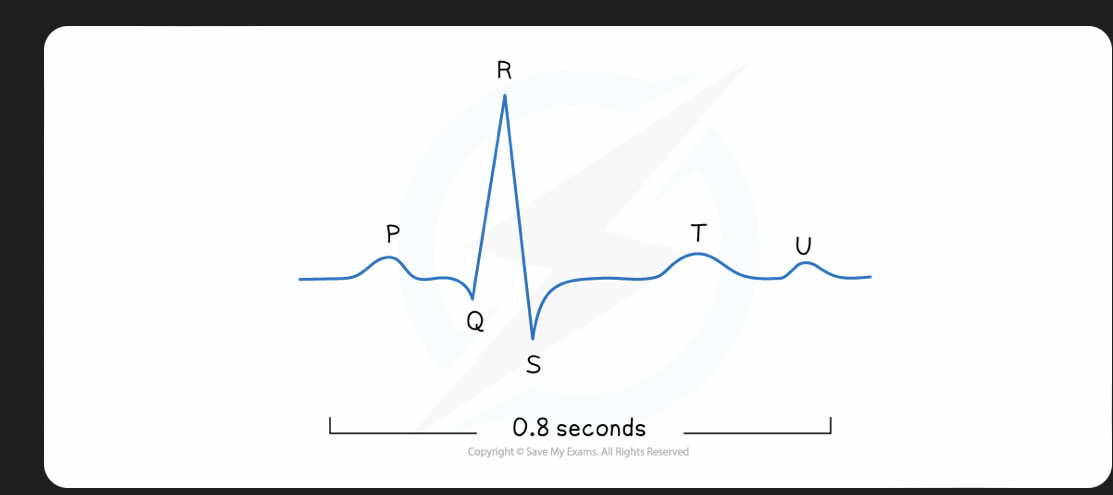
What is ECG?
electrocardiogram -shows electrical activity in the heart
In an ECG: What is the P wave What is the QRS wave What is the T wave, what is the U wave
P = Atrial systole QRS = ventricular systole T = diastole U= repolarisation
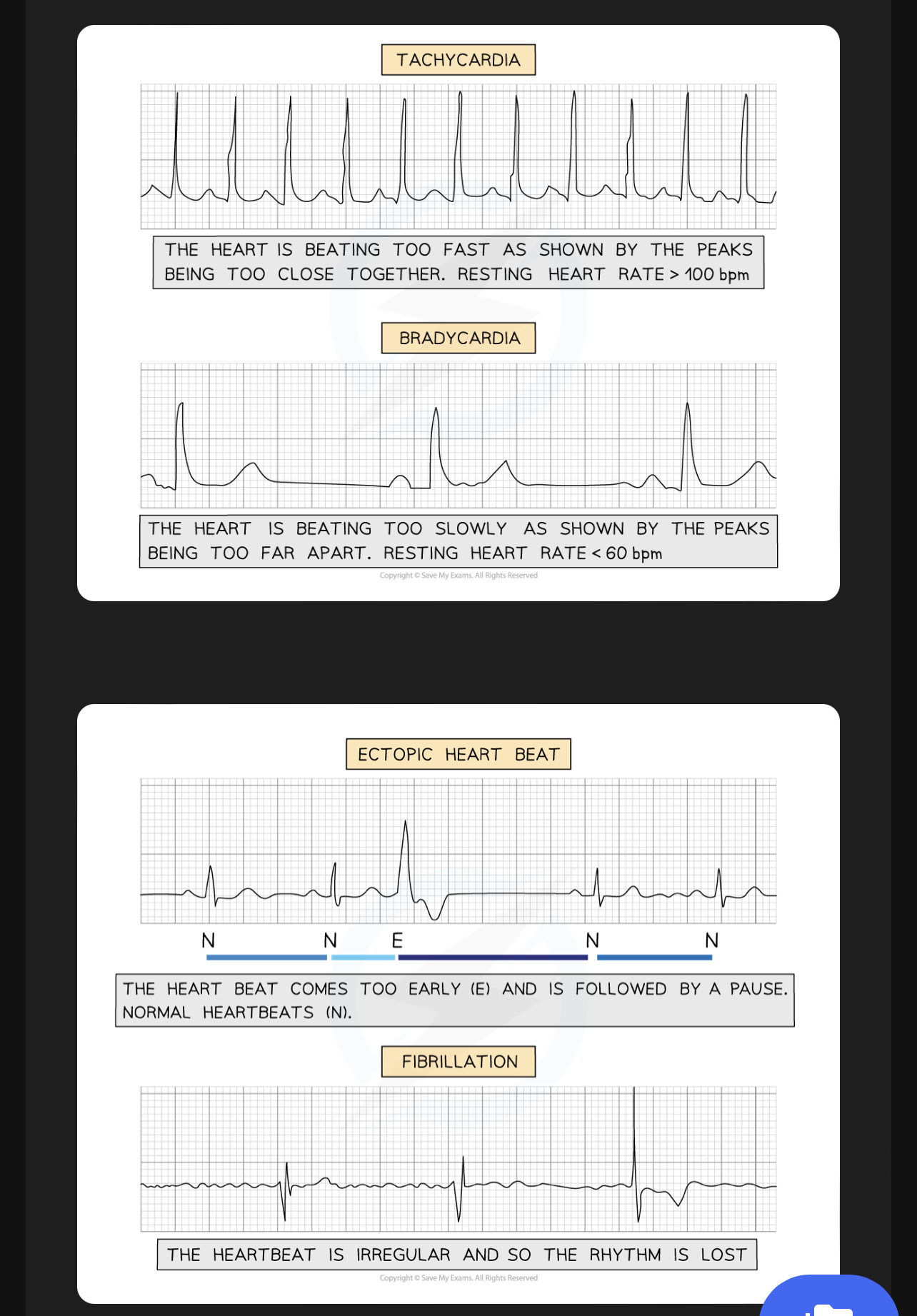
What is the name of a fast heart rate What is the name of a slow heart rate what is the name of a heartbeat followed by a pause What is the name of an irregular heartbeat
Tachycardia, Bradycardia, ectopic heartbeat, Fibrillation (atrial or ventricular fibrillation)
Structure of haemoglobin
• globular protein (soluble & specific 3d shape) • quaternary structure made of 4 polypeptide chains (2α
What hormone releases red blood cells when o2 delivery is low
The hormone erythropoietin (EPO) stimulates erythrocyte production
when O2 delivery is low
How does the first oxygen molecule affect how easily the other 3 oxygen molecules bind to Haemaglobin
The first oxygen molecule combines relatively slow with first haem group. Binding causes structure of Haemaglobin molecule to change. This change in structure makes it easier for second third and fourth oxygen molecule to bind to their haem group. Cooperative binding increases affinity (attraction) of Haemaglobin for oxygen
Explain gas exchange at the lungs
Haemoglobin picks up oxygen because of the increased oxygen pressure in the
capillaries of the lungs
explain gas exchange at tissues
Release oxygen to body cells as the oxygen pressure in the tissues is lower.
The relationship of partial pressure and oxygen saturation of haemoglobin is illustrated by what
Oxygen dissociation curve
Out of oxygen carbon monoxide and carbon dioxide which ones bind together
oxygen and carbon monoxide bind to the same site and co2 binds to a different site
How is carbon dioxide carried in the blood?
5% dissolved in plasma 10% combined with haemoglobin to form carbaminohaemoglobin 85% transported into the form hydrogen carbonate ions (HCO3-)
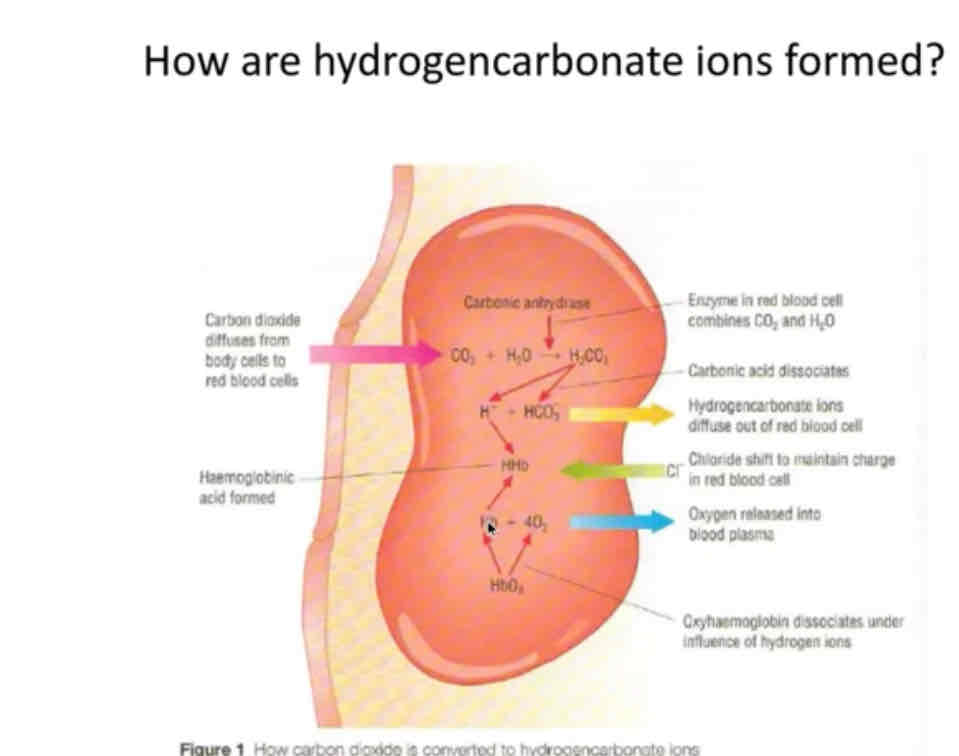
How do hydrogencarbonate ions form
•Carbon dioxide diffuses from cells into body •Fuses with water and uses enzyme carbonic anyhydrase to form carbonic acid •carbonic acid dissociate into H+ ion and HCO3- ion (That is how 85% is transported around body) •HCO3 diffuses out of cell and chloride ions shift in to balance negative charge
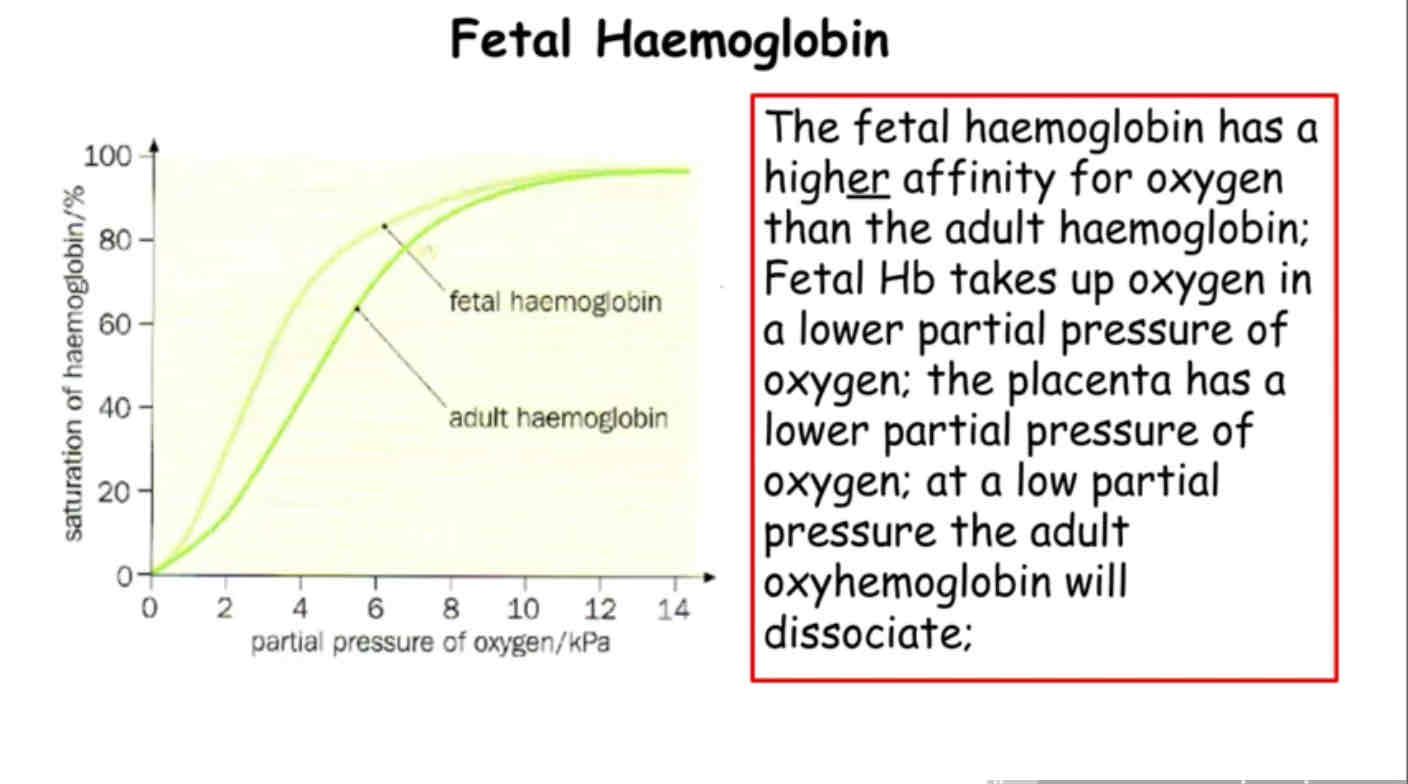
What has a higher affinity fetal haemoglobin or adult haemoglobin
Fetal haemoglobin -shifts to the left and has a higher affinity than adult haemoglobin allowing oxygen to move from maternal blood (higher level of oxygen) to foetus blood (low level of oxygen) at the placenta.
Does myoglobin have a higher affinity or lower affinity than foetal haemoglobin
Higher
What happens to oxygen dissociation curve when we increase co2 (Bohr effect)
Shifts to the right because shape of Haemaglobin is changed , Haemaglobins affinity for oxygen is reduced. There is more dissociation of oxyhaemaglobin so more o2 available for respiration.
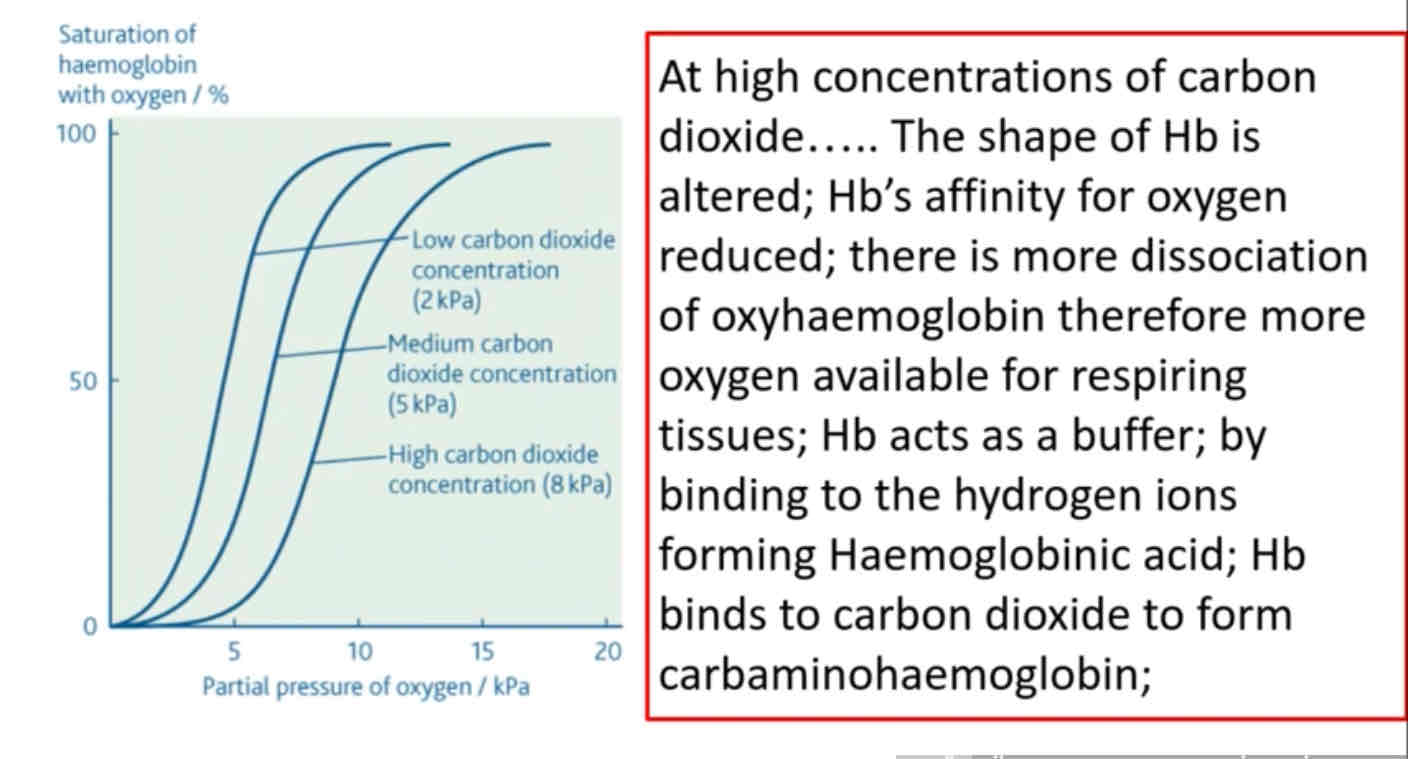
What happens to oxygen dissociation curve when we Decrease co2
Shifts to the left