Psych disorders exam 2
1/141
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
142 Terms
OCD key terms
Exposure and response prevention
Thought-action fusion
Exposure and response prevention (ERP)
Type of CBT treatment for OCD
Expose someone to obsessions and then prevent the response
Ex: germ obsession → have someone touch doorknob → they cannot wash their hands to tolerate obsession
KEY: cannot do compulsion anymore
Thought-action fusion
Belief that thoughts are equivalent to their action counterpart (“these thoughts can hurt me”)
Think that the thoughts are just as dangerous as the action
Worsens the cycle
Thought stoppage does not really work that well
Treatment for OCD
ERP
Some medications → including SSRIs
New directions of treatment involve interventions like deep brain stimulation to help reset neural pathways
Can be invasive
Hoarding disorder
Now on its own a disorder
Acquire stuff and cannot get rid of it
Genetic predisposition/biological component
Treatment looks different than normal treatment for OCD
Resistance to treatment:
Could have been going on for years
Ego- syntonic : in line with what you believe (opposite of ego - dystonic)
Difficulty making decisions
Personifying objects
Not many longitudinal studies out there now
History of traumatic loss (anecdotal evidence)
In theory → use ERP but tough
Risk of hoarding grows over time/ age → less control you have as you get older
Body dysmorphic disorder
Obsession with perceived flaw in appearance
Perception of the flaw - and outside reaction - that matters
In our own society → probably getting easier to fall prey to this → constant feedback on appearance
Should not be double jeopardied from eating disorder (separate thing) symptomology
To the point of despair and distress
Facial features, skin… → does not involve change in eating/diet plans
Self-esteem really suffers
Other disorders in obsessive compulsive category
Trichotillomania: hair pulling disorder
Excoriation (skin picking) disorder
Other types of OCD:
Substance/medication induced, due to other medical conditions, specified OCD like Koro (fear of retracting genitalia)
PANDAS/PANS
PANDAS and PANS
PANDAS:
SUDDEN onset of OCD symptoms in child after strep infection
Brain inflammation
Often misdiagnosed
PANS:
More general also SUDDEN
Can be after covid, Lyme…
Used to write neat and tidy → not anymore
Different than typical child with OCD because it is SUDDEN
Important to get actual medical treatment → suffers so much might need blood treatments
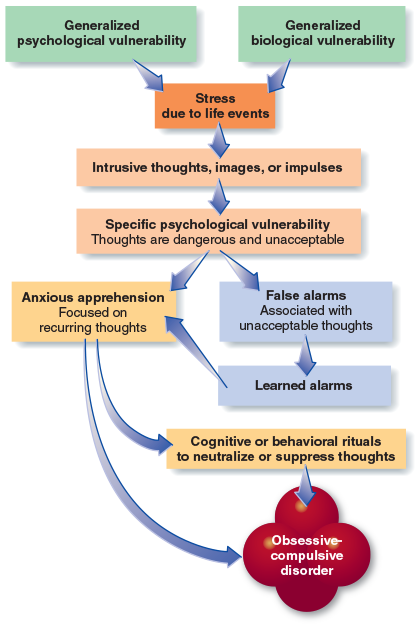
OCD etiology
Hypothesis: early experiences taught them that some thoughts are dangerous and unacceptable because the the terrible things they are thinking might happen and they would be responsible
These early experiences would results in specific psychological vulnerability to develop OCD
Thought-action fusion
Strength of religious belief → associated with thought-action fusion and severity of OCD
Model of Etiology:
PTSD - and what is trauma
Still under anxiety umbrella
One of the few disorders where a specific event must happen as part of the criteria
Feeling helpless appears to be a significant component
Trauma: level of danger was significant → body goes into fight or flight mode
Criteria for PTSD
Exposure to trauma
Trauma must occur in real life, not online, unless work-related (not really true now)
Intrusion symptoms - memories, dreams, dissociations, distress at exposure, or physiological reaction
Avoidance of stimuli, detachment, inability to recall
Negative thoughts or mood associated with the event
I month had to pass since trauma in order to get diagnosis
One subtype: delayed onset → could be years after the trauma
Moral injury
The trauma is going against your own value
More complicated emotionally (shame, guilt, societal scrutiny)
Hard to gear these people towards treatment
Hyacinth fellowship → for those who had accidentally killed/injured someone
Maryann Gray
Social support
Protective factor → loneliness can make it more likely to develop PTSD
Neurological predisposition to PTSD
Genetic factors predispose individuals to be easily stressed and anxious, which then may make it more likely that a traumatic experience will result in PTSD
Shown in study of female undergraduates who witnessed a shooting, specific characteristics of what is referred to as the serotonin transporter gene involving two short alleles (SS) described as increasing the probability of becoming depressed also increased the probability of experiencing symptoms of acute stress after the shooting, even though other factors such as amount of exposure to the shooting were equalized
Elevated/restricted CRF → heightened activity in HPA axis
Damaged hippocampus
Treatment for PTSD
Forced debriefings might be harmful → need to feel more autonomous
Imaginal exposure gaining traction
Virtual reality being explored
EMDR: controversial as to long term efficacy, but no known harms
Protocol where as someone talks about their trauma - moves eyes in specific patterns, triggering different brain activity
How much does eye movement really matter?
Tetris → data that playing after trauma might prevent traumatic injury and development of PTSD → change how we encode memory
Other in trauma-stressor-related category
Reactive attachment disorder (children) → trouble with attaching
Disinhibited social engagement disorder → too easily attached
Acute stress disorder → not yet reached the 1 month mark
Somatic symptom disorder
Somatic symptoms present, creating high anxiety
Illness anxiety disorder
Preoccupation with having or acquiring a serious illness
Somatic symptoms not present, or are just mild
Hypochondriasis would now fit here
In class exercise regarding anxiety
Gave a list of words → had a choice to chose a threatening versus non-threatening choices
Example of kinds of ways we can measure threat sensitivity
However there are many confounds
Somatic symptom disorder criteria
Presence of one or more somatic symptoms
Symptoms are often medically unexplained
Excessive thoughts, feelings, and behaviors related to symptoms (e.g. excessive thoughts about seriousness of symptoms, frequent complaints, requests for help, health-related anxiety, excessive research)
Substantial impairment in social/occupational functioning
Research to date is limited due to recent redefinition of disorder in DSM-5
Statistics of somatic symptom disorder
Relatively rare condition
Onset is usually in adolescence
More likely to affect unmarried low socioeconomic status women
Runs a chronic course
Illness anxiety disorder criteria
Very similar to DSM-IV hypochondriasis
Clinical description:
Severe anxiety about the possibility of having/acquiring a serious disease
Actual symptoms are either mild or absent
Strong disease conviction
Medical reassurance does not seem to help
Illness anxiety disorder statistics
Affects approximately 1-7% of the general population
Affects all ages approximately equally
Often co-morbid with anxiety mood disorders
Culturally specific disorders
Dhat: symptoms (e.g. dizziness, fatigue) attributed to semen loss in some Indian cultures
Kyol goeu or khyal: “wind overload” among khmer people of Cambodia
Fear that wind cannot circulate effectively through body
Dizziness, weakness, fatigue, trembling are seen as signs of illness
Etiology → somatic symptom/related disorder
Consistent overreaction of physical signs/sensations
Cause is unlikely to be found in isolated biological and psychological factors
Genetic component is present
May have learned from family to focus anxiety on physical sensations
Other factors:
Illness in family during childhood
Stressful life events
Benefits of illness
Conversion disorder (functional neurological symptom disorder)
One or more symptoms of altered voluntary motor or sensory function
Symptoms do not match established medical conditions
Not better explained by another mental or medical disorder
Causes significant impairment or distress
Ex: suddenly cannot see
Factitious disorder
Manufacturing symptoms
Need to distinguish from malingering
Faking, but no clear external motivation, sick role perhaps
Might be internal motivation
Munchausen syndrome:
By proxy is most common → doing it someone else
Person physically creates the symptoms themselves
Ex: putting stuff on skin to create lesions
Ex: gypsy rose blanchard → made to believe she was paralyzed and had a terminal illness
Malingering
Not a psych disorder
Ex: want to win a lawsuit so you will say you have PTSD
External motivation
Development of hypochondriasis

Freuds belief about etiology → conversion disorder
Four basic process:
1: individual experiments a traumatic event (unacceptable, unconscious conflict)
2. Because the conflict and the resulting anxiety are unacceptable, the person represses the conflict, making it unconscious
3. The anxiety continues to increase and threatens to emerge into consciousness, and the person “converts” it into physical symptoms, thereby relieving the pressure of having to deal directly with the conflict
The reduction of anxiety is considered to be the primary gain or reinforcing event that maintains the conversion symptom
4. The individual receives greatly increased attention and sympathy from loved ones and may also be allowed to avoid a difficult situation or task
Freud considered such attention or avoidance to be the secondary gain, the secondarily reinforcing set of events
What was freud right and wrong about
Correct on three counts but not on the fourth, although firm evidence supporting any of these ideas is sparse and Freud’s views were far more complex
Getting sick on purpose is also unacceptable, so this motivation is detached from the person’s consciousness
Because the conversion symptoms is successful to an extent in obliterating the traumatic situation, the behavior continues until the underlying problem is resolved
Freud thought that because symptoms reflected an unconscious attempt to resolve a conflict, the patient would not be upset by them
But there is little empirical evidence to support, and many actually show depression and anxiety
Social and cultural influences → conversion disorder
Tend to occur in less educated, lower socioeconomic groups where knowledge about disease and medical illness is not well developed
Incidence of these disorders has decreased over the decades
Most likely explanation is that increased knowledge of the real causes of physical problems by both patients and loved ones eliminates much of the possibility of secondary gain so important in these disorders
Treatment → conversion disorder
Identify and attend to the traumatic or stressful life event if it still present (either in real life or in memory)
Work to reduce any reinforcing or supportive consequences of conversion symptoms (secondary gain)
In class exercise → body sensations
Told to mark down what you noticed in your body in one minute
Shows that attention matters
Hyper focus on bodily sensations
Hypersensivity to threats
Different than being mindful → no negative interpretation
Dissociation
Detaching, zoning out, not fully there, normal to a point
Dissociative identity disorder
Not schizophrenia
Representation in popculture
Etiology: severe childhood trauma
“scab” metaphor
As a way to not have an open wound anymore
Perhaps an extreme version of PTSD
Involves high levels of suggestibility
Alters: other identities
Typically a host alter → might not be original identity
Some involuntarily bodily actions might change
Likely connected to dissociation as a whole
False memory syndrome
Memories can be planted, sometimes inadvertently
Even the way questions are asked - suggestibility
Source monitoring error:
Specific cognitive error when someone remembers information correctly, but no not remember where it came from
In context of DID, have to be careful of childhood trauma, law reinforcement
Other dissociative disorder
Depersonalization - derealization disorder:
No drugs or substance
People slipping into states → distressing/cannot control
Dissociative amnesia:
No traumatic brain injury, no organic cause
Cannot remember or learn new information
Dissociative fugue: (now subtype of dissociative amnesia)
You traveled, do not remember how you got there
Psychosis
Delusions and hallucinations
Positive symptoms of schizophrenia
Delusions:
Grandeur → elevated sense of self
Persecution → paranoia, people are out to get you, idea of gang stalking
Capgras → people believe their loved ones were replaced by a double
Cotards → bodily delusions, ex: believe they are dead or believe they are missing an arm
Hallucinations
Auditory is most common
Can also be visual, taste, smell, tactile…
Negative symptoms of schizophrenia
Avolition → lost energy
Apathy → lack of caring
Alogia → absence of speech
Anhedonia → absence of pleasure
Affective flattening → not facial expressions, completely monotone, everything is compressed (emotional expression)
Disorganized symptoms
Disorganized speech → not making sense, word salad
Cognitive slippage → losing train of thought
Tangentiality → leaping from one thing to another
Loose associations → unclear connections
Inappropriate affect → ex: laughing at upset news
Catatonia → not moving, speaking, reacting
Echolalia: repeating what someone else does
Waxy rigidity → can move muscles, but harden in certain poses
Prodromal stage
Period before diagnosis where things started to get strange, but does not meet criteria
Adolescent/early teen years → bring genetic predispositions out
Psychotic break: when someone becomes truly detached from reality
Findings from SPECT studies
Neuroimaging shows that the part of the brain most active during auditory hallucinations is Broca’s area
Involved in speech production (not comprehension)
Having thoughts → instead of speaking, they hear them
Onset and prevalence of schizophrenia worldwide
About 0.2% to 1.5% (or about 1% of population)
Often develops in early adulthood
Can emerge at any time: childhood cases are extremely rare but not unheard of
Important points regarding schizophrenia
Schizophrenia covers a wide range of symptoms; two different people might have very different behaviors
In fact, new research into genetic markers may indicate eight distinct disorders
Medication treatment needed for psychotic symptoms, but side effects can be problematic
Homeless is common
Risk of violence is very exaggerated in media
Schizophrenia is generally chronic
Most suffer with moderate to sever lifetime impairment
Life expectancy risk for suicide
Increased risk for accidents
Self care may be poorer
What was schizophrenia previously divided into
Subtypes based on content on psychosis
This is no longer the case in DSM-5, but outdated terms are still in partial use
Included paranoid, catatonic, residual (minor symptoms persists after past episode), disorganized (many disorganized symptoms) and undifferentiated
Other psychotic disorders
Schizophreniform disorder
Schizoaffective disorder
Delusional disorder
Brief psychotic disorder
Attenuated psychosis syndrome
Schizophreniform disorder
Psychotic symptoms lasting between 1-6 months
>6 = schizophrenia
Associated with relatively good functioning
Most patients resume normal lives
Lifetime prevalence: approximately 0.2%
Schizoaffective disorder
Symptoms of schizophrenia and who exhibited the characteristics of mood disorders (for example, depression or bipolar disorder)
In addition to the presence of a mood disorder, delusions or hallucinations for at least two weeks in the absence of prominent mood symptoms
Such persons do not tend to get better on their own
Delusional disorder
Delusions: beliefs that are not generally held by other members of a society
Persistent belief that is contrary to reality, in the absence of other characteristics of schizophrenia
Persistent delusion that is not a result of an organic factor (such as brain seizures) or of any sever psychosis
Tend not to have flat affect, anhedonia, or other negative symptoms o schizophrenia, but they may become socially isolated because they are suspicious of others
The delusions are often long-standing. sometimes persisting over several years
Delusional subtypes
Erotomanic
Irrational belief that one is loved by another person, usually of higher status
Grandiose
Believing in one’s inflated worth, power, knowledge, identity, or special relationship to a deity or a famous person
Jealous
Believes sexual partner is unfaithful
Persecutory
Believing oneself (or someone else) is being malevolently treated in some way
Somatic
Person feels afflicted by a physical defect or a general medical condition
Separate delusional disorder
Condition in which an individual develops delusions simply as a result of a close relationship with a delusional individual
Content and nature of the delusion originate with the partner and can range from the relatively bizarre to the fairly ordinary
Brief psychotic disorder
Characterized by the presence of one or more positive symptoms such as delusions, hallucinations, or disorganized speech or behavior lasting one month or less
Often precipitated by extremely stressful situations
Attenuated psychosis syndrome
Disorder involving the onset of psychotic symptoms such as hallucinations and delusions, which puts a person at high risk for schizophrenia
Schizophrenia etiology
Multiple gene variances combine to produce vulnerability
Frank Kallmann published major study of the families of people with schizophrenia
Severity of the parent’s disorder influenced the likelihood of the child having schizophrenia
All forms of schizophrenia were seen within the families (you may inherit a general predisposition for schizophrenia that manifests in the same form or differently from that of your parent)
You have the greatest chance of having schizophrenia if it has affected your identical twin
Quadruplet studies → outcomes all differed
Presence of de novo mutations in family members (mutation in germ cell)
Appears to be a protective factor if children are brought up in healthy supportive homes
Can still pass on the genes to children as carrier
Acute and permanent side effects are common with first generation meds
Parkinson’s like side effects
Tardive dyskinesia
Compliance with medication if often a problem
Aversion to side effects
Financial cost
Poor relationship with doctors
New directions: Avatar therapy
Avatars → patients interact with a digital embodiment of their auditory hallucination, represented by a computer-generated face, with a personalized series of dialogues
Patients can customize how the face looks and sounds
Therapist helps the process, can be empowering for the patient
Psychological treatment of schizophrenia
Illness management/recovery
Engages patient as an active participant in care
Continuous goal setting and tracking
Modules include: social skills training, stress management, substance use issues addressed
Depression
“Slowing down”
Most of the day, nearly everyday
At least two weeks - will be diagnosed with major depression disorder - also a building block
Cognitive symptoms:
Thought processes
Sense of worthlessness, hopelessness, helplessness, difficulty making decisions, concentrating
Disturbed physical function:
Eating, sleeping (either too much or too little
Emotional symptoms - anhedonia (this is key):
Sadness, loss of pleasure, feeling numb, irritable
“unable to engage with the fabric of life”
Mania
Opposite pole of depression
High energy and motivation
Nervous system turned up
Only needs to last one week to meet criteria (even less if hospitalized)
Manic episode is typically a building block → body crashes afterward
“Marriage plot” → good representation of mania in fiction, feels good in the moment
Typical signs of mania
Hyperactivity
Grandiose plans, ex: max out credit card
Rapid speech, flight of ideas
Impulsivity - where danger might come in
Irritability - especially near end of manic episode
Difficulty sleeping, concentrating, staying still
Writing really fast
Increased fights, alcohol consumption, productivity, creativity, sex, appetite, sensitivity, noise, driving dangerously
Poor judgment
Hypomania
Not itself a disorder
Low level of mania
Does not cause marked impairment in functioning
Building block
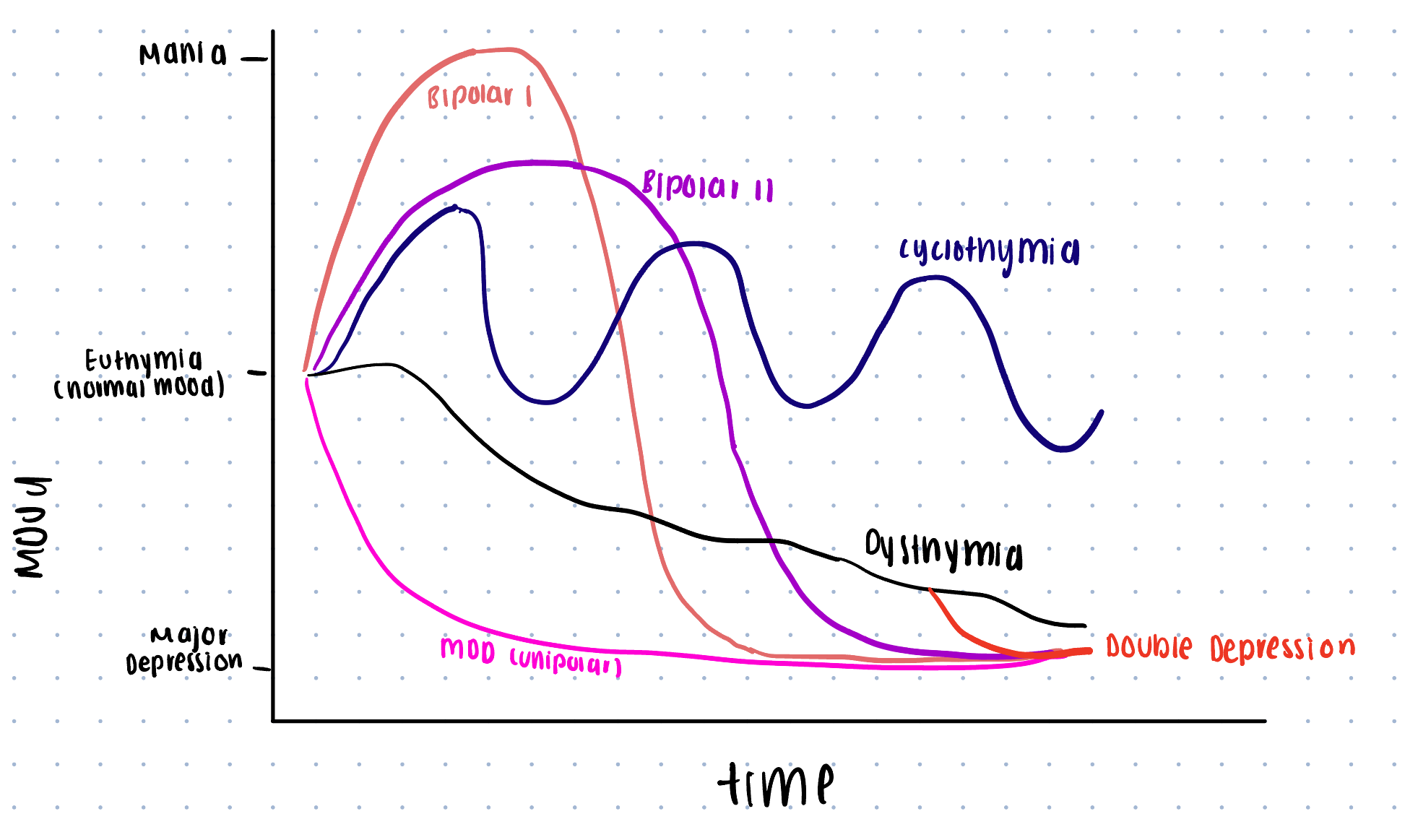
Unipolar vs. Bipolar (just name types)
Bipolar I
Bipolar II
Cyclothymia
Dysthymia
Double depression
Bipolar I
Full mania and full depression
Bipolar II
Hypomania and full depression
Cyclothymia
Chronic cycles of hypomania and mild depression; few periods of euthymia (never exist normally) (at least two years)
Dysthymia (persistent depressive disorder)
Chronic mild depression, 2 years or longer
Double depression
Major depressive disorder episode on top of baseline of persistent depressive disorder
Higher risk of suicide
Graph of unipolar vs bipolar
Case study of persistent depressive disorder
1st year student with roommate problems
“Laura” → flat affect
No sadness or irritability
No autism
She did not meet criteria for major depressive disorder
Emptiness to her, nothing there, does not really care, not getting excited about things, zero typical emotional functioning
Needed to find something to giver her a spark → had her be open to exploration
Gradually realized, one time she felt something was when she was with animals
Changed major, volunteering, started to build a life
She had never felt typical, but still had a meaningful life
Kids: DMDD (disruptive mood dysregulation disorder) vs bipolar
Constantly diagnosed bipolar as kids → medicated incorrectly
Did not have bipolar disorder
Cannot regulate mood → really worked up
More tailored treatment now
Premenstrual dysphoric disorder (new to DSM)
Significant depressive symptoms occurring prior to menses during majority of cycles, leading to distress and impairment
Controversial:
Advantage: legitimizes difficulties people face
Disadvantage: pathologies an experience many consider to be normal
Mood disorders across US subcultures
Similar prevalence among US subcultures but experience of symptoms may vary
E.g. some cultures are more likely to express depression as somatic concern
Higher prevalence among Native Americans: 4x rate of general population
Genetic contributions to mood disorders
Twin studies:
Concordance rates high in identical twins
2-3 times more likely to present with mood disorders than fraternal twin of a depressed co-twin\
Severe mood disorders have strong genetic contribution
Heritability rates are higher for females compared to males
Some genetic factors confer risk for both anxiety and depression
Neurobiological influences - mood disorders (name them)
Neurotransmitter systems
Endocrine system
Sleep disturbance
Neurotransmitter systems - mood disorders
Serotonin and its relation to other neurotransmitters
Serotonin regulates norepinephrine and dopamine
Mood disorders are related to low levels of serotonin
Permissive hypothesis: low serotonin “permits” other neurotransmitters to vary more widely, increasing vulnerability to depression
Endocrine system - mood disorders
Elevated cortisol
Stress hormones decrease neurogenesis in the hippocampus: less able to make new neurons
Sleep disturbance
Hallmark of most mood disorder
Depressed patients have more intense REM sleep (less time in restful stage) and go into it more quickly
Sleep deprivation may temporarily improve depressive symptoms in bipolar patients - some causal effect
Psychological etiology of depression
Stress, trauma, context of memories
Reciprocal gene-environment model
Cognitive errors (Aaron Beck)
Overgeneralization → one thing wrong, everything is bad
Arbitrary inference → idea that two things are connected through arbitrary inference
Depressed thoughts becoming “sticky”
Ruminating, cycling
Learned helplessness
Do not confuse with overcoming societal barriers
Martin selgman to explain findings
Learning under stress → dogs
Mild shock - run a maze, some would just stop trying
Martin Selgman’s “Depressed Attributional Style”
Could be considered symptomology/etiology
3 ways of thinking (cognitive, about negative things, cognitive distortions) in depressed people:
Internal → internal causes to bad things
“It’s me”
Can measure this distortion in a lab
Global → about everything
Mountains out of mole hills
Similar to overgeneralization
Stable → believe things will not change
Ex: fail a test, think you will never improve
Role of attention
Ex: selective attention test → gorilla example shown in class
What you pay attention to dictates what evidence you have
Social and cultural etiology of depression
Gender imbalances - genetic, environmental, or both?
Social support - can become a cycle
Martial satisfaction - particularly in men
Emotional and support needs in marriage basket, less outside marriage
After divorce, men tend to get remarried quicker
Societal stressors: trauma, poverty, job less, etc.
Integrative theory of etiology
Biological and psychological vulnerabilities interact with stressful life events to cause depression
Biological vulnerability: e.g. overactive neurobiological response to stress
Psychological vulnerability: e.g., depressive cognitive style
8 specifies to describe depressive disorders
With psychotic features (mood-congruent or mood-incongruent)
Hallucinations, delusions, somatic delusions
With anxious distress (mild to severe)
Makes suicidal thoughts and fatal suicide a more severe condition
With mixed features
At least three symptoms of mania
With melancholic features
Most severe somatic symptoms, like weight loss, low sex drive, anhedonia
With atypical features
Consistently oversleep, overeat (higher incidence of diabetes)
With catatonic features
Absence of movement (catalepsy)
With peripartum onset
Peri: surrounding
Period of time just before and after birth
Manic episodes important to recognize
Present with fathers too
CBT and interpersonal therapy
More minor: baby blues
Difficulty understanding why they are depressed
Rapid decline in reproductive hormones
With season pattern
SAD
Late fall - beginning spring
Must have occurred for at least two years with no evidence of nonseasonal major depressive episodes
Excessive sleep, increased appetite/weight gain
Changes of melatonin production (increase in winter)
Circadian rhythm misaligned
Integrated grief vs complicated grief
Integrated grief: grief that evolves from acute grief into a condition in which the individual accepts the finality of death and adjusts to the loss
Complicated grief: associated with activation of dopamine neurotransmitter system
After 6 months
Suicidal thoughts increase substantially
Areas of brain associated with close relationships and attachment are active in grieving people, in addition to areas of brain associated with more general emotional responding
Prolonged grief disorder
Stress and depression
Dependent on context, even with same stressful life event, context might make things worse
Also dependent on meaning → how the person sees the stressor
One crucial issue is the bias inherent in remembering events
Current moods distort memories
Only useful way to study stressful life events is to follow people prospectively to determine more accurately the precise nature of events and their relation to subsequent psychopathology
Humiliation, loss, and social rejection are the most potent stressful life events that likely lead to depression
Gene-environment correlation model
Parenting styles and rigid gender roles
Parenting styles encouraging stereotypic gender roles are implicated in the development of early psychological vulnerability to later depression or anxiety
Specifically, a smothering, overprotective style that prevents the child from developing initiative
“Sudden surge” in depression among girls that occurs during puberty
Younger girls just entering a new school find it stressful and girls who mature early physically have more distress and depression
Women place greater value on intimate relationships
Women ruminate more and blame themselvesTr
Treatment for depression
Therapy
Can alter neurobiology
Risk of medication only - mood disorders
“Bandaid effect”
Higher risk of relapse
No one monitoring side effects
Not giving a sense of autonomy that you can get through it yourself
Not changing the thoughts/behavior that need to be changed
Common types of therapy - mood disorders
CBT
Psychodynamic psychotherapy - relationships/attachments - deep history
Interpersonal psychotherapy - relationships
Existential therapy - search for meaning
Algerian therapy - looking at barriers and assessment of yourself
Gestalt therapy - how you fit into the world around you
New directions branching off CBT
Acceptance and commitment therapy (ACT):
Mindfulness and accepting and moving on from thoughts rather than fighting them
“Happiness trap”: is a great primer on this
Diffuse → sense of separation
Antidepressant medication (not 1st line of defense)
Tricyclics (rise of overdoses)
MAOIs (MAO inhibitors) - lifestyle annoyances and side effects
SSRIs (1st line of defense)
Selective serotonin reuptake inhibitors
General sexual side effects
Zoloft
Paxil
Prozac
Celexa
Lexapro
SNRIs
Mixed reuptake inhibitors: act on norepinephrine and dopamine as well
Wellbutrin (zyban)
Pristiq
Effexor
TMS
Transcranical magnetic stimulation)
Magnets on outside of head
Decent data on helpfulness
Reset neural pathways
Might have more side effects
Usually do meds first
Newer directions for treatment of mood disorders
Esketamine (nasal administered ketamine) and also ketamine infusions
Psychodelics - psilocybin, MDMA
The environment matters a lot, need to be guided
Some try micro-dosing
Not a good control, if you are high you know you are high
Gut bacteria - high fibers, fermented, no sugar or salt or processed foods
Modified ECT (electroconvulsive therapy which is very invasive)
More localized
Resetting neural pathways
Deep brain stimulation
Invasive
Electrode in localized area
Treatment for bipolar disorder
Lithium
Other mood stabilizers
Med (usually lithium) is still first line of defense
Psychotherapy helpful in managing the problems (e.g. interpersonal, occupational) that accompany bipolar disorder
Family therapy can be helpful
Suicide stats
More than homicides
3:2 in US
1100 per year on college campuses
4/5 young adults give clear warnings
Second leading cause of death among college students
May even be underreported