6F: REPRODUCTIVE SYSTEM
0.0(0)
Card Sorting
1/143
Earn XP
Description and Tags
Last updated 3:09 PM on 12/4/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
144 Terms
1
New cards
Functions of the Reproductive System
Production of gametes, fertilization, development and nourishment of a new individual, production of reproductive hormones.
2
New cards
Gametes
Reproductive cells of the body. In males, they are known as sperm cells and in the ovaries of females, they are known as oocytes (eggs).
3
New cards
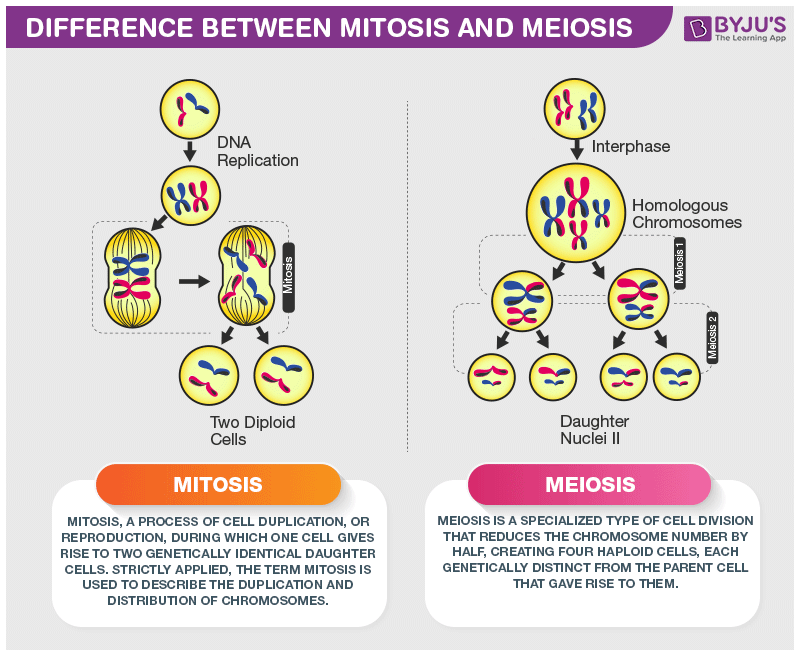
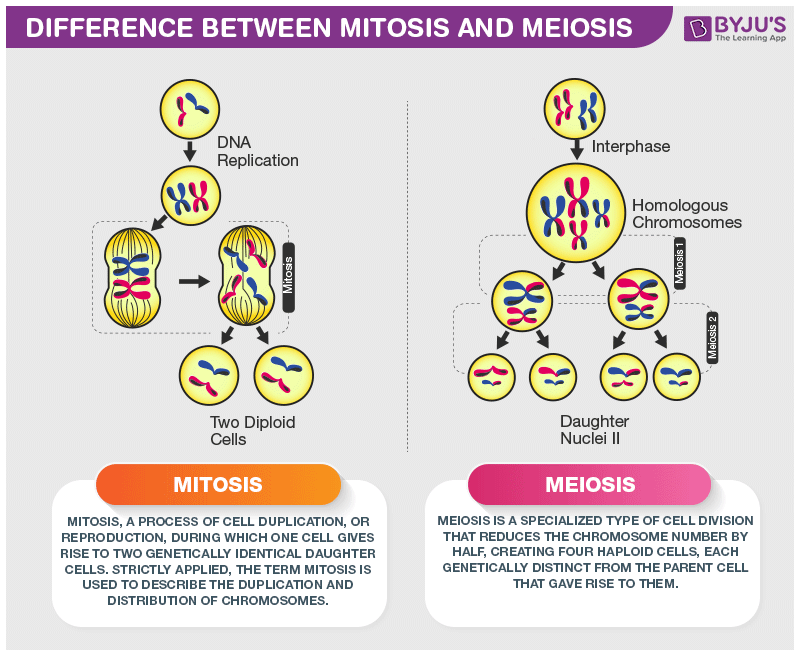
Meiosis
Process of cell division that results in gametes. Consists of two cell divisions that results in four cells, each of which contains half the number of chromosomes as the parent cell; occur in the testes and ovaries. It occurs only in the testes of males and ovaries of females.
4
New cards
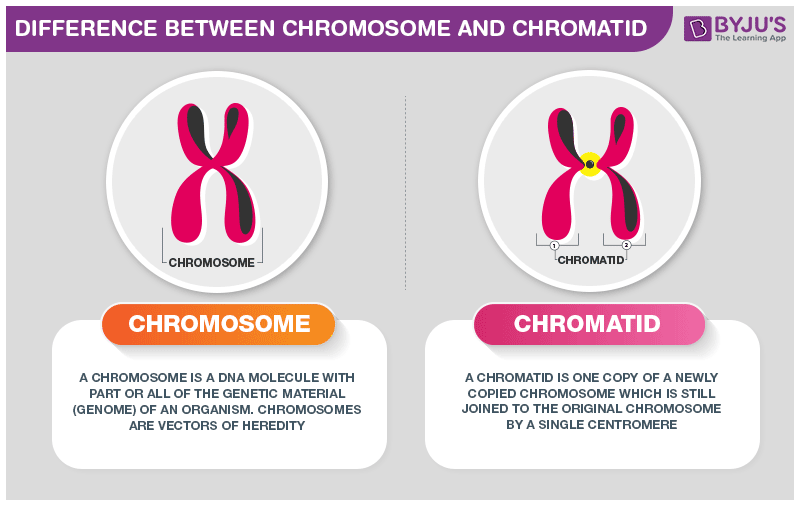
Chromatid
One of a pair of duplicated chromosomes, joined by the centromere, which separates from its partner during cell division.
5
New cards
Reduction Division
The first cell division of meiosis. The number of chromosomes in each cell is reduced from 46 (23 pairs) chromosomes to 23 total chromosomes.
6
New cards
Synapsis
Pairing of homologous chromosomes during prophase of the first meiotic division.
7
New cards
Crossing Over
An event that allows the exchange of genetic material between chromosomes. It occurs during prophase I of meiosis.
8
New cards
Male Reproductive System
Consists of the testes, a series of ducts (the epididymides, the ducta deferentia/vas deferens, and the urethra), accessory glans (the seminal vesicles, the prostate gland, and the bulbourethral glands), and supporting structures (the scrotum and penis).
9
New cards
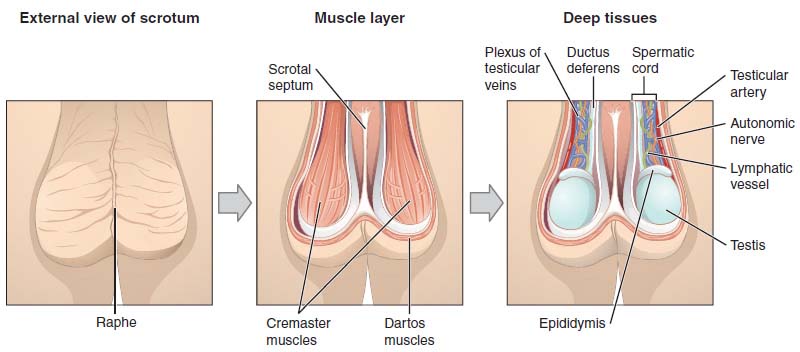
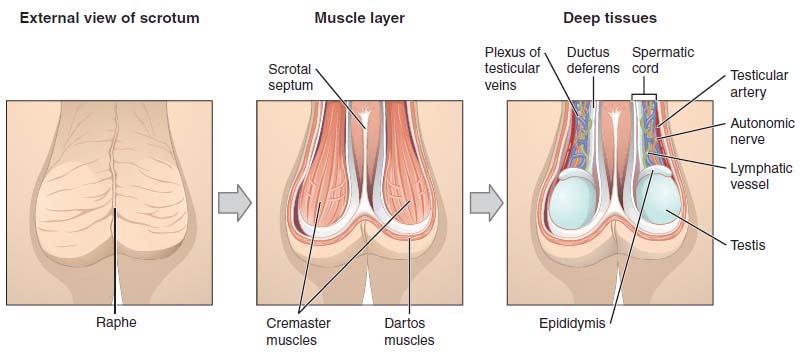
Scrotum
Saclike structure containing the testes. It is divided into right and left internal compartments by an incomplete connective tissue septum. The wall of this structure includes the skin, and a layer of smooth muscle tissue called the dartos muscle.
10
New cards
Dartos Muscle
Layer of smooth muscle beneath the skin of the scrotum. In cold temperatures, this muscle contracts, causing the skin of the scrotum to become firm and wrinkled and reducing its overall size.
11
New cards
Cremaster Muscle
Extension of abdominal muscles in the scrotum that contract and help pull the testes nearer the body. These changes in size and position of the scrotum help keep the testes warm.
12
New cards
Testes
Also known as the male gonads. These are oval organs, each about 4-5 cm long, within the scrotum. The outer part of each of these structures consists of thick connective tissue capsule. These organs produce testosterone and sperm cells.
13
New cards
Seminiferous Tubules
Tubules in the testes in which sperm cells develop.
14
New cards
Interstitial Cells
Endocrine cells located outside the seminiferous tubules. They secrete the hormone testosterone, and are also known as Leydig cells.
15
New cards
Spermatogenesis
The formation and development of sperm cells. It occurs in the seminiferous tubules.
16
New cards
Germ Cells
One of the two types of cells contained in the seminiferous tubules. These cells are the ones that divide and differentiate during spermatogenesis to form sperm cells.
17
New cards
Sustentacular Cells
One of the two types of cells contained in the seminiferous tubules that are also known as Sertoli cells. These cells are large and extend from the periphery to the lumen of the seminiferous tubule. They nourish the germ cells and produce a number of hormones.
18
New cards
Spermatogonia
Most peripheral germ cells in the seminiferous tubules scattered between the sustentacular cells; divide by mitosis and some form primary spermatocytes.
19
New cards
Spermatocyte
Cell arising from a spermatogonium and destined to give rise to spermatozoa.
20
New cards
Spermatid
Cell in the late stage of the development of the sperm cell (male gamete). It is haploid and is derived from the secondary spermatocyte.
21
New cards
Spermatozoon (pl. Spermatozoa)
Male gamete or sex cell, composed of a head, midpiece, and tail; contains the genetic information transmitted by the male; sperm cell.
22
New cards
Acrosome
A caplike organelle surrounding the anterior portion of a sperm cell, containing enzymes that facilitate entry of the sperm cell through the zona pellucida.
23
New cards
Zona Pellucida
Extracellular coat surrounding the oocyte; appears translucent.
24
New cards
Rete Testis
Network of canals at the termination of the straight portion of the seminiferous tubules.
25
New cards
Efferent Ductule
Small duct that leads from the testis to the epididymis.
26
New cards
Epididymis
Elongated structure connected to the posterior surface of the testis; site of storage and maturation of the sperm cells.
27
New cards
Capacitation
Process whereby the sperm cells develop the ability to fertilize oocytes. It occurs after ejaculation of semen into the vagina and prior to fertilization.
28
New cards
Ductus Deferens
Also known as vas deferens. It is a tube that carries sperm from the testis into the body cavity of the male. It runs from the epididymis to the ejaculatory duct and its total length is about 45 cm.
29
New cards
Spermatic Cord
Structure that contains the ductus deferens, the testicular artery and veins, lymphatic vessels, as well as the testicular nerve. It is also surrounded by the cremaster muscle and two connective tissue sheaths.
30
New cards
Ampulla of the Ductus Deferens
An enlargement of the vas deferens at its termination point just before the site where the duct of the seminal vesicle joins the ductus deferens. It functions as storage chambers for semen and contribute secretions to the seminal fluid.
31
New cards
Seminal Vesicle
Sac-shaped gland near the ampulla of each ductus deferens. It is one of two glandular structures that empty into the ejaculatory ducts; its secretion is one of the components of semen.
32
New cards
Male Urethra
Extends from the urinary bladder to the distal end of the penis. It serves as a passageway for both urine and male reproductive fluids.
33
New cards
It can be divided into three parts: (1) the prostatic urethra, (2) the membranous urethra, and (3) the spongy urethra.
34
New cards
Prostatic Urethra
One of the parts of the male urethra. It passes through the prostate gland.
35
New cards
Membranous Urethra
One of the parts of the male urethra. It passes through the floor of the pelvis and is surrounded by the external urinary sphincter.
36
New cards
Spongy Urethra
One of the parts of the male urethra. It extends the length of the penis and open at its end.
37
New cards
Penis
The male organ of copulation and functions in the transfer of sperm cells from the male to the female. It contains three columns of erectile tissue.
38
New cards
Erection
Engorgement of erectile tissue with blood, such as in the erectile tissue of the penis, causing the penis to enlarge and become firm.
39
New cards
Corpora Cavernosa
Two columns of erectile tissue that form the dorsal portion and the sides of the penis.
40
New cards
Corpus Spongiosum
The third, smaller erectile column that occupies the ventral portion of the penis. It expands over the distal end of the penis to form a cap, the glans penis.
41
New cards
Prepuce
Also known as the foreskin. It is a loose fold of skin that cover the glans penis.
42
New cards
Circumcision
The surgical removal of the prepuce, usually short after birth. This surgery can be necessary to avoid chronic infections and maintain normal circulation.
43
New cards
Prostate Gland
Consists of both glandular and muscular tissue and is about the size and shape of a walnut. It surrounds the urethra and two ejaculatory ducts. The secretion of this gland is a milky fluid that is discharged into the urethra as part of the semen. This secretion regulates pH and aids in sperm cell travel to the oocyte.
44
New cards
Bulbourethral Glands
Also known Cowper glands. They are a pair of small, mucus-secreting glands located near the base of the penis. It produces a mucous secretion just before ejaculation that aids in sperm movement and survival as the sperm enter the female reproductive tract.
45
New cards
Semen
A mixture of sperm cells and secretions from the male reproductive glands. The seminal vesicles produce about 60% of the fluid, the prostate gland contributes approximately 30%, the testes contribute 5%, and the bulbourethral glands contribute 5%.
46
New cards
Prostaglandins
Hormones secreted by the seminal vesicle that stimulates smooth muscle contractions of the female reproductive tract to propel sperm cells through the tract.
47
New cards
Gonadotropin-Releasing Hormone (GnRH)
Hypothalamic hormone that stimulates the secretion of LH and FSH from the anterior pituitary gland.
48
New cards
Testosterone
Steroid hormone secreted primarily by the testes; aids in spermatogenesis, controls maintenance and development of male reproductive organs and secondary sexual characteristics, and influences sexual behavior.
49
New cards
Puberty
Time period during which individuals become capable of sexual reproduction. The reproductive system matures and assumes its adult functions, and the structural differences between males and females become more apparent.
50
New cards
Follicle-Stimulating Hormone (FSH)
Hormone of the anterior pituitary glands that, in the female, stimulates the follicles of the ovary, assists in the maturation of the follicle, and causes secretion of estrogen from the follicle; in the male, it stimulates the epithelium of the seminiferous tubules and is partially responsible for inducing spermatogenesis.
51
New cards
Luteinizing Hormone (LH)
Hormone of the anterior pituitary glands that, in the female, initiates final maturation of the follicles, their rupture to release the oocyte, the conversion of the ruptured follicle into the corpus luteum, and the secretion of the progesterone; in the male, it stimulates the secretin of testosterone in the testes and is sometimes referred to as interstitial cell-stimulating hormone (ICSH).
52
New cards
Secondary Sexual Characteristics
Structural and behavioral changes, other than in the reproductive organs, that develop at puberty and distinguish males from females. It includes hair distribution and growth, skin texture, body fat distribution, skeletal muscle growth, and changes in the larynx.
53
New cards
Emission
The accumulation of sperm cells and semen in the urethra. It is stimulated by sympathetic action potentials that originate in the lumbar region of the spinal cord.
54
New cards
Ejaculation
The forceful release of semen from the urethra. It results from the contraction of smooth muscle in the wall of the urethra and skeletal muscles surrounding the base of the penis.
55
New cards
Orgasm
Climax of sexual act, often associated with a pleasurable sensation.
56
New cards
Resolution
Phase that occurs after ejaculation. In this phase, the penis becomes flaccid, an overall feeling of satisfaction exists, and the male is unable to achieve erection and a second ejaculation.
57
New cards
Inhibin
Hormone produced by the sustentacular cells of the male reproductive system. It inhibits FSH secretion through negative feedback.
58
New cards
Estrogen
A hormone produced by the follicles of ovaries and corpus luteum. Its functions are:
- Proliferation of endometrial cells.
- Development of mammary glands (especially duct systems).
- Positive feedback before ovulation, resulting in increased LH and FSH secretion; negative feedback with progesterone on the hypothalamus and anterior pituitary after ovulation, resulting in decreased LH and FSH secretion.
- Development and maintenance of secondary sexual characteristics.
- Proliferation of endometrial cells.
- Development of mammary glands (especially duct systems).
- Positive feedback before ovulation, resulting in increased LH and FSH secretion; negative feedback with progesterone on the hypothalamus and anterior pituitary after ovulation, resulting in decreased LH and FSH secretion.
- Development and maintenance of secondary sexual characteristics.
59
New cards
Progesterone
A hormone produced by the corpus luteum. Its functions are:
- Enlargement of endometrial cells and secretion of fluid from uterine glands; maintenance of pregnant state.
- Development of mammary glands (especially alveoli).
- Negative feedback, with estrogen, on the hypothalamus and anterior pituitary after ovulation, resulting in decreased LH and FSH secretion.
- Enlargement of endometrial cells and secretion of fluid from uterine glands; maintenance of pregnant state.
- Development of mammary glands (especially alveoli).
- Negative feedback, with estrogen, on the hypothalamus and anterior pituitary after ovulation, resulting in decreased LH and FSH secretion.
60
New cards
Oxytocin
A hormone released by the posterior pituitary that stimulates contraction of uterine smooth muscle and contraction of cells in the breast, resulting in milk letdown in lactating females.
61
New cards
Human Chorionic Gonadotropin (hCG)
A hormone produced by the placenta that maintains the corpus luteum and increases its rate of progesterone secretion during the first one-third (first trimester) of pregnancy; increases testosterone production in testes of male fetuses.
62
New cards
Erectile Dysfunction (ED)
Failure to achieve erections. It is also sometimes called impotence and can be a major source of frustration. This condition can be due to reduced testosterone secretion resulting from hypothalamic, pituitary, or testicular complications. It can also be due to defective stimulation of the erectile tissue by nerve fibers or reduced response of the blood vessels to neural stimulation.
63
New cards
Infertility
The inability or the reduced ability to produce offspring. In males, the most common cause of this condition is low sperm cell count.
64
New cards
Artificial Insemination
Process by which concentrated sperm cells are collected through several ejaculations and inserted into the female reproductive tract.
65
New cards
Female Reproductive System
Consists of the ovaries, the uterine/fallopian tubes, the uterus, the vagina, the external genitalia, and the mammary glands.
66
New cards
Broad Ligament
The ligament that spreads out on both sides of the uterus and attaches to the ovaries and uterine tubes.
67
New cards
Suspensory Ligament
The ligament that extends from each ovary to the lateral body wall.
68
New cards
Ovarian Ligament
The ligament that attaches the ovary to the superior margin of the uterus.
69
New cards
Mesovarium
Mesentery of the ovary; mesentery that attaches the ovary to the posterior surface of the broad ligament.
70
New cards
Oogenesis
The production, growth, and maturation of an egg, or ovum.
71
New cards
Oocyte
Female gamete or sex cell; a secondary oocyte and a polar body result from the first meiotic division, which occurs prior to ovulation; a zygote and a polar body result from the second meiotic division, which occurs following union of the sperm cell with the secondary oocyte.
72
New cards
Oogonia
Cell that gives rise to oocytes; has a diploid number of chromosomes.
73
New cards
Theca
A capsule that forms around the secondary follicle.
74
New cards
Antrum
A single, fluid-filled chamber that is formed by the fusion of fluid-filled vesicles.
75
New cards
Cumulus Cells
Granulosa cells located in the vicinity of the oocyte.
76
New cards
Ovulation
Release of a secondary oocyte from a mature follicle.
77
New cards
Polar Body
Oocyte receiving little cytoplasm; results from the first and the second meiotic division.
78
New cards
Fertilization
Union of the sperm cell and oocyte to form a zygote. It begins when a sperm cell penetrates the cytoplasm of a secondary oocyte. It returns the chromosome number back to 46.
79
New cards
Corpus Luteum
Yellow endocrine body formed in the site of a ruptured follicle immediately after ovulation; secretes progesterone and estrogen.
80
New cards
Corpus Albicans
Remnants of the degenerated corpus luteum. It forms if pregnancy does not occur after ovulation has been completed.
81
New cards
Uterine Tube
Also known as fallopian tubes or oviduct. It is a structure associated with each ovary and extends from the area of the ovaries to the uterus. They open directly into the peritoneal cavity near each ovary and receive the secondary oocyte.
82
New cards
Fimbriae
Long, thin processes that surrounds the opening of each uterine tube. They also nearly surround the surface of the ovary.
83
New cards
Ampulla
Part of the uterine tube near the ovary wherein fertilization usually occurs.
84
New cards
Implantation
Process by which the fertilized oocyte (zygote) travels to the uterus and embeds itself into the uterine wall.
85
New cards
Uterus
Hollow muscular organ in which the fertilized oocyte develops into a fetus. It is as big as a medium-sized pear and is oriented in the pelvic cavity with the larger, rounded part directed superiorly.
86
New cards
Fundus
The part of the uterus superior to the entrance of the uterine tubes.
87
New cards
Body
The main part of the uterus.
88
New cards
Cervix
The narrower part of the uterus that is directed inferiorly.
89
New cards
Uterine Wall
Composed of three layers: the perimetrium, the myometrium, and the endometrium.
90
New cards
Perimetrium
Outer serous layer of the uterine wall. It is formed from visceral peritoneum and is also simply known as the serous layer.
91
New cards
Myometrium
Middle layer of the uterine wall that consists of smooth muscle, is quite thick, and accounts for the bulk of the uterine wall. It is also known as the muscular layer.
92
New cards
Endometrium
The innermost layer of the uterine wall. It consists of simple columnar epithelial cells with an underlying connective tissue layer. The superficial part of this layer is sloughed off during menstruation.
93
New cards
Spiral Glands
Simple tubular glands formed by the folds of the endometrium.
94
New cards
Prolapsed Uterus
A condition wherein the ligaments that support the uterus or the muscles of the pelvic floor are weakened, as may occur due to childbirth. As a result, the uterus can extend inferiorly to the vagina and may require surgical correction if severe.
95
New cards
Vagina
The female organ of copulation; it receives the penis during intercourse. It allows menstrual flow and childbirth. It extends from the uterus to the outside of the body.
It consists of an outer muscular (smooth muscle with many elastic fibers) layer that helps increase its size, as well as an inner mucous membrane composed of moist stratified squamous epithelium that forms a protective layer.
It consists of an outer muscular (smooth muscle with many elastic fibers) layer that helps increase its size, as well as an inner mucous membrane composed of moist stratified squamous epithelium that forms a protective layer.
96
New cards
Hymen
A thin mucous membrane that covers the vaginal opening of young females. It is most commonly perforated by one or several holes. It is usually greatly enlarged during the first sexual intercourse; however, it can also be perforated or torn earlier in a young female's life during a variety of activities, including strenuous exercise.
97
New cards
Vulva
Also known as the pudendum. It is the external female genitalia that consists of the vestibule and its surrounding structures.
98
New cards
Vestibule
The space into which both the vagina and the urethra open. The urethra opens into this structure just anterior to the vagina.
99
New cards
Labia Minora
Two narrow, longitudinal folds of mucous membrane enclosed by the labia majora; they unite anteriorly to form the prepuce. These folds also border the vestibule.
100
New cards
Labia Majora
Two rounded folds of skin surrounding the labia minora and vestibule.