Physiology of gaseous exchange and mechanisms of ventilation
1/47
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
48 Terms
What respiratory muscles are active during inspiration?
contract to increase thoratic capacity, diaphragm, for deep breaths: external intercostals, accessory muscles
What muscles are active during expiration?
relaxation decreases thorcic capacity, elastic recoil of lung
What muscles are active during forced expiration?
contraction decreases thoratic capacity, abdominal muscles, internal intercostals, some in the back and neck
What are the accessory muscles for inspiration called?
scalenes and sternocleidomastoids
What abdominal muscles are involved in forced expiration?
internal and external oblique, rectoabdominal and transverse abdominal
What happens in inspiration?
at the end of quiet expiration, the respiratory muscles are at rest, balance between forces of calapse and expansion of the thoratic cavity
inspiration, inspiratory muscles contract, decreased thoratic volume, increased intrapleural pressure, increased lung volume, decreased alveolar pressure so negative pressure gradient so air enters the lungs
Whar are the calapsing and expantion forces acting on the lungs?
callapse - elastic recoil of lungs, expantion - elastic recoil of chest wall and rib cage anatomy
What happens in expiration?
relaxation of inspiritory muscles, decreased thoracic volume, increased in intrapleural pressure, decreased lung volume, increased alveolar pressure, air leaves the lungs to functional residual capacity
What happens in forced expiration?
contraction of expiratory muscles, decreased thoratic volume, increased intrapleural pressure, decreased lung volume, increased alveolar pressure, air leaves lungs below functional residual capacity
What is the plural cavity?
space inbetween the parietal pleura and the visceral pleura with plural fluid in it, negative pressure sucks the two membranes togther so chest can move lung, if there is air in it it calapses the lung
How does inspiration and expiration affect the plural membranes?
inspiration - active, driven centrally, expand rib cage, increases -ve, interplural pressure pulls lungs open creating air flow
normal expration - passive as elastic recoil, muscles relax, lungs recoil (elastic fibres), created +ve pressure, forces air out
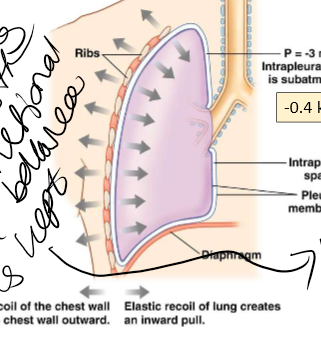
What is intrapleural pressure equal to?
intrathoracic pressure, not a constant value
What holds the two pleural membranes together?
surface tention so when chest expantion takes the parietal pleura with it, the visceral pleura will follow with the lung tissue
What are the two parts of the airways?
conducting (no gas exchange) and respiratory (gas exchange)
What parts of the airway are in the conducting airways?
treachea, bronchi and bronchioles
what is the structure of the trachea and bronchi?
cartalige and smooth muscle pipe - sturdy as they need to remain open
what is the structure of bronchioles?
smooth muscle
What parts of the airway are part of the respiratory airways?
repiritory broncioles and alveoli
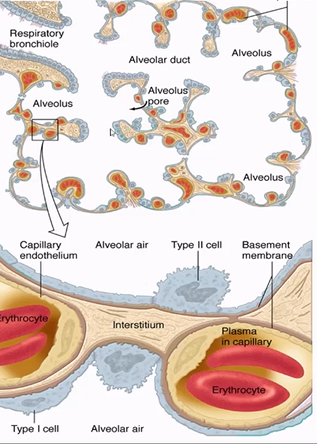
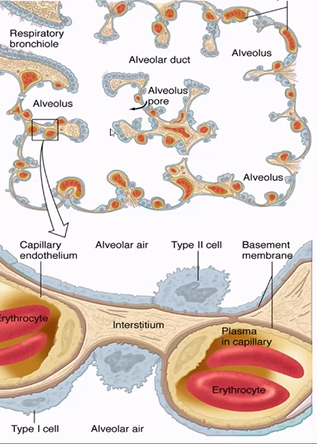
What do the alvoli overall structure look like?
hexagonal interconnected sacks with thin walls

What are the functions of the airway?
deliver O₂ and remove CO₂ from the blood, body pH balance (regulatory arterial blood CO₂ or pCO₂), defence systems, metabolic, vocal and olfaction
What is respirtory rate detmined by?
CO₂ concentration, changes blood pH as acidic
What are the defence systems of the airway?
warm and humidify inspired air (so don’t damage alvoli), prevent particles from entering lungs , disarm/remove particles that do enter the lungs, nycicukary system and cough, phagocytic cells, inflammatory and inmmunologic responces
What happens to bronchioles during ventilation?
bronchioles are attached to alveoli/lung interstitium, inspiration pulls bronchioles open, expiration bronchioles get smaller, at low lung volume they close and trap gas in the lungs - reduces total volume breathed, volume at which they callapse increases in various lung diseases, major site of smooth muscle contraction and obstruction in athsma, smooth muscle regulated slightly by tone of parasympathetic nervous system innovation onto it vs the adrenaline circulating
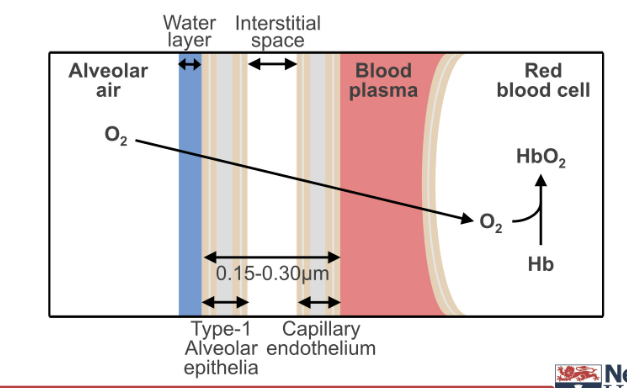
What are the 5 layers of the wall of the alvoli from air to blood?
alveolar epithelium, basement membrane, interstitium (thin), basement membrane, capillary endothelium
What are the types of alvolar cells?
Type 1 - primary lining cells, flat, 95% of surface
Type 2 - tall/fat granular, 60% cover 5% surface area, produce surfactant
What does surfactant do?
reduce surface tention in the lungs, make it easier for them to expand, outside of alvoli are covered in water, they want to stick together, reducing surface tention reduces this
What is the interstitium?
area with lots of elatic fibres, allowing lungs to be stretchy
What immune cells are found in the lungs?
alveolar macrophages, scavange particles and surfactant
What is the overall stucture of the alvoli togther?
interconnected honeycomb of cavities, shared interconnecting walls, stress on one transmitted to neighbours, allows mechanical stress to be shared across a larger area of lung parenchyma, mechanism contributes to elastic recoil of the lung in dstention and resists the collapse of individual alveoli in atelectasis

Describe the oxygen cascade
small amount lost from atmosphere to trachea due to humidification adding water
large amount lost between that and alveolus due to alveolar gas equation
tiny amount lost on way to pulmonary capillary due to diffusion
tiny amount lost on way to artery due to physiological shunt
mitrocondra have very low pO₂ as lots of them and using the air
veins have a lot more than mitrocondria due to tissue metabolism
What is a physiological shunt (blood gasses)?
pullmony circulation also supplies blood to the conducting airways which doen’t pick up oxygen
What is the oxygen delivery system?
lungs and cardiovascular system
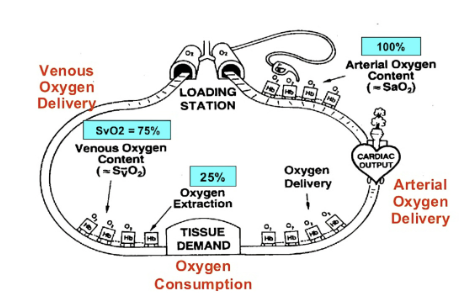
What is the saturation of haemoglobin at different points?
at the lungs 99-100%, 75% at the tissues (unload 25%), if excessive tissue demands so low venous ox saturation so harder to get up to 100% at the lungs, only a problem in elivated altitudes for most people
What is Dalton’s law?
total pressure of a mixture of gases = to sum of partial pressures of all consitiuent gases
What is partial pressure?
in a mixture of gases, the presure the gas would exert if occupied the volume alone, proportional to the relative amount of gas, in solution (when interfacing between a gas and liquid) concentration is proportionals to gas partial pressure and to amount/solubility, in blood should technical use the word tention
What is Henry’s law?
amount of given gas dissolved in a given liquid is directly proportional to partial pressure of the gas in contact with the liquid, proportionallity constant changes depending on solubility of gas in liquid, for any partial pressure of gas solubility is inversly proportional to tempreture, if warmed up the gas wants to leave the solution, but temp is maintained in the body
What is the gas tention of solution?
the partial pressure of a gas with whch that solution is in equilibrium
Explain how the partial pressures of oxygen change
alveolar PO₂ lower than atmospheric air as only oart of alveolar air replaced with inspired air in each breath, why alveolar gas composition relativly constant, aterial PO₂ lower because of shunting of pulmonary blood (some conditions can cause major shunting)
Why are PO₂ and PCO₂ still important even though there are other assisstance mechanisms?
determine how much gas carried by other systems (e.g. Hb saturation), transfer of gasses is driven by tention/pp differences, dissolved O₂ from hyperbaric 100% O₂ inspiration important in treatment of CO poisoning
What is the problem with O₂ and CO₂ just in the blood?
not enough for adaquate delivery or removal
What increase the blood’s O₂ capacity?
heamoglobin (primary mechanism)
What increases the blood’s CO₂ capacity?
conversions
How efficent is gas diffusion between alveoli and blood?
rapid equilibration of pulmonary capillary blood in alveolus, diffusion across alveoli is rapid
What is Ficke’s law for gases?
diffusion is proportional to surface area, membrane thickness, gas partial pressure differences, gas solubilities
What would impare gas exchange at the alvolar membranes?
conditions where the membrane where thicker or the surface area was reduced, high altitude affects partial pressure differences (less oxygen to be absorbed)
How does emphysema (COPD) alveolar O₂ exchange?
exchange of O₂ and CO₂ decreased due to loss of alveolar surface area
How does lung fibrosis affect alveolar O₂ exchange?
O₂ diffusion slowed due to thickened alveolar membrane
When O₂ alveolar exchange is affected why is CO₂ exchange okay?
diffuses 20x faster as more soluble