Cardiovascular system 1
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
38 Terms
visceral pericardium
info
on surface
simple squamous
parietal pericardium
location and contents
pericardial sac around heart
simple squamous
loose CT
pericardial space
location and function
contains pericardial fluid
lubrication and protection
layers of heart
epicardium
myocardium
endocardium
epicardium
outermost layer
consistent with visceral pericardium
myocardium
wall of heart
cardiac muscle with CT
endocardium
lines the chamber
inner lining
simple squamous
right and left atria
thin walled
irregular shape
carnival and dorsal
interatrial septum divides them
right and left ventricles
thick walled
angled
caudal and ventral
interventricular septum divides them
valves
description, types
flaps of CT, cusps
Atrioventricular (AV) valves
Semilunar valves
Atrioventricular (AV) valves
Right – tricuspid
Left - mitral
Separating each atrium from each ventricle
Chordae tendineae
“heart strings”
Papillary muscles
attach to chordae tendineae
Semilunar valves
Aortic
between left ventricle and aorta
Pulmonary
between right ventricle and pulmonary artery
Pulmonary circuit
right side of heart
Heart to lungs (deoxygenated blood) and back (with oxygenated blood)
Pick up oxygen, give off carbon dioxide
Systemic circuit
left side of heart
Heart to body with (with oxygenated blood) and back (with deoxygenated blood)
Pick up carbon dioxide, gives off oxygen to tissues (cells)
pulmonary circuit expanded
Deoxygenated blood from body enters right atrium
Through right AV valve (tricuspid) into right ventricle
Through pulmonary semilunar valve into pulmonary artery
Pulmonary artery branches to smaller arteries
to smaller arterioles
to capillaries of alveoli of lungs
Venules to veins
to larger veins
to pulmonary vein into left atrium of heart
systemic circuit expanded
Oxygenated blood from pulmonary vein
to left atrium of heart
Through left AV valve (mitral valve) to left ventricle
Through aortic semilunar valve to aorta
Branches to large arteries to smaller arteries
to arterioles to capillaries in tissues all over body
Venules to veins to larger veins
to cranial and caudal vena cavae to right atrium
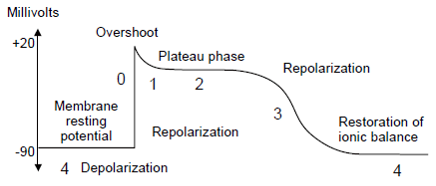
cardiac action potential
Fluctuating resting membrane potential (RMP)
Leaky Na+ channels
Slowly increases RMP to threshold
2. Voltage gated Na+ channels open
Na+ rushes into cell for rapid voltage increase depolarization
3. Plateau phase as Ca++ enters cell
4. Repolarization as K+ leaves cell
myocardium
microscopic anatomy
Mostly cardiac muscle
striated
Purkinje fibers
Specialized cells for initiation and carrying of A.P.
Intercalated disks
Specialized cell junctions for flow of A.P. contract as one unit
characteristics of cardiac muscle
intrinsic
No nerve impulse needed
Initiates its own action potential within the heart itself within the right atrium via sinoatrial (SA) node
characteristics of cardiac muscle
involuntary
Not under conscious control
A.N.S. (Parasympathetic/Sympathetic) controls rate and force
conduction network
spreads AP through heart
Pacemaker: Sinoatrial (SA) node in right atrium
Sets rate of firing
Spreads across both atria
AP -> Atrioventricular (AV) node
Pause as atria contract
AP -> AV bundle
Right and left bundle branches -> Down ventricular septum
Purkinje fibers through walls of ventricles
Carry AP impulse very quickly
ECG - electrocardiogram
Measures electrical movement across heart—moves across body
Tells us heart rate, regularity of beats
sinus rhythm
normal
arrhythmia
abnormallity
leads
points of electrode attachment
Parts
P wave
depolarization of atria
PR interval
conduction through AV valve
QRS complex
depolarization of ventricles (strongest and fastest)
T wave
repolarization of ventricles
cardiac muscle
physical and mechanical events of heart filling, contraction
can be interposed on electrical events
systole
contraction
created high pressure
diastole
relaxation and filling
lower pressure
events in the heart pt 1
AV valves
open when atrial pressure is greater than ventricular pressure
SL valves open
when ventricular pressure is greater than arterial pressure
AV valves close
when ventricular pressure is greater than atrial (as ventricles contract)
First heart sound
”lub” or S1 sound
events in the heart pt 2
Turbulent blood against closed valves
produced when the ventricles contract and AV valve close
SL valves close
at end of ventricular systole when arterial pressure is greater than ventricular pressure
Second heart sound
”dub” or S2 sound
Turbulent blood against closed valves
Occasional third heart sound
rapid ventricular filling
Especially in large, slow hearts
Heart murmurs
valves don’t close completely or blood flow is extra turbulent
mammalian fetal circulation
2 special vessels through umbilical cord
Umbilical vein
One vessel
From placenta to fetus
Relatively oxygen and nutrient rich blood
Umbilical arteries
Two vessels
From fetus to placenta
Relatively oxygen and nutrient poor blood
3 shunts (bypasses)
3 shunts
Ductus venosus
Bypasses liver
Umbilical vein connects to caudal vena cava
Foramen ovale
Right to left atrium
Bypasses lungs
Will close with first breath
Ductus arteriosus
Pulmonary artery to aorta
Bypasses lungs
portal systems
blood system from one organ to another
bypassing general circulation
Hepatic
Renal
Hepatic
Hepatic portal vein collects blood from gastrointestinal tract to liver
Liver processes nutrients
“Filters” blood: wastes, drugs
Blood enters the caudal vena cava (unoxygenated)
Renal
Hind limbs to renal portal system to kidneys
maintain consistent blood supply to kidney when filtration is reduced
Filters toxins before sending back to general circulation
Lower vertebrates (birds, reptiles, amphibians, fish)
single circuit systems
fish
2 chambers in heart (atrium and ventricle)
amphibians
3 chambered heart
2 atria and 1 ventricle
reptiles
Most have 3 chambered heart
2 atria and 1 ventricle