W1 - Ingestion
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
What are Salivary Glands?
A typical exocrine gland consisting of acini and ducts that secrete saliva into the oral cavity which is part of the GIT Lumen
How do Exocrine glands work?
produces secretion inside acini and delivers it via ducts onto surfaces or cavities.
Exocrine glands include salivary glands and are accessory structures to digestion —> not in direct contact with food but secrete their substance into GIT which then interacts with food
What happens to fluid from exocrine glands?
Fluid from exocrine glands is taken from the extracellular fluid compartment and then modified by the duct cells to be hypotonic to allow better taste perception.
What structures are involved in salivation?
Acini (secretory)
Ducts (transport)
Myoepithelial cell (contractile)
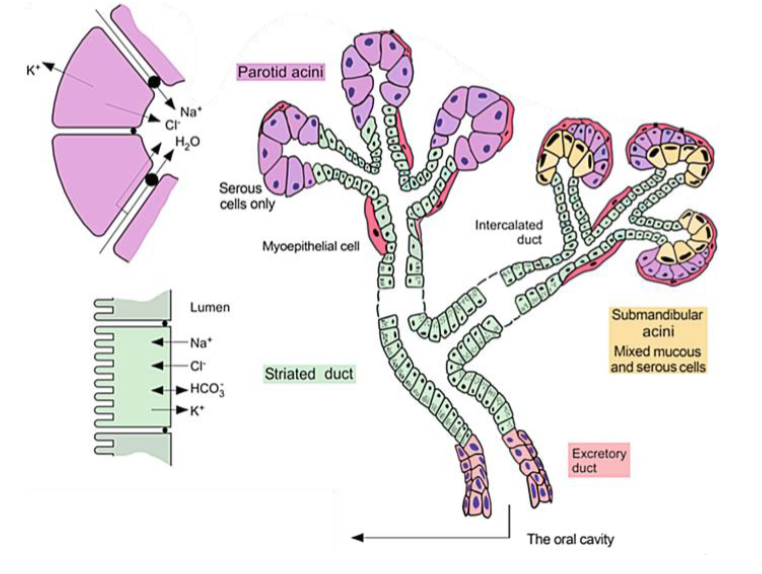
What are Acini? and what are there function in salivation?
What: Sac of secretory cells (mucous or serous type)
Function: Produce isotonic secretion from ECF by modifying the fluid with their own unique constituents and then send it through the ducts.
What are the type of secretory cells that make up the acini?
You can have mucous type or serous type secretory cells
Acini of the Mucous gland = musin glycoprotein
Acini of the Submandibular gland = mixed gland
Acini of the Parotid gland = mainly serous
Why do Acini produce their isotonic secretions from ECF?
because the ECF has a rich blood supply so it borrows blood plasma
How do Acini produce isotonic secretion from ECF?
by modifying the fluid with their own unique constituents and then send it through the ducts.
This allows the external solution to have the same solute concentration and water concentration as the body/ intracellular fluids.
What are Ducts? What is their main purpose/ function?
What: a tube or vessel of the body through which fluids pass.
Function: transport saliva to oral cavity
What is the function and the ductal cells in salivation? and how is this achieved
Function: makes fluid fit for purpose
How: Modify the isotonic fluid secreted by the acini into a hypotonic secretion (saliva) by reabsorbing Na and Cl
How do the ducts keep the fluid hypotonic?
They have little permeability to water and therefore exchange of ions can occur but not water.
Why is it important for the duct cells to modify the isotonic solution to become hypotonic?
Hypotonic solutions have a lower osmotic pressure than the body/ intracellular fluids. This allows better taste perception as it prevents the ions in the saliva from overpowering the taste of some of the food molecules.
What are myoepithelial cells and what are their functions?
What: Contractile cells
Function: Push secretions (saliva) out of the acini and proximal ducts —> into the distal ducts —> then into the opening where they need to be delivered
where are myoepithelial cells located
Mostly around acinic and proximal parts of the duct
What are the constituents of Saliva?
Water (>99%)
Electrolytes
Buffers
Mucous Glycoproteins
Antimicrobials (endogenous)
Digestive Enzymes
Nitrogenous Wastes
What is the function of water in saliva?
Keeps oral cavity clean by moistening it - nothing sticking to teeth for too long
Allows swallowing by lubricating food
Dissolving and distributing food particles for taste
What happens when you have a dry mouth?
Can’t taste food properly - water is needed to dissolve and distribute the food particles
Mouth becomes dirty - needs to be constantly flushed to be kept clean
Cannot swallow effectively - foods need to be lubricated
What is the function of electrolytes in saliva?
Maintain tonicity
Examples = Na, K, Cl
What is the function of buffers in saliva?
Buffers are alkaline —> Maintain pH of 7 by neutralizing acid from oral microbes (ferment them)
Examples = HCO3 (bicarbonate)
What is the function of mucous glycoproteins in saliva?
Mucins lubricate the oral cavity
More sticky - provide protective barrier in oral cavity
Why are buffers important in saliva?
Buffers are alkaline substances and help to neutralise acids from oral microbes in order to maintain a pH of 7. If the pH becomes too acidic, the enamel of the teeth will be dissolved.
What is the function of Antimicrobials in saliva?
Control oral microbes - prevents over-colonization
Example: lysozyme, IgA
What is the function of digestive enzymes in saliva?
Digestion of macronutrients - smaller they are allows us to taste them more
Types of digestive enzymes
α amylase (ptyalin) digests complex carbs e.g. starch (amylose)
Lingual lipase digests lipids e.g. triglycerides
What is the function of nitrogenous wastes in saliva?
Have no function, hence wastes —> they are secreted into mouth and then excreted through faeces ( similar to excretion at kidneys)
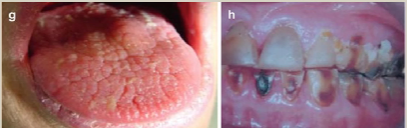
What is Xerostomia
a condition of dry mouth due to inadequate salivation. This can be caused by a number of etiologies:
general conditions e.g. dehydration, emotional stress (effects NS which regulates salivation)
diseases (pathological) e.g. Sjögren’s syndrome, diabetes, cystic fibrosis
therapies (iatrogenic) e.g. opioids, radiation -- based on stimulation of NS
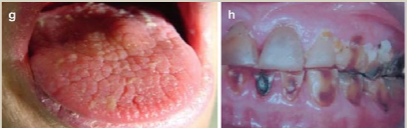
What are consequences of Xerostomia?
Xerostomia = dry mouth due to inadequate salivation
Based on the composition of saliva, some consequences of xerostomia are;
Teeth rot - not cleaned
Incomplete digestion - lack of digestive enzymes
How is Salivation controlled?
salivation consists of secretomotor activity. Secretomotor activity is controlled by the parasympathetic nervous system.
This produces 2 types of salivary secretions (serous, mucous)
What are the two types of salivary secretions and how are they controlled?
Secretomotor activity is controlled by the parasympathetic nervous system.
Two types of secretions:
Serous – contains enzymes, electrolytes, antibodies, etc
Mucus – contains mucins for lubrication, little bit of protection
What do the 2 different types of salivary secretions contain?
Serous – contains enzymes, electrolytes, antibodies, etc
Mucus – contains mucins for lubrication, little bit of protection
How much do each glands contribute to the secretomotor activity of saliva?
Parotid Gland - 20 - 25%
Submandibular Gland - 70 - 75%
Sublingual Gland - 5%
Which types of salivary secretions does each gland produce?
Parotid Gland - Serous only
Submandibular Gland - serous and mucus
Sublingual Gland - serous and mucous
Which gland is the main contributor to salivary excretions?
Parotid gland —> responsible for 75% of secretions
What innervates the parotid gland (PSNS)?
Glossopharyngeal nerve (CN IX)
What innervates the submandibular gland (PSNS)?
Chorda Tympani of Facial Nerve (CNVII)
What innervates the sublingual gland (PSNS)?
Chorda Tympani of Facial Nerve (CNVII)
What is the brain stem responsible for (in terms of reflex)
responsible for unconscious control of basal physiological functions that contribute to homeostasis and general daily regulations in out body.
What is the cerebral cortex responsible for (in terms of reflex)
conscious control over body movements
Stimuli of the Unconditioned (innate) Salivation reflex
mechanical (chewing, texture of food)
chemical (taste of food)
Salivation Reflex - Unconditioned (innate) Reflex
Stimulus → brain stem (salivatory nucleus) → glands
Sensory Input of the Unconditioned (innate) Salivation reflex
Comes from different cranial nn. with varying levels of contribution. Delivers signals to the salivatory nucleus of the brainstem.
Motor Output of the Unconditioned (innate) Salivation reflex
All PSNS. Nerve involved is dependent on the gland:
glossopharyngeal nn. = parotid gland
facial nn. = submandibular and sublingual gland
Salivation Reflex - Conditioned (learned) Reflex
Stimulus → cerebral cortex → brain stem → glands
Stimuli of the Conditioned (learned) Salivation reflex
sensory (sight, smell, sound of food)
cognitive (thought of food). e.g. ice cream truck
Classical conditioning
when a controllable (external) conditioned stimulus is used to hijack the reflex.
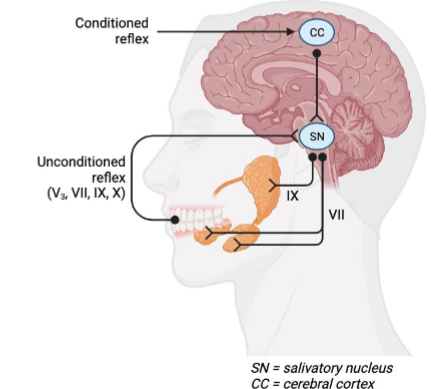
What is this?
the salivatory reflex
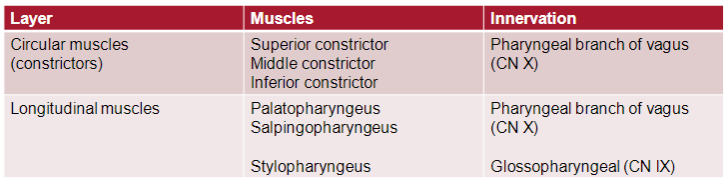
Compared to the remaining GIT, why are pharyngeal muscles unique?
Motility in the oral cavity and pharynx is controlled by skeletal muscle, whereas the rest of the GIT (excl. anus) is controlled by smooth muscle. THEREFORE… pharyngeal muscle activity can be voluntary or involuntary
What are the palatal mm. used for?
Together with the tongue, these assist with the voluntary phase of swallowing.
What are the pharyngeal mm. used for?
Pharyngeal mm. assist with the involuntary phase of swallowing/ deglutition.
These include the pharyngeal constrictors and laryngeal elevators
ext. pharyngeal constrictors (circular mm.) - contract and constrict the lumen above the bolus of food
int. laryngeal elevators (longitudinal elevator mm.) – pull the pharyngeal wall up and over the bolus of food
What is deglutition?
the action or process of swallowing
What are the 3 phases involved in deglutition?
Oral Phase - Voluntary
Pharyngeal Phase - Involuntary
Esophageal Phase (in transit) - Involuntary
Steps of Oral Phase of Deglutition
Oral phase (voluntary)
Tongue moves the bolus posteriorly and creates a seal - vacuum needed to swallow food
Soft palate moves posteriorly and closes the passage to the nasopharynx to avoid bolus moving into nasal cavity (this occurs if do it too quickly)
Epiglottis is elevated and the laryngeal inlet is opened to allow breathing
Upper esophageal sphincter is closed due to tonic contraction
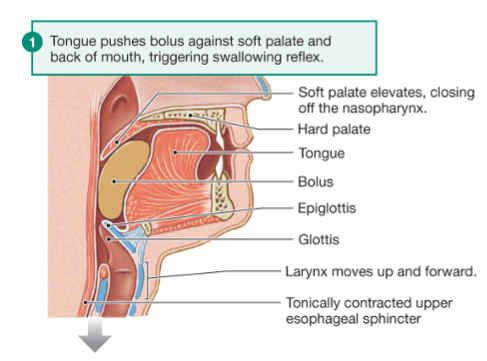
what does it mean if a sphincter is closed due to tonic contraction?
tonic = always tone/ tension
THEREFORE…. Tonic contraction = sphincter only opens when something wants to move from upstream of the sphincter to downstream of the sphincter
Steps of Pharyngeal Phase of Deglutition
Pharyngeal phase (involuntary)
Epiglottis is depressed (movement is primarily due to the bolus pushing on it)
Laryngeal inlet is closed to avoid bolus entering the respiratory system (Breathing is temporarily inhibited)
Pharyngeal muscles contract to move the bolus inferiorly (so food isn't caught at the back of throat)
The upper esophageal sphincter relaxes and opens to allow passage of bolus
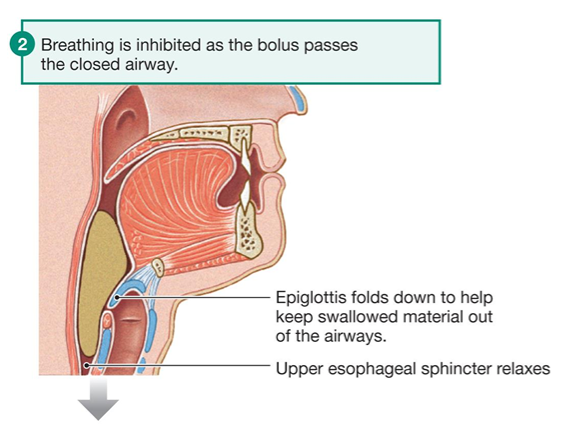
What stimulates the Pharyngeal Phase of Deglutition? What is the response
Pharynx stretches due to presence of the bolus from the oral phase. Baroreceptors detect the stretch and signal the sphincter to relax and constrictors to contact to allow safe passage of bolus of food
Steps of the Oesophageal Phase of Deglutition
Esophageal phase - in transit (involuntary)
Esophagus (smooth muscle) undergoes peristalsis to move food inferiorly to the stomach
Lower esophageal sphincter relaxes and opens to allow entry of bolus into the stomach
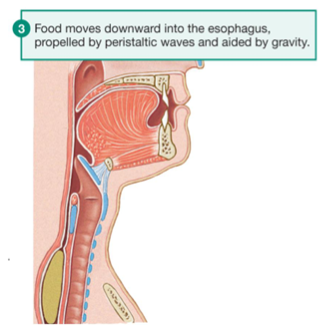
What forms the lower esophageal sphincter?
the esophageal hiatus in the muscular part of the diaphragm
Innervation of Pharyngeal Muscles
Innervation to these muscles is via the pharyngeal plexus (parasympathetic).
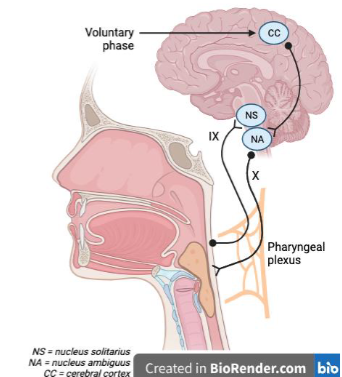
Deglutition reflex - Voluntary Phase
Stimulus → cerebral cortex → brain stem → muscles
Bolus in mouth, reflex is not stimulated
Deglutition reflex - Involuntary Phase
Stimulus → brain stem → muscles
Bolus enters pharynx, reflex is stimulated
Deglutition reflex
Stimulus — Distension (activates stretch receptors)
Afferent signal to brainstem via CN IX
Efferent signal to pharynx via pharyngeal plexus (mainly CN X, also CN IX and XI)
pharyngeal muscles contract
upper esophageal sphincter relaxes
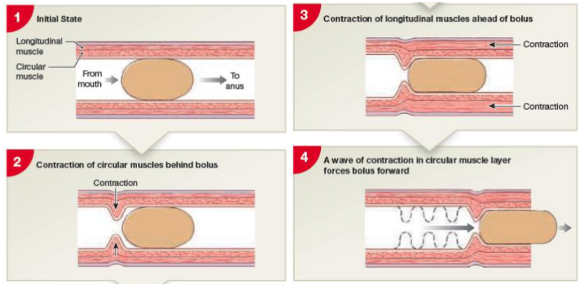
What is peristalsis?
Peristalsis is a contraction of smooth muscle that propels food unidirectionally through the GIT.
Steps of Peristalsis
Initial State — Bolus is formed in the mouth and enters the GIT
ext. circular muscles behind the bolus contract
int. longitudinal muscles ahead of the bolus contract
A wave of contraction in circular muscular layer forces the bolus forward
What do secretions control?
salivation
What does motility control?
deglutition/ motility
Overall explanation of exocrine secretion
Glands contain secretory cells.
These borrow contents of ECF, including plasma and then modify the fluid with their unique constituents and send it through the ducts.
The Ducts modify the contents of secretion and then secrete their contents into the lumen of the GIT
Examples of secretion other than salivation
Stomach: gastric pits that secrete protein-digesting enzymes and HCl
Liver: bile ducts that secrete lipid-digesting bile, stored in the gallbladder
Pancreas: exocrine secretions include macronutrient-digesting enzymes and bicarbonate (pancreas = Car wash of GIT)
What is the major difference between salivary secretion and other GIT secretions?
Endocrine control
Overview of muscles role in motility
Can be smooth or skeletal muscles
Input = Distension from the bolus of food stimulates stretch receptors
Output = Muscles contract to propel contents
Overview of sphincters function in motility
Without stimulus = tonically contracted = permanent tension to close them (sympathetic)
With stimulus = relaxed and open
Overall control of motility
Parasympathetic nervous system
Stimulus: the presence of food in the mouth
Output: contraction of the constrictor muscles.
How does motility operate in other parts of the GIT?
Stomach: propulsion includes peristalsis and churning (multidirectional)
Intestines: propulsion includes peristalsis and segmentation (bidirectional)
Sphincters: pyloric (smooth muscle), anal (smooth and skeletal muscle)
What are the major differences between pharyngeal motility and other GIT motility?
muscle type (smooth muscle)
intrinsic control (enteric nervous system).
Overview