Nursing Care for Digestive and Elimination Disorders
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
116 Terms
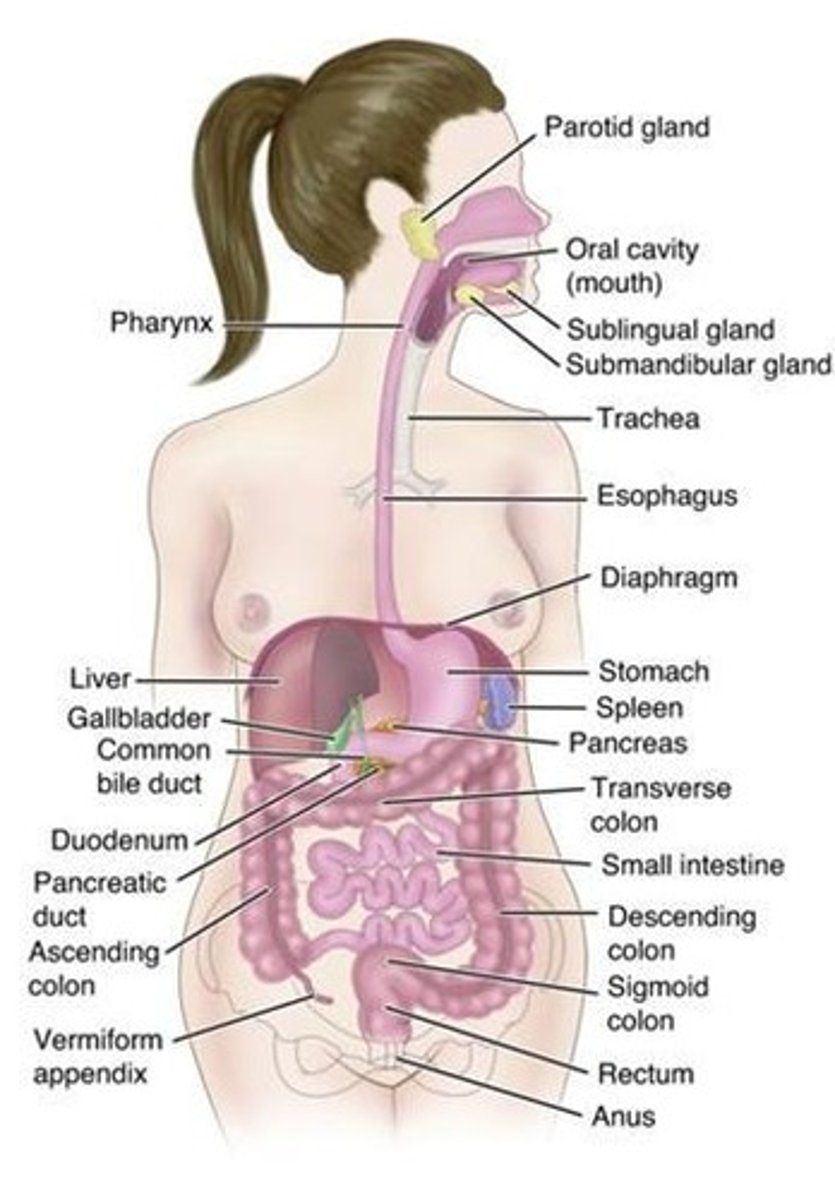
What are the objectives of the lesson on alterations in digestion?
Describe the structure and function of the gastrointestinal tract, explain the mechanical and chemical processes of digestion and absorption, describe pathophysiology and management of irritable bowel syndrome, discuss nursing management of intestinal obstruction, and use the nursing process for inflammatory bowel disease.
What are the gerontologic considerations regarding digestion?
Difficulty chewing, increased heartburn, malabsorption, food intolerances, decreased motility, constipation, and indigestion.
What is intestinal obstruction?
A blockage that prevents the normal flow of intestinal contents through the intestinal tract.
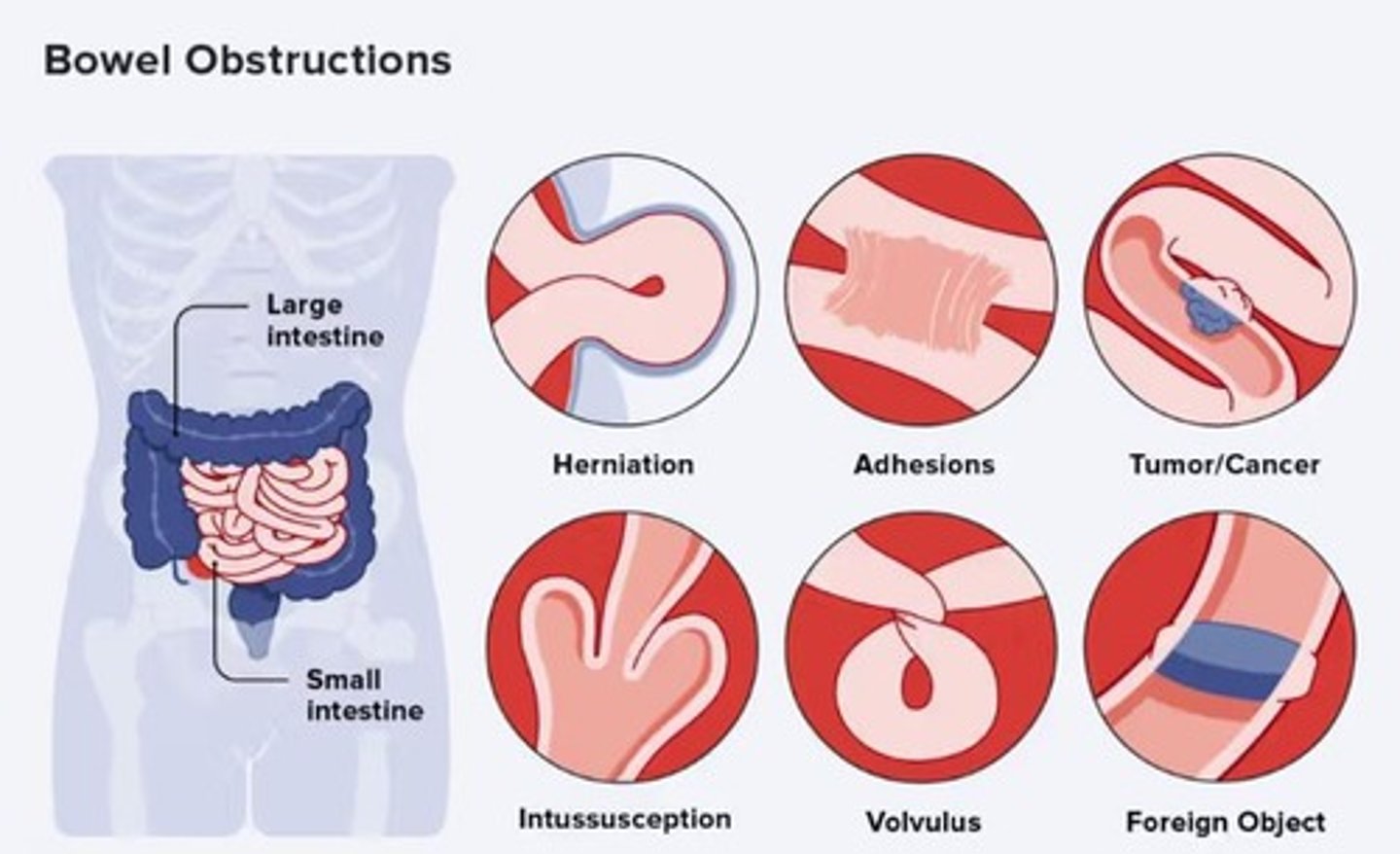
What are the two types of small intestine obstructions?
Mechanical and functional (or paralytic) obstructions.

What are the clinical manifestations of small intestine obstruction?
Crampy, wave-like pain, passing blood or mucus without gas or fecal matter, vomiting, dehydration, abdominal distention, metabolic acidosis, hypovolemic shock, and septic shock.
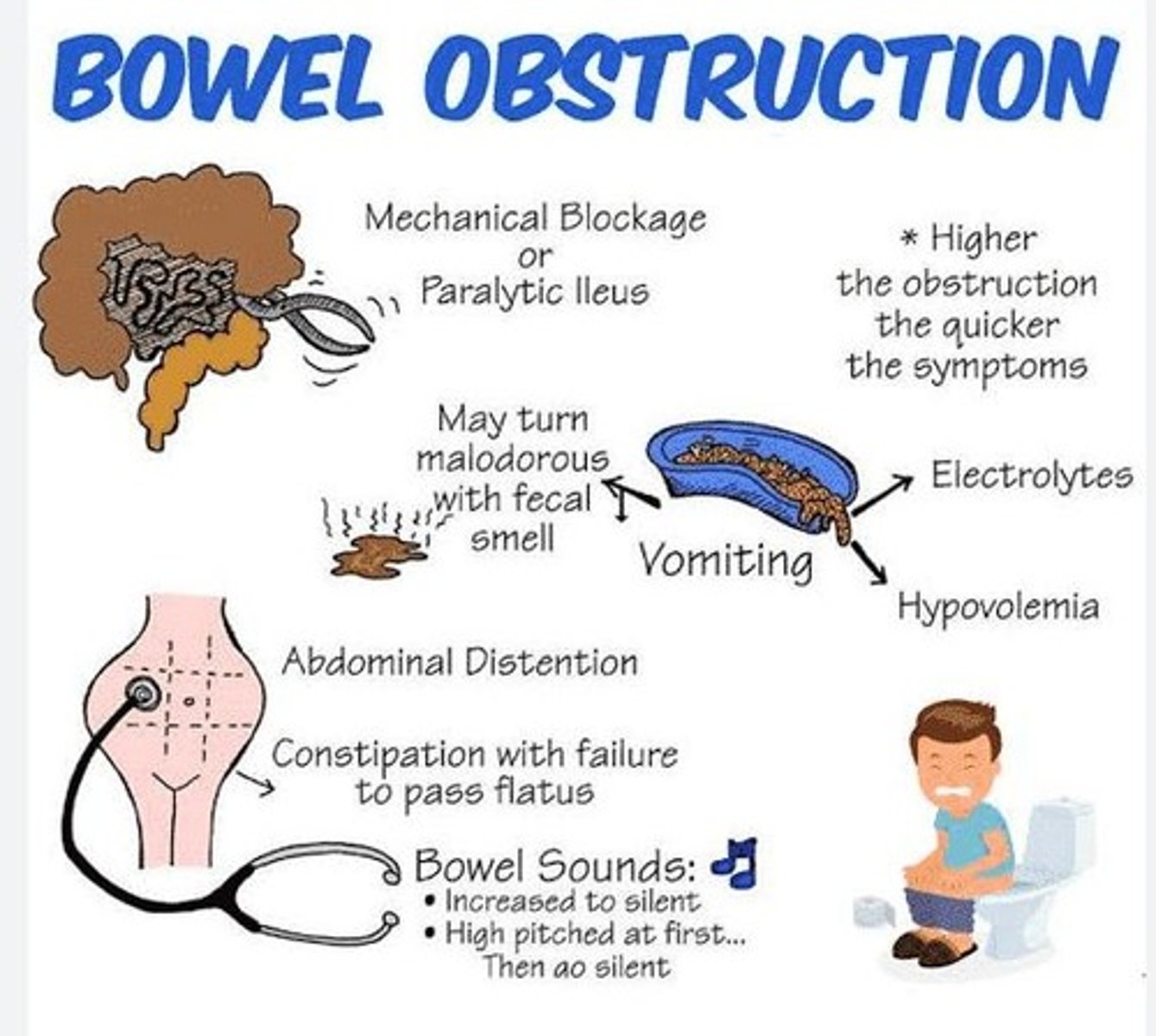
What are the early assessment diagnostics for small intestine obstruction?
Abdominal X-ray, CT scan, labs including CBC and electrolytes, and high-pitched hyperactive bowel sounds.

What are the late assessment diagnostics for small intestine obstruction?
Hypoactive or absent bowel sounds.
What are the medical/surgical management options for intestinal obstruction?
Bowel decompression, stimulation of peristalsis, hernia repair, adhesion division, and removal.

What nursing management is required for a patient with intestinal obstruction?
NG tube maintenance, monitoring nutritional status, assessing for resolution through bowel sounds, abdominal distention, and passing of stool or flatus.

What are the clinical manifestations of large intestine obstruction?
Slow development, constipation, changes in stool shape, blood in stool, weakness, anorexia, abdominal distention, visible bowel loops, and crampy lower abdominal pain.
What are the early assessment diagnostics for large intestine obstruction?
Constipation, abdominal distention, abdominal X-ray, CT, MRI, and labs showing normoactive bowel sounds.
What are the late assessment diagnostics for large intestine obstruction?
CBC, electrolytes, hypoactive or absent bowel sounds, and hyperresonant abdomen.
What is the medical management for large intestine obstruction?
Restoration of intravascular volume, correction of electrolyte abnormalities, NG aspiration, and decompression.
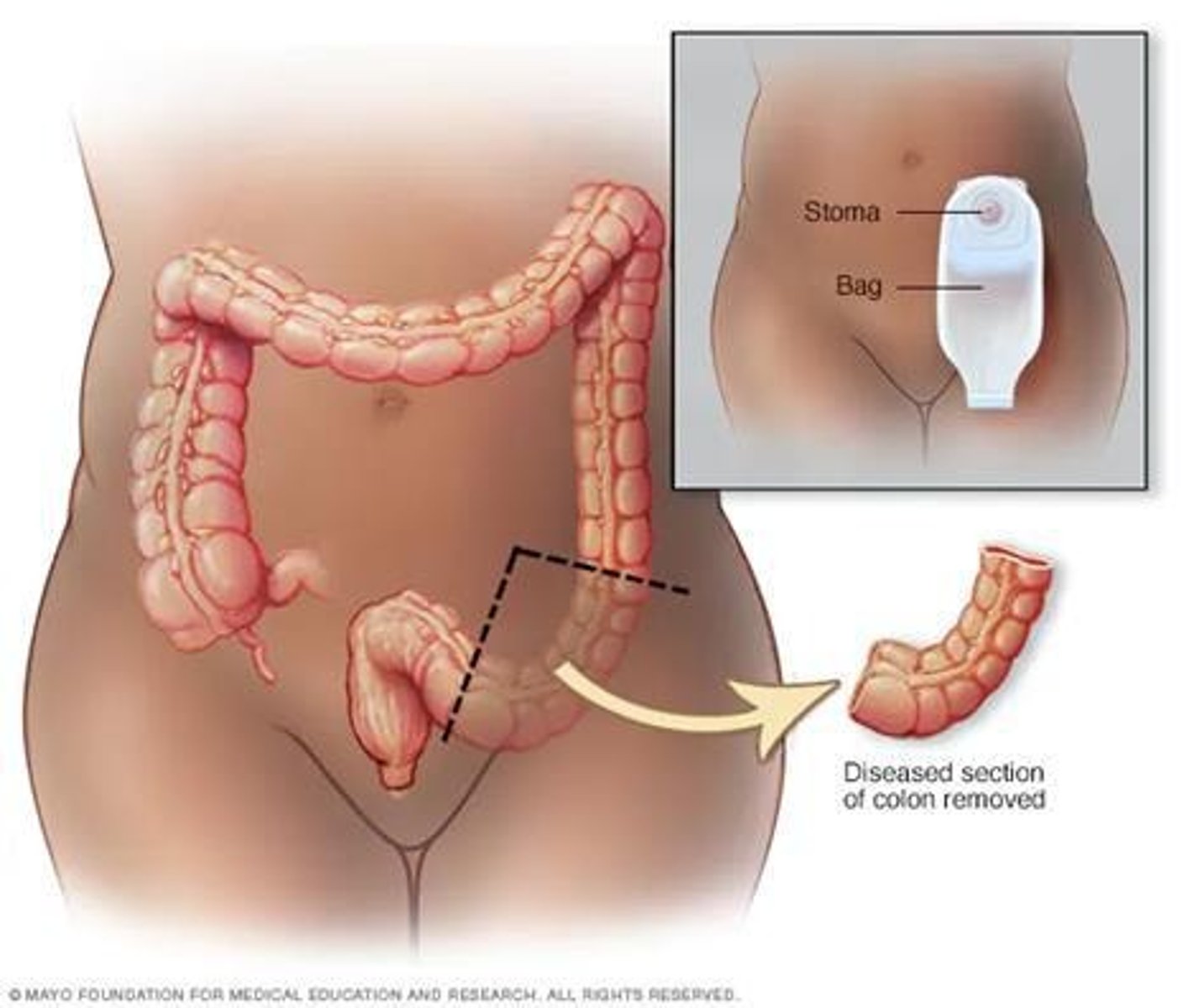
What procedures may be performed for large intestine obstruction?
Colonoscopy, rectal tube, metal colonic stent, resection, temporary/permanent colostomy, and ileoanal anastomosis.
What components are included in the nursing process for patients with intestinal obstruction?
Assessment (H&P, vital signs, pain, bowel sounds, abdominal distention), diagnosis (acute pain, constipation, dysfunctional motility, ineffective tissue perfusion, imbalanced nutrition), planning, interventions, and evaluation.
What are some nursing diagnoses for patients with intestinal obstruction?
Acute pain related to constipation or inflammation, constipation related to malabsorption, dysfunctional gastrointestinal motility related to various conditions, ineffective tissue perfusion related to obstruction, and imbalanced nutrition related to vomiting or altered absorption.
What is the goal of patient education regarding intestinal obstruction management?
To educate the patient and family about the management of the therapeutic regimen or pending procedure.
What is the expected outcome for a patient undergoing management for intestinal obstruction?
The patient will be free from abdominal pain, bloating, and distention.
What are the expected outcomes for a patient with bowel obstruction?
Patient will demonstrate active bowel sounds and the passage of flatus, be free from complications of worsening bowel obstruction, and maintain nutritional and electrolyte lab values within normal range.
What interventions should be taken for a patient with bowel obstruction?
Monitor for symptoms indicating worsening or resolving obstruction, provide emotional support, administer IV fluids and electrolytes, prepare for surgery if needed, and provide routine postoperative care.
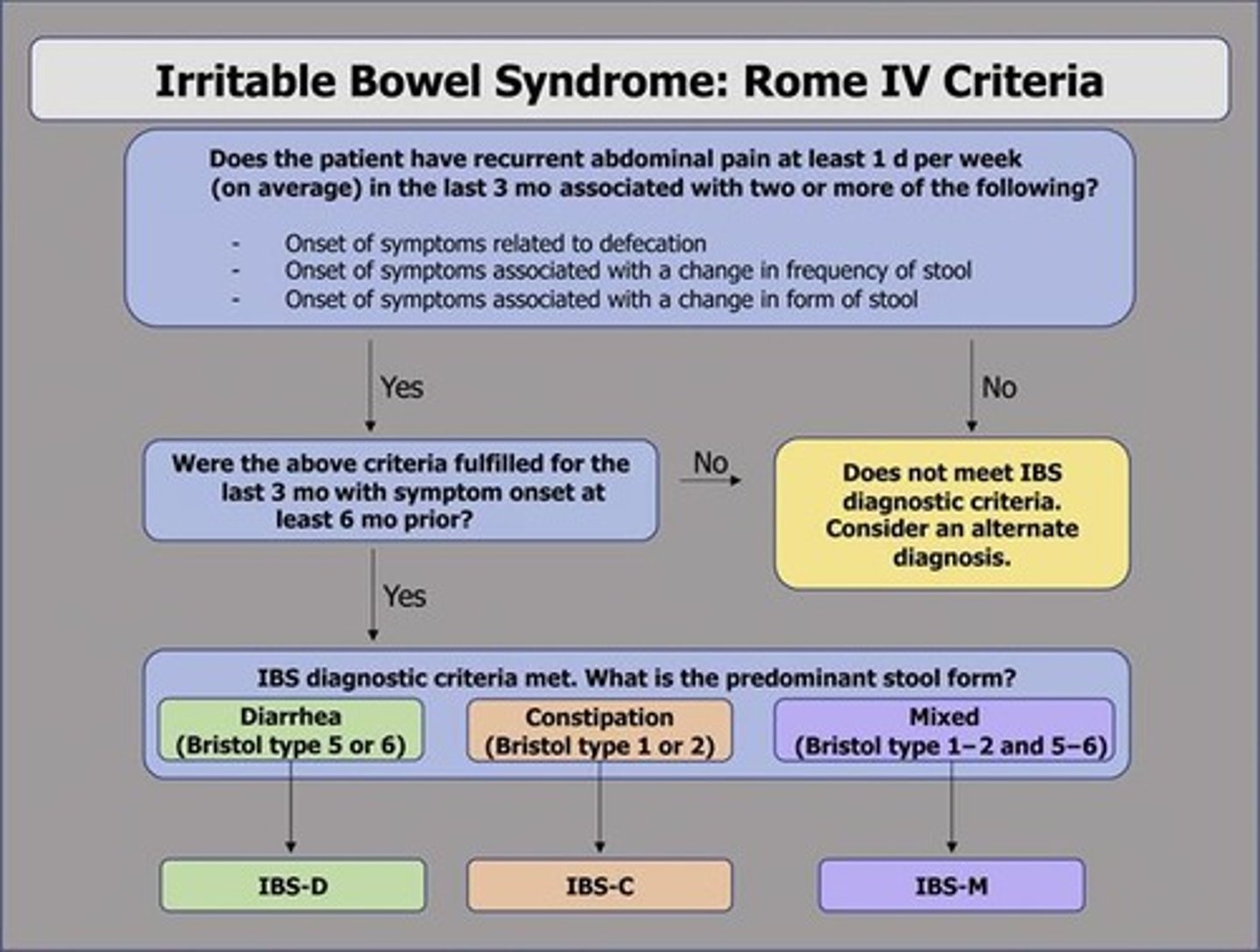
What are the clinical manifestations of Irritable Bowel Syndrome (IBS)?
Alterations in bowel patterns, abdominal pain, bloating, and abdominal distention.
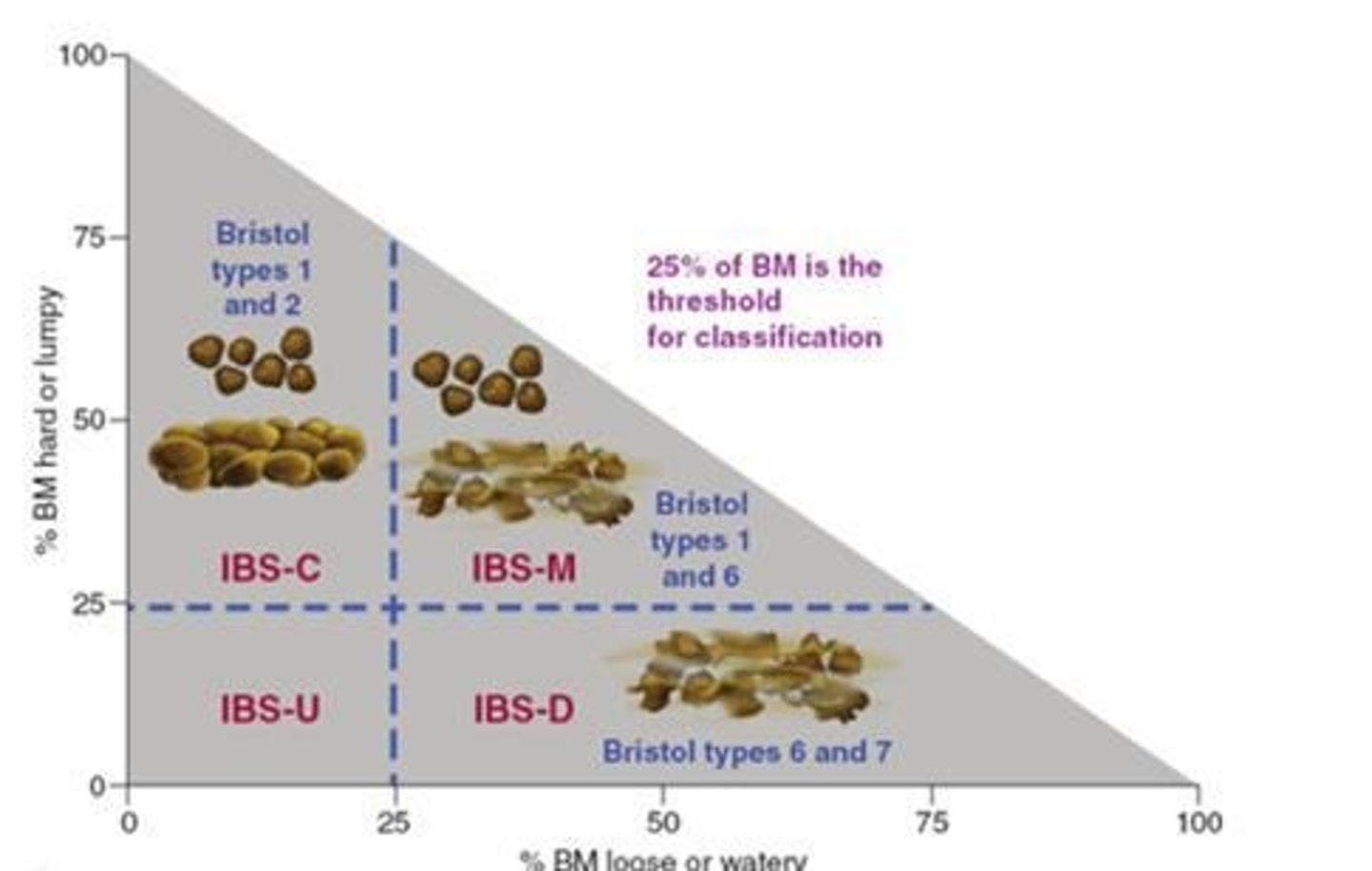
What types of Irritable Bowel Syndrome (IBS) exist?
Constipation (IBS-C), Diarrhea (IBS-D), Combination (IBS-M), and Unclassified (IBS-U).
What diagnostic procedures are used for IBS?
Proctoscopy/Colonoscopy, Barium enema, Manometry, Electromyography, CBC, CRP, fecal calprotectin, serologic testing, stool studies, and contrast radiography studies.
What is the medical management for IBS?
Relieve abdominal pain, control diarrhea/constipation, implement lifestyle modifications (stress reduction, adequate sleep, exercise), and nutrition (high soluble fiber, restriction diet, low FODMAP diet).
What pharmacologic therapies are used for IBS?
Antidiarrheals (IBS-D), Alosetron, Rifaximin, Eluxadoline, Lubiprostone (IBS-C), muscle antispasmodics, antidepressants, peppermint oil, and probiotics.
What nursing assessments are important for IBS?
Health history, abdominal pain, bloating, constipation, diarrhea, and fatigue.
What nursing diagnoses may be applicable for a patient with diarrhea?
Diarrhea related to inflammation, irritation, or malabsorption of the bowel, presence of toxins, or segmental narrowing of the lumen.
What nursing diagnoses may be applicable for a patient with constipation?
Constipation related to deficient fluid volume.
What are some nursing interventions for managing IBS symptoms?
Monitor daily weights, avoid foods that exacerbate symptoms, encourage small meals, encourage participation in diet planning, assess and monitor pain, provide non-pharmacological interventions for pain control, monitor vital signs, and educate on condition, treatment, and outcomes.
What should the nurse evaluate after interventions for bowel obstruction?
Patient and family verbalize understanding of management, patient is free from abdominal pain, bloating, and distention, and maintains nutritional and electrolyte lab values within normal range.
What are examples of mechanical bowel obstructions?
Strictures, Adhesions, Hernias, Tumors, and Intussusception.
What is the significance of a stool diary in IBS assessment?
It helps track bowel patterns and symptoms related to defecation, frequency, and form.
What lifestyle modifications are recommended for IBS management?
Stress reduction, adequate sleep, and regular exercise.
What dietary recommendations are made for patients with IBS?
High soluble fiber intake, restriction diet, and low FODMAP diet.
What emotional support should be provided to patients with bowel obstruction?
Provide emotional support and comfort to help alleviate anxiety and stress.
What is the role of IV fluids in the management of bowel obstruction?
To maintain hydration and electrolyte balance as prescribed.
What is the purpose of preoperative education for patients with bowel obstruction?
To prepare the patient for surgery if their condition does not respond to nonsurgical treatment.
What routine postoperative care is provided after bowel obstruction surgery?
Includes abdominal wound care and monitoring for complications.
What should be monitored to assess the effectiveness of interventions for bowel obstruction?
Daily weights, vital signs, pain levels, and understanding of the disease process.
What is the expected outcome regarding pain management for patients with bowel obstruction?
Achieve and maintain tolerable pain control.
What should patients verbalize regarding their treatment regimen?
Understanding of the management of the therapeutic regimen or pending procedure.
What are the key components of nursing care for patients with IBD?
Educate on condition, treatment, and outcomes; provide emotional support for individual and family; identify coping strategies; refer to resources as needed.
What are the goals of evaluation in nursing care for IBD?
Achieves and maintains stable weight, tolerable pain control, effective coping mechanisms, improvement in symptoms, and fluid and electrolyte balance.
What are the two main types of Inflammatory Bowel Disease (IBD)?
Crohn's disease and ulcerative colitis.
What are some risk factors for developing IBD?
Family history, Caucasian ethnicity, Ashkenazi Jewish descent, living in northern climates or urban areas, age (15-40 and 55-65), current smokers (Crohn's), and former smokers (UC).
What are common assessment findings in patients with IBD?
Nausea, diarrhea, extra-intestinal manifestations (fever, arthralgia, malaise, diaphoresis), family history, weight loss, dietary patterns, smoking history, sleep disturbances, tenesmus, allergies/food intolerances, and stool patterns.
What dietary modifications are recommended for managing IBD?
Oral fluids (clear liquids), low-residue high-calorie diet with vitamin therapy and iron replacement, avoidance of cold foods, avoidance of symptom-exacerbating foods, FODMAP diet, and enteral or parenteral nutrition.
What pharmacologic therapies are used in the management of IBD?
Aminosalicylates, antibiotics, corticosteroids, immunomodulators, and anti-tumor necrosis factor (TNF) agents.
What surgical interventions may be necessary for patients with IBD?
Laparoscopic strictureplasty, small bowel resection, intestinal transplant, proctocolectomy, and ileostomy.
What is Crohn's disease?
A form of IBD characterized by subacute and chronic inflammation of the GI tract that extends through all layers, commonly affecting the distal ileum and ascending colon.
What are common clinical manifestations of Crohn's disease?
Diarrhea, right lower quadrant pain unrelieved by defecation, cramping, abdominal tenderness, weight loss, malnutrition, secondary anemia, dehydration, fever, leukocytosis, steatorrhea, joint disorders, ocular disorders, skip lesions, and oral ulcers.
What diagnostics are used for IBD?
CT scan, MRI, CBC, ESR, and albumin/protein levels.
What complications can arise from IBD?
Intestinal obstruction, stricture formation, perianal disease, malnutrition from malabsorption, fluid and electrolyte imbalances, enterocutaneous fistula, abscesses, and colon cancer.
What is ulcerative colitis?
A chronic ulcerative and inflammatory disease affecting the mucosal and submucosal layers of the colon and rectum.
What are common clinical manifestations of gastrointestinal disorders?
Diarrhea (with mucus, pus, or blood), left lower quadrant pain, tenesmus, bleeding (mild or severe), anorexia, weight loss, fever, vomiting, dehydration, cramping, hypoalbuminemia, electrolyte imbalances, skin lesions, eye lesions, joint abnormalities, liver disease.
What are the complications associated with gastrointestinal disorders?
Perforation, bleeding, toxic megacolon.
What diagnostic procedures are used for gastrointestinal disorders?
Abdominal X-ray, colonoscopy, biopsy, CT/MRI to assess for abscesses, positive stool occult test, hemoglobin and hematocrit, WBC count, albumin, CMP for electrolyte imbalances, stool pathogen testing.
What nursing assessments are important for patients with gastrointestinal disorders?
Health history, vital signs, pain assessment, diarrhea frequency, nausea/vomiting, bowel habits, smoking history, bowel sounds.
What are common nursing diagnoses for patients with gastrointestinal disorders?
Diarrhea associated with inflammatory process, acute pain associated with increased peristalsis and GI inflammation, hypovolemia associated with anorexia, nausea, and diarrhea, impaired nutritional status, activity intolerance, anxiety related to impending surgery, difficulty coping, risk for impaired skin integrity.
What are the goals for planning in the nursing process for gastrointestinal disorders?
Attainment of normal bowel elimination patterns, relief of abdominal pain and cramping, prevention of fluid volume deficit, maintenance of optimal nutrition and weight, avoidance of fatigue, reduction of anxiety, promotion of effective coping, absence of skin breakdown, increased knowledge about the disease process.
What interventions are included in the nursing process for gastrointestinal disorders?
Maintaining normal elimination patterns, relieving pain, maintaining fluid intake, ensuring optimal nutrition, promoting rest, reducing anxiety, enhancing coping measures, preventing skin breakdown, monitoring for complications.
What is Gastroesophageal Reflux Disease (GERD)?
A common disorder marked by backflow of gastric duodenal contents into the esophagus, causing troublesome symptoms and/or mucosal injury.
What are the clinical manifestations of GERD?
Pyrosis (heartburn), regurgitation, dyspepsia (indigestion), dysphagia, hypersalivation, esophagitis, dental erosion, ulceration in pharynx and esophagus, laryngeal damage, pulmonary complications, esophageal strictures, adenocarcinoma.
What diagnostic procedures are used for GERD?
PPI trial, ambulatory pH monitoring, endoscopy, barium swallow, Nissen fundoplication.
What pharmacologic therapies are used for GERD?
Antacids, histamine-2 receptor antagonists, proton pump inhibitors, prokinetic agents, reflux inhibitors, surface agents/alginate-based barriers.
What nursing assessments are important for patients with GERD?
Health history, anorexia, nausea/vomiting, regurgitation, belching, dyspepsia, heartburn/pyrosis.
What are common nursing diagnoses for patients with GERD?
Impaired nutritional intake, imbalanced nutrition, risk for aspiration, acute pain related to irritated esophageal mucosa, knowledge deficit.
What are the goals for planning in the nursing process for GERD?
Client will ingest daily nutritional requirements, report pain relief, achieve and maintain adequate body weight, maintain patent airway, have increased knowledge of actions that reduce reflux.
What interventions can help manage GERD?
Encourage adequate nutritional intake, eat slowly and chew food, small frequent meals of non-irritating foods, swallow liquids with food, avoid tobacco and alcohol.
What are important pain relief strategies for GERD?
Small, frequent meals, avoid activities that increase pain, remain upright for 1-4 hours post-meal, do not eat before bed, be cautious with OTC antacids to avoid rebound acidity.
What are indicators of successful evaluation in the nursing process for GI disorders?
Patient ingests daily nutritional requirements, reports pain relief, maintains adequate body weight, has a patent airway, demonstrates increased knowledge of reflux management, and reports decreased anxiety.
What are the key learning objectives for the lesson on alterations in elimination?
The learner will be able to describe the pathophysiology, clinical manifestations, and management of constipation and fecal incontinence, explain factors contributing to urinary tract infections, use the nursing process for lower urinary tract infection care, and differentiate between adult dysfunctional voiding patterns.
What is the focus of the nursing process in relation to lower urinary tract infections?
The nursing process is used as a framework for the care of patients with lower urinary tract infections.
What should a nurse be able to differentiate regarding urinary incontinence?
A nurse should be able to differentiate between various adult dysfunctional voiding patterns.
What educational plan should be developed for a patient with urinary incontinence?
An education plan tailored to the specific dysfunctional voiding pattern of the patient should be developed.
What clinical manifestations are associated with constipation and fecal incontinence?
The lesson aims to describe the pathophysiology and clinical manifestations of constipation and fecal incontinence.
What factors contribute to upper and lower urinary tract infections?
The lesson includes an explanation of the factors contributing to both upper and lower urinary tract infections.
What is defined as fewer than three bowel movements weekly or hard, dry, small, or difficult to pass stools?
Constipation.
What are the types of constipation?
Functional, Slow-transit, Defecatory disorder, Opioid induced, Perceived, Secondary.
What are some clinical manifestations of constipation?
Fewer than three bowel movements per week, abdominal distention, pain, bloating, sensation of incomplete evacuation, straining at stool, elimination of small-volume hard stools, and tenesmus.
What criteria must be met according to the Rome IV criteria for diagnosing constipation?
Two or more of the following for the last 3 months: straining for at least 25% of bowel movements, lumpy or hard stools for at least 25% of bowel movements, sensation of incomplete bowel movements 25% of the time, sensation of anorectal obstruction at least 25% of the time, manual maneuvers needed at least 25% of the time, and less than 3 bowel movements per week.
What diagnostic tests can be used for constipation?
Barium enema, sigmoidoscopy, stool testing, anorectal manometry, defecography/colonic transit, lower GI endoscopy/X-ray.
What are some pharmacologic management options for constipation?
Bulk forming laxatives, saline agents, stimulants, emollient stool softeners, osmotic agents, and lubricants.
What are some complications associated with constipation?
Decreased cardiac output, syncope, orthostatic dizziness, fecal impaction, hemorrhoids, fissures, rectal prolapse, and toxic megacolon.
What gerontologic considerations are relevant to constipation?
Often choose processed foods low in fiber, decreased food/fluid intake, limited mobility, weak abdominal and pelvic muscles, polypharmacy, depression, weakness, dulled nerve impulses, and dependent laxative use due to overuse.
What patient education is important for managing constipation?
Nutrition, exercise, laxative use, and establishing a normal bowel pattern.
What is fecal incontinence?
Recurrent involuntary passage of stool from the rectum for at least 3 months.
What are the clinical manifestations of fecal incontinence?
Minor soiling, occasional urgency, loss of control, complete incontinence, poor control of gas, and diarrhea.
What assessments and diagnostics are used for fecal incontinence?
Rectal examination, endoscopy (sigmoidoscopy), radiography studies, barium enema.
What medical management strategies are used for fecal incontinence?
Treat underlying causes (diarrhea, fecal impaction, drug regimen), fiber supplements, biofeedback, sacral nerve stimulator, bowel training program, and surgery.
What patient education is important for fecal incontinence?
Bowel training program, bowel diary for 1-2 weeks, skin care (meticulous hygiene, perineal skin cleansers, skin protectants), internal or external collection devices, and emotional support.
What are urinary tract infections (UTIs)?
Infections caused by pathogenic microorganisms in the urinary tract.
What are the common sites of lower urinary tract infections?
Cystitis, prostatitis, and urethritis.
What are the common sites of upper urinary tract infections?
Pyelonephritis, interstitial nephritis, renal abscess, and perianal abscess.
What gerontologic considerations are relevant to urinary tract infections?
Cognitive impairment, frequent use of antimicrobial agents, neurogenic bladder, decreased prostatic secretions in men, decreased estrogen production in women, and early symptoms such as malaise, nocturia, urinary incontinence, foul-smelling urine, burning, urgency, fever, and delirium.
What assessments are used for urinary tract infections?
Pain/burning with urination, frequency, nocturia, incontinence, hematuria, and ~50% asymptomatic.
What diagnostics are used for urinary tract infections?
Urine culture, cellular studies (pyuria), dipstick testing, STDs, X-ray, CT, and ultrasound (kidneys).
What nursing process steps are involved in managing urinary tract infections?
Assessment, diagnosis, planning, interventions, and evaluation.
What interventions are included in the nursing process for urinary tract infections?
Relieving pain, administering medications as prescribed (antibiotics, analgesics, antispasmodics), applying heat to the perineum to relieve pain and spasm, and increasing fluid intake (e.g., cranberry juice to acidify urine).
What are some urinary tract irritants that should be avoided?
Coffee, tea, citrus, spices, cola, and alcohol.