COPD
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Define COPD
•Chronic Obstructive Pulmonary Disease
→Common, preventable, treatable
1)Airflow limitations
2)Abnormal inflammatory response
3)Increased mucus production
Progressive disease worsens over time
Persistent respiratory symptoms (this is different that asthma)
Describe how COPD can impact patient’s daily lives
•Difficulty with physical activities
•May not be able to wrok
•Hard to engage in social activities
•Increased confusion, memory loss, depression
•More emergency room visits
Is COPD more or less prevalent in rural communities?
•More prevalent (Double)
How does COPD prevalence and disease severity differ among females versus in males? How does COPD prevalence differ across ethnicity?
•More females die from COPD, and COPD is likely underdiagnosed in women
•Inequities across ethnicities most notable being American Indian and Alaskan Native descent
Describe the characteristics of patients in Wisconsin with COPD.
•Above the age of 65
•Less than a high school diploma
•Low income
•Divorced/widowed/separated
•Current or former smoker
•Have had asthma
What are the two underlying disease processes that lead to COPD?
Emphysema
Chronic Bronchitis
Emphysema
•Destruction of lung parenchyma leads to decreased lung elastic recoil
Symp: SOB, wheezing
Chronic Bronchitis
•Mucus overproduction leading to inflamed narrow airways, cilia destruction
Symp: Cough, mucus, wheezing
What impact can COPD have on lung parenchyma? What is the outcome of this?
•Destruction of lung parenchyma leads to decreased lung elastic recoil
What is the test that is required to diagnose COPD? What are the specific parameters within this test that must be met for a COPD diagnosis?
Spirometry:
FEV1/FVC <0.70
GOLD IV: Very Severe
FEV1 < 30% predicted
GOLD III: Severe
30% < FEV1 <50% predicted
GOLD II Moderate
50% < FEV1< 80% predicted
GOLD I Mild
FEV1>80% predicted
symptoms of COPD
Dyspnea: Shortness of breath
Chronic cough (often first symptom)
Chronic Sputum production
Wheezing, chest tightness
Lower respiratory tract infections
What is the age cutoff for a COPD diagnosis?
40 years old
What are the risk factors for COPD?
Exposure to particles
Socioeconomic status
Age and Sex
Genes
Asthma, chronic bronchitis
Childhood lung development & respiratory infection
What are our goals of therapy for COPD management?
Decrease symtpoms
Prevent disease progression
Prevent and treat exacerbations
Reduce mortality
LAMA nebulizers
Lonhala Magnair Nebulizer→ Glycopyrolate
Yupelri Nebulizer→ Revefenacin
What are the common and rare/severe side-effects of LAMAs?
Common: Dry mouth, bitter taste, nasopharyngitis
Rare: worsening narrow angle glaucoma, worsening urinary retention
Are cardiac risks a significant concern with LAMA use?
NO
What are some considerations regarding use of Yupelri?
Do not give with anticholinergic agents
Do not give with OATP1B1 and OATP1B3 inhibitors
Can LAMAs be used as monotherapy maintenance treatment for COPD?
sure
LABA Nebulizers
Brovana Nebulizer→ Aformoterol
Perforomost Nebulizer → Formoterol
What are the common and rare/severe side-effects of LABAs?
Common: Dry mouth, cough, nasopharyngitis
Rare: can produce sinus tachycardia, cardiac rhythm disturbances
In which type of patient might we consider monitoring more closely for cardiac rhythm disturbances?
QTC prolonging agents may potentiate effects of LABA on CV system
Monitor carefully in patients with CV disorder
Can LABAs be used as monotherapy maintenance treatment for COPD?
CAN be used as monotherapy for mild or moderate COPD
NOT rescue med
What are some unique considerations with Anoro?
Caution with ketoconazole and other strong CYP3A4 inhibitors
Summarize the role of bronchodilators (LAMAs and LABAs) for COPD management. Can they ever be used together? When?
LABA/LAMA combo therapy is commonly used as step up therapy in COPD if a patient remains symptomatic/ increase exacerbations on LAMA or LABA monotherapy
Are ICSs ever used as monotherapy for COPD?
NO
What is the “place in therapy” for ICS/LABA or ICS/LABA/LAMA treatment in COPD?
What was the ETHOS trial, and what did it demonstrate regarding ICS treatment?
Exacerbation reduction with triple therapy as comapred to ICS/LABA and LABA/LAMA
Higher eisoinophil counts may identify pateints with greater likelihood of beneficial ICS response
Describe patient-specific factors that may increase the risk of pneumonia with ICS treatment.
Eosinophil counts
Prior history pnuemonia
Over 55
BMI <25
Current smokers
STRONGLY favors use of ICS
History of hospitalizations for COPD exacerbations
2 or more moderate exacerbations of COPD per year
Blood eosinophils 300 or more
Asthma or history of asthma
FAVORS use of ICS
1 moderate exacerbation of COPD per year
Blood eosinophils 100-300
AGAINST ICS use
Repeated pneumonia events
Blood eosinophils <100
History of mycobacterial infeciton
MMRC
Modified Medical Research Council Dyspnea
→ 0 (minimal dyspnea) to 4 (significant dyspnea)
CAT
COPD Assessment Test
→ <10 low
→ 10-20 medium
→ >20 high
→ >30 very high
Higher score worse
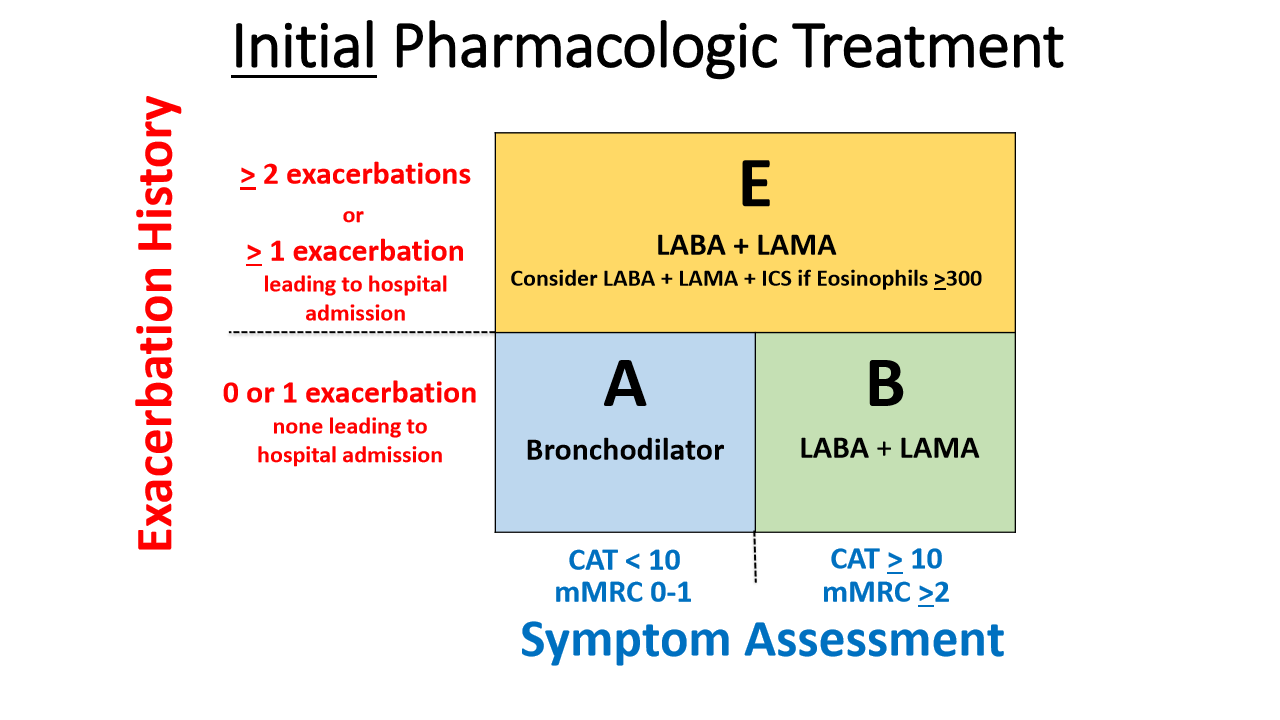
Draw the inital pharmacologic treatment boxes thing
roflumilast side effects, interaction
Side effects: Psychiatric events, Weight loss
Drug interactions: Do not use with strong CYP450 inducers
Contraindications: Liver impairment
Describe specifics regarding azithromycin and when this therapy might be used in COPD management.
Patients with severe COPD who are NOT current smokers. Only been studied for 1 year.
Side effects:
Impaired hearing
QTc prolongation
Increased bacterial resistance
True or false: theophylline, antioxidants, and expectorants are all very effective and safe treatment strategies for COPD management
FALSE