Liver / TIPS (4)
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
Qs A patient’s right brachial pressure is 120mmhg and left is 115mmhg. The patient’s left DPA & PT are 120mmhg and 140mmHg, respectively. Their right DPA and PT are 80 and 90mmHG, respectively. Calculate their ABI.
LT : 140/120 = 1.16
RT : 90/120 = 0.75
Qs what is claudication and at what ABI value would it typically occur? what about rest pain ABI value?
claudication → pain/cramping of legs when walking
classic claudication range → 0.5-.9
rest pain → .3-.5 (<.5)
Qs When analyzing segmental pressures, look for pressure gradient changes > ______mmHg; disease is always ____________ to the cuff detecting this pressure difference
30; proximal
Qs PPG produces flow waveforms via_______, and typically applied on one’s __________.
infrared light ; digits (fingers/toes)
what is portal hypertension and its most common cause?
elevated pressures in portal venous system from impeded blood flow through the liver
caused most commonely by cirrhosis
portal hypertension leads to
varices (swollen veins)
ascites
splenomegaly
what are the indicaitons for TIPS?
refractory variceal bleeding
refractory ascites
hepatic hydrothorax
what are some symptoms of patients with portal HTN who need TIPS
GI bleeding
black stools
vomiting blood
encephalopathy (failure to detoxify liver → can cause confusion/cognitive slowing)
decreased clotting factors
ascites
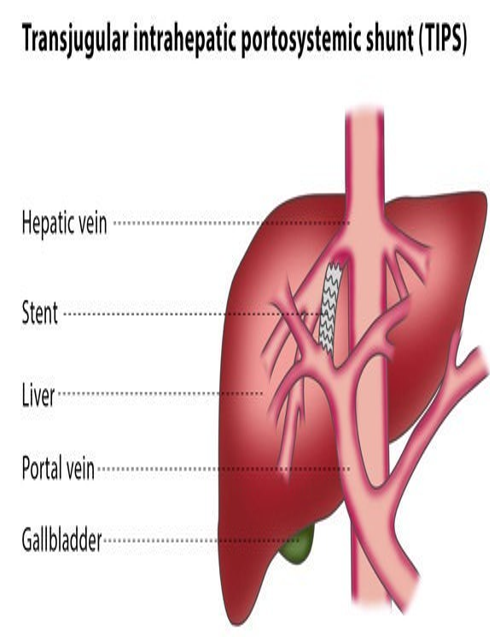
what does TIPS stand for?
transjugular intrahepatic portosystemic shunt
what is TIPS?
a stented channel between a portal vein and hepatic vein
typically RPV (posterior branch) and RHV
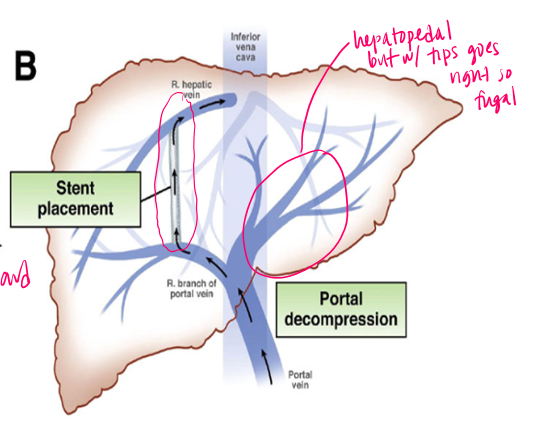
what kind of resistance does the TIPS shunt have?
low resistance
diverts blood around liver
what is the hemodynamic goal of TIPS?
redirect portal flow through the shunt
decrease portal venous pressure
reduct pressure gradient across liver
what are the complications of TIPS?
mechanical injury to liver
ischemic injury to liver
bleeding from procedure
recurrent vaiceal bleeding
recurring ascites/hydrothorax
worsening portal hypertension
how can we optimize color doppler when analyzing TIPS?
adjust PRF for venous flow
lower wall filter
optimize gain (no noise)
identify flow direction
what happens if color doppler is not optimized?
false stenoses
what are the required sampling sites for TIPS?
MPV (direction & wavefom)
PROX : portal end of TIPS (insertion of MPV)
MID stent
DISTAL : hepatic venous end, outflow (inserts into IVC)
portal branches if visualized
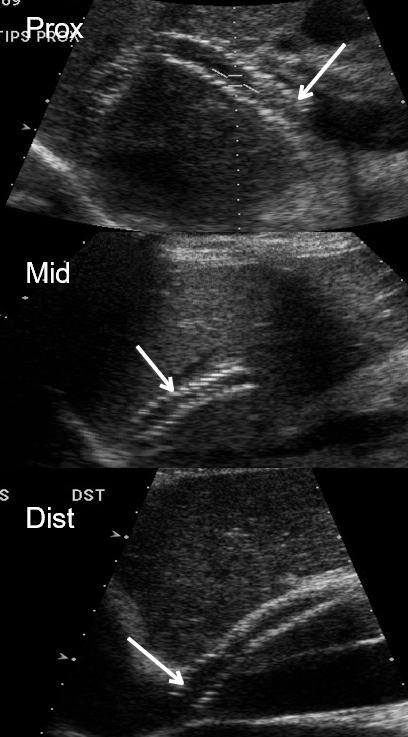
what kind of flow is expected in TIPS stent?
hepatofugal
portal to hepatic vein
what is a normal TIPS stent velocity?
90-190 cm/s
what is the abnormal threshold for significant dysfunction of TIPS stent?
if velocity is less than 30cm/s
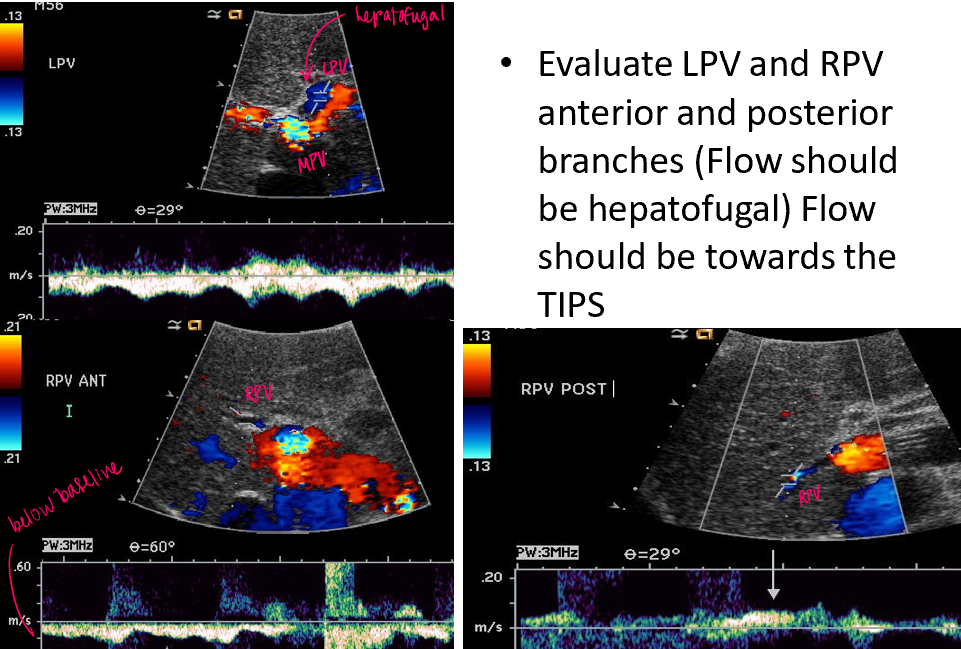
how does flow direction change in the MPV, LPV, RPV, Hep Art, with TIPS stent?
all vessels exhibit hepatofugal flow except the MPV (hepatopedal or bidirectional)
how will TIPS waveform appear 1 day post insertion?
early TIPS is pulsatile → takes time for pressure to equalize
early pulsatility = shunt open and is communicating with heart
pulsatility after weeks/months = outflow stenosis/cardiac influence
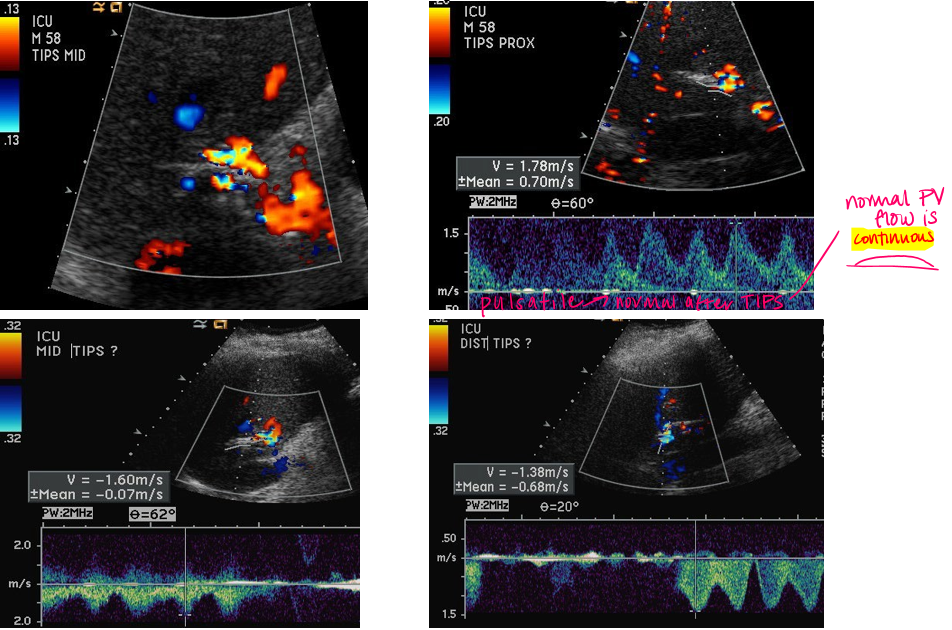
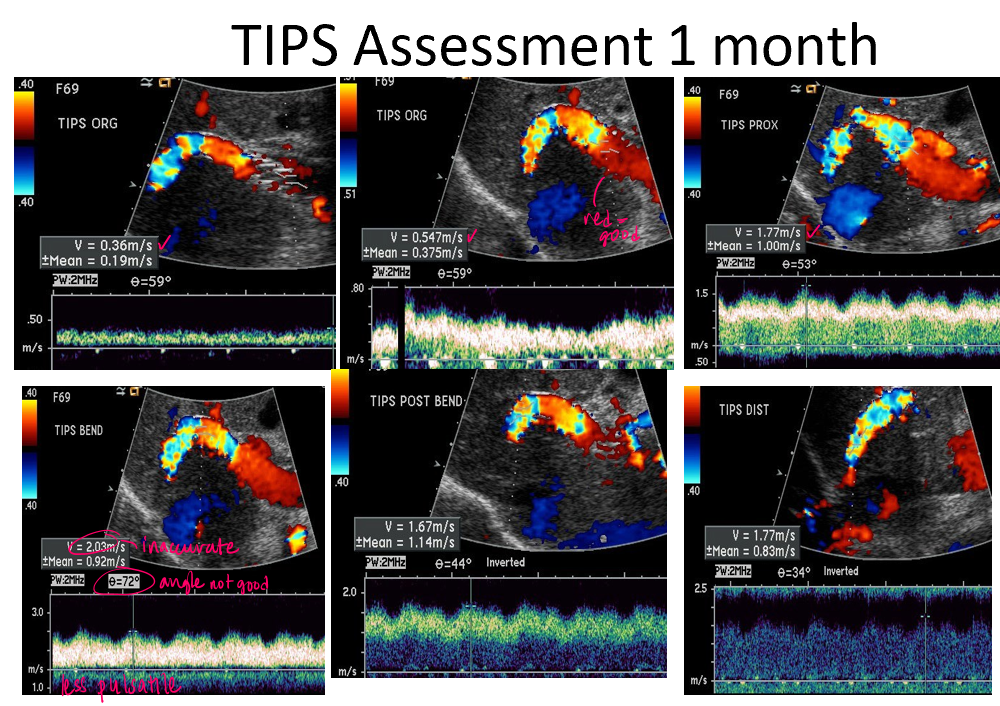
tips flow may appear pulsatile immediately after placement due to direct transmission of hepatic venous and cardiac pulsations through a newly created low resistant shunt
eventually → hemodynamic equilibration
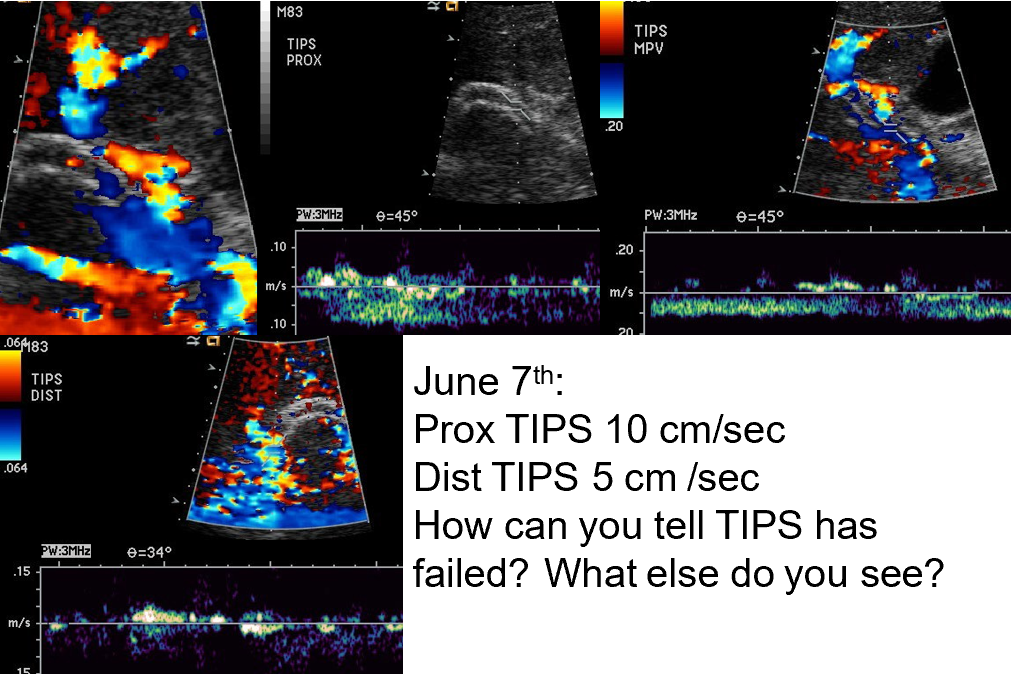
what are indications of TIPS failure?
thrombosis (occlusion) → absence of flow
partial thrombosis → residual flow reduced velocity
stent fibrosis → narrowing throughout stent
stenosis → site of high velocity in stent
generalized low velocity through stent
recanalization of previous varices
reduction of portal vein flow from baseline or directional change
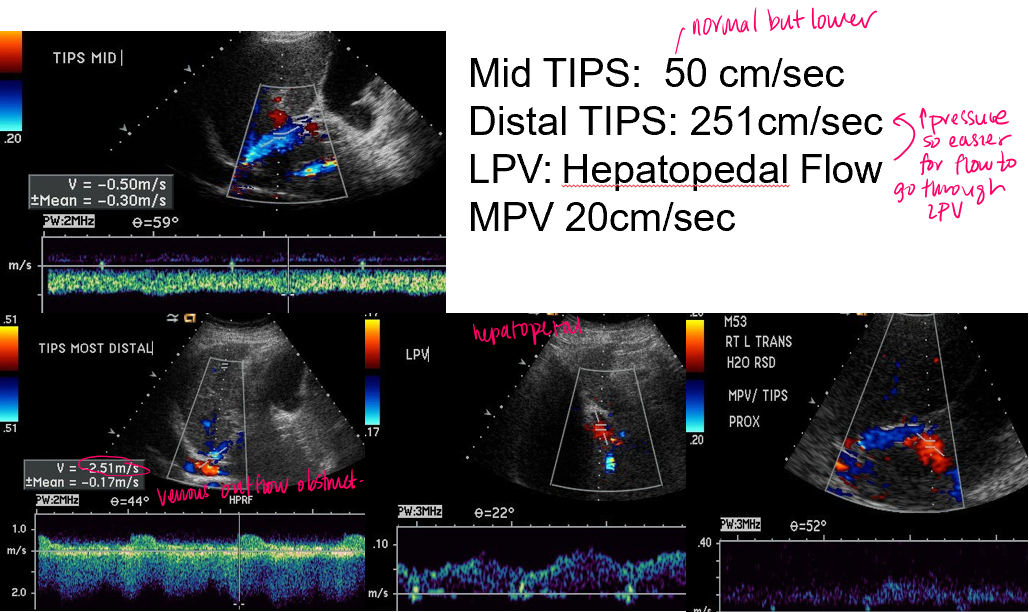
case example
mid TIPS velocities are 50cm/s → below normal
distal TIPS velocities are 251 cm/s → above normal
LPV is flowing in ‘normal direction’
should be hepatofugal flow with TIPS
Conclusion
stenosis of distal TIPS
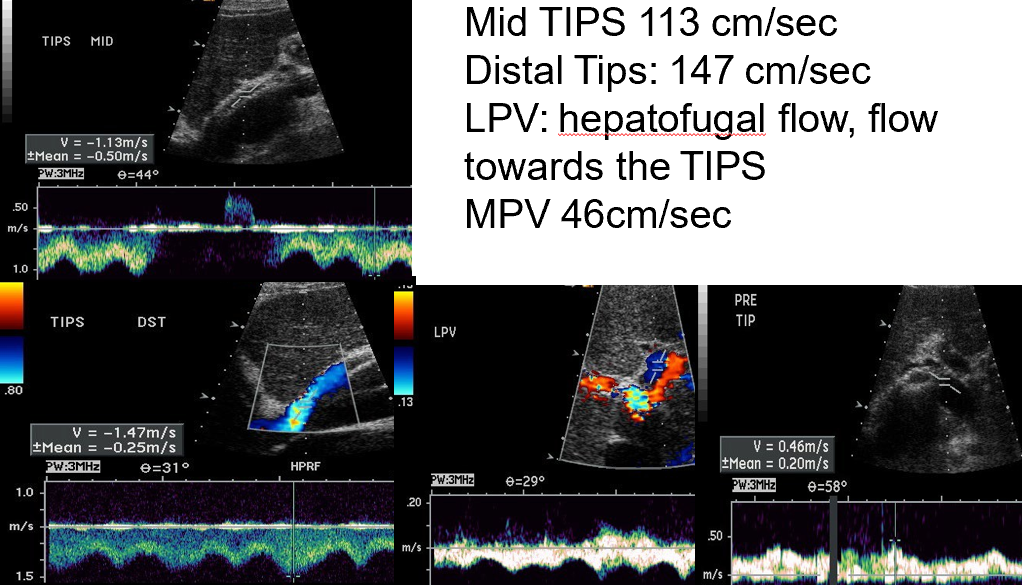
successful or unsuccessful revision of TIPS?
successful
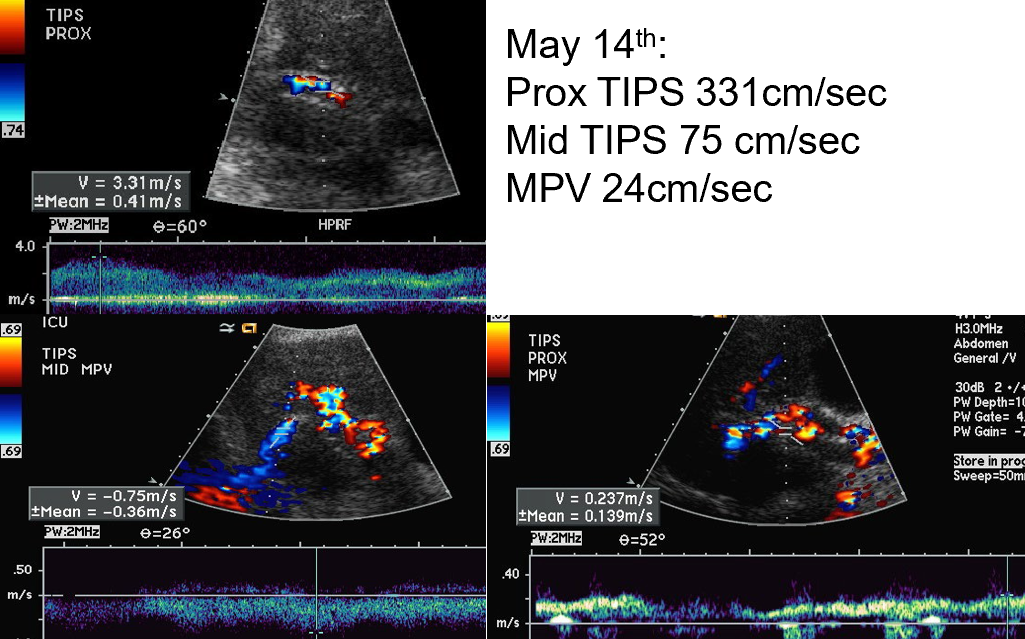
what does this show?
prox TIPS velocity → HIGH
mid TIPS velocity → low
MPV velocity → low
Conclusion : PT required a TIPS revision
downstream stenosis reduces forward flow → velocity drops upstream
low velocities
direction
upper right image of MPV → hepatofugal flow when MPV should be hepatopetal
how do we know if TIPS is functioning properly?
velocities in TIPS between 70-200 (or 90-190) cm/sec
LPV flow reversed (hepatofugal)
RPV flow reversed (hepatofugal in anterior and posterior branches)
MPV proximal to TIPS velocity → >30cm/s
varices recede with time
Qs A proper functional TIPS would demonstrate what kind of flow in each vessel?
LPV : hepatofugal
RPV (ant) : hepatofugal
RPV (post) : hepatofugal
MPV : hepatopetal / bidirectional
Qs A normal velocity of TIPS is?
>30
90-190 cm/s
Qs failure of TIPS dysfunction velocity is?
<30cm/s
Qs T/F : Hepatopetal flow is above the baseline
False : depends on angle
Qs How can you differentiate hepatic veins from portal veins?
waveform
PV continuous
HV to and fro
bmode
PV : echogenic bright walls
case 1 :
Recurrent ascites 6 months post-TIPS
Focal high velocity near hepatic venous end
Diagnosis? Location? Clinical implication?
diagnosis : classic outflow stenosis
location : distal end of TIPS (hep/ivc junction)
implication : reduced effective shunt flow, rising portal pressures → explains recurrent ascites
case 2
Recurrent variceal bleeding
No demonstrable flow in stent
primary concern?
what must be documented before calling it?
suspected occlusion → ONLY AFTER OPTIMIZATION
no color
no spectral
case 3
routine follow up
pulsatile but patent flow
normal or abnormal?
why?
we need to know how long after the procedure this is
normal right after TIPS procedure
but after a couple of months portal system should adapt and pressure gradients should stabilize
if there is still pulsatility → outflow stenosis