DIG Exam 3 ILA Eating Disorders Hundley
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
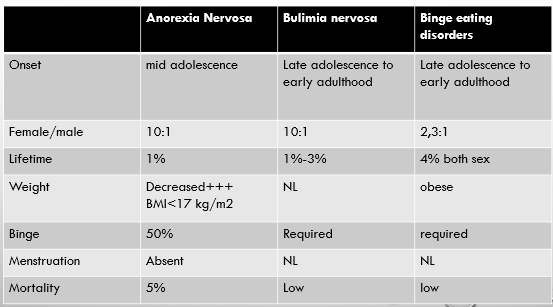
____-__% of anorexia patients die of medical complications annually
2-10
The mortality rate for anorexia is __x higher than the mortality rate of all other causes of death of adolescent girls and young women
12
Weight less than the minimum normal range for age and height
Fear of gaining weight or becoming fat despite being underweight
Disturbance in the way one’s body weight or shape is perceived
Excessive influence of body weight or shape on self-evaluation
Most common in adolescent/young adult females
Anorexia
Recurrent episodes of binge eating
Recurrent inappropriate compensatory behaviors aimed at preventing weight gain
Self-evaluation unduly influenced by body shape and weight
Bulemia
Recurrent episodes of eating large amount of food in brief period with sense of loss of control and marked distress
Binge Eating disorder
Presents in 0.5% adolescents and young adults
Male:female 1:3 to 1:12
Presents in 5% adolescents and young adults
Male:female 1:3 to 1:18
Presents in 1-4% adolescents and young adults
Male:female 1:2 to 1:6
Anorexia
Bulimia
Binge eating disorder
Do you ever make yourself sick because you feel uncomfortably full?
Do you worry you have lost Control over how much you eat?
Have you recently lost more than one stone (14 lbs) in 3 month period?
Do you believe you are fat when others say you are too thin?
Would you say that Food dominates your life?
1 point per yes, 2 or more indicates probable disordered eating
Scoff questionnaire
Non-specific complaints
Lethargy
Dizziness
Dysthymia
Anxiety
Amenorrhea
Presentation of eating disorder
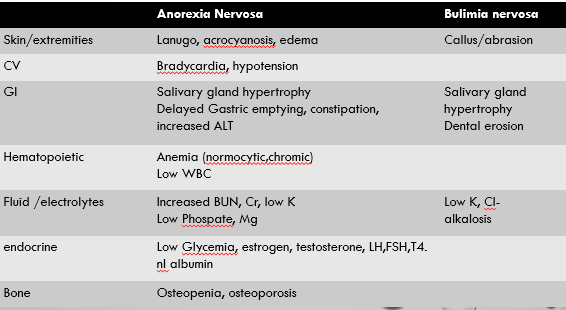
Physical Findings
Vital sign abnormalities
Exercise induced injury
Hair loss
Lanugo hair
Dental Erosions and caries
Parotid inflammation
Russell sign
Dehydration
Presentation of eating disorder
Marked calorie restriction
300-700 cal/day
Compensatory exercise
Restrictive clinical features
May have enormous calorie intake (>20,000 cal)
May have normal meal with excessive guilt
Binging clinical features
Chronic Emesis
Electrolyte disturbances
Dehydration
Parotitis
Esophogeal injury
Ipecac – potentially irreversible cardiac dysfunction
Purging clinical features
Melanosis Coli
Chronic laxative abuse clinical feature


Dental erosion and caries

Lanugo hair

Parotid inflammation
Major Depression – 50-75%
Anxiety - 60%
OCD - 40%
EtOh or drugs – 27%
Significant psychiatric co-morbidities
Complete Physical
ECG
Bradycardia
QT prolongation
CBC
Leukopenia
Anemia
CMP
Hypokalemia, Hyponatremia
Hypophosphotemia and Magnesimia
Liver enzyme abnormalities
Hypoalbuminemia
Workup for suspected eating disorder
Depression, anxiety, and social withdrawal, as well as the specific symptoms of disordered eating.
Psychiatric symptoms: irritability, obsessionality, and preoccupation with food may be secondary to semi starvation and may remit with refeeding.
Physical symptoms of semi starvation or malnutrition:
Lanugo, osteopenia or osteoporosis, dehydration, hypothermia, cardiovascular or renal irregularities, gastrointestinal and endocrine disturbances.
changes in neuropsychological functioning.
Laboratory results may be normal, especially in restricting AN, but patients still may be at risk for cardiac events resulting from malnutrition.
Anorexia nervosa signs and symptoms
Binge-eating/purging type: During and off current episode of anorexia nervosa, the person has regularly engaged in binge eating or purging behavior (i.e., self-induced vomiting or the misuse of laxatives, diuretics, or enemas) Self-evaluation is unduly influenced by body shape and weight (DSM5)
Restricting type: without the above behavior.
Types of anorexia nervosa
Depression, anxiety, and social withdrawal, as well as the specific symptoms of disordered eating.
due to purging behavior
dental enamel erosion secondary to vomiting
Finger callus (russell’s signs)
gastrointestinal symptoms (bloating, nausea, vomiting)
salivary gland hypertrophy
electrolyte disturbances (from the vomiting)
Misuse of stimulant laxatives: hypomagnesia or hypophosphatemia
Binge eating is associated with gastric distention and, in rare cases, gastric rupture
Bulimia nervosa signs and symptoms
Purging type: During the current episode of bulimia nervosa, the person has regularly engaged in self-induced vomiting or the misuse of laxatives, diuretics, or enemas.
Nonpurging type: During the current episode of bulimia nervosa, the person has used other inappropriate compensatory behaviors, such as fasting or excessive exercise, but has not regularly engaged in self-induced vomiting or the misuse of laxatives, diuretics, or enemas.
Types of bulimia nervosa
Refusal to maintain body weight at or above a minimally normal weight for age and height (Energy restriction below requirements-DSM 5)
weight loss leading to maintenance of body weight less than 85% of that expected.
Failure to make expected weight gain during period of growth, leading to body weight less than 85% of that expected).
Intense fear of gaining weight or becoming fat even though underweight.
Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight.
In post-menarchal females, amenorrhea, that is, the absence of at least three consecutive menstrual cycles
Diagnostic criteria for anorexia nervosa
Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
Eating, in a discrete period of time (e.g.,within any 2-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances.
A sense of lack of control over eating during the episodes (e.g. ,a feeling that one cannot stop eating or control what or how much one is eating).
Recurrent inappropriate compensatory behavior in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, enemas, or other medications; fasting; or excessive exercise.
The binge eating and inappropriate compensatory behaviors both occur, on average, at least twice a week for 3 months. Self-evaluation is unduly influenced by body shape and weight.
The disturbance does not occur exclusively during episodes of anorexia nervosa
Diagnostic criteria for bulimia nervosa
A 17-year-old teenager is evaluated during an office visit. She is brought in by her mother who is concerned about her focus on diet and weight. The patient states that she believes that she is obese and feels as though she needs to diet to achieve a more appropriate body weight. She also reports exercising on a daily basis to help her lose weight. Dietary history suggests that most of the time she consumes very little food, but at least twice per week she will eat large amounts of high-calorie desserts over the course of 1 to 2 hours. She describes feeling guilty after doing so and will make herself vomit. Medical history is otherwise unremarkable, although she indicates that her menstrual periods are highly irregular.
On physical examination, vital signs are normal. BMI is 23. The parotid glands are enlarged, but the remainder of the examination is unremarkable.
Which of the following is the most likely diagnosis?
Bulimia nervosa
Subspecialty consultation
Pediatrics/Adolescent Medicine
Endocrine
Gastroenterology
Mental Health Providers
Location of therapy depends on severity
Nutritional Rehabilitation
Important in Anorexia
Weight gain Goals
1-1.5 Kg/week inpatient
0.2-0.5 kg/week outpatient
Cognitive Behavioral Therapy
Interrupt problem behaviors
Decrease Concern about body shape and weight
Remission of Binge and Purge 30-50%
Especially successful in Bulimia and BED
Interpersonal Therapy
Recognition of interpersonal problems that contribute to eating disorders
Combines with CBT
Family Based Therapy in adolescents and children
Medications have stronger evidence for bulimia treatment
Treatment of eating disorders
1-1.5 Kg/week __patient
0.2-0.5 kg/week ____patient
in
out
weight gain goals
weight restoration to at least 90% of predicted weight.
restoration of all clinical consequences , hypotension, hair loss, osteopenia)
Goals of treatment
they typically exaggerate their food intake and minimize their symptoms.
Some resort to subterfuge to make their weights appear higher: water-loading before they are weighed.
Example: a 19 year old admitted for bradycardia and hypotension has a BMI of 13k/m2. the next day she has gained 3lbs on a 1000calories per day. What explains this weight gain?
How patients resist weight gain goal
reassure the patient that weight gain will not be permitted to get out of control
weight restoration is medically and psychologically imperative
Physicians job
current weight
the rapidity of recent weight loss
the severity of medical and psychological complications
determinants for intensity of initial treatment
<75% ideal body weight or weight loss despite treatment
Feeding Refusal
Body fat <10%
Vital Signs
Bradycardia (<50 during day, <45 at night)
SBP<90 Temp <35.5
Cardiac
Arrhythmia
Prolonged Qtc
Syncope
Orthostasis
Electrolyte Disturbance
Kcl < 3
Cl < 90
GI manifestations
Hematemesis
Intractable emesis
Esophageal Laceration
Suicidal Ideation
Signs of Hepatic, Renal, or cardiovascular compromise
Admit to hospital
Nutritional restoration can almost always be successfully accomplished by oral feeding
Calories can then be gradually increased to achieve a weight gain of 1–2 kg (2–4 lb) per week, (typically requiring an intake of 3000–4000 kcal/d.)
Much less in adolescents : 300 calories daily above pre treatment caloric level.( which can be as low as 6-700 calories.)
Team: psychiatrists or psychologists experienced in the treatment of AN is usually necessary.
Oral treatment
Antidepressants
Strong evidence of improvement in binge/purge in bulimia
Only Fluoxetine has indication
Bupropion not recommended due to increase risk of seizures in bulimia
Topiramate
Medium quality evidence of benefit in Bulimia
Caution advised secondary to side effect – weight loss
Medication treatment for weight loss specifically bulimia
Naltrexone and ondansetron – __ evidence of efficacy
No
Antidepressants no better than placebo in _____
anorexia
Antidepressants in setting of concurrent depression, no improvement in depression until weight is ______
restored
Small studies with improvement of weight in anorexia
Atypical antipsychotics
Grade A evidence
Imipramine
Topiramate
SSRI (sertraline, citalopram)
Lisdexamfetamine
Patients >18 years
Must monitor for cardiac disease and inadequate intake
Treatment for Binge eating disorder
Life-threatening complication in about 6%
Most common in patients <70kg
Widespread organ dysfunction from failure to make ATP
Longstanding undernutrition depletes phosphorus stores
Insulin secretion shifts phosphorus intracellularly
Hypophosphatemia results in 12-72 hours post re-feeding
Refeeding syndrome
Recommend 1200-1500 cal/day with increase of 500cal/day to goal of 3500 (female) or 4000 (male)cal/day
Refeeding
Peripheral edema
Cardiopulmonary function
GI symptoms including bloating
Refeeding syndrome
Monitor for these during refeeding
Decreased serum potassium
Increase Energy (carbohydrate, Fat and Protein)
increased insulin K+ to shift from extracellular fluid into K+-depleted cells
Decreased serum phosphorus (as the body resumes synthesis of ATP)
Edema related to fluid shifts or congestive heart failure.
Refeeding syndrome
1/3 do well
1/3 revert to disordered eating in times of stress
1/3 chronic relapsing course
Prognosis of eating disorder
Prolonged disease duration
Low Initial Weight
Pre-renal Azotemia
Premorbid obesity
Compulsive Exercise
OCD traits
Conflicting family relationships
Neurotic Personality
Poor prognostic indicators
5X more likely to have premature death
18x more likely to die of suicide
33% recovery in 5 years with standard therapy
50% recovery with FBT
Anorexia
highest mortality of any mental illness
Anorexia
33-66% full recovery by 5 years
Less common mortality – 2X more likely to have premature death
Bulimea
30-80% recovery
No difference in mortality than general population
Complications related to obesity
Binge eating disorder
CBT is the ________ of therapy for these syndromes
cornerstone
20% developed a chronic course of illness.
50% of patients with AN develop bulimic symptoms
better outcomes for adolescent patients, but time to recovery nevertheless may be protracted (5 to 6 years).
Anorexia nervosa outcome
on average, problematic eating behaviors persist for several years in treated patients
most individuals with BN achieve full recovery at some point, but rates of relapse are high (i.e., 35%)
one third of patients continue to exhibit some symptoms.
Bulimia nervosa outcome
comparison
Comparison