Intro to Bacteria
1/188
Earn XP
Description and Tags
Year 1 - Semester 1
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
189 Terms
types of infectious pathogen
prions, viruses, bacteria, fungi, parasites
virus
a fragment of genetic code within a protective shell of proteins or membrane which uses host cell transcription and translation machinery for replication
mycoplasma
a type of bacteria that doesn’t have a cell wall (pleomorphic) making it the smallest replicating organism, lives off live or dead organisms (parasitic/saprophytic) as they require external supply of cholesterol, amino acids and fatty acids
typical structures found in prokaryotic cells
cell wall, cell membrane, cytoplasm, nuclear region
functions of bacterial plasma membrane
transport of nutrients, energy generation, secretion, synthesis of peptidoglycan, contains regulatory proteins
peptidoglycan
a polysaccharide backbone linked by peptide bridges that forms bacterial cell walls, penicillin will bind to it
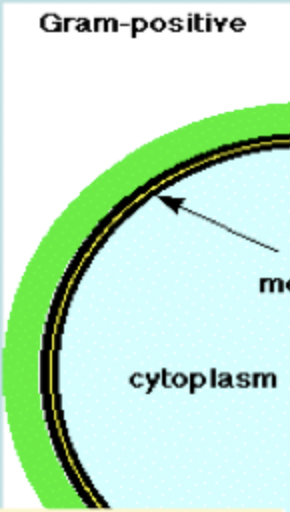
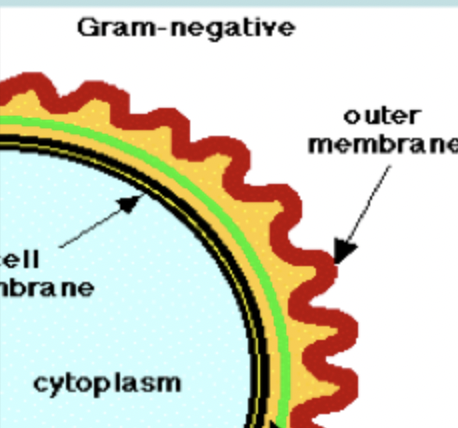
main groups of bacteria based on cell wall structure
gram-positive and gram-negative
gram-positive bacteria
a group of bacteria characterized by a thick cell wall made of peptidoglycan that retains a violet color after being stained with crystal violet in the Gram stain test
gram-negative bacteria
bacteria with a distinctive cell envelope with a thin peptidoglycan layer situated between an inner cytoplasmic membrane and an outer membrane (so peptidoglycan isn’t outer layer) that do not retain the crystal violet stain used in the Gram staining method of bacterial differentiation
acid-fast organisms
microbes that have a waxy cell wall that protects them from acids, alkalis and digestion in phagocytes and impedes the entry of molecules (bacteria contain mycolic acid)
pyrogenic
causes an inflammatory response resulting in a fever
endotoxins
lipopolysaccharides found in the outer membrane of gram-negative bacteria that can trigger a severe immune response, they are released when bacteria die
structures found on the surface of bacterial cells
flagella, fimbriae, pili, capsules
bacterial chemotaxis
bacteria sense a stimulus and switch flagella on and move towards the stimulus so that they can make use of it
what are flagella made of?
protein subunits called flagellin
fimbriae and pili
hair-like structures on the surface of bacterial cells which allow attachment to surfaces, bacterial conjugation and twitching motility
true bacterial capsule
a discrete detectable layer of polysaccharides deposited outside the cell wall
bacterial slime layer
a less discrete structure or matrix which embeds bacterial cells
how is bacterial genotypic classification determined?
entire genome, ribosomal rRNA sequences, DNA hybridisation, multilocus sequence typing
how is phenotypic bacterial classification determined?
cell morphology, physical characteristics, biochemical reactions, culture properties, oxygen requirements
function of porin proteins in bacterial cells
they form pores on the surface of the outer cell membrane which allows nutrients to diffuse into the cell from outside
phases of bacterial growth
lag, exponential growth, stationary, decline
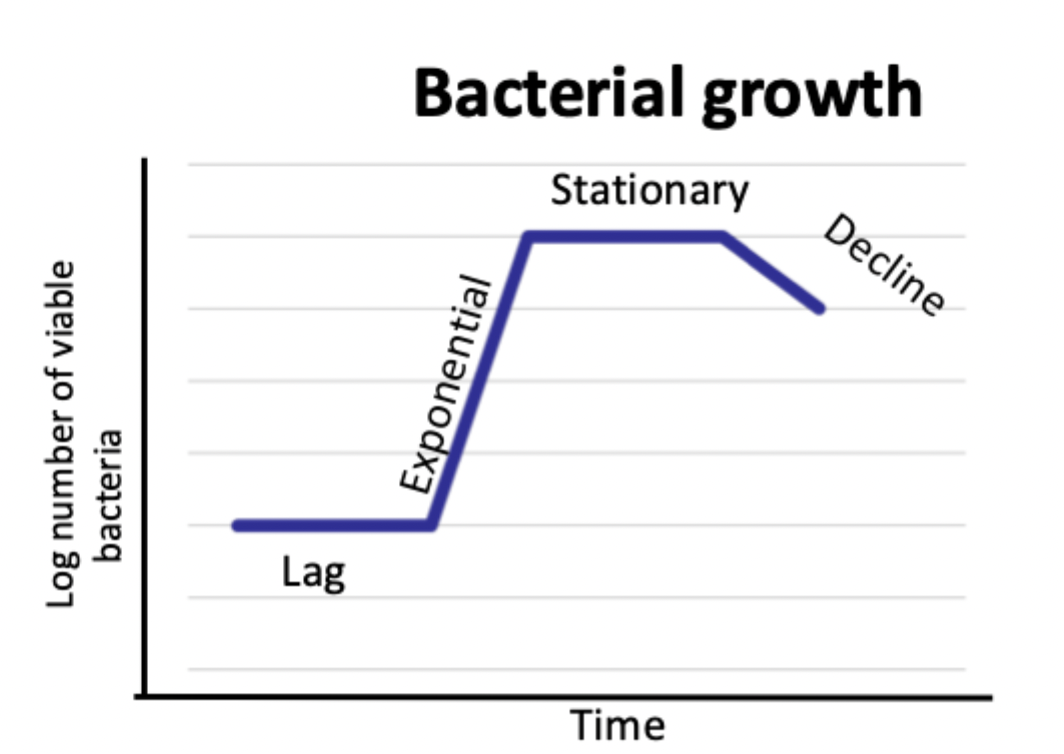
lag phase of bacterial growth
after inoculation metabolism is required to acquire essential constituents in order to divide
exponential phase of bacterial growth
binary fission causes exponential increase
stationary phase of bacterial growth
essential nutrients are depleted and toxic metabolic products accumulate in the media, competition causes some bacteria to die off
decline phase of bacterial growth
old cells die rapidly followed by young
ways to count bacteria
microscopic counting, colony counting, opacity, turbidity
bacterial enumeration via microscopic counting
an arbitrary number of fields are counted from a direct fixed smear within a counting chamber
bacterial enumeration via colony counting
serial dilution are made and a fixed volume is spread on each plate and incubated, the number of colonies is counted
heterotroph
an organism that uses pre-formed organic compounds for energy
autotroph
an organism that uses carbon dioxide for energy
requirements for bacterial nutrition
large quantities of carbon and nitrogen, peptones in culture media usually provide essential nutrients and C/N, phosphates are essential for nucleic acid production, sulphur is needed in amino acid production, Ca2+, Fe3+, Mg2+ and K+ are important enzyme co-factors
microbial responses to nutritional deficiency
extracellular molecules collect nutrients, cells enter semi-starvation state, sporulation and resting cells
defined culture medium
a medium that has known amounts of known chemicals
complex culture medium
a medium whose exact chemical composition is unknown
selective culture medium
a medium that limits the growth of unwanted microbes or alows the growth of desired ones
differential culture medium
a medium that enables differentiation between different microbes
factors that affect bacterial growth
temperature, pH, moisture, atmospheric composition, osmotic pressure
mesophilic
an organism that grows at moderate temperature between 20-45 degrees
microaerophiles
organisms that require oxygen but only in small amounts
aerobes
organisms that use oxygen in metabolism
anaerobes
organisms that can growth without oxygen
types of anaerobes
obligate, aerotolerant, facultative
obligate anaerobes
organisms that are killed or inhibited by oxygen
aerotolerant anaerobes
organisms that don’t use oxygen but are not killed by it
facultative anaerobes
organisms that can grow with or without oxygen
why are microorganisms preserved in labs?
to allow vaccine production, for research and teaching
how are microorganisms preserved in a lab?
freezing in liquid nitrogen or with a cryoprotectant or desiccation (freeze drying and storing as ampoules in the dark)
aseptic technique
a technique that prevents microbial contamination of cultures or wounds
sepsis
microbial contamination
asepsis
absence of significant contamination
antimicrobial chemicals
substances expected to destroy pathogens but not to achieve sterilisation
disinfectant
an antimicrobial used on inanimate objects
antiseptic
an antimicrobial used on living tissue
disinfection
the destruction of microorganisms by direct exposure to chemical or physical agents
sterilisation
destroying all microbial life on lab and surgical procedures
antisepsis
when chemicals are applied to body surfaces to destroy/inhibit pathogens
bacteriostatic
inhibits bacterial reproduction
factors that affect the efficacy of microbial inactivation
type of microbe, life cycle phase, presence of organic matter, number of microbes present, exposure time, working concentration
physical methods for microbial inactivation
refrigeration, freezing, boiling, vacuum packing, pasteurisation, filtration, radiation
flash pasteurisation
heating a substance to 72 degrees for 15 seconds (high temp short time)
ultra high temp pasteurisation
heating a substance to 140 degrees for 1 second, sterilises product but can affect taste
thermal death point
lowest temperature at which all microbes in a liquid suspension will be killed in 10 mins
thermal death time
minimum length of time in which all bacterial will be killed at a given temperature
decimal reduction time
time taken for 90% of bacteria at a given temperature to be killed
what is the most resistant type of microbe?
prions
what is the least resistant type of microbe?
viruses with lipid envelopes
autoclave
steaming under pressure to improve sterilisation as steam can directly contact material
features of moist heat sterilisation
denatures proteins, steam can reach higher temperature so more effective, steam must directly contact material to sterilise it
dry heat sterilisation methods
direct flaming, incineration, hot-air sterilisation
is filtration effective at removing viruses?
no, because they are too small
types of radiation used for sterilisation
gamma radiation and ultraviolet light
chemical methods for microbial inactivation
disinfectants, detergents, acidification, sulfur dioxide, increasing osmotic pressure
how does increasing osmotic pressure prevent food spoilage?
water is drawn out of cells which causes them to become dehydrates or die
how does sulphur dioxide prevent food spoilage?
acts as a reductant and antibacterial
acidic-anionic detergents
detergents where the anion reacts with the plasma membrane of cells
cationic detergents
detergents made of quaternary ammonium compounds which are strongly bactericidal
types of disinfectants
surfactants, phenols/phenolics, halogens, alcohols, heavy metals
features of phenol disinfectants
skin irritant, strong odour, acts as local anaesthetic
features of phenolic disinfectants
effective against gram-positive bacteria, they destroy plasma membranes and denature proteins
features of chlorine disinfectants
oxidising agents, widely used, form bleach with water, fair sporicidal activity, used in pools and drinking water
features of iodine disinfectants
more reactive and germicidal, alters protein synthesis and membranes, wound antiseptic when mixed with alcohol, form detergent complexes with organic molecules
features of alcohol disinfectants
killd bacteria and fungi but not endospores or naked viruses, denature proteins and disrupt plasma membranes, evaporate so don’t leave a residue, used to mechanically wip microbes off skin, not good for open wounds as they coagulate proteins
features of heavy metal disinfectants
toxic as metal ions combine with sulfhydryl groups to denature proteins
when are copper disinfectants used?
to kill algae in pools and fish tanks and in dairy cow footbaths
pathogen
a microbe that causes harm to the host
commensal
a microbe that lives on/in the host without causing harm
saprophyte
a microorganism that feeds on and decomposes dead organic material
infection
the colonisation of a host by microorganisms that have the potential to cause disease
pathogenesis of a disease
the biological mechanisms that lead to the diseased state
virulence
the relative ability of a pathogen to cause disease in the host
opportunistic pathogen
a microorganism that can be part of the normal flora but may be harmful if it moves from one part of the body to another
strict pathogen
a microorganism always associated with disease
2 main parts of bacterial pathogenesis
bacterial virulence factors that damage/alter host cells and tissues, host response
steps of bacterial pathogenesis
exposure to pathogen
pathogen adheres to skin or mucosa
pathogen invades through epithelium
pathogen colonises, grows and produces virulence factors
further growth of pathogen at original and distal sites
further interaction of virulence factor with host molecules causes damage
features of a pathogen that determines pathogenesis
virulence, environmental stability, route of entry, infective dose, tissue tropism, susceptibility to host defence, interaction with other pathogens
features of host that determine pathogenesis
species, breed, age, sex, genetic factors, physiological factors, immune competence
2 main types of virulence factors
factors that promote colonisation of host and factors that cause damage to the host
Koch’s postulates
four criteria developed by Robert Koch to establish a specific microbe as the cause of a specific infectious disease
microbe is found in all cases and all sites of the disease
microbe is isolated from infected persons and maintained in pure culture
pure cultured microbe causes symptoms of disease on inoculation
microbe is re-isolated from intentionally infected host