PDA toxicology
1/622
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
623 Terms
After assessing the circulation of a patient, what is the next step in the guide to the management of poisoned patients?
a. Assess CNS
b. Identify toxidrome
c. Specific laboratory analysis
d. Alter toxin pharmacokinetics
a. Assess CNS
Select the respiration rate that could be classified as bradypnea
a. 14 rpm
b. 15 rpm
c. 25 rpm
d. none of the above
d. none of the above
Which of the following does NOT cause bradycardia
a. Opioids
b. Anticholinergics
c. B-adrenergic antagonists
d. Baclofen
b. Anticholinergics
The majority of the poisoned patients benefit from gastrointestinal decontamination
a. True
b. False
b. False
What of the following pupil sizes could be classified as mydriasis?
a. 1mm
b. 2mm
c. 4mm
d. 5mm
d. 5mm
Mydriasis can be found in....
a. anticholinergic toxidrome
b. sympathomimetic toxidrome
c. opioid toxidrome
d. A & B
d. A & B
The following group cannot cause a sympathomimetic toxidrome
a. Amphetamines
b. Cocaine
c. Bath salts
d. tricyclic antidepressants
d. tricyclic antidepressants
Benzodiazepines can be used to treat seizures, agitation, and ethanol withdrawal syndrome
a. True
b. False
a. True
What is the definition of toxicokinetics
a. study of absorption, distribution, metabolism, and excretion of xenobiotics
b. term used to describe the relationship between xenobiotic conc and symptoms
c. study of absorption, distribution metabolism and excretion of toxic agents
d. study of toxic concentration of xenobiotics and clinical effects
c. study of absorption, distribution metabolism and excretion of toxic agents
Rate the following from fastest to slowest absorption
a. IV
b. Inhalation
c. IM
d. Oral
a. IV, b. Inhalation, c. IM, d. Oral
Difference between the concentrations of the xenobiotic on the opposing sides of the membrane
a. passive diffusion
b. facilitated diffusion
c. active transport
d. endocytosis
a. passive diffusion
The pH, motility, and blood flow of the stomach are factors influencing absorption
a. True
b. False
a. True
Absorption is the amount of xenobiotic that reaches the systemic circulation unchanged
a. True
b. False
b. False
A large volume of distribution means the drug is highly concentrated in the bloodstream
a. True
b. False
b. False
Which method can NOT be used in a patient whose airway protective reflexes are lost and is not intubated
a. gastric emptying and orogastric lavage
b. Multiple-dose activated charcoal
c. activated charcoal
d. None of them can be used
d. None of them can be used
What is the recommended dose of activated charcoal to prevent absorption?
a. 5mg
b. 50mg
c. 500mg
d. 5g
b. 50mg
What substances can be excreted through urine alkalinization?
a. weak acids
b. weak bases
c. strong bases
d. strong acids
a. weak acids
Hemodialysis is an effective intracorporeal technique to enhance the elimination of xenobiotics
a. True
b. False
b. False
- extracorporeal
What is the most predominant reaction of phase 1
a. Hydrolysis
b. Oxidation
c. Conjugation
d. None of the above
b. Oxidation
Which receptor type is primarily involved in benzodiazepine withdrawal?
a. GABA-A
b. Dopamine Receptor
c. Mu-opioid receptor
d. Beta Adrenergic
a. GABA-A
Which of the following substances can cause cholinergic toxidrome?
a. Organophosphates
b. Cocaine
c. Amphetamines
d. Benzodiazepines
a. Organophosphates
Which receptor is primarily responsible for nicotine's effects on the nervous system?
a. GABA receptor
b. Dopamine receptor
c. Nicotinic acetylcholine receptor
d. Serotonin receptor
c. Nicotinic acetylcholine receptor
Which of the following is the most common withdrawal symptom of benzodiazepine toxicity?
a. Increased heart rate
b. Salivation
c. Hallucinations
d. Vomiting
c. Hallucinations
Which method is most appropriate for a conscious, alert patient who ingested a toxic dose of aspirin 1 hour ago?
a. Gastric lavage
b. Activated charcoal
c. Whole bowel irrigation
d. Induced emesis
b. Activated charcoal
What is the main reason multiple-dose activated charcoal (MDAC) is useful in salicylate overdose?
a. It enhances renal elimination
b. It interrupts enterohepatic and enteroenteric recirculation
c. It neutralizes acidic metabolites
d. It prevents CNS penetration
b. It interrupts enterohepatic and enteroenteric recirculation
Which antidote is correctly matched with its toxic exposure?
a. Atropine - opioid overdose
b. N-acetylcysteine - salicylate overdose
c. Flumazenil - TCA overdose
d. Fomepizole - methanol poisoning
d. Fomepizole - methanol poisoning
Which of the following increases the absorption time of aspirin justifying decontamination even>6 hours after ingestion
a. Increased renal clearance
b. Low protein binding
c. High first-pass metabolism
d. Formation of gastric bezoars
d. Formation of gastric bezoars
What is the primary route of elimination enhanced by urinary alkalinization?
a. Biliary excretion
b. Renal excretion of weak acids
c. Renal tubular secretion
d. Glomerular filtration of lipophilic drug
b. Renal excretion of weak acids
Which absorption-modifying technique is useful for sustained-release drug ingestions or body packers?
a. Activated charcoal
b. Whole bowel irrigation
c. Gastric lavage
d. Induced emesis
b. Whole bowel irrigation
A patient presents with signs of atropine toxicity. Which of the following symptoms would you most likely observe?
a. Dry mouth and mydriasis
b. Sweating and salivation
c. Bradycardia and miosis
d. Diarrhea and bronchorrhea
a. Dry mouth and mydriasis
Which of the following is the most appropriate first step in managing dermal exposure to a pesticide?
a. Apply topical corticosteroids
b. Neutralize with vinegar
c. Remove contaminated clothing and wash skin with soap and water
d. Apply activated charcoal to the skin
c. Remove contaminated clothing and wash skin with soap and water
In which of the following scenarios is gastric lavage most appropriate?
a. Iron overdose, 6 hours post-ingestion
b. Acetaminophen ingestion, 8 hours ago
c. Amitriptyline overdose, 30 minutes ago, with protected airway
d. Cocaine body-packer with stable vitals
c. Amitriptyline overdose, 30 minutes ago, with protected airway
Which of the following characteristics makes a substance less likely to be adsorbed by activated charcoal?
a. Lipophilic
b. High molecular weight
c. Strong acid or base
d. Neutral pH and small size
c. Strong acid or base
Which of the following is the most appropriate initial step in managing ocular exposure to a toxic chemical?
a. Apply antibiotic eye drops immediately to prevent infection.
b. Perform eye irrigation with normal saline for at least 15 minutes
c. Patch the eye and refer to ophthalmology.
d. Administer systemic antihistamines to reduce inflammation.
b. Perform eye irrigation with normal saline for at least 15 minutes
A drug with a high volume of distribution (Vd) is primarily found in the plasma and is easily removed by hemodialysis.
a. True
b. False
b. False
A 35-year old farm worker is brought into the ER with salivation, lacrimation, urination, diarrhea and muscle twitching after pesticide exposure. His HR is 50 bpm and pupils are pinpoint.
Which of the following is the most appropriate antidotal therapy?
A. Flumazeril
B. Atropine
C. N-acetylcysteine
D. Naloxone
B. Atropine
A 17-year old female is brought to the ED by her parents after being found confused and agitated in her room. They report finding an empty bottle of an OTC sleep aid. On exam, she is flushed, her skin is dry, and her pupils are dilated and non-reactive to light. She is disoriented, attempting to remove her clothing, and muttering incoherently. Her vital signs are: BP: 135/88 mmHg, HR: 118 bpm, RPM: 14 rpm, T: 38.9 C
Which of the following substances could be responsible for this pts symptoms? Select all that apply
A. Diphenhydramine
B. Atroping
C. Jimson Weed
D. Organophosphates
E. Physostigmine
A. Diphenhydramine
C. Jimson Weed
A 19-year old college student is brought to the ED by campus police 4 hours after ingesting an unknown quantity of ER diltiazem tablets in a suicide attempt. She is currently alert. The healthcare team is considering use of activated charcoal.
Which of the following PK properties is most important to consider when deciding whether activated charcoal is likely to be beneficial at this point?
A. Rate of absorption (Ka)- predicts onset of action; depends on dosage form
B. Extent of absorption (F or BA)- predicts intensity of effect; influenced by first-pass metabolism
C. Volume of distribution (Vd)- determines tissue penetration
D. Elimination of half-life- predicts drug duration in the body
A. Rate of absorption (Ka)- predicts onset of action; depends on dosage form
A 34-year old male presents to the ED after ingesting a large number of iron tablets in a suspected suicide attempt, approx. 2 hours ago. The poison control center recommends consideration of WBI to limit further drug absorption. His med history and presentation include:
Adynamic ileus (non-mechanical intestinal obstruction)
Chronic Renal Insufficiency
Active nausea and vomiting
Which of the following are contraindications to performing WBI in this pt? Select all that apply
A. Adynamic ileus
B. Iron tablets
C. Active vomiting
D. Chronic renal insufficiency
A. Adynamic ileus
C. Active vomiting
A 45 yo is brought to the ED after ingesting a large quantity of an unknown drug during a suicide attempt. Her symptoms include confusion, hypotension, & respiratory depression. Blood samples confirm the presence of a highly lipophilic drug with the following PK profile:
Vd: 6.5 L/kg
High protein binding
Extensive tissue penetration, esp. into adipose and CNS tissue
Minimal renal clearance
The toxicology team is considering potential treatment options, including enhanced elimination strategies
Based on this drug's distribution, which of the following is the most appropriate conclusion?
A. The drug is likely to remain in the plasma and is easily removed by hemodialysis
B. The drug distributes extensively into tissues, making hemodialysis ineffective
C. The drug's distribution is limited, and urinary alkalinization would significantly increase clearance
D. The drug is poorly absorbed and has limited clinical toxicity
B. The drug distributes extensively into tissues, making hemodialysis ineffective
A 22-year old male is brought to the Ed with suspected overdose. He is currently exhibited salivation, lacrimation, urination, diarrhea, and bronchorrhea.
Which of the following receptor types is most likely responsible for his symptoms?
A. Alpha-1 adrenergic receptors
B. Beta-2 adrenergic receptors
C. Muscarinic cholinergic receptors
D. Dopaminergic receptors
C. Muscarinic cholinergic receptors
A 17 yo male with a history of neurological condition is brought to the ED by his parents after being found lethargic and confused. His family reports he may have taken a large amount of med. On exam, pt is somnolent but arousable. Vital signs are stable. He has a dry mouth, mild hypotension, and occasional myoclonic jerks (Tourette's syndrome). His med list includes: haloperidol, clonidine, sertraline
The clinical team suspects overdose of his antipsychotic medication, which was recently increased.
Which of the following neuroreceptors is most likely involved in both the therapeutic effect and toxic presentation of this dose?
A. GABA-A receptors
B. Dopamine D2 receptors
C. Alpha-2 adrenergic receptors
D. NMDA glutamate receptors
B. Dopamine D2 receptors
A 26 yo male with a hx of drug use disorder presents to the clinic with complaints of muscle aches, diarrhea, runny nose, and yawning. He appears agitated and restless but is afebrile. Pupils are dilated, and vital signs show mild hypertension and tachycardia.
Which of the following best describes the likely cause of his symptoms?
A. Cocaine withdrawal
B. Benzodiazepine withdrawal
C. Opioid withdrawal
D. Serotonin syndrome
C. Opioid withdrawal
A 29 yo grad student presents to the campus clinic complaining of persistent headache, fatigue, difficulty concentrating, and feeling irritable. She mentions that these symptoms began 2 days ago after she decided to "cut out coffee completely". She previously consumed 4-5 cups a day for the past 3 years. She denies use of other substances, meds, or change is sleep or diet.
Vitals are stable. Neurological exam is normal except for slowed verbal responses and low energy.
Which of the following receptors is most likely involved in the pts symptoms?
A. Dopamine D2 receptors
B. NMDA glutamate receptors
C. Adenosine receptors
D. GABA-A receptors
C. Adenosine receptors
Excitatory neurons fire ____________, inhibitory neurons _______________________
- regularly
- suppress this activity
Therefore, all action is fundamentally a result of...
disinhibition in the CNS
What does a xenobiotic that persistently activates inhibitory pathways cause?
causes adaptive neuronal changes
Action occurs when inhibitory tone is ____________, allowing _______________ to reach end organs
- reduced
- excitatory signals
Tonic inhibition = _________________
sustained inhibition
When the xenobiotic is reduced or removed....
Withdrawal syndrome occurs
Characteristics of Withdrawal Syndromes (2)
1. A preexisting physiologic adaptation due to constant xenobiotic exposure
2. Reduction of the xenobiotic below a threshold causes physiological disruption
- this is different from tolerance, dependence, and addiction
Tolerance
higher dose needed for the same effect (right-shift of dose-response curve)
Dependence
body requires the xenobiotic to avoid withdrawal
Addiction
compulsive drug-seeking, psychological in nature
DSM-5 Criteria for Withdrawal: Withdrawal is defined by: (2)
1. A characteristic syndrome when the substance is removed, or
2. Use of the same (or similar) xenobiotic to relieve/avoid withdrawal
True Withdrawal vs. Posttoxicity Syndromes
• Withdrawal syndrome: Requires both DSM-5 features, is managed by reintroducing and tapering the drug.
• Posttoxicity syndrome (e.g., from cocaine):
- Symptoms like lethargy, irritability, hypersomnolence.
- No drug is taken to relieve symptoms, resolves without treatment.
- Misnamed as “withdrawal” but doesn’t meet full criteria
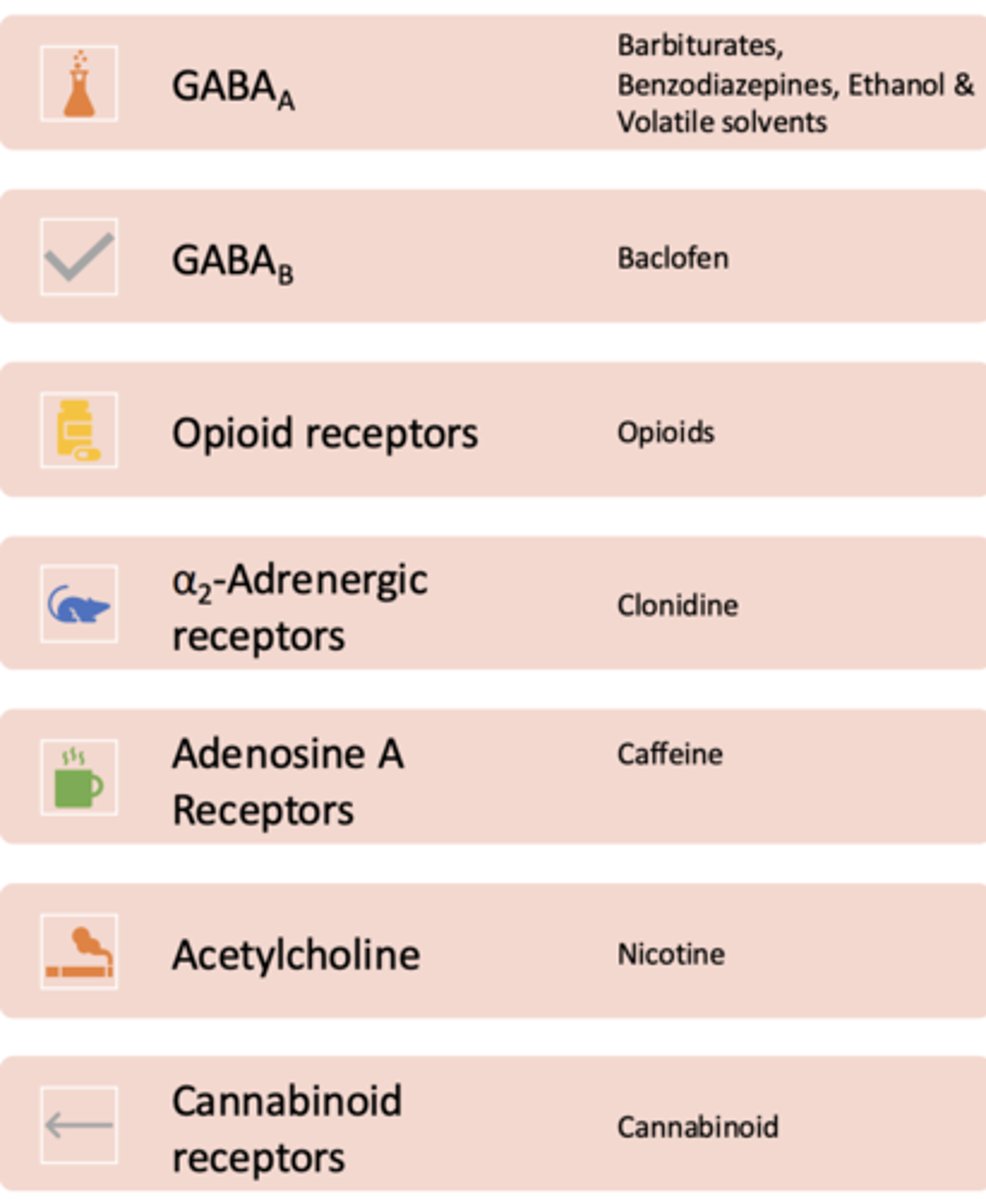
Receptors:
- GABAa- Barbiturates, Benzodiazepines, Ethanol & Volatile solvents
- GABAb- baclofen
- Opioid receptors- opioids
- α2 -Adrenergic receptors- clonidine
- Adenosine A Receptors- caffeine
- Acetylcholine- nicotine
- Cannabinoid receptors- cannabinoid
Benzodiazepines
- Symptoms of withdrawal:
- Pathophysiology
- Treatment:
Symptoms of withdrawal: anxiety, tremors, insomnia, agitation, seizures, hallucinations
Pathophysiology: chronic use increases GABAa activity. The brain compensates with decreased receptor sensitivity
Treatment: Tapering doses, long-acting BZDs (diazepam), supportive care
Barbiturates
- Symptoms of withdrawal:
- Pathophysiology
- Treatment:
Symptoms of withdrawal: Anxiety, agitation, tremors, seizures, delirium, possible CV collapse
Pathophysiology: Chronic use leads to CNS depression via GABAa. Withdrawal causes CNS hyperexcitability
Treatment: Phenobarbital taper (crosstolerance); intensive monitoring/support
Ethanol
- Symptoms of withdrawal:
- Pathophysiology
- Treatment:
Symptoms of withdrawal: tremors, irritability, insomnia, hallucinations (visual), seizures, delirium
Pathophysiology: ethanol increases GABAa and decreases NMDA. Withdrawal causes an increase in glutamate and a decrease in GABA = hyperexcitation
Treatment: Benzodiazepines, thiamine, fluids/electrolytes
What is a typical clinical symptom of ethanol withdrawal?
A. Bradycardia and severe sedation
B. CNS excitation, such as tremors, seizures, and agitation
C. Depressed mood and lack of energy
D. Hypotension and confusion
B. CNS excitation, such as tremors, seizures, and agitation
Opioid (heroin, morphine, oxycodone, fentanyl) withdrawal syndrome
- Symptoms: (12)
- Pathophysiology:
- Treatment:
Symptoms: yawning, lacrimation, rhinorrhea, piloerection, diaphoresis, mydriasis, NV, diarrhea, muscle aches, insomnia, anxiety
Pathophysiology: chronic use leads to a decrease in endogenous opioid production and receptor down regulation. This causes an abrupt stop = overactive nonadrenergic output
Treatment, First-line: buprenorphine or methadone (opioid agonist therapy); clonidine (α2-agonist for autonomic symptoms); antiemetics; loperamide for diarrhea
Withdrawal is very uncomfortable but not ___________________
life-threatening (unlike alcohol or barbiturates)
Baclofen
- Receptor Target:
- Withdrawal Symptoms:
- Pathophysiology:
- Treatment:
Receptor Target: GABAb agonist
Withdrawal Symptoms: seizures, hallucinations, psychosis, rebound spasticity, insomnia, hypertension
Pathophysiology: abrupt discontinuation leads to loss of chronic GABAb mediated inhibition and CNS hyperexcitability
Treatment: reintroduce baclofen; benzodiazepines for seizures; supportive care
Clonidine
- Receptor Target:
- Withdrawal Symptoms:
- Pathophysiology:
- Treatment:
Receptor Target: α2-adrenergic agonist
Withdrawal symptoms: Rebound hypertension, tachycardia, anxiety, agitation, headache
Pathophysiology: sudden stop causes excessive NE release from loss of α22 inhibition
Treatment: Restart clonidine and taper slowly; short-term antihypertensives (beta-blockers)
Caffeine
- Receptor Target:
- Withdrawal Symptoms:
- Pathophysiology:
- Treatment:
Receptor Target: adenosine receptor antagonist
Withdrawal symptoms: Headache, fatigue, irritability, difficulty concentrating, nausea
Pathophysiology: withdrawal causes adenosine rebound activity (vasodilation, decreased alertness)
Treatment: Gradual taper; NSAIDs for headache; hydration
Nicotine
- Receptor Target:
- Withdrawal Symptoms:
- Pathophysiology:
- Treatment:
Receptor Target: nicotinic acetylcholine (nAChR)
Withdrawal symptoms: Irritability, anxiety, restlessness, increased appetite, insomnia, depression
Pathophysiology: nicotine up-regulates and desensitizes nAChRs. Withdrawal causes dopaminergic and cholinergic dysregulation
Treatment: NRT (gum, patch), buproprion, varenicline
Cannabinoids
- Receptor Target:
- Withdrawal Symptoms:
- Pathophysiology:
- Treatment:
Receptor Target: CB-1 receptor agonist
Withdrawal symptoms: Irritability, insomnia, decreased appetite, anxiety, depression, headaches
Pathophysiology: chronic use causes endogenous cannabinoid signaling. Withdrawal causes CNS dysregulation and stress response activation
Treatment: Supportive care; in some cases, gabapentin or mirtazapine used off-label
Which of the following is the most appropriate treatment for seizures due to baclofen withdrawal?
A. Opioids
B. Benzodiazepines and GABAA agonists
C. Dopamine agonists
D. Antidepressants
B. Benzodiazepines and GABAA agonists
Which of the following substances is most likely to cause a withdrawal syndrome similar to that of alcohol and benzodiazepines?
A. Cocaine
B. Opioids
C. Caffeine
D. Nicotine
B. Opioids
What is a typical clinical symptom of ethanol withdrawal?
A. Bradycardia and severe sedation
B. Hypotension and confusion
C. Depressed mood and lack of energy
D. CNS excitation, such as tremors, seizures, and agitation
D. CNS excitation, such as tremors, seizures, and agitation
T/F: Cocaine and amphetamines cause withdrawal syndrome (as seen with other substances like opioids or alcohol)
FALSE
do not cause withdrawal syndrome
MOA of cocaine and amphetamines
- dopamine reuptake inhibitors (cocaine) or DA and NE releasers (amphetamines)
- do not directly alter neurotransmitter systems in a way that leads to physical dependence
Lack of physical dependence of cocaine and amphetamines
increase neurotransmitter activity acutely, but they don't promote long-term neuroadaptation in the same way as drugs like alcohol or opioids
Opioids and GABAergic drugs cause ______________ of receptors, which leads to ________________________ and withdrawal when the drug is removed
- downregulation
- physical dependence
Cocaine and amphetamines lead to....
psychological dependence (cravings and compliance use), but not physical dependence (seizures, tremors) in the same way that opioids or alcohol do
Alcohol, benzodiazepines, and opioids cause ________________, leading to physical dependence
tolerance (where increasing doses are needed for the same effect)
T/F: Cocaine and amphetamine cause the same chronic tolerance/neuroadaptation as alcohol, benzodiazepines, etc.
FALSE
do NOT
What does withdrawal opioids and alcohol typically involve?
increased glutamate release and decreased GABAergic function
- causes the hyperexcitability seen in withdrawal symptoms
- cocaine and amphetamines do not alter neurotransmitter systems in a way that causes this type of neurochemical imbalance
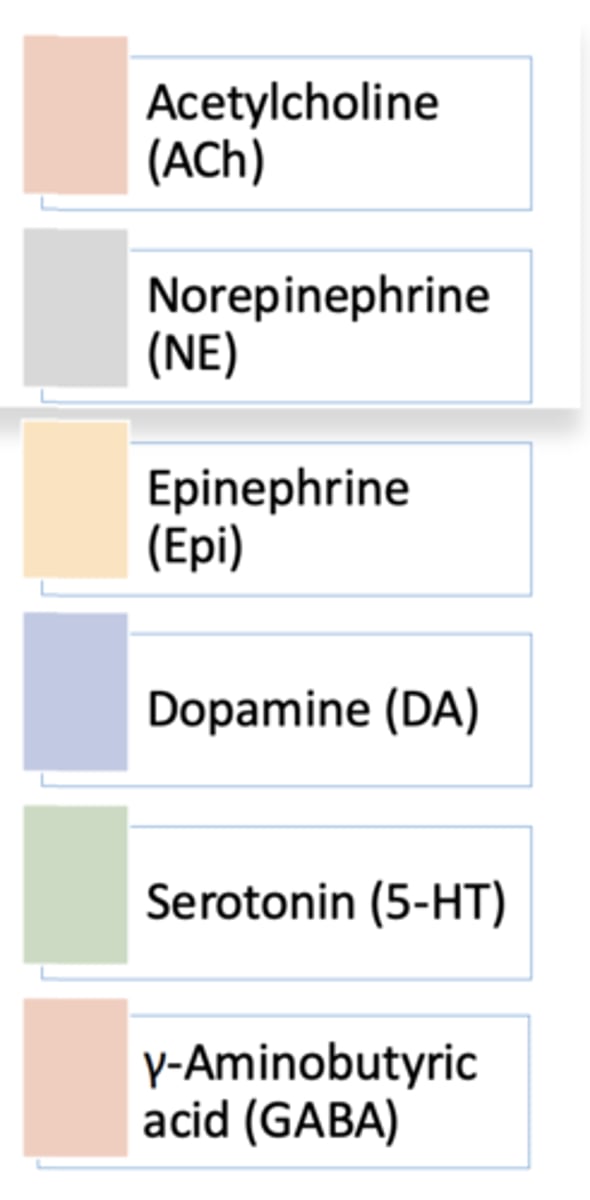
Toxicology often focuses on how xenobiotics disrupt.....
neurotransmission-the relay of signals between neurons or from neurons to muscles, ex: Ach, NE, Epi, DA, 5-HT, GABA
T/F: Most toxic substances affect more than one receptor or pathway
TRUE
effects are complex, not always easily predicted by a single mechanism
T/F: Toxic effects are always due to one neurotransmitter
FALSE
effects may overlap
Examples of Multimodal Toxicologic Effects: Doxepin (a trycyclic antidepressant
Blocks: (2)
Antagonizes: (6)
Inhibits reuptake of: (3)
• Blocks: Sodium & potassium channels
• Antagonizes: H1, H2, α-adrenergic, muscarinic ACh, D2, GABAA receptors
• Inhibits reuptake: NE, serotonin, adenosine
Neurons maintain a resting membrane potential of -65 mV due to.... (2)
• Na⁺/K⁺-ATPase
• Impermeability to large, negatively charged intracellular proteins
Channels vary structurally but share conserved sequences, explaining how xenobiotics may...
affect multiple types
Voltage-gated channels open with...
changes in membrane potential
Ligand-gated channels open with...
binding of neurotransmitters
The 3 stages voltage-gated Na+ channels have
-Resting: Closed
-Activated: Open, Na⁺ influx
-Inactivated: Temporarily nonfunctional until repolarization restores resting state
What is action potential propagation triggered by?
- by Na⁺ or Ca²⁺ influx (depolarization)
- blocked K⁺ efflux
Na+ channel activation is....
self-propagating
Repolarization
Primarily K⁺ efflux, minor Cl⁻ influx
Acetylcholine (ACh) Location
- CNS:
- PNS:
• CNS: Brain and spinal cord; diffuse cortical projection
• PNS: Autonomic and somatic motor fibers
ACh synthesis:
- Enzyme:
- Substrates: 2
- Enzyme: Choline acetyltransferase
- Substrates: Acetyl-CoA + Choline
ACh release mechanism
Ca²⁺- dependent exocytosis
ACh inactivation
- Primary enzyme:
- Choline reuptake:
- Primary Enzyme: Acetylcholinesterase (AChE) → Choline + Acetic acid
- Choline reuptake: Na⁺- dependent ChT transporter
ACh receptors (2)
- Nicotinic Receptors (nAChRs)
- Muscarinic Receptors (mAChRs)
ACh receptors: Nicotinic Receptors (nAChRs)
- Location:
- Type:
• Location: CNS, autonomic ganglia, adrenal medulla, NMJ.
• Type: Ligand-gated ion channel (Na⁺/Ca²⁺ influx)
ACh receptors: Muscarinic Receptors (mAChRs)
- Location:
- Type:
• Location: CNS, parasympathetic end organs, sweat glands
• Type: G protein-coupled receptors
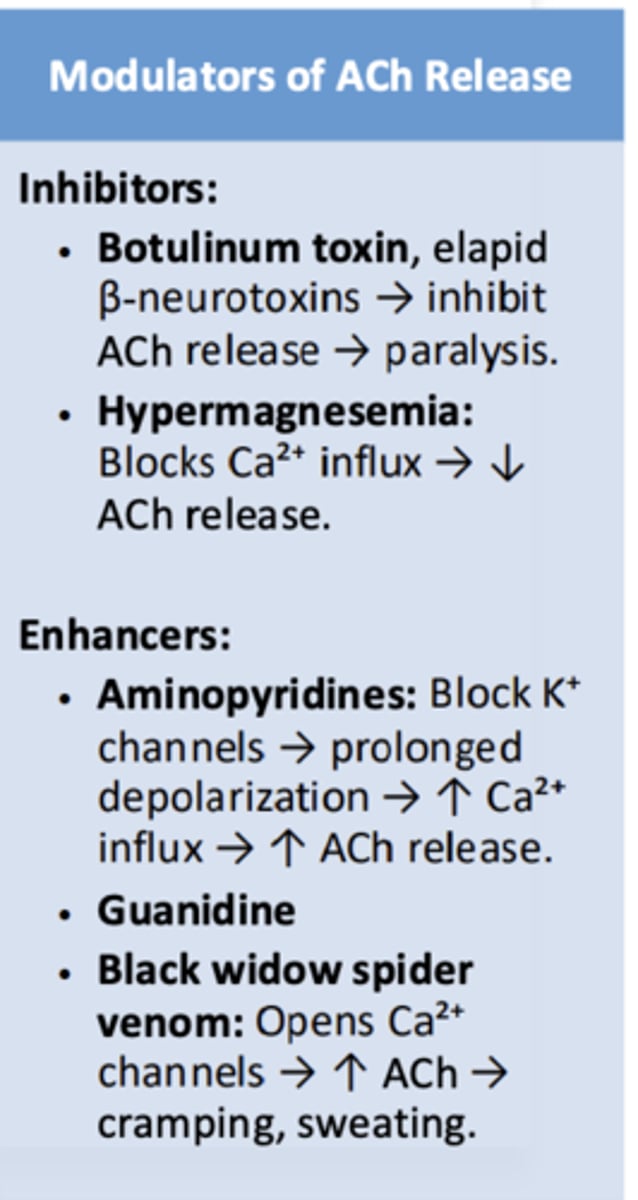
Modulators of ACh release can be....
- inhibitors (botulinum toxin, hypermagnesemia)
- enhancers (aminopyridines, guanidine, black widow spider venom)
Muscarinic receptor peripheral effects of agonists
SLUDG- salivation, lacrimation, urination, diarrhea, GI upset, emesis), bradycardia, miosis, bronchospasm