intro in pharmacology (10)
1/114
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
115 Terms
what is a drug?
a chemical substance which produces
eg could increase heart rate , pressure a specific physiological response within the body
what is a medicine
it is a preparation given for the treatment or prevention of disease
can be a drug or eexcipients: inactive ingredients
supports the drug, has an active ingredient in there which helps the drug perform well
what types of medicines are the eyes related to
diagnostic
therapeutics: bacterial conjunctivitus , blood vessels dilate
most px will be taking medications which could cause issues for the eye

how does a drug affect the body
pharmacodynamics
happening at a cellular level: the process is underpinned by drugs binding to proteins in or on cells. drugs influence the biochemical processes occuring in the cell
impact of tissues, organs → effects seen in organ systems
eg. topical anaesthetic eg lidocaine
eg targets nerve cells → stops sensation of pain, touch as cornea is very sensitive
eg used to numb cornea in contact tonometry
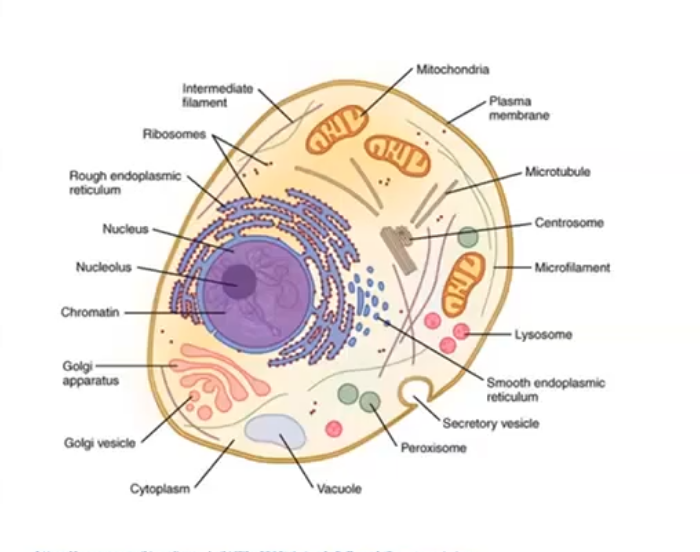
animal cells
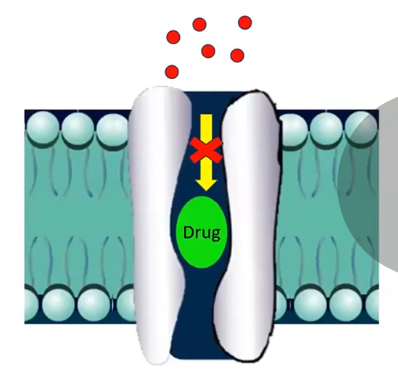
if drug finds it hard to enter the cell it acts on the protiens on the outside eg the glycolipids or glycoproteints of the cell membrane
phopholipid bilayer: hydrophillic heads pointing out hydrophobic tail in layer
drugs find it hard to cross the bilayer

cell membrane
regulates what goes into or out the cell
phopholipid bilayer: phosphate heads are hydrophillic
lipid tails are hydrophobic: forms a stable layer in water free area between inner and outer layers of the membrane
proteins embedded, some act as carriers, some act as channels, some stick out the edge to form receptors
cholesterol for stability of structure
what is the cell membrane mainly made from
mianly made from lipid:
this influences which drugs can pass through
most drugs unable to pass through unaided
therefore effects exerted on membrane bound extracellular proteins
proteins
chain of amino acids
20 different amino acids in human proteins
determined by length of chain, order of amino acids, folding into the 3d shape
20,000 diff proteins
why do proteins make good drug targets
lots of different proteins means lots of potential targets
involved in many key physoological processes
certain proteins are only found in certain sites eg the heart has specific proteins so need drugs to target those exact proteins
what are the 4 main protein targets of drugs
the molecule of a drug must bind to a target to produce an effect
targets on/in a cell:
receptors
ion channels
carrier molecules
enzymes
drug target 1: receptors
chemical messengers released allow communication and coordination between/within different cells tissues and organs:
common messengers are usuall:
hormones
neurotransmimtters like acetylcholine and noradrenaline which is important for pupil dilation
mediators: histamine which is important for ocular allergies,like from allergic conjunctivitis
when allergic respinse occurs, histamine is released which makes bv more permeable causing them to leak
whats a receptor
a site of tissue or molecule in a cell membrane that responds specifically to these messengers
the messengers bind to the receptor to initiate a response
may be referred to as a ligans which is used to describe a drug that binds to a receptor
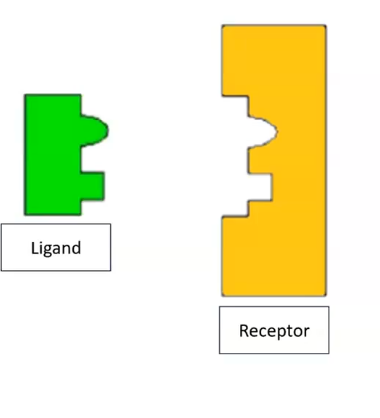
ligand and receptors
ligans is the appropriate shape to fit into a receptor; eg lock and key
right shape = specificity : only that ligand will bind to particular receptor
binding cayses small change to the receptor site: triggers intracellular activity within the cell
when ligand binds to receptor activity is triggered
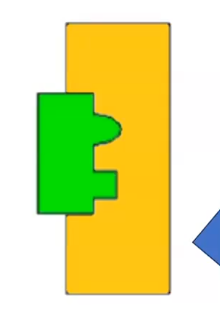
drugs and receptors
drug is mimicking the ligand and will bind to the receptor, preventing the ligand rom binding
if the drug initiates a response and an activity is produced then this is known as an agonist . 2 drugs that work together
if drug does not initiate a respinse/ prevents one then it is an antagonist drug. no activity is produced
agonist
bind to receptors and have the same effect as the ligand
it is a drug that replicates the action of a neurotransmitter
what is a direct acting agonist
similar strucure to the transmtter and duplicates the action of the neurotransmitter by acting on receptor sites of the effector
what is an indirect acting agonist
cause the action to occur either by exciting the nerve fibre , thereby causing a release of the transmitter or by oreventing the recycling or reuptake of the transmitter, thus allowing it to continue its activity ]
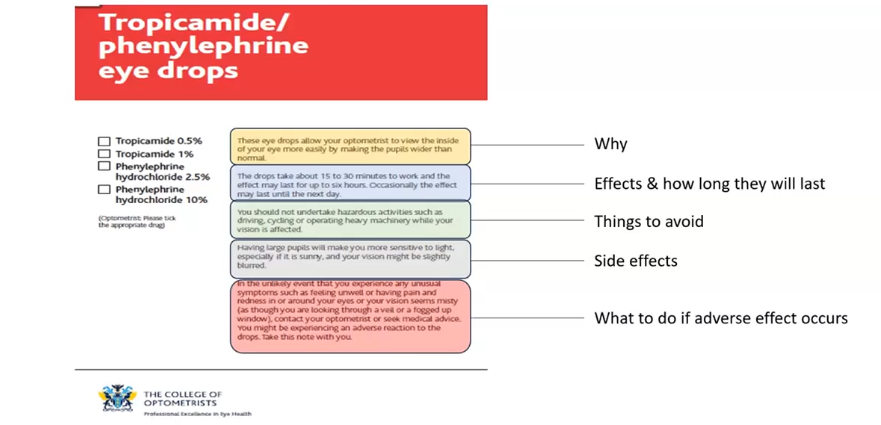
phenylephrine
mimics the neurotransmitter that stimulates the iris radial muscles
causes pupil to get bigger
antagonists
either block the receptor sites or block the release of the neurotransitter thus preventing action of the effector
has affinity but no efficacy
tropicamide
it is an agononist
it blocks receptor sites on the iris sphincter muscle
temporarily paralyses the iris sphincter
pupil not able to constrict
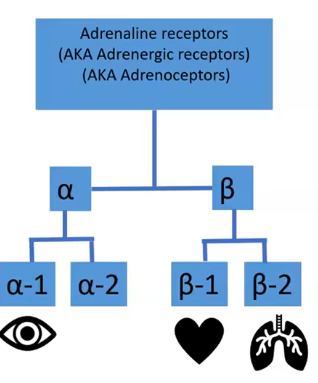
sub types of receptors
receptors belong to families; have classes and sub classes
drugs can be targeted at specific sub types of receptors
but they may accidently bind to other receptors of that class= unwanted side effects
eg phenylephrine stimulates alpha-1 sub type in the iris
drug target 2: ion channels
ion channels: atoms or molecules that carry a small charge
makes them more stable eg Na + are highly reactive in elemental uncharged state
= + cation , - anion
many processes rely on ions moving across cell membranes eg filteration of waste by kidneys, heart beats etc
channels regulate passage of ions across the cell membrane ]specific to their own ion eg potassium channels
can use a drug to block passage pf ions to prevent a response or make one occur
eg drug effects on ion channels
drug inserts itself into the channel, blocking the passage of ions
eg lidocaine
topical anaesthetics used by optometrists to numb the cornea
sodium ions cant move across so ap isnt generated,
drug target 3: carrier molecules
proteins using ATP to actively transport substance across the cell membrane
could be transporting ions and neurotransmitters
eg fluoxetine block transporters for seratonin
drug target 4: enzymes
most biochemical reactions happening in each cell are catalysed by enyzmes
drugs generally inhibit enzymes : might be one step or might inhibit one step of a pathway
eg statins inhibit HMG CoA reductase : reduces cholesterol
ADME
how does a drug get to its site of action
why are some medicines swalled, others injected , inhaled
why do some drugs last longer than others
A: absorbs: how does it get into the body
B: distributes: where does it go
M: metabolites: how its broken down
E: eliminates drugs: how does it leave
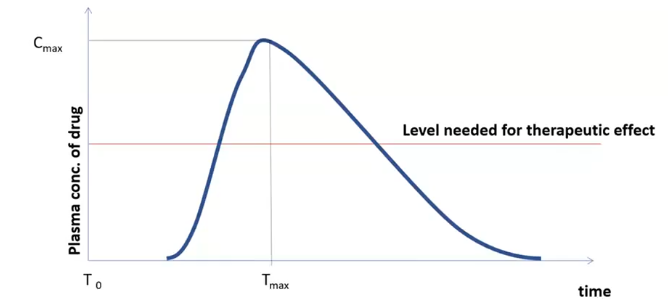
oral dose of a drug: pharmacokinetic curve
at more blood reaches the plasma, the concentrtion of plama of drug rises and peaks
then drops
can work out amount of plasma needed for a max response
need the drug to reach certain threshold for it to work
when drops the pain eg might be returning here
at beginning the drug is disintegrating, absorpting and distrubuting itself to areas of the body, and by the time it drops, metabolism slows, extretion and storage occurs
drug administeration
progresses from initial dosage → biologically available form which can pass through or acorss tissues
3 pathways
topical : applied diectly to the site where the drug needs to act ey eye drops
enteral: absorbed into the bloodstream via digestive tract eg tablets
parentral: introduced directly into the body NOT via digestive system eg insulin injection, inhaler
enteral administeration
passes through the oesophagus , down into the stomach, then to the small intestine then to the large intestine
the drug itself needs to be able to survive the harsh conditions of the stomach
drug absorbed in the stomach and/or small intestine so it can reach the circulatory system
once absorbed into the blood stream it will encounter the liver
absorption in the stomach or small intesitne → liver → systemic circulation
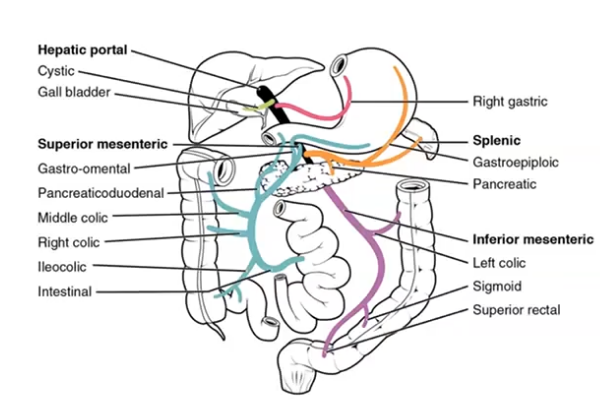
first pass metabolism
grugs are absorbed from the GI tract pass into the hepatic portal vein : travels directly to the liver
all of the substances that we absorb from the gut will first pass through the liver
steps of first pass metabolism
drug is absorbed by the gi tract
travels immediately to the liva via hepatic portal vein
metabolised by enzymes in the liver- can be to such extent that most of drug doesnt reach the systemic circulation
remaining drug is distribued around the body by circulatory system
drug distribution
drugs distributed around the body via the bloodstream - very few drugs exert in the blood itself
drugs need to move out of the bloodstream into the intersitual fluid to act on target proteins in/on cells
drugs are not evenly distributed throughout the body
many drugs do not travel dissolved in blood: bind to proteins in the blood
only the free unbound drug that is available to have a therapeutic effect
plasma protein binding
proteins in blood can help or hinder drug response
in the blood drug can be bound to proteins or unbound
bound drugs
bound to plasma proteins eg albumin
protein +drug = protein drug complex
which reduces the amount of drug free to have a pharmacological effect
drug plasma protein forms a resevoir of drug , but only the free unbound drug is available to the tissues to exert a therapeutic effect
helps drugs reach regions remote to administeration site
hinders as when bound, cannot readily leave the capillaries and affect target tissues
effect of drug solubility
aqueous solubility:
water soluble drugs have difficulty crossing cell membranes, so will remain in circulation , stay in bloodstream and in danger of being excreted
they are cleared by the liver or kidneys so little practical use
lipid solubility
enters the cell readilt therefore widespread distribution, easier to cross cell membranes so reach target
cell membrane as barriers to drug movement
polar molecules are hard to cross the cell membrane
cell membranes are mainly lipid, barrier to molecules excpet lipids , lipid soluble substances diffuse easily through the lipid bilayer
most drugs are lipid soluble in their unionised form whereas ionised forms are not
lidocaine swithces from ionised to unionised form : kept in acidid form to stay ionised, and unionsies when goes into the eye so it can pass through cell membrane
extent to which drug is ionised depends on local pH. kept in acidic standards
drugs that are polar or ionised are less anle to cross membranes which is why drugs often interact with proteins on the outside of the cells
drug metabolism
changing drugs via chemical reactions into compounds that are easier to eliminate
need to break down the drug into its metabolites
products of these chemical reactions= metabolites
as drugs are metabolised, their therapeutic effect diminshes , the drugs become less active ( but not always)
non polar drugs molecules are changed into polar molecules
usually metabolism decreases biological activity but may increase, retain or change
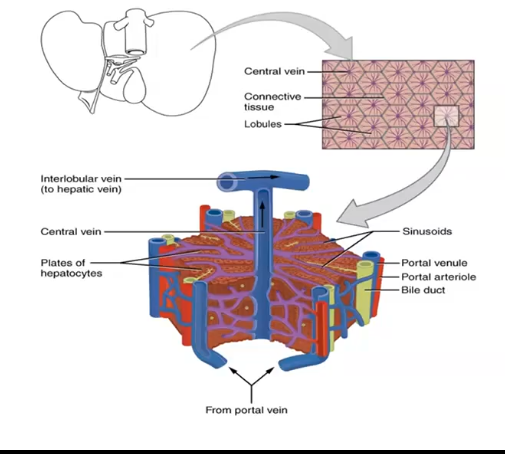
role of the liver in metabolism
blood being brought form hepatic portal vein reaching nutrients
moves through the sinusoids , and mix with enzymes and leave
main metabolic site= liver
perfused by blood containing frug from the gut
high conc of drug metabolising enzymes compared to other parts of the body
enzymes are key facilitators of durg metabolism:
aim of metabolism is to transform substances into a form that is easier for the kidneys to excrete
cytochrome P450
large family of enzymes
orally administered drugs will all pass through the liver and P450 metabolism
extent of metabolism will determine the amount of drug that makes it into circulation and is available to target sites
diseases that affect the liver = reduced ability to metabolise drug
more will circulate in the body , so harder to break down so will stay in the bloodstream
drug metabolism: phase 1 reactions
modification
most common type: oxdation
aims to intoduce or expose functional groups: increase in polarity of compound
drug metabolism: phase 2 reaction
conjugation
attachment of an ionised group to the drug
makes drug more water soluble
what is a prodrug
most drugs become less active/useful once metabolised by prodrugs do not
a prodrug is pharamcologically inactive when administered, remain inactive until metabolised
converted into active metabolite once it is metabolised
why do we use prodrugs
active drug may be diffiuclt to administer
to enhance absorption - allows to use a low quantity of the drug so easier to pass barriers
protects from rapid metabolism
overcomes toxicity problems
could be used to increase ocular drug penetration or if active drug might vause issues outside the eye eg allergy
drug elimination
excretion: removing a drug and its metabolites from the body
major routes= via the kidneys and also bile/intestines
other routes: lungs, sweat, salica, tears, milk
will be issues if patient has kidney issues as excretion is limited
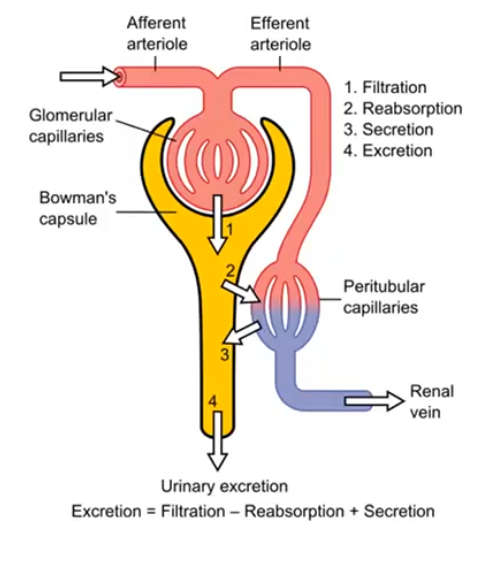
what 3 processes facilitate excretion in the kidney nephron
glomerular filteration
tubular secretion
tubule reabsorption
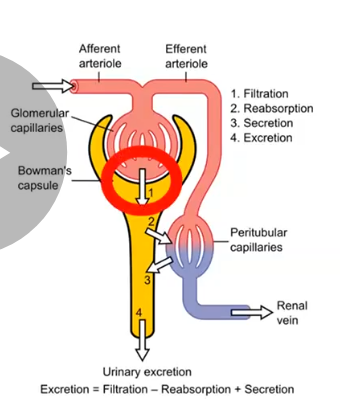
filteration at the glomerulus
hydrostattic pressure of blood flowing in capillaries drives glomerular filteration
pushes the blood acorss semi permeable membrane into bowmans capsule
allows molecules polar and non polar up to size of small proteins to move from blood into nephron
drugs which are protein bound will not cross the barrier
so small molecules can leave the blood to be exctreted
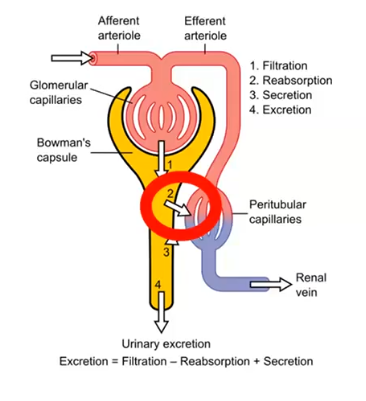
active secretion
this is how majority od the drugs enter the tubule
acitve as it is going against the concentration gradient : from cappilaries into the tubule
there are 2 carrier systems: one for basic dugs one for acidic drugs
if prolonged drug effect is required, agents can be administeed to block tubule secretion to slow excretion, and stay in bloodstream longer
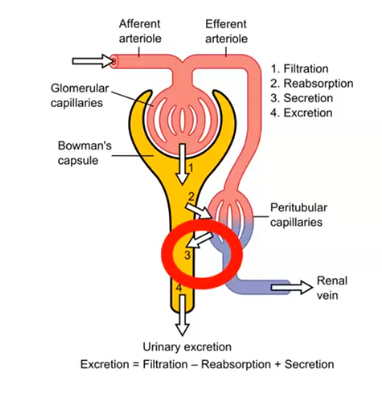
passive reabsorption
some of the drugs once in tubule will pass back into the blood stream from tubule
drugs enter the tubule, but could then be reabsorbed back into the blood
occurs via passive diffusion
majority of the water that has entered the nephron is reabsorbed back into the blood, and takes lipid soluble drugs with it. this increases time taken to eliminate lipid soluble drugs
drug specificity
usefulness of drug depends on its ability to act on a particular receptor
two way process: certain classes of drugs bind to certain receptors, or certain receptors recognise certain ligands
no drug has complete specifity - doesnt just stimulate just 1 receptor : other targets may be activiates, leading to side effects
affinity
the strength of attraction between a drug and its receptor - probability of a drug occupying a receptor at any given instant
high affininty high probability
high affininty on its own doesnt always produce a high response - eg antagonists may have a high affinity but produce no response
lab measure= conc of a drug required to occupy 50% the available receptors
eficacy
AKA intrinsic activity : measure of the ability of the drug to activate receptor and lead to a cellular response
measure of mgnitidue of the effect once drug is bound to receptor
max response achieved by a drug -
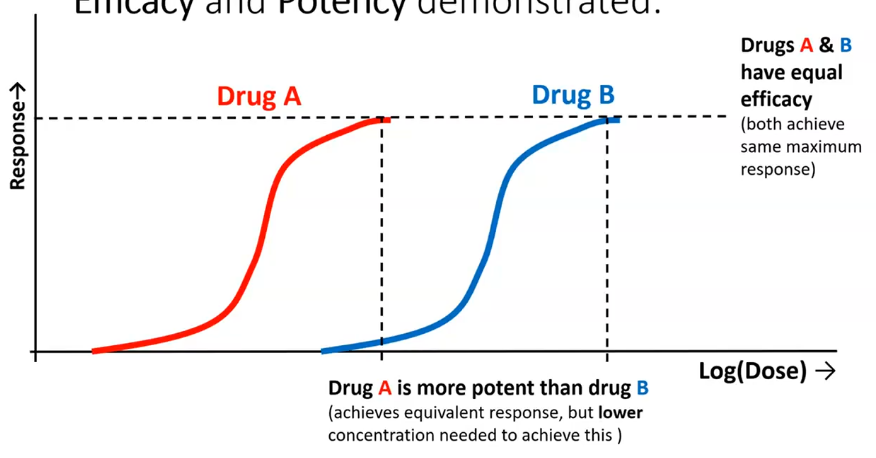
potency
the dose required to produce a specific intensity of response
highyl potent drug evokes a response at low concentrations
lower potency would need a higher concentration
ED50 can be a good indicator of potency ( effectice dose in 505 of population)
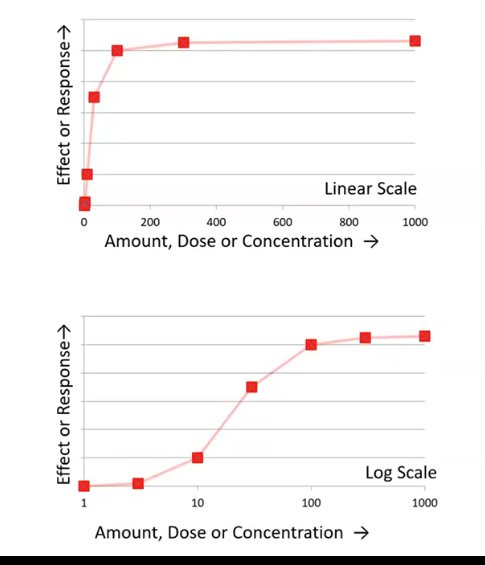
dose response curves
graph which tracks the response to various conc or doses of a drug
quantiative relationship between physiological responses and conc of agonist
respons could be heart rate , blood pressuer etc
will eventually hit a plateu: doses more than 400 will have on effect on response
on log scale: raph stretched out so shows a conc can magnify the response with the dose
efficacy and potency demonstrated
comparing drug a and b
both drugs have equal efficiacy as both ahieve max response
have different potency
drug a is more potent than drug b as less conc is needed from a to achieve the same efficiacy than drug b
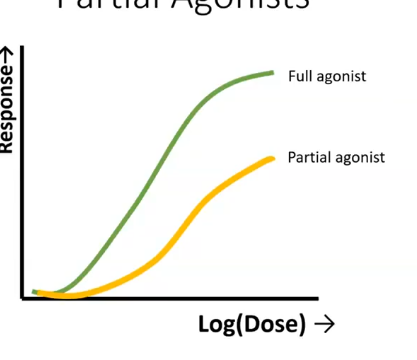
partial agonist
full agonist: max response prodyced by a drug = max response tissue can give
partial agonists: elicits a max respnse which falls short of thr max response tissue can give
has partial efficacy
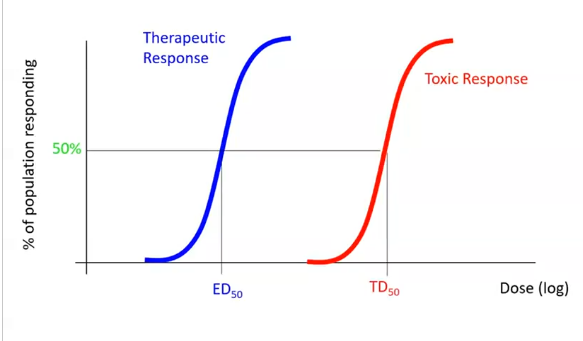
therapeutic index
measuring percentge of population that gets the response we want
low dose then 0% will be cured
can also track toxi respinse/ bad side effects of the same drug
higher dose, then greater proportion will experience a toxic response
therapeutic index is the gap between the 2 curves
TD50= dose that gives a toxis response in 505 of population
ED50= dose that is therapeutically effectice in 50 % of populatio
safer drug= larger TI/larger gap
large dose needed for a toxic response and small effective dose needed
competitive antagonists
competes with agonists for the binding site
without activation
increasing the agonist conc can overcome this as shifts our dose-response curve to the RIGHT
balance will be dtermined by relative affinity of each molecule for binding site
non competitive antagonist
does not compete with agonists for the binding site
agonist and antagonist can be bound to receptor simultanouesly
still opposes the action of the agonist
effect is to reduce the maximal effect produced
effect cant be reversed by increasing agonist conc
reversible competitive antagonist
will eventually dissociate from the receptor
frees the receptor to be occupied again
eg tropicamide
cyclopentolate is reversable antagonist that temporarily inhibits the accom response
irreversible competitive antagonist
binds permanently to a receptor
strong bond to the receptor
permanently deactivates
body produces new set of receptors
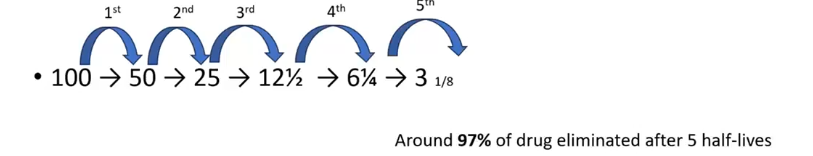
plasma half life
the amount of time it takes for the conc of the drug in your plasma/drug to decrease by 50%
measures of how long a drug stays in the body
can indicate duration of action
drugs with a short half life need more frequent dosing
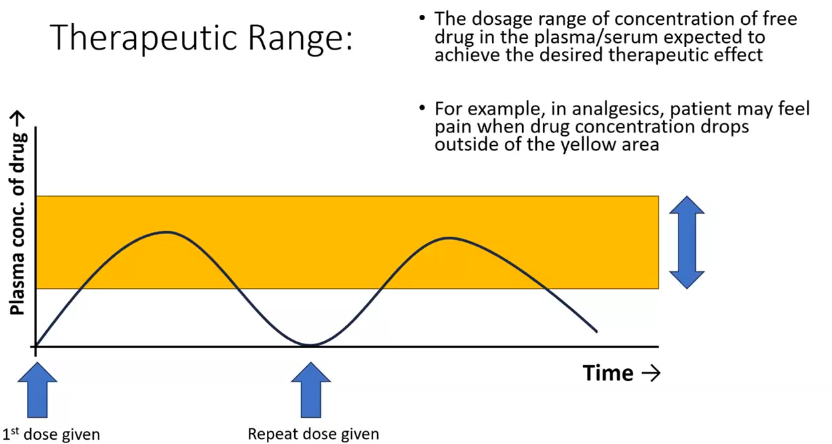
therapeutic range
may be that drug is only affective at a certain range/conc
need to ensure how long the patient will remain in therapeutic range for
drug interactions
actions of a drug may be altered if taken with other substances
eg
other drugs
foods
herbal product
interactions might increase or decrease the effect of these drugs
pharmacodynamic interactions:
alters the sensitivity of tissues to another drug
agonistic or antagonistic effect
occur at receptor level
eg synergistic combination of using tropicamide and phenylephrine together to maximise pupil dilation
pharmacokinetic interactions
can affect:
absorption
distribution, protein binding
metabolism
excretion
tend to affect the magnitude and duration of effect, rather than type of effect
practical advice:
when taking case history; make sure u ask/ record
all px current drus
other medicines other than counter that are being taken
herbal products
nutrional supplements
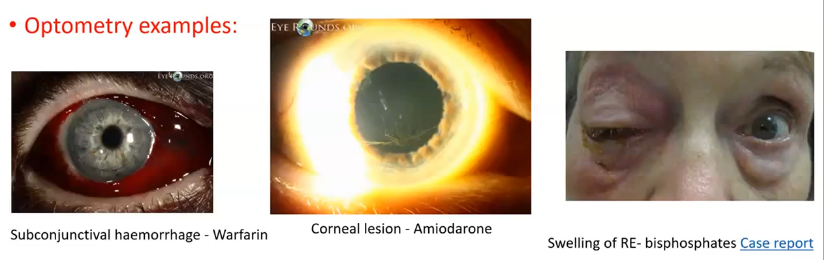
adverse drug reactions
a response to a medicinal product which is noxious and unintended (MHRA)
eg:
is px taking warfarin, likely to develop subconjunctival haemorrhages
amiodarone- can cause corneal lesions
biphosphates: swelling of the eye
part 2
what diognostix drugs do uk optometrists have acces to upon qualification
pupil dilating: topicamide HCl and phenylephrine HCl
accomodation relaxing: cyclopentolate HCl
ocular suface and tear film investigation : fluorescein, lissamine green
anaesthetics: proxymetacain HCl , tetracaine HCl, oxybuprocaine HCl , lidocaine HCl
what to ask the patient before installing drugs
have experienced adverse reactions to eye drops in the past
havs a history of drug induced adverse incidents
have any relevant medical conditions
take any systemic drugs
expected knoweledge of drugs
actions: how the drug works
interactions: any other drugs, herbal remedies, foods that might impact on the way the drug works
cautions: helps assess the risks, can be used, but cautiously
contraindications: more restrictive than a caution- drug should be avoided if this present
side effects: other side effects that this drug might cause
what should you explain to the patient
why are you instilling the drug
what effects the drops might have
how long they will last for
the side effects they might have
if dilating their pupils, that they might not be able to drive and must not undertake any activity which is not advsised after dilation and for how long
what to do if they experience an adverse reaction
leaflet for eye drops that are given to the patients
bnf
the british naitonal formulary
covers all the drugs available in the UK
emc: electronic version
eye specific drug: college of optometrist formulary
a px reportd in their case history that they are taing the antidepressant phenelzine 15mg every other day
wold u be able to use phenylephrine to dilate the px pupils?
on bnf:
drug → interactions → filter by drug name
storage of drugs in optometric practice
keep drugs out of reach of patients
store according to the manufacturers instructions
includes: out od reach and sight of children, out of light etc
room temp 8-25 degrees: eg tropicamide, cyclopentolate, lidocaine, phenylephrine, oxybuprocaine, tetracaine
fridge 2-8 degrees: proxymetacaine, chloramphenicol
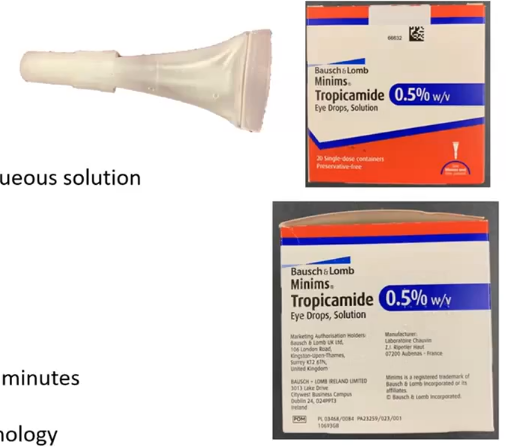
packaging: minims
bausch and lomb
single use applicators containing aqueous solution : 0.5 mk approx 12 drops in one minim
preservative free
supplied in boxes of 20 applicators
sterilised by autoclavin at 115 degrees for 30 minutes
widely used in optom and opthalmology: must be fully conversant with this method of drug administeration
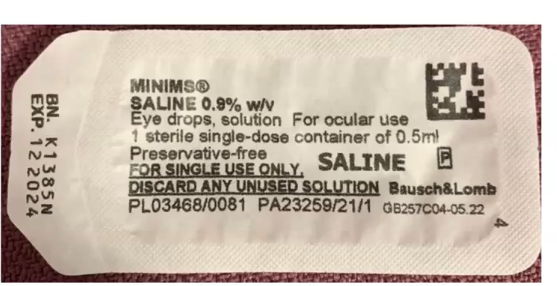
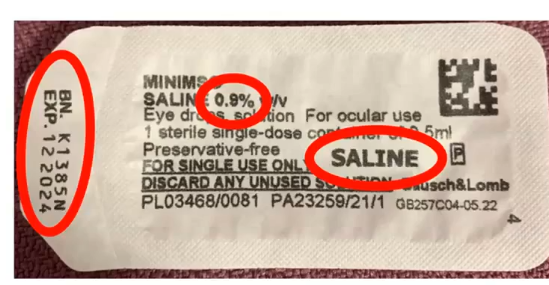
what to record
need to record the drug used including its dosage
the number of drops given
the time it was given
whether it was in the right eye or left or both
need the batch number
expiry date of the drug
procedure for obtaining the informed consent
inform px about the technique wish to use and the rationale
inform px that whether drops will sting , how long side effects nd chances of any adverse reactions
px informed not to drive after
if px has to operate hevay machinery or perform dangerous tasks, make ant=other appt for them where they can have their pupils dilated
safety checks
case history notes
does px hace any symptoms sugestive of angle closure
does px have any systemic or ocular diseases that could be aggravated by use of drug
does px have any systemic condition that could be aggravated by the instillation of drug
has px been given similar drops before and did they have a reaction to this
estimate size of anterior angle before instilling drugs
check for contraindications on slit lamp such as subluxated crystalline lens, disolcated intraocular lens implant, or pigmentary glaucoma, if any present then avoid mydriasis
choosing the approproate drug and dosage
does px have any systemic or ocular disease that could be aggravated by the drug . eg phenylephrine 105 shouldnt be given to those with severe cardiac diease, hypertension and hyoptension
does px have any disease that could influence choice of diagnostic drug. eg those with kidney disease must be given lowest dose of drug
eg iris colour: px with loghter iris respond uicker to drugs so lower doses given
drug instillation procedure
the px should be seated comfortably after washing hands and gaining consent
ask px to tilt their head backwards with the chin raised slightly
gently pull down their lower eyelid and pull it forward to form a pouch
insitl a drop into the temporal side of the pouch and gently release the lower eyelid
ask px to look don ad gentrl release upper eyelid over the eye
if 2 or more drops used, wait at least 3 mins between ech drop to ovoid the lacrimal pool from overfilling and falling out the eye after washing hands
dispose drug
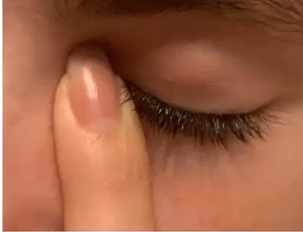
occlusion of the nasolacrimal duct
can press finger over the lacrimal sac for 10 seconds
prevents excess drug entering nasolacrimal duct
disposal
domestic waste: paper and cardboard, empty minim box, plastic/paper wrapper of the minim
non hazardous healthcare waste: used contact tonometry probes. larger quantities of cls
non hazardous pharmaceuticals waste : most pharmaceutical products: yellow bn with blue lid
hazardous waste: blue bin, anything that has come intocontact with an infected eye, clinical: chloromphenicol . non clinical: cleaning products
sharps: needles
how do i dispose of minims
these are classes as no hazardous pharmaceutical waste
whether used or unused
dispose of in a medicine disposal box : normallu as a blue lid, incinerated
this is for all pharmacy and prescirption only medicines that we use in minim form
exception = not pharmacologically , which can be disposed this way or emptied down the sink and place in a non hazardous healthcare waste
barriers for an eyedrop to cross
to reach its destination, drugs applied via eyedrops must cross anatomical barriers and bypass protective mechanisms of the eye
hits tear film → cornea
ony around 4% of the drug will reach the anterior chamber to go to the iris sphincter
conjunctival sac
lower fold created by conjunctiva over inside of the lids ( palpebral) and over the eyeball (bulbar)
max volume of fluid that can holf is approx 30 microlitres , if the lid is pulled down
have to leave time between each drop going into same eye otherwise 2nd drop washes out the first
most of the drug istilled here is cleared by the nasolacrimal drainage
route of our eyedrop
lower conjunctiva sac → (some spill onto eyelid or skin or around eye 0
mixes with tears →( some heads to puncta → nasolcrmal duct → systemic circulation or blown out of nose)
enters cornea → then into the aq hummour in the anterior chamber ( some might go to the trabecular meshwork or uveosclera and intothe systemic ciruclation)
then goes into the iris tissue
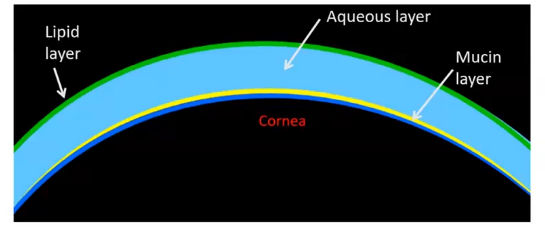
tear film
lipid layer on top which reduces evaporation of the tears
mucin layer sits against cornea, and helps spread the tears
volume approx 7-30 microlitres
tear turnover 16% per min : can increase to 80% per min following drop instillation
increased tear turnover is caused by drug irritation or ph deviation
blinking will also increase drainage due to eyelid muscle contraction
a large proportion of the drug is washed away within 2-3 minutes of drop instillation
cornea
has 3 layers: fat- water- fat
epithelium and endothelium: linked by cells with tight junctions, restrict passage of large molecules, relatively hydrophobic and lipophillic
stroma: plays a lesser role in resistance to drug passage
overall, corneal penetrance increases with hydrophobicity
corneal epithelium
high lipid content
non ionised lipid soluble molecules pass through easily
formidable barrier for water soluble molecules to pass
corneal stroma
water soluble molecyles pass easily across the stroma
ionised or polar moleucles can [ass across easily
non ionised molecules will have to ionise to assist movement
corneal endothelium
high lipid content
non ionised lipid soluble molecules find it easier to cross
forms of opthalmic drugs
aqueous solutions
oily solutions ( for drugs destoryed by water)
gels
ointments
creams
properties of opthalmic drugs : viscosity
aq solution: low viscosity
short term retention in the eye
short term drug effect
higher risk of systemic absorption
better vision
high viscosity: gel/ointments
long term retention in the eye
long term drug effect
lower risk of systemic absorption
poorer vision
influence of viscosity
diagnostic drugs
lower viscosity aq solutions
short duration of contact with the eye
minimal ocular absorption of the drug
therapeutic drugs (daytime use)
low viscosity
maintains good vision after drug instillation
repeated administeration of the drug required
therapeutic drug ( night use ony)
high viscosity
maintains high contact time with the eye - good therapeutic effect
causes smeary vision, but this can be tolerated
properties of opthalmic drugs: pH
pH of the tear fluid around 7.35 range 7-7.4
opthalmic drugs with pH significantly higher or lower than tear pH will sting
optimum comfort appears to be obtained with a slightly alkaline solution
pH of a solution can affect the efficiacy of a number of drugs
buffers are used to control the pH of opthalmic preparations
acetic acis, boric acis, potassium bicarbonate, sodium citrate, sodium phosphate
pH of solutions used in the eye normallu in the range 6-8
optometry eg of acids
anaesthtics we use usually sting on instillation due to their pH
there are weak bases: so to keep them stable they are formulated with a low pH. This keeps higher proportion ionised ( and stable)
properties of opthalmic drugs: tonicity
cornea is semi permeable membrane: tonicity of the pre corneal tear film can influence the fluid content of the cornea
tonicity of natural tears = 0.9% saline : range is 0.5% -2% tolerable
hyper vs hypotonic. eyedrops tend to be slghtly hypertonic
hypertonic can cause tearing and redness , tearing will reduce the conc of the drug
presevatives
these are required for multi dose preparations
prevents contamination during storage and administeration
preservatives can be toxic to human cells
normally used in low concs
most commonly used eye drop preservative:
benzalkonium chloride
antimicrobial effect denatures proteins and disrupts cell membrane
has mild toxic effects on cornea and conjunctiva
has been shown to increase corneal permeability
what is mydriasis vs miosis
mydriasis= pupil dilation
miosis = pupil constriction
natural response of the pupil to bright light is miosis
why do we dilate a patients pupil
pupil is constantly changing shape
need to override this response to aid our examination
will allow a better view
when bright light is shon on the eye, the pupil will constrict making it hard to see past the pupil so drug overrides this and opens up the aperture