BPH 206 Final USE THIS
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
How can you motivate someone to make a behavior change?
Use Motivational Interviewing (MI)
What drives behavior change?
Behavior change is driven by the client's own motivations and reasons for change. MI helps clients discover their capacity for change by developing discrepancy and encouraging them to articulate their own reasons for change.
What is the importance of the change scale?
Scaling assesses readiness to change by asking clients to rate the importance and confidence of making a change on a scale (e.g., 1 to 10). This helps identify where to start and what work needs to be done.
When is it appropriate to use Motivational Interviewing?
MI is appropriate when clients are ambivalent about change or resistant to making a change. It is effective in various contexts, including substance abuse, diabetes management, clinical pain management, and smoking cessation.
Motivational Interviewing
an evidence-based approach to behavior change
How to motivate someone to make a behavior change, what's the best way to increase motivation?
• Partnership
• Acceptance
• Evocation
• Compassion
Partnership
Collaboration → joint decision-making
Client → Expert on their life
Practitioner →• Expert in behavior change, Honors client's wisdom
Acceptance
Nonjudgmental stance
• Avoid arguing
• Roll with Resistance
• Work with ambivalence
Express empathy
Curious/Seeking to understand
Respect for autonomy
Compassion
Promote client's well-being selflessly
Support client's self-efficacy
Evocation
Client → Possesses the capacity needed for change
Practitioner → (Below)
• Develops discrepancy (cognitive dissonance) to encourage change
• Helps client discover their capacity &reasons (motivation) for change
Motivational interviewing has four fundamental processes that describe the flow of conversation
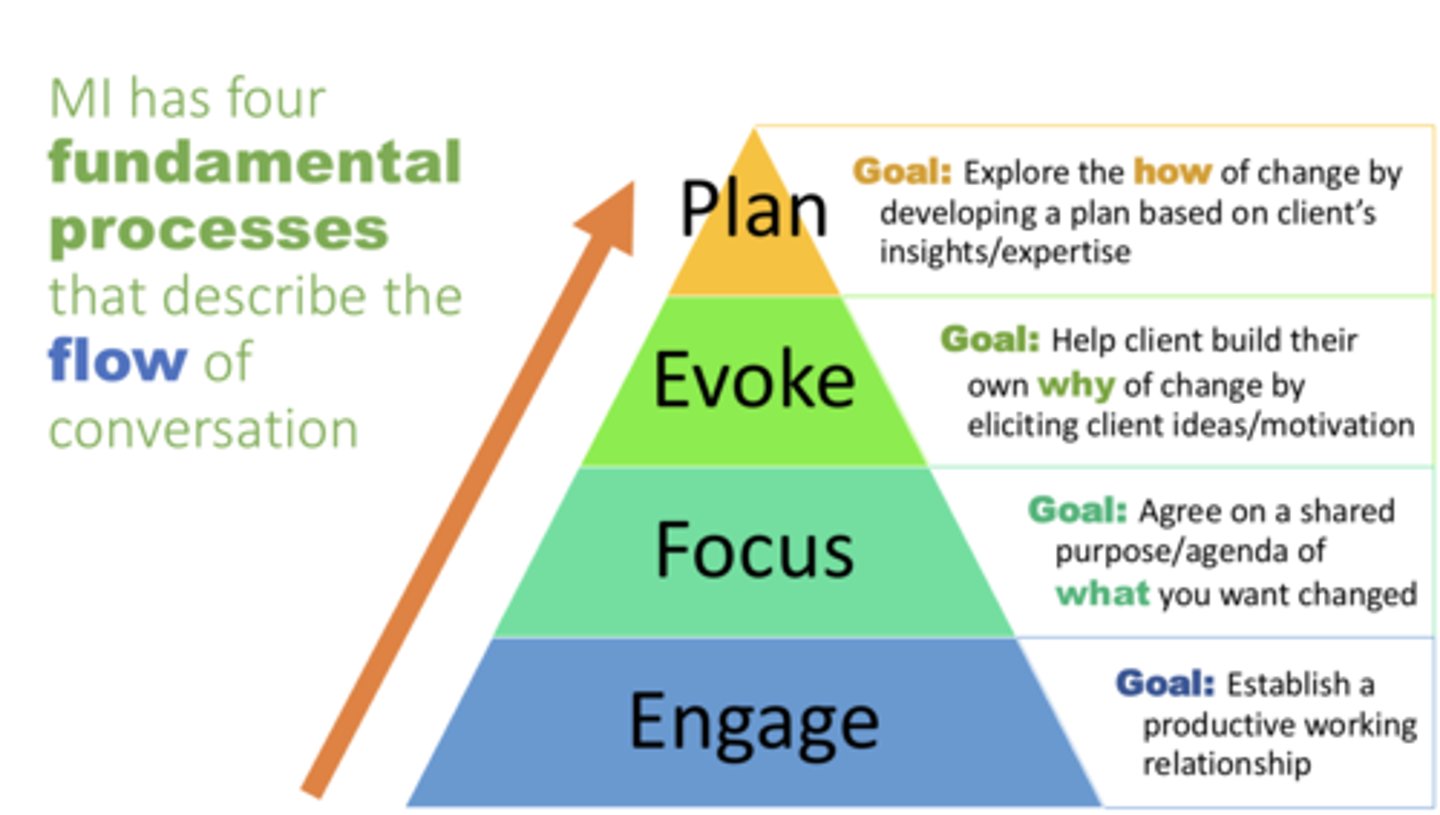
Engage
Goal: Establish a productive working relationship
Focus
Goal: Agree on a shared purpose/agenda of what you want changed
Evoke
Goal: Help client build their own why of change by eliciting client ideas/motivation
Plan
Goal: Explore the how of change by developing a plan based on client's insights/expertise
The four motivational interaction techniques
Open-ended Questions, Affirmation, Reflection, and Summary
Open-ended Questions
Draw out/Explore client's experiences, perspectives, & ideas
Guide the client to reflect on how change may be meaningful or possible
EX; What do you know about...?; What are your thoughts about...?
Affirmation
Reinforce strengths, efforts, past successes
→Gives hope and builds self-efficacy
Be enthusiastic!
Reflection
Repeat, rephrase, or suggest what the client is trying to communicate
→Builds rapport/trust Demonstrates empathy
Summary
Reinforce key points made by the client in an intentional way
→• Acknowledge reasons against change sustain talk•
Emphasize reasons in favor of change change talk
Encourage movement from sustain talk to change talk when appropriate
Public Health Accreditation Board
developed a voluntary accreditation process.
Approximately two-thirds of theU.S. population is served by a PHAB-accredited health department.
Presence of an academic health department can provide evidence for fulfilling a number of PHAB criteria.
improve the quality, accountability, and performance of public health departments
OSHA (Occupational Safety and Health Administration) What are the primary roles of key federal agencies that influence health but are not part of HHS (OSHA, USDA, DHS, EPA)?
Ensures workplace safety by setting standards and preventing work-related injuries and illnesses.
USDA (Department of Agriculture) What are the primary roles of key federal agencies that influence health but are not part of HHS (OSHA, USDA, DHS, EPA)?
Ensures food safety, promotes nutrition, and manages food assistance programs (e.g., SNAP).
DHS (Department of Homeland Security) What are the primary roles of key federal agencies that influence health but are not part of HHS (OSHA, USDA, DHS, EPA)?
Protects from threats (terrorism, disasters) and manages health response during emergencies (e.g., pandemics).
EPA (Environmental Protection Agency) What are the primary roles of key federal agencies that influence health but are not part of HHS (OSHA, USDA, DHS, EPA)?
Protects human health by regulating pollution, toxic chemicals, and environmental hazards.
NIH (National Institutes of Health) Know the primary roles of key public health agencies
Lead research agency; also funds training programs and communication of health information to the professional community and the public.
FDA (Food and Drug Administration) Know the primary roles of key public health agencies
Consumer protection agency with authority for safety of foods and safety of efficacy of drugs, vaccines, and other medical and public interventions.
HRSA (Health Resources and Services Administration) Know the primary roles of key public health agencies
Seeks to ensure equitable access to comprehensive quality health care.
IHS (Indian Health Service) Know the primary roles of key public health agencies
Provides direct health care and public health services to federally recognized tribes (Indians)
AHRQ (Agency for Healthcare Research and Quality) Know the primary roles of key public health agencies
Research agenda to improve the outcomes and quality of health care, including patient safety and access to services
CDC (Center for Disease Control) Know the primary roles of key public health agencies
Lead agency for prevention, health data, epidemic investigation, and public health measures aimed at disease control and prevention.
SAMHSA (Substance Abuse and Mental Health Services Administration) Know the primary roles of key public health agencies
Works to improve quality and availability of prevention, treatment, and rehabilitation for substance abuse and mental illness.
How Can Public Health Agencies Work Together to Respond to an Outbreak of Disease?
Steps in investigating a food borne outbreak:
1. Detect a possible outbreak.
2. Define and find cases.
3. Generate hypotheses about likely sources.
4. Test the hypothesis.
5. Find the point of contamination and the source of the outbreak.
6. Control the outbreak.
7. Decide that an outbreak is over.
Home rule or local autonomy model
authority is delegated from the state to the local health department
Branch office model
the local health department can be viewed as a branch office of the state agency with little or no independent authority or funding
What are the 3 core functions of public health?
assessment, policy development, assurance
Assessment
Obtaining data that defines the health of the population overall as well as specific groups within the population
Policy development
Developing evidence-based recommendations and other analyses of options to guide implementation
Assurance
Oversight responsibility for ensuring key components of an effective health system
CARE & Oxfam International
Provide services and advocate for global health-related crises
What are the functions of public health agencies at the federal, state, and local levels, and what agencies operate at each level?
Federal Level:
Function: Develop national health policy, fund programs, conduct research, respond to national/global health threats.
Agencies: CDC, FDA, NIH, CMS, EPA, OSHA, USDA, DHS.
State Level:
Function: Coordinate public health activities within the state, enforce state health laws, manage statewide disease surveillance, and oversee local health departments.
Agencies: State health departments, State EPA divisions, State emergency management agencies.
Local Level:
Function: Deliver public health services directly to the community (e.g. immunizations, health education, restaurant inspections, outbreak response).
Agencies: Local/county health departments, city public health offices.
What Are the 10 Essential Public Health Services?
Core function: Assessment◦
1 - Assess and monitor population health.
2 - Investigate, diagnose, and address health hazards and root causes.
Core function: Policy development
3 - Communicate effectively to inform and educate.
4 - Strengthen, support, and mobilize communities and partnerships.
5 - Create, champion, and implement policies, plans, and laws.
6 - Utilize legal and regulatory actions.
Core function: Assurance
7 - Enable equitable access.
8 - Build a diverse and skilled workforce.
9 - Improve and innovate through evaluation, research, and quality improvement.
10 - Build and maintain a strong organizational infrastructure for public health.
What is the impact of public health funding cuts and what are their implications for public health response?
Reduced workforce: Fewer staff to conduct inspections, outreach, education, and disease investigations.
Delayed or weakened emergency response: Slower reaction to outbreaks, natural disasters, and other public health crises.
Cuts to prevention programs: Less funding for services like vaccination clinics, health screenings, and chronic disease prevention.
Increased health disparities: Vulnerable populations lose access to essential services.
Higher long-term costs: Preventable diseases and health issues become more expensive to treat later.
Lower community resilience: Communities become less prepared for health emergencies and long-term public health challenges.
Parachute Science
A type of research where scientists, often from well-resourced countries, conduct field work in a foreign country, typically a developing nation, without meaningfully engaging or acknowledging the contributions of local researchers or institutions.
What is the CDC’s Do Not Board (DNB) List and why is it used?
A list maintained by the CDC of individuals with contagious diseases who are prohibited from boarding commercial flights to prevent disease spread. Used to prevent outbreaks.
What is the Fulbright program?
A prestigious international exchange program funded by the U.S. government that supports students, scholars, artists, and teachers to study, teach, or conduct research in countries other than their own
Reductionist thinking
looks at one factor or variable at a time
Systems thinking
looks at the impacts of multiple factors and how they work together as parts of a system. Often utilizes data derived from reductionist thinking but goes beyond to look at multiple factors that cause disease and disease outcomes
What are patterns of epidemiologic transitions and their meanings?
Epidemiologic transitions refer to the changes in disease patterns and causes of death over time, often associated with demographic transitions. These patterns help understand shifts from infectious diseases to chronic diseases as societies develop.
(Step 1) What are the steps in a systems analysis?
Identify influences - Identify risk factors or determinants that are thought to affect or influence the possibility of occurrence of a disease or the outcome of a disease.
(Step 2) What are the steps in a systems analysis?
Estimate the relative strength of the influences - Estimate the magnitude or strength of each factor or influence taking into account its relative risk and prevalence or at least the relative strength, such as weak, moderate, or strong.
(Step 3) What are the steps in a systems analysis?
Examine the interactions between factors - How is the occurrence of disease or the outcome of disease affected when two or more influences are present?
(Step 4) What are the steps in a systems analysis?
Identify feedback loops - Identify ways that an influence increases or decreases the impact of other factor(s) over time.
(Step 5) What are the steps in a systems analysis?
Identify bottlenecks - Identify points in the system or constraints that need to be addressed in order for the other factors or influences to have their potential impacts.
(Step 6) What are the steps in a systems analysis?
Identify leverage points - Identify points in the system that present opportunities for interventions to have greater than otherwise expected impacts.
Syndromes
• Some diseases predispose to other diseases.
• Patterns of risk factors/symptoms that tend to occur together.
(a group of symptoms which consistently occur together, or a condition characterized by a set of associated symptoms.)
Syndemic
• The occurrence together of two or more diseases that interact to magnify the occurrence and/or overall burden of disease.
• Not always detrimental, as one disease may provide protection against other diseases.
(Part A) Understand systems diagrams and meaning behind symbols
Positive feedback loop: One factor affects another factor by accentuating or increasing its impact.
• Product of the signs is positive.
Negative feedback loop: One factor affects another factor by dampening or decreasing its impact.
• Product of the signs is negative.
(Part B) How can systems thinking help identify bottlenecks and leverage points to improve population health?"
Bottleneck: A point at which events are slowed, presenting obstacles to the success of an intervention.
• Example: Delays in reaching care after a motor vehicle injury.
Leverage point: A point in the system in which successful interventions produce better-than-expected outcomes.
• Example: Smoking cessation programs for pregnant women.
One Health
The collaborative effort of multiple health science professions, together with their related disciplines and institutions - working locally, nationally, and globally - to attain optimal health for people, domestic animals, wildlife, plants, and our environment
Culture Tailoring
Is the process of modifying public health programs, messages, or interventions to align with the cultural values, beliefs, practices, language, and context of a specific population
What are the benefits of cultural tailoring?
- Builds trust and engagement
- Improves health outcomes and participation
- Addresses health inequalities and barriers
- Honors community voices and lived experiences
Familias Unidas
An evidence-based, culturally informed family intervention aimed at preventing/reducing drug use, sexual risk behaviors, and behavior problems among Hispanic youth
Familias con Orgullo
An intervention targeting Hispanic sexual minority youth, focusing on parental support, emotion regulation, and fostering social support and resilience.
eHealth Familias Unidas for Mental Health
Integrated components targeting internalizing symptoms and suicide risk, including new video sessions and interactive exercises.
ADAPT-ITT model
How to culturally adapt a program
- Highly community-engaged approach
- Uses a variety of data sources in order to inform the adaptation
- Multiple points of adaptation (at least 3 drafts are produced)
- Systematic - documentation of adaptation process
Step 1: Assessment
Who is the new target population?
Step 2: Decision
What evidence-based intervention/program will be selected for adaptation?
Step 3: Administration/Adaptation
What in the original program needs to be adapted? How should it be adapted?
Step 4: Production
How do you produce an initial draft and document adaptations that you made to the prior program?
Step 5: Topical Experts
Who can help to adapt the EBI (evidence based intervention)?
Step 6: Integration
What is going to be included in the adapted program that will be pilot tested?
Step 7: Training
Who needs to be trained?
Step 8: Testing
Was the adaptation successful? Did it enhance short-term outcomes?