Week 4: M/S
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
41 Terms
3 different settings of operative nursing
pre-op: same day surgical admission (elective) or emergency
intra-operative: operating room or abulatory
post-op: post anesthesia recovery unit → ambulatory or admission to hospital
nurses work in all settings
elective surgery
pt has waited at home, waited on list for surgery, check in for surgery, has known for a long time
pre-operative
important to understand how did pts have surgery
can tell you how prepared they are
how their mental health/anxiety are
abulatory surgery
surgery that occurs in a dr office, dentist office
walk in walk out
eg. wisdom teeth, skin biopsy
surgical indications
diagnosis: exploration to complete a biopsy → understand and diagnose
cure and repair
palliation: can complete surgery to prolong quality of life
prevention: if someone has higher chance of getting cancer, etc
exploration: to see what is going on
cosmetic improvement
pre-operative assessments
consults or diagnostic testing
assess medical regime, emotional status + physical assessments if indicated
review past medical diagnoses and surgical procedures → have they (or fam) reacted to anasethesia before
review prescribed medications → anticoagulation meds especially
pre-operative education
protocol for routine medications before surgery
which medications to stop before surgery
NPO instructions
pain menagment options
infection prevention and wound care
post-op discharge and care
pre-op day of surgery assessment
pre-op checklist; pacemaker?, prosthetic?, contacts, vitals, personal belongings, ECG results, bloodwork results
confirms consultuations are completed
identifies any changes in physical assessment
establish baseline data
review pre-op diagnostic tests
review medications
consider cultural considerations
consent ability → consent completed
pre-operative considerations
allergies
systems assessments
fluid and electrolyte status
nutritional status
labs and diagnostic tests
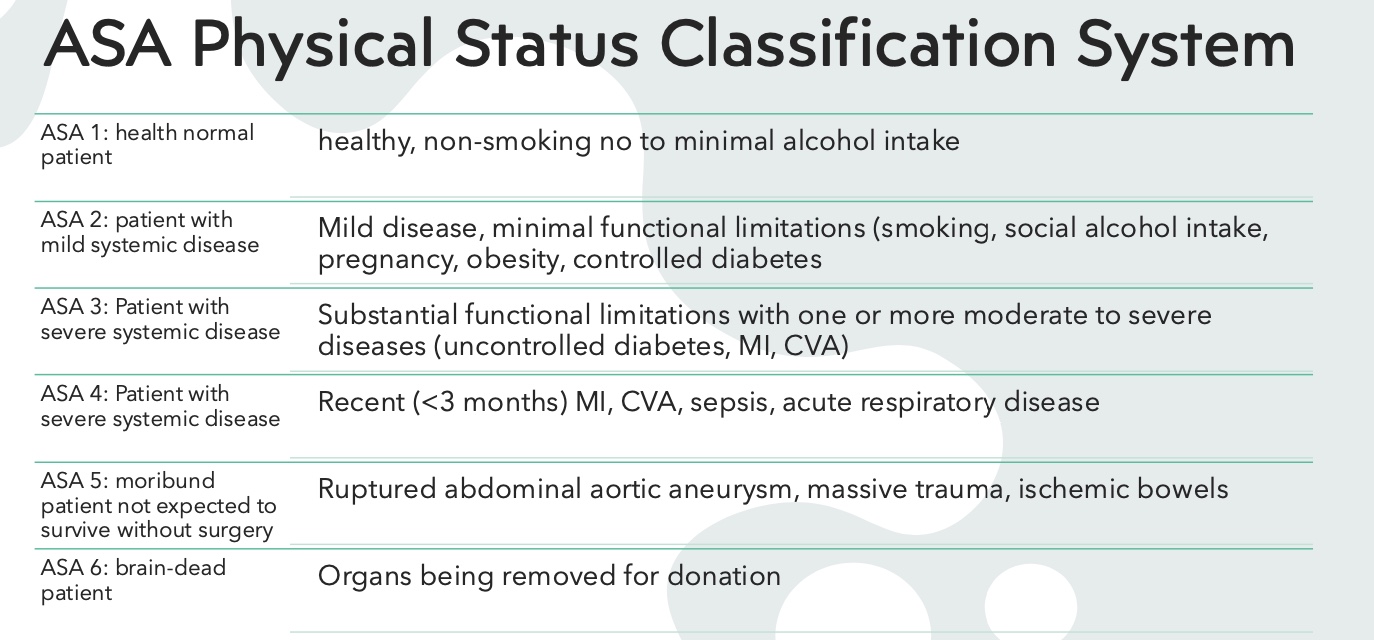
ASA physical status classification system
surgical approches
open: -otomoy
minimally invasive: laparsopic (-oscopy), robotic
laparoscopic surgery
miniimally invasive
holes are smaller
3 ports (tweezer like machines): scope, cotilizaer to stop bleeding, tool)
robotic surgery
all instruments can go through same hole
similar to laparoscopic surgery
who is the intraoperative team
RNs: circulating nurse, scrub nurse (in some cases)
RPNs: scrub nurse
RNFA (first assist): can harvest graft of vein and put it where necessary
anaesthesiologist: manage airway and vital signs, give medications, respond to changes, monitor vent, put in IVs
surgeon
what is a circulating RN
running room to room, counting supplies
not sterile, is documenting, assisting in telling scrub nurse whats next
what is a scrub nurse
hang up materials to surgeon, know when to give materials and which ones to give, knows when to shut up
classification of anesthesia
general: IV/Inhalation → opioids, benzodiaepines, antiemetics
local: variety of routes
regional: spinal, epidural, nerve
procedural: sedatives with/without analgesia
clinical events in the operating room
anaphaylactic reactions
malignant hyperthermia
excess blood loss
what is malignant hyperthermia
genetic in nature
triggered by anesthesia and can cause cardiac death
signs are: rigedity, rise in CO2 levels, rise in temp
postoperative care
protect the patent who was placed at physiologic risk during sugery
prevent complication after surgery
usually occurs in PACU (post anesthesia care) which is close to the OR in proximity
what are the 3 phases of recovery
1: care during immediate post-op period: focused on life sustaining needs with constant monitoring
goal: prepare pt for safe transfer to phase 2 or inpt unit
2: pt is abulatory
goal: prepare pt for transfer to extended care environment or home with discharge teaching
3: extended observation
PACU initial assessment
anaesthesiologist and preioperative nurse give report to PACU nurse
priority of care monitoring and management of airway and circulation, pain, temp, surgical site, and assessment of response to reversal of anaesthesia agents
ABCs, pulse ox, telemetry or arterial blood pressure monitoring, temp/skin, LOC/orientation/sensation/motor skills, assessing drains
very focused assessment
vitals should be where they were pre-op → back to normal
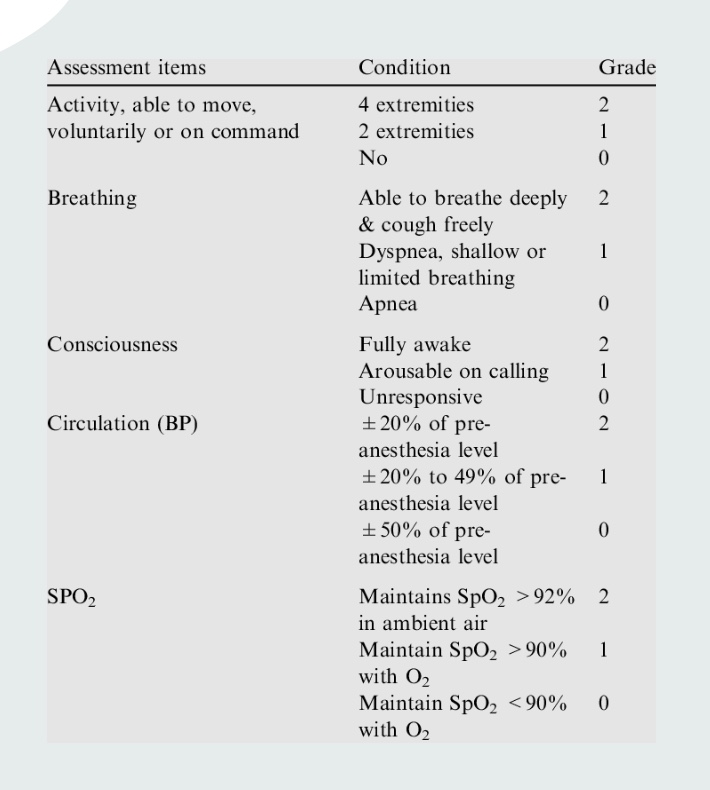
aldrete scale
immediate post-op resp complications
airway obstruction
atelectasis
aspiration
bronchospasm
hypoventilation
resp depression
immediate post-op CVS complications
hypotension: blood loss (check drains for blood), pain meds
hypertension: increase ICP, full bladder, anxiety, pain crisis, hyperthermia
dysrhythmias: existing heart disease, electrolyte imbalances
notify anaesthesa if vitals or rhythms are abnormal → will have not in chart
immediate neuro complications PACU
emrgence delirium: hypoxia, anesthesia agents, bladder distension, immobility, sensory/cogntive impairments, inadequate pain control, polypharmacy, dehyration/malnutrition
delayed awakening: greater than 20-30 min (usually reversible)
pain and discomfort in PACU
anxiety related to pain
frequent pain assessments: pain scale, observations, vitals + assess effectvity of pain modalities
temp alterations in PACU
hypothermia
heat loss from surgery
cold fluids in OR
anesthesia agents
uses bear huggers (warm circulating blanket) or warm fluids (not often) to reverse
GI complication in PACU
nausea and vomiting
GU complications in PACU
low urine output
cute urinary retention
skin alterations
surgical wounds and/or dressings: monitor drainage amount/colour
drains: consider why pt has this, what expected output, colour, amount, + where is it going
surgical site infections: use teach-back method to see understanding
signs of surgical site infection
drainage
peri-wound area is red an angry
warm, fever
smells bad
emotional considerations
anxiety and depression
radical surgery
poor diagnosis post-op
grief
loss
change in independence
what is general surgery
anything to do with the GI tract
Esophagus
Small and large bowel
Rectum
Stomach (gastric)
Liver
Pancreas
Gallbladder
esophagectomy
indication: esophageal cancer
surgical approch: thoractonomy or minimally invasive (thoracoscopy/robotic)
surgical length: 8-10 hr
length of stay: 4-7 days → admitted to ICU for 1-2 days for closer monitoring
post-op considerations: JP drain, epidural/pain control, chest tube (due to proximity to lungs in case of complications), wound care, J-tube for feeding+strict NPO
Small Bowel Resection
indication: bowel cancer, crohn’s, scar tissue/adhesions causing small bowel obstruction, bowel perferation
surgical approch: laparoscopy, robotic/laprotomy
surgical length : 2-4 hours
length of stay: minimally invasive: 1-2 days; open: 3-5 days
post-op considerations: JP drain, epidural/pain contorl, ileostomy (high vs no output, wound care)
colectomy → large bowel resection
indication: bowel cancer, IBD, diverticulities, bowel perforation
surgical approch: laparoscopu, robotic, or laparotomy
surgical length: 2-4 hr
length of stay: minimally invasive: 1-2 days OR open; 3-5 days
post-op considerations: JP drain, epidural/pain control, Ileostomy or colostomy, wound care, changes to output or bowel movements
appendectomy
indications: appendicitis, very rarely appendiceal cancer
surgical approch: laparoscopy
surgical length: 1-2 hr
length of stay: usually same day or 1-2 days
post-op: pain from laparoscopy air, infection
cholecystectomy
indications: gallstones
surgical approch: laparoscopy
surgical length: 1-2 hr
length of stay: usually go home post-op, or 1-2 days
post op considerations: pain from laparoscopy air, retained gall stones
pancreaticoduodenectomy (whipples)
indications: pancreatic or bile duct cancer
surgical approach: laparotomy
surgical length: 6-8 hr
length of stay: 4-7 days
post-op considerations: pain modalities, wound care, drains, nutritional support
used for early found pancreatic cancer
considerations for surgery
past medical history: how does it influence length of stay? what considerations for post-op management?
discharge info: edication on new drains/ostomies, educations on potential complications/when to seek medical attention → teach-back + follow up info
minimizing complications: pain control, abulation, nutrition