Lecture 4 Adaptive Immunity
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
2 branches in adaptive immunity
Humoral - B cells becoming plasma cells making antibodies
Cell mediated response - CD8+ T cells (killer T cells) and CD4- helper T cells (helps both branches)
Antigenicity
the ability of a substance (antigen) to be specifically recognized by the immune system, especially by antibodies or T cell receptors
Immunogenicity
the ability of a substance to provoke an immune response in the body.
This means the molecule doesn’t just get recognized (antigenicity) — it actually activates immune cells and leads to antibody production or T cell activation.
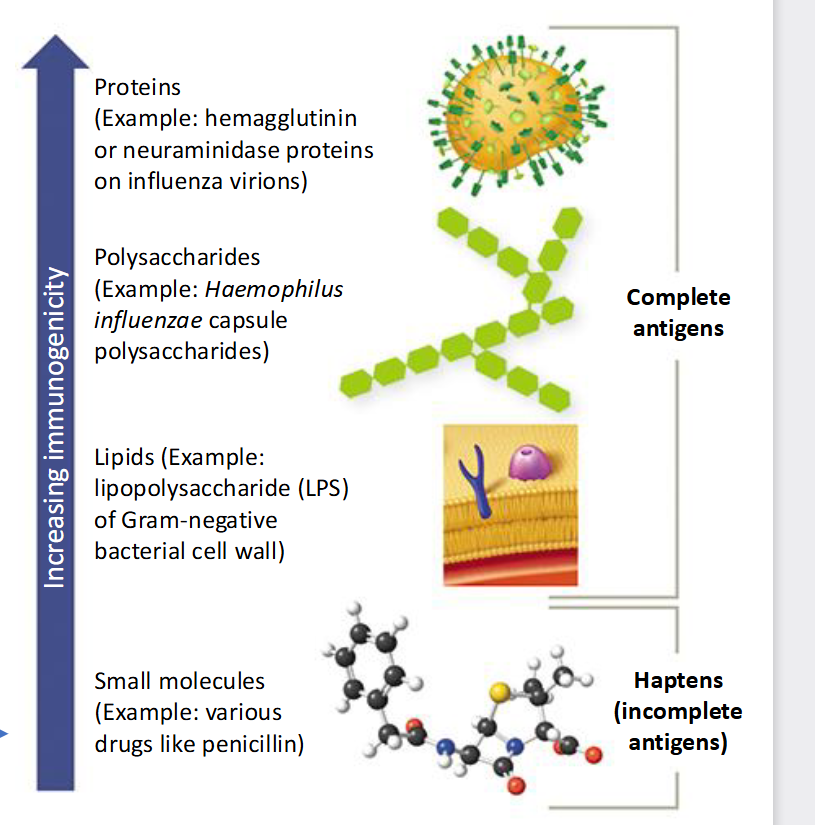
Increasing Immunogenicity
Small molecules (Ex:drugs like penicillin) —> Lipids (Ex: (LPS) of Gram negative bacterial cell wall) —> Polysaccharides (Ex: Haemophilus influenzae capsule polysaccharides) —> Proteins (Example: hemagglutinin or neuraminidase proteins on influenza virions)
CD8+
Cytotoxic T Lymphocyte killer cells that directly kills
CD4-
Helper T Lymphocyte, promotes phagocytosis in macrophages by producing a lot of activating cytokines
Humoral Immunity
Microbes: Extracellular microbes
Responding Lymphocytes: B cells
Mechanism: B cell becomes a plasma cell that secretes antibodies
Functions: Blocks infections and eliminates extracellular microbes
Cell mediated Immunity Helper T cells
Microbes: Phagocytosed microbes that live w/in macrophages
Responding Lymphocytes: Helper T lymphocytes
Mechanism: Activated macrophage
Functions: Elimination of phagocytosed microbes
Cell mediated Immunity Killer T cells
Microbes: Intracellular cell replicating w/in infected cell
Responding Lymphocytes: cytotoxic T cells
Mechanism: Cytotoxic T cells kills infected cells
Functions: Kill infected cell and eliminate reservoirs of infections
Cells of the Adaptive Immune System
Lymphocytes (B and T), Antigen-presenting cell (dendritic, macrophages, B cells), and Effector cells (T lymphocytes and Macrphages)
Lymphocytes (B and T)
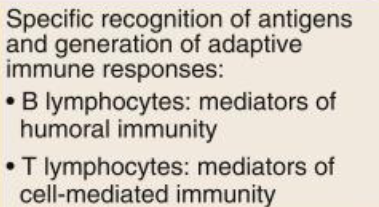
Antigen-presenting cell (dendritic, macrophages, B cells)
Effector cells (T lymphocytes and Macrphages)
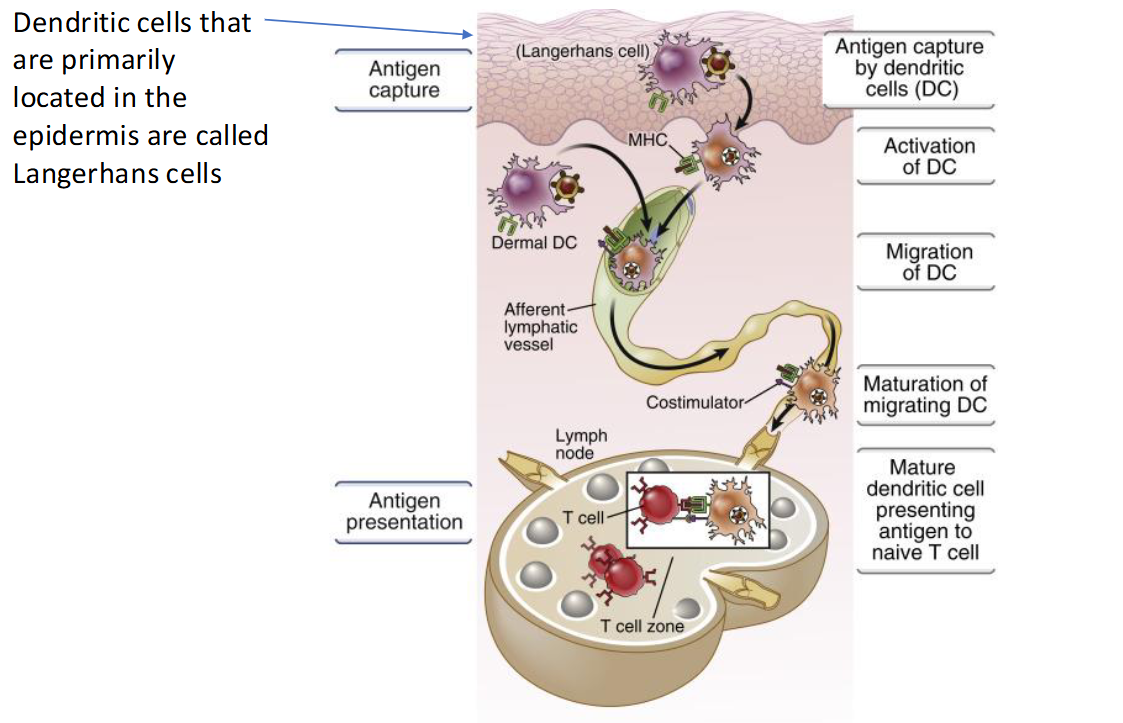
Maturation and tissue differentiation of lymphocytes T cells lineage
Bone marrow cell —> T lymphocyte goes to Thymus —> move out to blood —> to the peripheral secondary lymphoid organs —> the spleen and the mucosal and cutaneous lymphoid tissue.
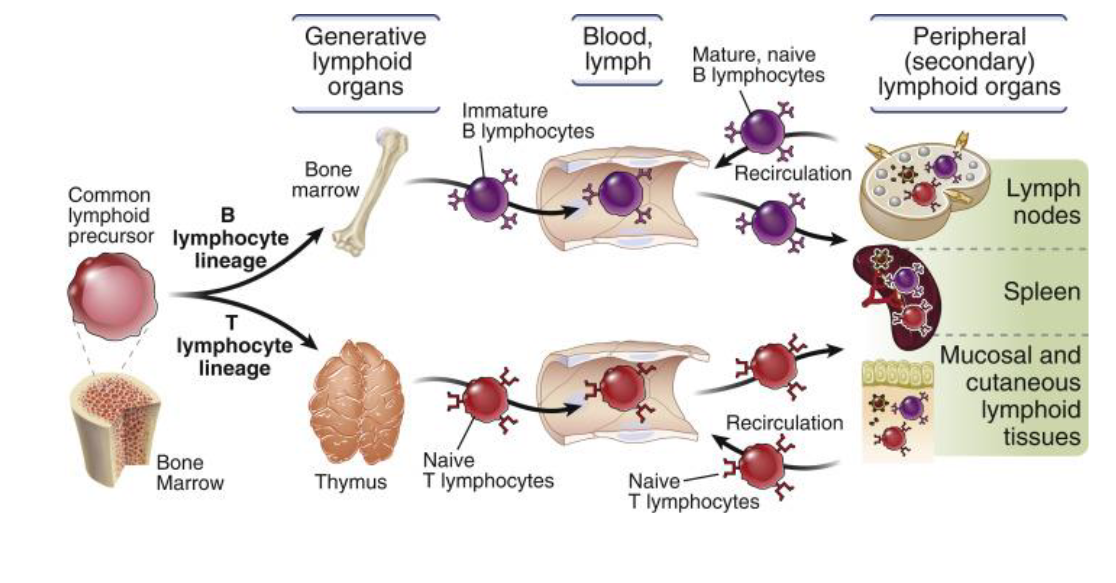
Maturation and tissue differentiation of lymphocytes B cells lineage
Bone marrow cell —> B lymphocyte goes to Bone marrow —> move out to blood —> to the peripheral secondary lymphoid organs —> the lymph nodes and spleen
Migration of macrophages
Fetal hematopoietic (yolk, sac, liver) stem cell (bone marrow) will produce macrophage precursors and these precursors will develop and grow into different types of residential macrophages in brain, liver, lung, or spleen
Brain macrophage
Microglial cells
Liver macrophage
Kupffer cells
Lung macrophage
Alveolar macrophage
Spleen macrophage
Sinusoidal macrophages
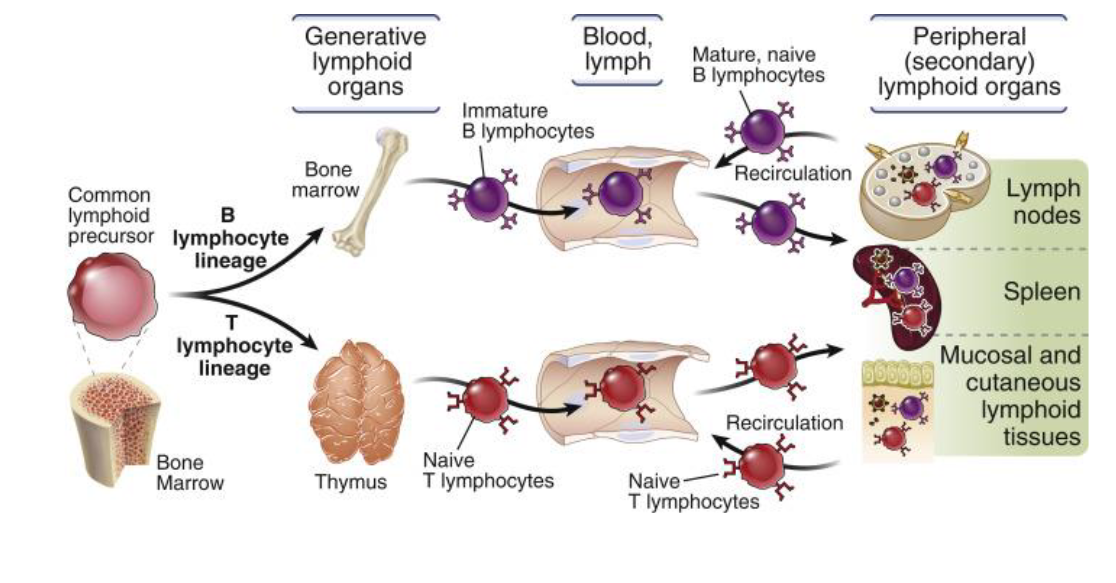
What triggers the Adaptive system
Capture, transport and presentation of protein antigens
Presentation of protein antigens
T cells need to get triggered to and cells do that by bringing a peicepiece of the antigen and presenting it to the T cell so the T cell can then respond
Major Histocompatibility Complexes
membrane bound protein complexes, there is MHC class 1 and MHC class 2
MHC Class I Loctaion
Found on all nucleated cells
MHC Class I what they do
Presents peptides from inside the cell intercellular (self or viral proteins) which then get recognized by CD8⁺ cytotoxic T cells
MHC Class 1 Function
lets T cells detect virus-infected or abnormal cells by antigen presentation
MHC class 2 location
Found mainly on antigen- presenting cells (APCs) such as macrophages, dendritic cells, and B cells
MHC class 2 what they do
Presents peptides from engulfed extracellular microbes which get recognized by CD4⁺ helper T cells
MHC class 2 function
helps activate immune responses against extracellular pathogens by antigen presentation
Only professional phagocytes
have MHCII (macrophages, dendritic cells, and B cells)
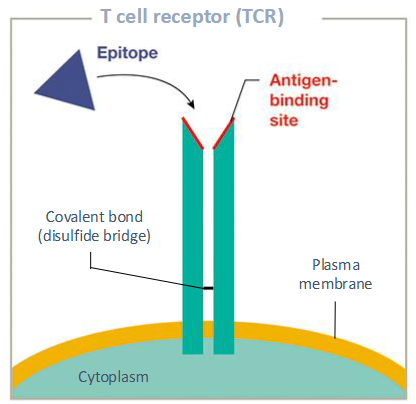
Epitope
the specific molecular region on an antigen that an immune cell, such as an antibody or a B or T cell, recognizes and binds to, thereby initiating an immune response
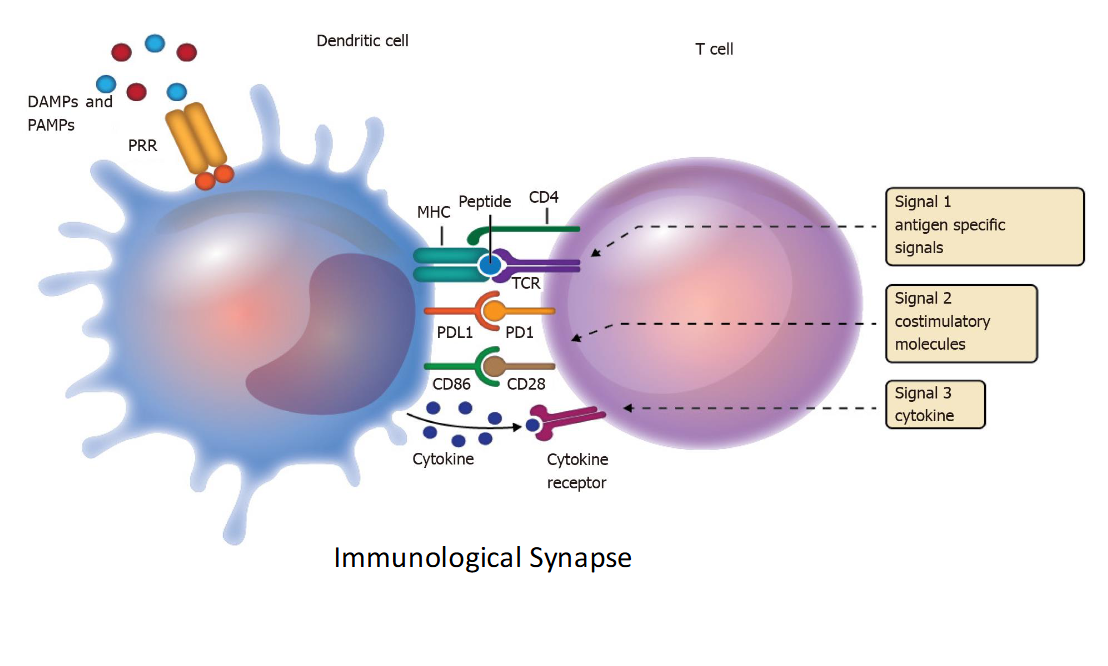
T Cell Activation: 3 signals
Antigen specific signals
Costimulatory molecule binding
Cytokines bind to cytokine receptors
For full activation of T cells, you need all 3 signals
CD4+ Helper T cells “Help
Both Branches of Adaptive Immunity (humoral and cell)
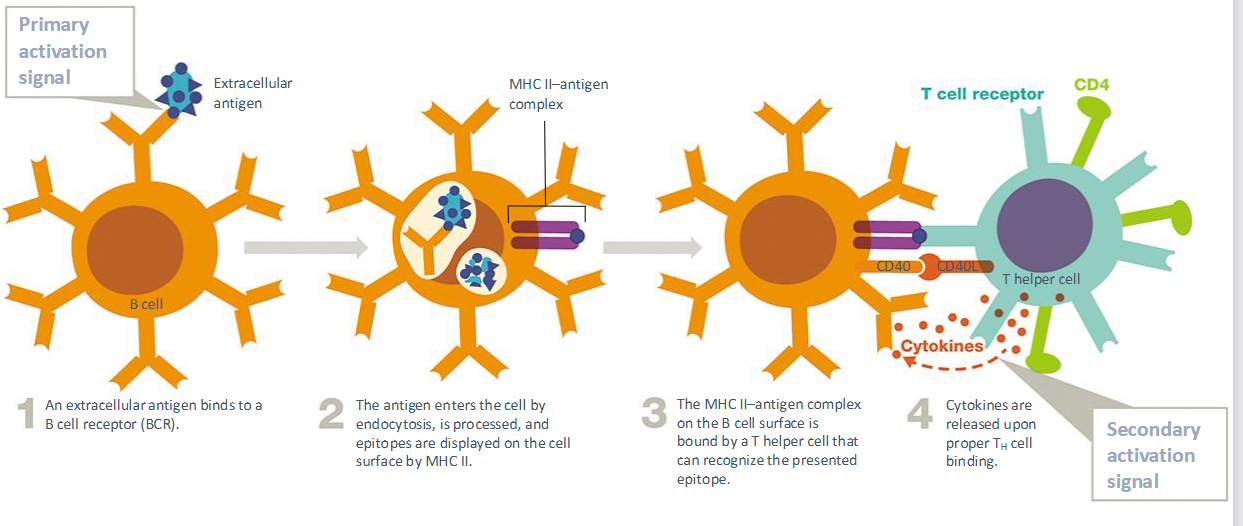
How does CD4+ Helper T cells help Humoral branch
Help B cells become plasma cells making antibodies
How does CD4+ Helper T cells help Cell branch
They stimulate the cytotoxic T cell killers
Subset of helper T cells that target different parts
TH1, TH2, TH17, Tfh
TH1 cells
interferon gamma stimulated and it target macrophages by intercellular pathogens
Can cause autoimmunity and chronic inflammation
TH2 Cells
Targets eosinophils by helmith (parasite) and cause allergies
Th17 cell
Targets neutrophils by extracellur bacteria and fungi, results in neutrophil recruitment and activation as well as inflammation
Tfh
Targets B cells by extracellular pathogens and results in antibody production and autoimmunity
Cytotoxic T Lymphocyte Roles in Antigen Elimination process
When a cell is infected with a virus or if it is cancerous, interferons are released
• Recruits activated T cytotoxic cells to the area
• Enhances MHC I production inside host cells
• Puts the immune system on high alert
How killer T cells actually kill:
T cytotoxic cell binds to an MHC I– antigen complex:
Releases perforins
-Forms pores in the target cell
Releases granzymes
-Enter through the pore
-Break down host cell proteins
-Induce apoptosis
Antibody Structure and Isotypes
IgG, IgA, IgM, IgE
IgG
Monomer, most abundant in body, long half life
Very important b/c it crosses the placenta and gives babies immune systems

IgA
Monomer or dimer, second most abundant, the antibody that is in milk resistant to stomach acid

IgM
Monomer or pentameter, third most abundant, the first antibody you're going to see in the blood when anybody gets infected with something

IgE
Rare, fights parasites and mediates allergic reactions (e = eosinophil)

Most antigens are
T dependent, and require T helper cells to fully activate B cells
T-independent antigens
Some antigens dont need help from T cell like some polysaccharides in bacteria because they have multiple binding sites
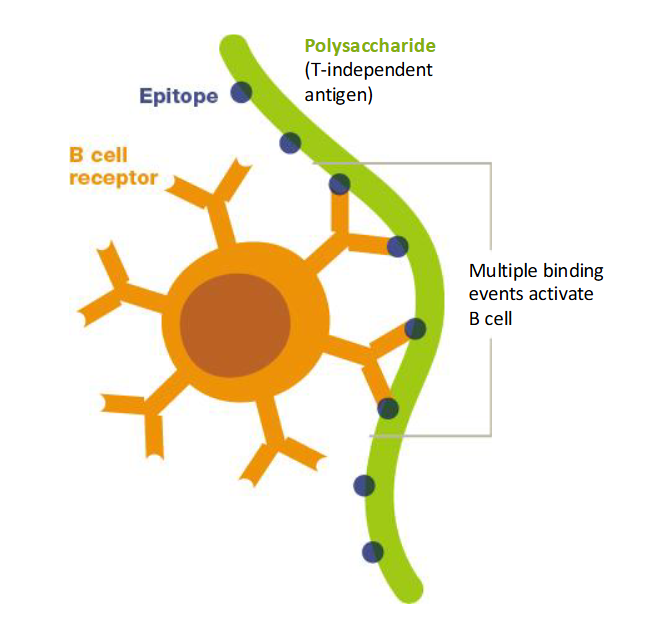
Activated B cell (T independent)
proliferate and differentiate into plasma cells and memory cells
How antibodies eliminate invaders
Neutralization, activate complement, or Increase phagocytosis
Neutralization
Antibodies block viruses by binding to their spike proteins, which prevents the virus from attaching to and entering our cells
Primary Antigen Exposure
When your body encounters an antigen for the first time
Slower, weaker response because the immune system is “learning” the antigen
Secondary Antigen Exposure
On re-exposure to the same antigen, Memory B cells quickly recognize it and rapidly produce antibodies.
Faster, stronger, longer-lasting response (this is the basis of vaccines).
4 types of Acquisition of Humoral Immunity
Naturally acquired active immunity
Naturally acquired passive immunity
Artificially acquired active immunity
Artificially acquired passive immunity
Naturally acquired active immunity
You make your own antibodies after a natural infection.
Example: recovering from chickenpox → long-lasting immunity.
Naturally acquired passive immunity
You receive antibodies naturally from another person.
Example: maternal antibodies passing to baby through placenta (IgG) or breast milk (IgA).
Artificially acquired active immunity
You make your own antibodies after medical exposure to antigen.
Example: vaccination with weakened or inactivated pathogens.
Long-lasting immunity (with memory)
Artificially acquired passive immunity
You receive ready-made antibodies through medical treatment.
Example: injection of antivenom or monoclonal antibodies.
Immediate, short-term protection.
Active immunity
your body makes the antibodies → long-term (memory).
Passive immunity
you receive antibodies from outside → short-term (no memory).