Lecture 7: Cardiac Output, Venous Return, and Their Regulation Muscle Blood Flow and CO During Exercise. The Coronary Circulation
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
The quantity of blood pumped into the aorta each minute by the heart. This is also the quantity of blood that flows through the circulation. (LV > Aorta)
CO is one of the most important factors that we must consider in relation to the circulation because it is the sum of the blood flows to all the tissues of the body.
What is the definition of Cardiac Output (CO)?
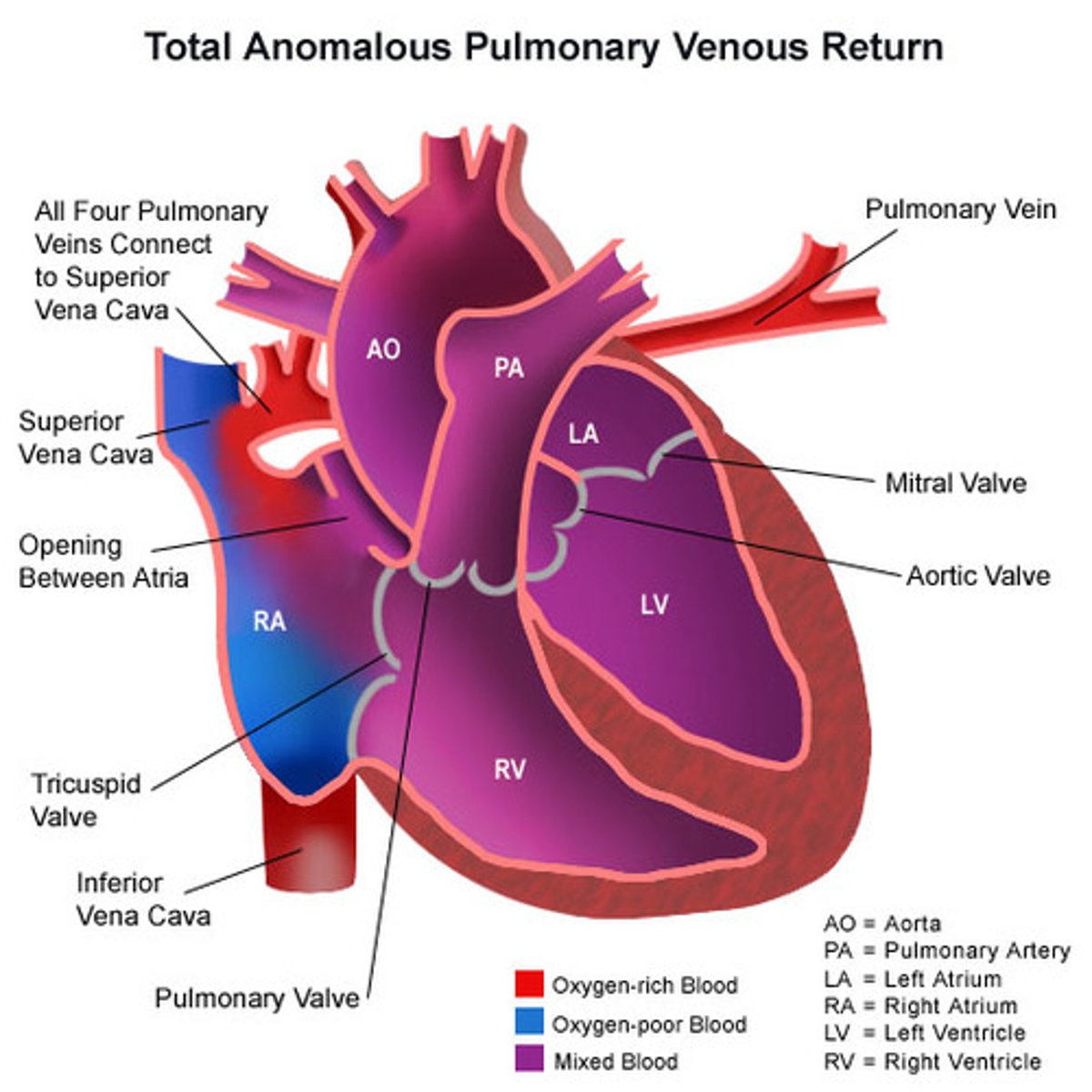
The quantity of blood flowing from the veins into the right atrium each minute.
•The venous return and the CO must equal each other except for a few heartbeats at a time when blood is temporarily stored in or removed from the heart and lungs.
What is the definition of venous return (VR)?
Venous Return (VR)
•Venous return is important because the more blood returns to the heart, the more blood can be pumped out.
What is the major determinant of Cardiac Output (CO)?
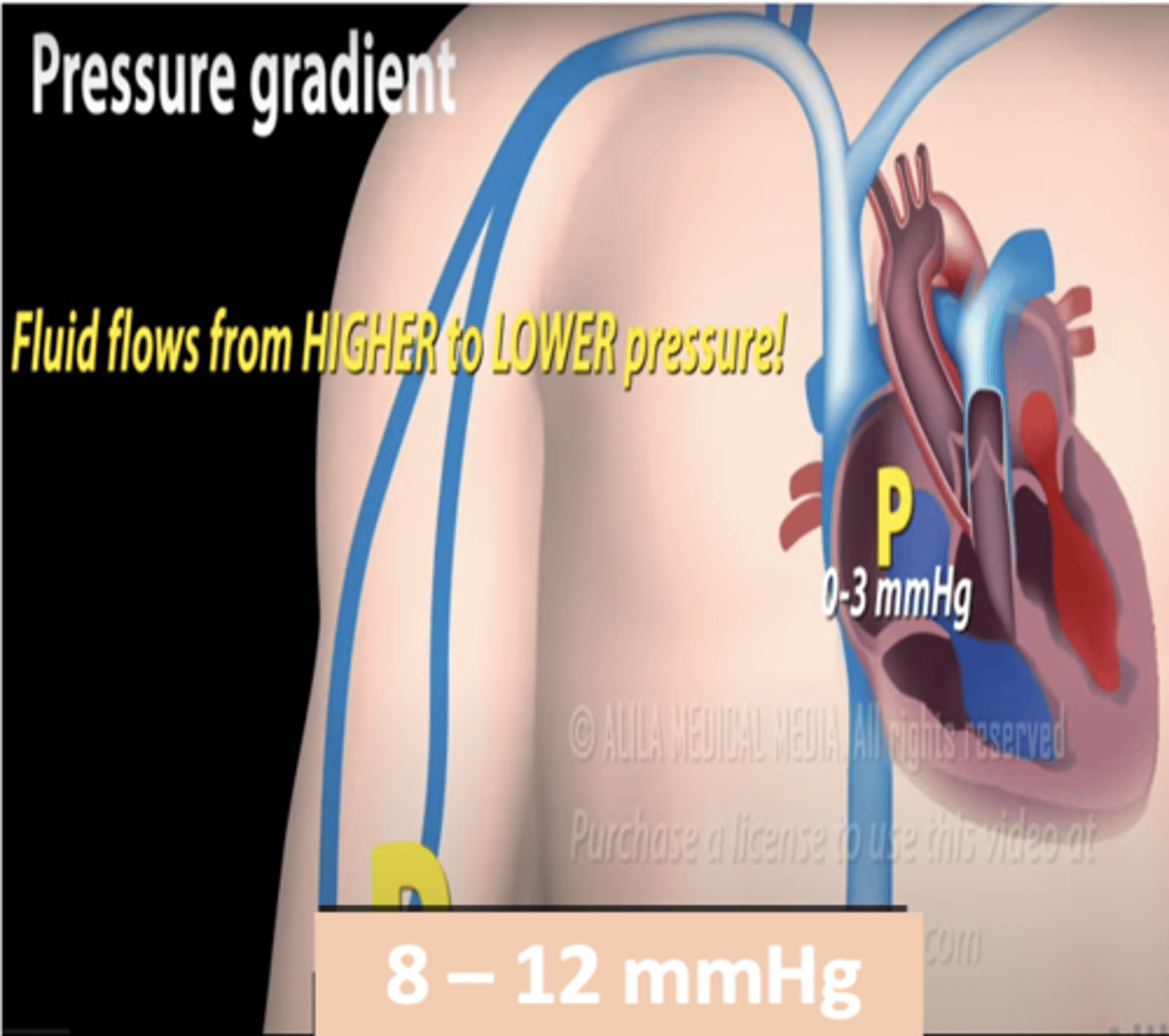
Venous pressure (8-12 mmHg) and right atrial pressure (0-3 mmHg)
(Flows from high to low pressure)
What is the major force driving peripheral blood back to the heart? (factors that facilitate venous return)
During everyday activities, such as walking the muscles contract and squeeze blood in the veins upwards, toward the heart
The one-way valves prevent blood from flowing down again when the muscles relax.
What is one of mechanisms by which physical exercise increases CO to meet the body’s needs?
Increasing the rate and depth of breathing
What is another way the body raises CO during physical exercise?
1. Basic level of body metabolism
2. Whether the person is exercising
3. The persons age
4. The size of the body
What factors directly affect cardiac output? (4)
5-6 L/min
What is the resting cardiac output averages for males?
4-9 L/min
What is the resting cardiac output averages for Females?
5 L/min
What is the average cardiac output for the resting adult?
Cardiac output per square meter of body surface area.
The CO increases approximately in proportion to the surface area of the body.
Therefore, CO is frequently stated in terms of the cardiac index, which is the
2.5-4.2 L/min/m2
The cardiac index of the normal adult range is what?
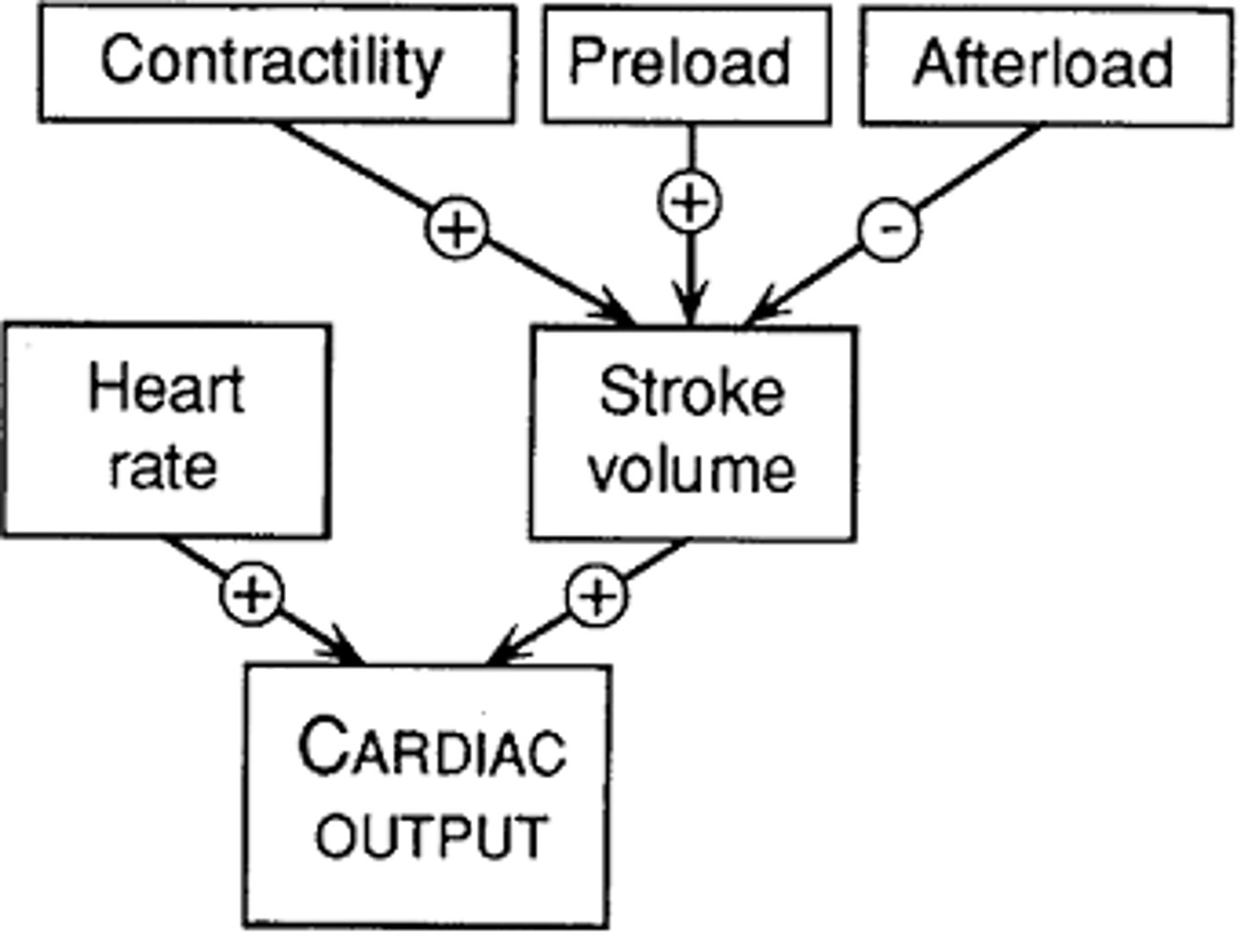
contractility, preload, and afterload
What are the three distinct influences on stroke volume
increasing the contractility of the cardiac muscle
Increased cardiac sympathetic nerve activity tends to increase stroke volume by
increasing the afterload on cardiac muscle fibers.
Increased arterial pressure tends to decrease stroke volume by
increase stroke volume through Starling's law.
Increased ventricular filling pressure increases end-diastolic volume which tends to increase
the force of a cardiac muscle contraction is directly proportional to the initial length of its muscle fibers
What is the Frank-Starling law of the heart?
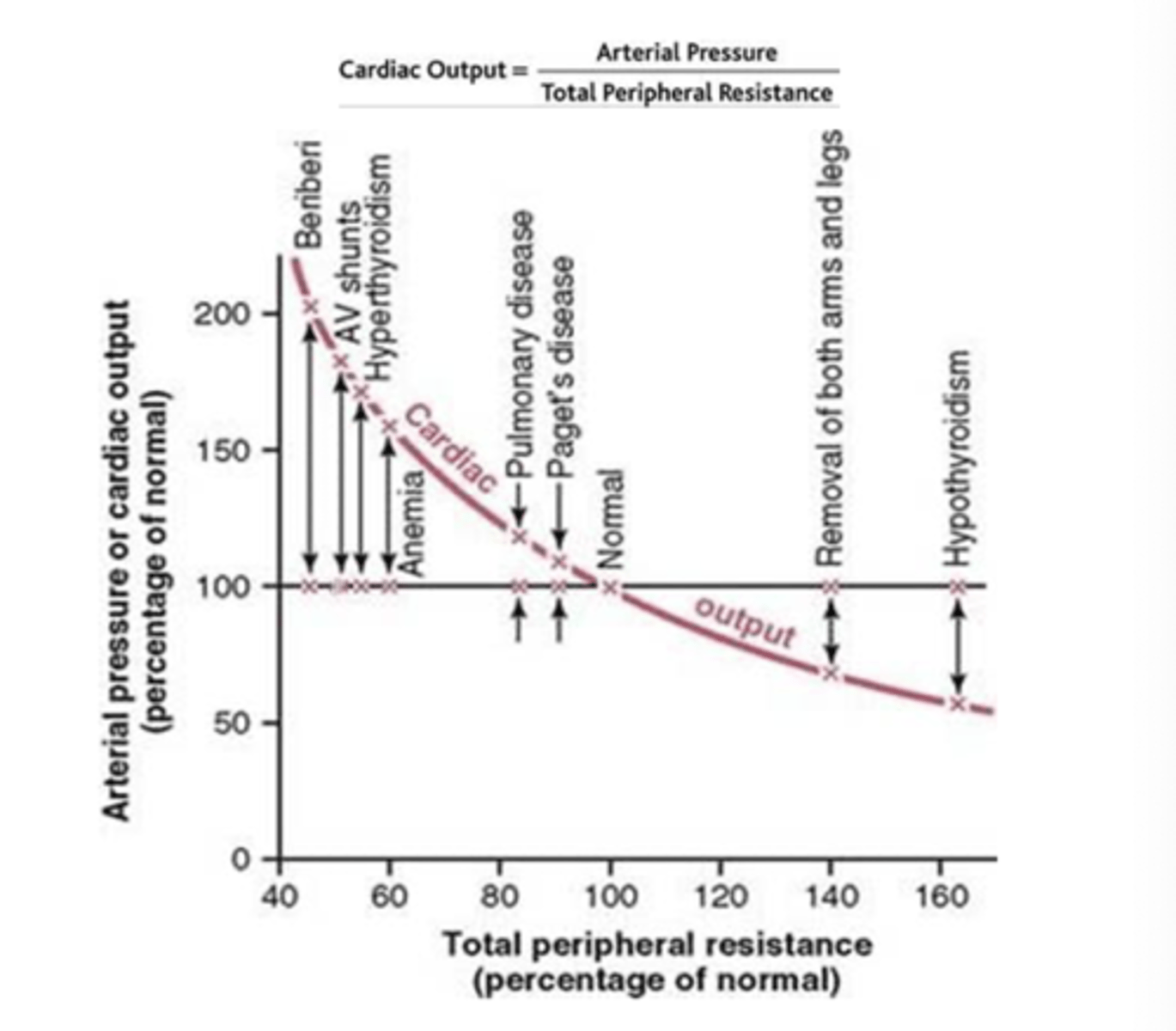
Decreases
When the total peripheral resistance increases above normal, the cardiac output
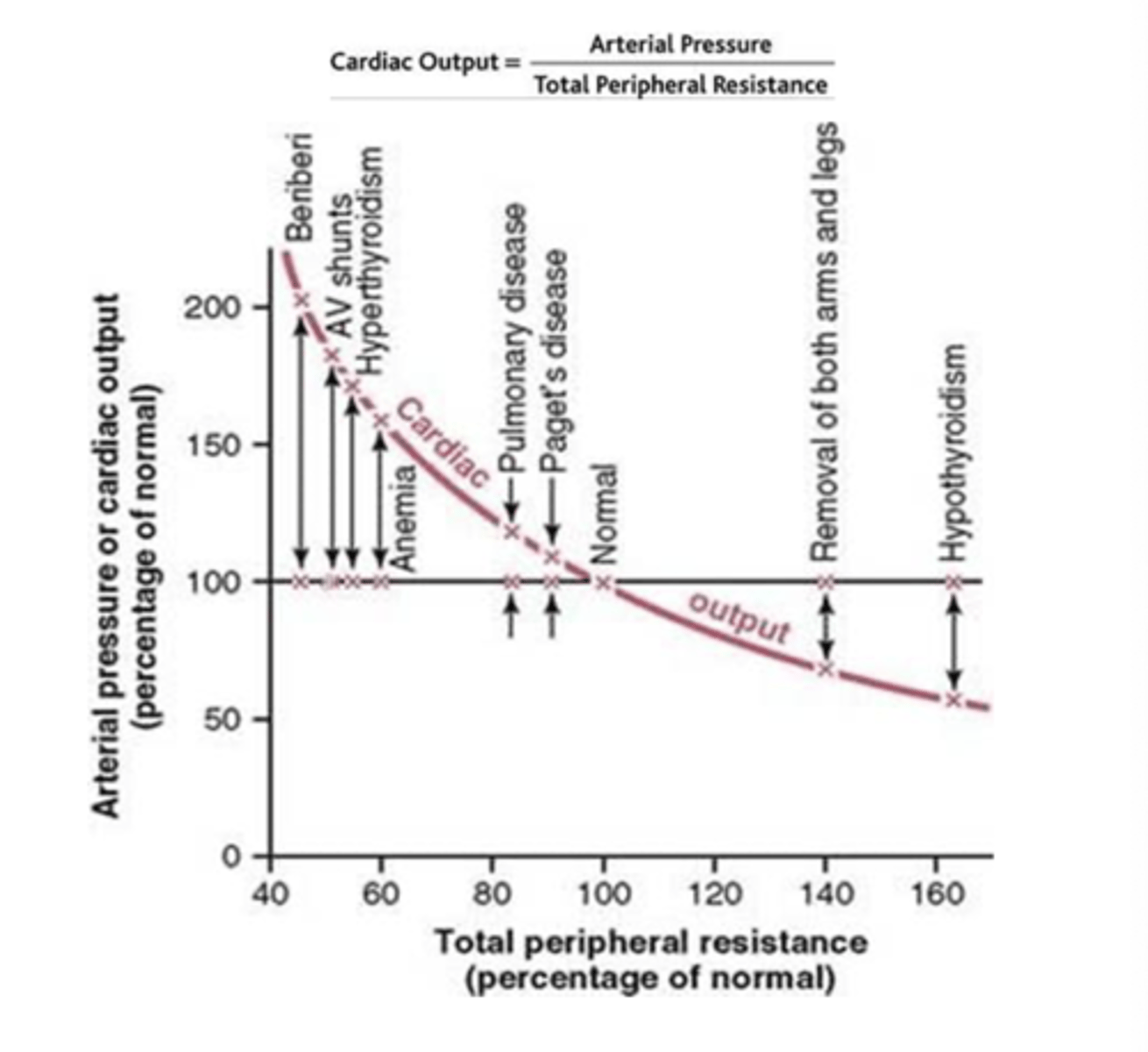
increases
when the total peripheral resistance decreases, the cardiac output
local control of vascular resistance in response to muscle tissue metabolic needs.
During exercises, the blood flow to the skeletal muscles and coronary artery blood flow to the heart increase. The regulation of each of these is achieved mainly by
(1) mass discharge of the sympathetic nervous system throughout the body with consequent stimulatory effects on the entire circulation,
(2) increase in arterial pressure
(3) increase in cardiac output.
What are the three major effects occur during exercise that are essential for the circulatory system to supply the tremendous blood flow required by the muscles.
•a mechanical response that increases venous return and
•a chemical response that dilates blood vessels in active muscle.
How does muscle contraction directly affect the cardiovascular system in what two ways?
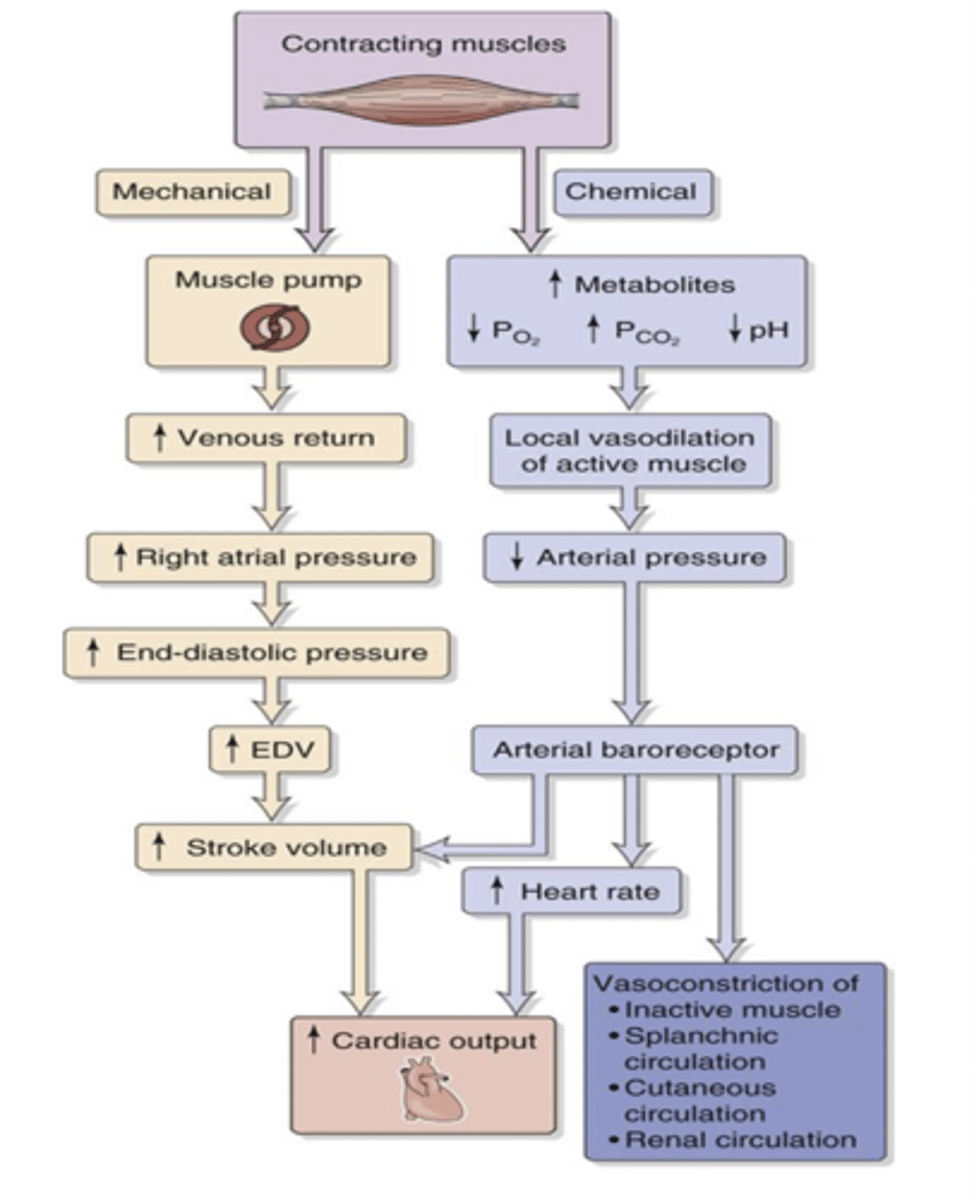
Changes in CO₂ and O₂ levels
What is a common factor that indicates a change in metabolic activity?
causes vasodilation.
How does an increase in CO₂ levels affect blood vessels (arterioles)?
Increased blood flow.
What is the result of vasodilation in response to increased CO₂ levels?
It helps deliver more oxygen and nutrients while removing waste products like CO₂.
Why is vasodilation important in metabolic regulation?
hey typically cause vasodilation.
What is a common effect of inflammatory chemicals on blood vessels?
Histamine and nitric oxide.
Name two examples of inflammatory chemicals that influence blood vessel behavior.
Increased metabolic wastes accumulate
What happens when there is decreased blood flow?
Vasodilation, leading to increased blood flow
What is the body's response to increased metabolic wastes?
Stretch of the arterial wall due to increased pressure.
What triggers the myogenic response in blood vessels?
Reflex constriction of the arterial wall.
What is the result of the myogenic response?
They supply most of the heart muscle with blood.
What do epicardial coronary arteries supply?
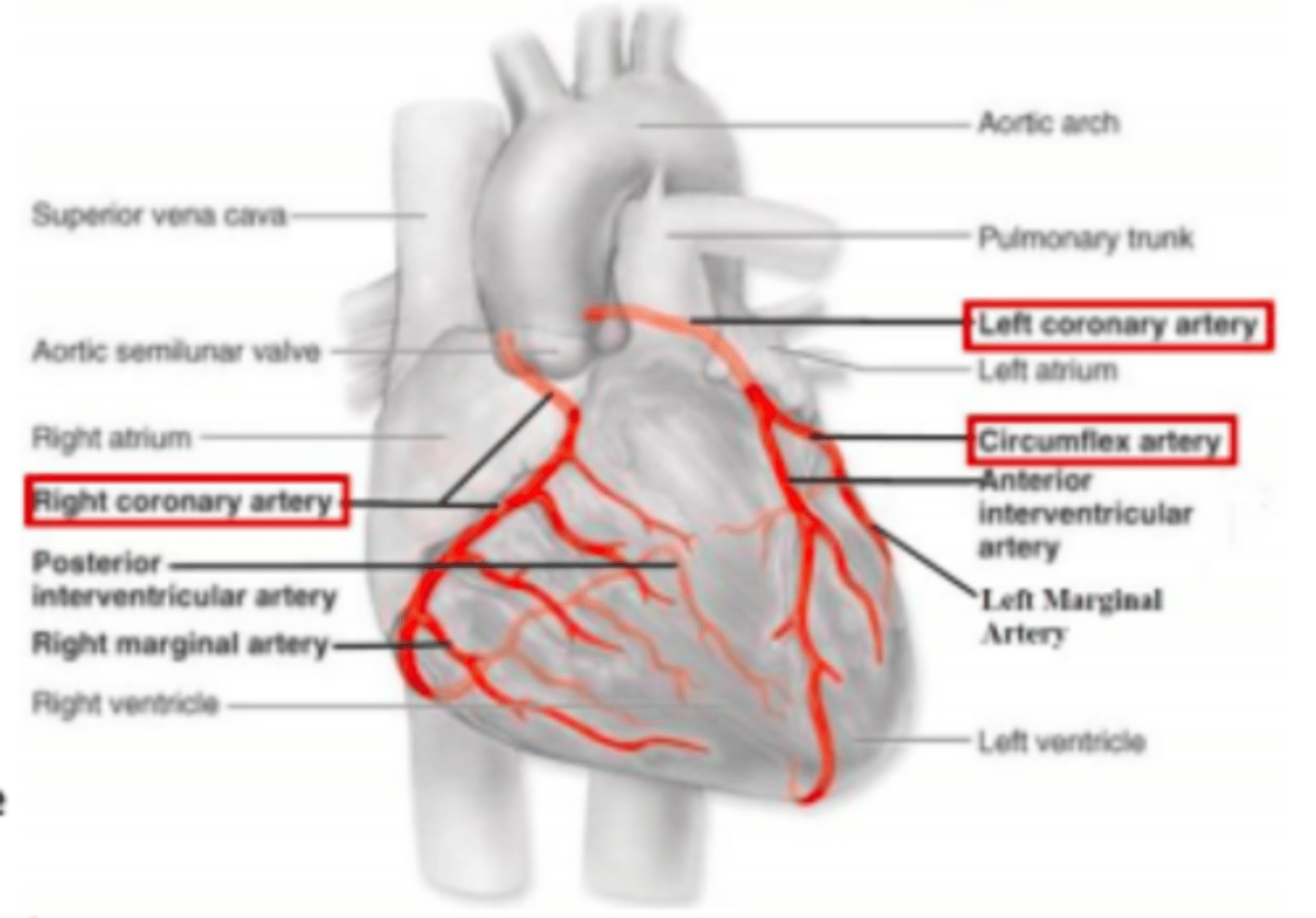
Smaller arteries derived from the epicardial coronary arteries that penetrate the heart muscle to supply nutrients.
What are intramuscular arteries?
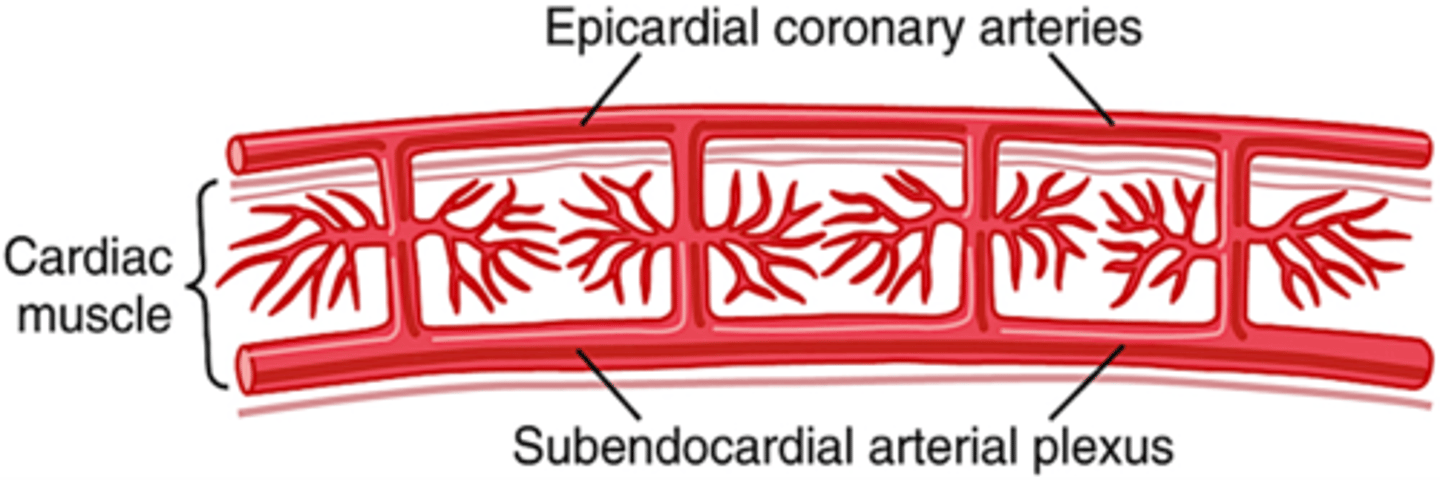
It reduces blood flow due to compression by ventricular muscle contraction
How does systole affect blood flow through the subendocardial plexus of the left ventricle?
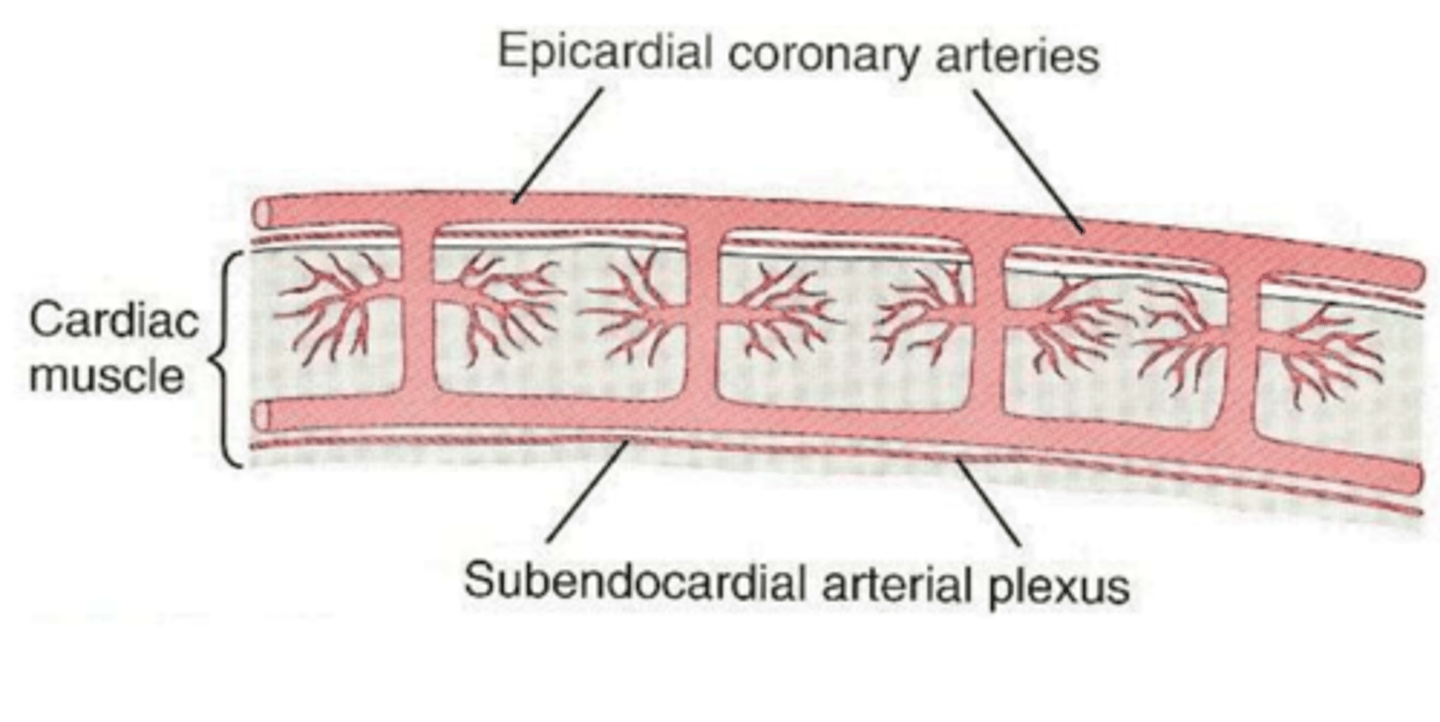
Extra vessels in the subendocardial plexus normally compensate.
How does the heart compensate for reduced blood flow in the subendocardial plexus during systole?
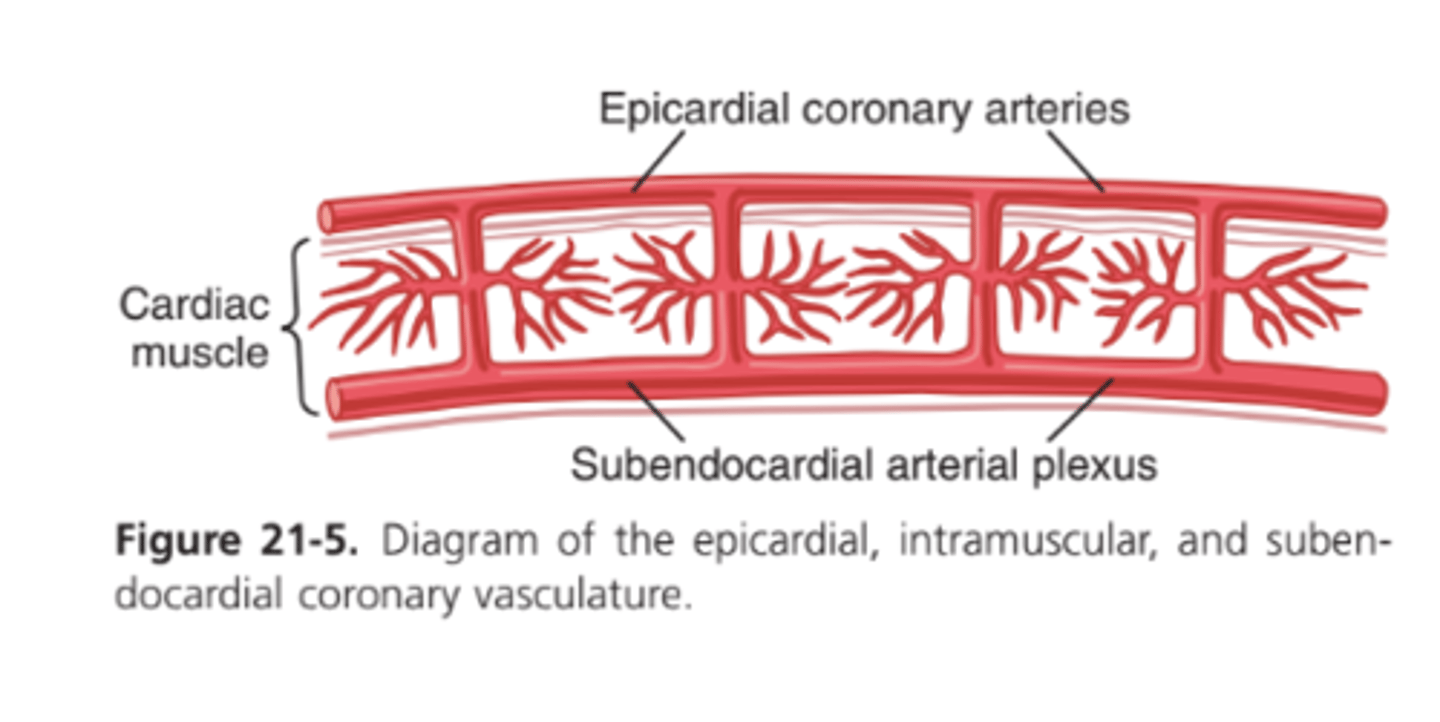
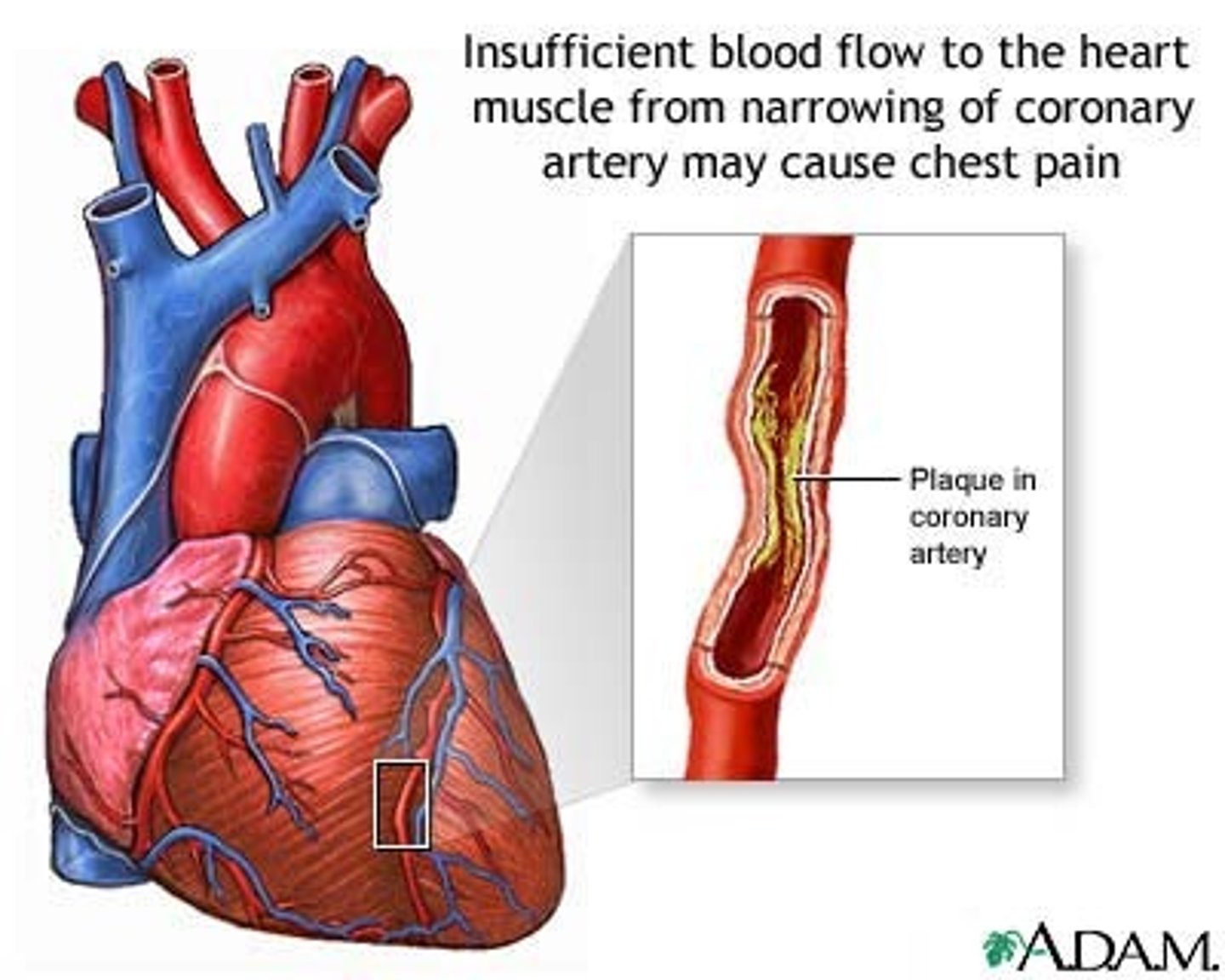
It plays a key role in certain types of coronary ischemia.
Why is the difference between blood flow in the epicardial and subendocardial arteries clinically important?
Local Muscle Metabolism
What is the primary controller of coronary blood flow?
It is regulated almost exactly in proportion to the oxygen needs of the cardiac musculature.
How is coronary blood flow regulated?
About 70% of the oxygen.
What percentage of oxygen in coronary arterial blood is typically removed by the heart?
The coronary blood flow increases almost directly proportional to the additional oxygen consumption.
How does the heart respond to an increased metabolic demand for oxygen?
A decrease in oxygen concentration in the heart, leading to the release of vasodilator substances.
What triggers coronary vasodilation according to current speculation?
Adenosine.
Which substance is known for its strong vasodilator effect in the heart?
ATP degrades to AMP, and portions of AMP are further degraded to release adenosine
How is adenosine formed in the heart during low oxygen conditions?
Much of it is reabsorbed into cardiac cells and reused.
What happens to adenosine after it causes vasodilation?
Potassium ions, hydrogen ions, carbon dioxide, prostaglandins, and nitric oxide.
Name other substances besides adenosine that act as vasodilators in the heart.
Acetylcholine (ACh).
Which neurotransmitter is released by the vagus nerves in the parasympathetic nervous system?
It slows the heart rate and slightly depresses heart contractility.
What effect does ACh from the vagus nerves have on the heart?
By decreasing cardiac oxygen consumption, which leads to coronary artery constriction.
How does the parasympathetic nervous system indirectly affect coronary blood flow?
Parasympathetic activity decreases cardiac oxygen consumption.
What is the relationship between parasympathetic activity and cardiac oxygen consumption?
Norepinephrine and epinephrine.
What neurotransmitters are released by the sympathetic nervous system?
They increase heart rate and contractility.
How do norepinephrine and epinephrine affect the heart?
The metabolic rate increases.
What happens to the heart's metabolic rate under sympathetic stimulation?
Local regulatory mechanisms cause vasodilation, increasing blood flow in proportion to metabolic needs.
How does the coronary blood flow respond to increased metabolic demands of the heart?