Chapter 13: Disorders of the Eye
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
Chapter 13: Disorders of the Eye
Eye disorders can result from injury, disease processes, or aging
Common eye disorders nurses should recognize:
Macular degeneration
Cataracts
Glaucoma
Macular Degeneration (Age-Related Macular Degeneration, AMD)
Progressive loss of central vision due to damage to the macula
Population: Leading cause of vision loss in older adults
Key Point: No cure
Vision Pattern:
Central vision loss
Peripheral vision preserved (important NCLEX distinction
AMD affects central vision only
Dry = gradual
Wet = fast and severe
Types of Macular Degeneration
Dry Macular Degeneration
Most common form
Cause: Gradual blockage of retinal capillary arteries
Pathophysiology:
Reduced blood supply to the macula
Ischemia and necrosis from loss of retinal cells
Progression: Slow, gradual decline in vision
Wet Macular Degeneration
Less common but more severe
Cause: Abnormal neovascularization
Pathophysiology:
New blood vessels with thin, fragile walls
Leakage of blood and fluid into the retina
Progression: Rapid vision loss
AMD affects central vision only
Dry = gradual
Wet = fast and severe
Macular Degeneration Risk Factors
Dry Macular Degeneration
Smoking (strongest modifiable risk factor)
Hypertension (vascular damage)
Female sex
Short body stature
Family history
Diet low in carotene and vitamin E (reduced antioxidant protection)
Age > 60
Caucasian race
Wet Macular Degeneration
Can occur at any age (less age-dependent than dry form)
Macular Degeneration Expected Findings
Loss of depth perception
Objects appear distorted (metamorphopsia)
Blurred vision
Loss of central vision
Blindness (advanced disease)
Macular Degeneration Exams
Diagnostic Procedures
Ophthalmoscopy
Examines the fundus of the eye, including:
Retina
Optic disc
Macula
Blood vessels
Visual Acuity Tests
Snellen chart (distance vision)
Rosenbaum chart (near vision)
Macular Degeneration Care
Wet Macular Degeneration Interventions
Laser therapy to seal leaking blood vessels
Ocular injections to inhibit abnormal blood vessel growth
Anti–endothelial growth factor (anti-VEGF) agents:
Bevacizumab
Ranibizumab
Client Education
Encourage intake of foods high in antioxidants, carotene, and vitamins E and B12
As vision loss progresses, clients may have difficulty:
Eating
Driving
Writing
Reading
Performing activities of daily living
Refer clients to community resources for:
Transportation assistance
Reading devices
Large-print books
A nurse is providing teaching for a client who has a new diagnosis of dry macular degeneration. Which of the following instructions should the nurse include in the teaching?
a
Increase intake of deep yellow and orange vegetables.
b
Administer eye drops twice daily.
c
Avoid bending at the waist.
d
Wear an eye patch at night.
Increase intake of deep yellow and orange vegetables.
When taking action, the nurse should instruct the client to increase dietary intake of carotenoids and antioxidants to slow the progression of the macular degeneration.
A client who has primary open-angle glaucoma should administer eye drops twice daily.
A client who is at risk for increased intraocular pressure, such as following cataract surgery, should avoid bending at the waist.
A client who has had eye surgery, such as cataract surgery, should wear an eye patch at night to protect the eye from injury.
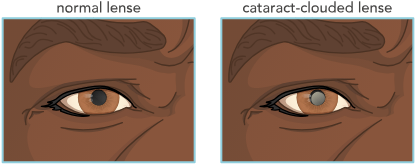
Cataracts
Opacity of the lens that results in impaired vision
Common Causes of Cataracts
Age-Related
Drying of the lens due to water loss
Increased lens density from lens fiber compaction
Traumatic
Blunt or penetrating eye injury
Foreign body in the eye
Radiation or ultraviolet light exposure
Toxic
Long-term use of:
Corticosteroids
Phenothiazine derivatives
Beta blockers
Miotic medications
Associated Conditions
Diabetes mellitus
Hypoparathyroidism
Down syndrome
Chronic sunlight exposure
Complicated (Secondary to Eye Disease)
Retinitis pigmentosa
Glaucoma
Retinal detachment
Health Promotion and Disease Prevention of Cataracts
Teach clients to wear sunglasses outdoors (UV protection)
Educate clients to use protective eyewear during:
Sports
Hazardous activities (welding, yard work)
Encourage annual eye examinations
Especially important for adults over age 40
Cataracts Risk Factors
Advanced age
Diabetes
Heredity
Smoking
Eye trauma
Excessive sun exposure (UV damage)
Chronic medication use, including:
Corticosteroids
Phenothiazine derivatives
Beta blockers
Miotic medications
Cataracts Expected Findings
Decreased visual acuity
Frequent prescription changes
Reduced night vision
Decreased color perception
Blurred vision
Diplopia (double vision)
Physical Assessment Findings
Progressive, painless loss of vision (key NCLEX clue)
Visible lens opacity
Absent red reflex
A nurse is caring for a client who has a new diagnosis of cataracts. Which of the following manifestations should the nurse expect?
Select all that apply.
a
Eye pain
b
Floating spots
c
Blurred vision
d
White pupils
e
Bilateral red reflexes
c Blurred vision
d White pupils
Eye pain is associated with primary angle-closure glaucoma and floating spots are a manifestation associated with retinal detachment.
Bilateral red reflexes are absent in a client who has cataracts.
Cataracts Exams
Diagnostic Procedures
Ophthalmoscopy
Direct visualization of lens opacity
Confirms presence of cataracts
Cataracts Care
Assess visual acuity using the Snellen chart
Examine external and internal eye structures with an ophthalmoscope
Determine functional ability related to decreased vision (ADLs, safety)
Increase lighting in the client’s environment
Provide adaptive devices for reduced vision:
Magnifying lenses
Large-print books and newspapers
Talking devices (clocks, watches)
Cataracts Meds
Anticholinergic Agents
Atropine 1% ophthalmic solution
Action:
Causes mydriasis (pupil dilation)
Causes cycloplegia (relaxes ciliary muscles)
Uses:
Preoperative pupil dilation
Visualization of internal eye structures
Nursing Action:
Fast onset
Long duration of action
Client Education
Inform clients that medication effects may last 7 to 12 days
Teach that atropine can cause photosensitivity
Instruct to wear sunglasses to protect eyes
Cataracts Therapeutic Procedures
Surgical removal of the lens
Small incision is made
Lens removed in one piece or fragmented using sound waves (phacoemulsification)
Posterior capsule preserved
Intraocular lens (IOL) implanted
Replacement lens may correct refractive errors, improving vision
Postoperative Nursing Actions
Focus on:
Preventing increased intraocular pressure (IOP)
Preventing infection
Administering ophthalmic medications
Providing pain relief
Teaching home self-care and fall prevention
Client Education
Wear sunglasses outdoors or in bright light (photosensitivity)
Report signs of infection:
Yellow or green drainage
Avoid activities that increase IOP, including:
Bending over at the waist
Sneezing
Blowing the nose
Coughing
Straining
Head hyperflexion
Tight or restrictive clothing (tight collars)
Sexual intercourse
Limit activities, such as:
Tilting head back to wash hair
Cooking and housekeeping
Rapid, jerky movements (vacuuming)
Driving or operating machinery
Playing sports
Report pain with nausea or vomiting (possible increased IOP or hemorrhage)
Expect best vision in 4 to 6 weeks, not immediately
Report immediately:
Lid swelling
Decreased vision
Bleeding or discharge
Sudden sharp eye pain
Flashes of light or floating shapes (possible retinal detachment)
Cataracts (Image)
Cataracts Complications
Infection
Can occur after surgery
Client education
Report immediately:
Yellow or green drainage
Increased redness
Eye pain
Decreased visual acuity
Increased tear production
Photophobia (light sensitivity)
Bleeding
Possible several days after surgery
Client education:
Report immediately:
Sudden change in vision
Increase in eye pain
A nurse is providing postoperative teaching to a client following cataract surgery. Which of the following statements should the nurse include in the teaching?
a
“You can resume playing golf in 2 days.”
b
“You need to tilt your head back when washing your hair.”
c
“You can get water in your eyes in 1 day.”
d
“You need to limit your housekeeping activities.”
D. “You need to limit your housekeeping activities.”
Do not instruct the client to resume playing golf for several weeks. This could cause a rise in intraocular pressure (IOP) or possible injury to the eye.
Do not instruct the client to tilt the head back when washing their hair. This could cause a rise in IOP or possible injury to the eye.
The client should not get water in their eyes for 3 to 7 days following cataract surgery to reduce the risk for infection and promote healing.
Glaucoma
Disorder of the optic nerve due to increased intraocular pressure (IOP)
Caused by:
Decreased aqueous humor drainage
Increased fluid secretion
Leads to optic nerve atrophy and visual field defects
Normal IOP: 10 to 20 mm Hg
Types Glaucoma
Primary Open-Angle Glaucoma (POAG)
Most common form
Angle between iris and sclera remains open
Impaired aqueous humor outflow due to blockage in:
Canal of Schlemm
Trabecular meshwork
Results in gradual increase in IOP
Onset: Slow and painless
Primary Angle-Closure Glaucoma
Sudden closure of the angle between iris and sclera
Causes rapid increase in IOP
Onset: Sudden
Medical emergency requiring immediate treatment
Secondary Glaucoma
Results from:
Eye trauma
Eye surgery
Eye tumors
Uveitis or iritis
Neovascular disorders
Degenerative disease
Central retinal vein occlusion
Clinical Importance
Glaucoma is a leading cause of blindness
Early diagnosis and treatment are critical to prevent vision loss
Health Promotion and Disease Prevention of Glaucoma
Encourage annual eye examinations
Especially for adults over age 40
Educate clients on early symptoms, including:
Gradual vision reduction
Mild eye pain
Glaucoma Risk Factors
Increasing age
Infection
Eye tumors
Diabetes mellitus
Genetic predisposition
Hypertension
Eye trauma
Severe myopia
Retinal detachment
A nurse is caring for a male older adult client who has a new diagnosis of glaucoma. Which of the following should the nurse recognize as risk factors associated with this disease?
Select all that apply.
a
Sex
b
Genetic predisposition
c
Hypertension
d
Age
e
Diabetes mellitus
b Genetic predisposition
c Hypertension
d Age
e Diabetes mellitus
Glaucoma Expected Findings
Primary Open-Angle Glaucoma
Headache
Mild eye pain
Loss of peripheral vision (tunnel vision)
Decreased accommodation
Halos around lights
Elevated IOP
Greater than 20 mm Hg
Often 22 to 32 mm Hg
Onset: Gradual and often asymptomatic early
Primary Angle-Closure Glaucoma
Rapid onset of markedly elevated IOP
≥ 30 mm Hg
Decreased or blurred vision
Colored halos around lights
Pupils nonreactive to light
Severe eye pain with nausea
Photophobia
Medical emergency
Glaucoma Exams
Visual Assessments
Measure decreased visual acuity
Assess peripheral vision loss
Tonometry
Measures intraocular pressure
Normal IOP: 10 to 20 mm Hg
Elevated in glaucoma, especially angle-closure type
Gonioscopy
Determines drainage angle of the anterior chamber
Differentiates open-angle vs angle-closure glaucoma
A nurse is caring for a client who has diabetes mellitus and reports a gradual loss of peripheral vision. The nurse should recognize this as a manifestation of which of the following diseases?
a
Cataracts
b
Open-angle glaucoma
c
Macular degeneration
d
Angle-closure glaucoma
Open-angle glaucoma
A client who has angle-closure glaucoma experiences sudden nausea, severe pain, and halos around lights
A client who has cataracts experiences a decrease in peripheral and central vision due to opacity of the lens.
A client who has macular degeneration experiences a loss of central vision.
Glaucoma Care
Monitor intraocular pressure (IOP)
Report IOP > 20 mm Hg
Assess for:
Decreased vision
Light sensitivity
Aching or discomfort around the eye
Explain the disease process and allow clients to express concerns
For angle-closure glaucoma, treat severe pain and nausea with:
Analgesics
Antiemetics
General Eye Drop Education
Use medications exactly as prescribed (often every 12 hours)
Instill 1 drop at a time
Wait 5 to 10 minutes between different eye drops
Do not touch the applicator tip to the eye
Wash hands before and after use
Use punctal occlusion after instillation
Apply gentle pressure to the inner corner of the eye to reduce systemic absorption
Cholinergic Agents
Adrenergic Agonists
Beta Blockers
Carbonic Anhydrase Inhibitors
Prostaglandin Analogs
Systemic Osmotics
Glaucoma Meds
Glaucoma Meds
General Eye Drop Education
Use medications exactly as prescribed (often every 12 hours)
Instill 1 drop at a time
Wait 5 to 10 minutes between different eye drops
Do not touch the applicator tip to the eye
Wash hands before and after use
Use punctal occlusion after instillation
Apply gentle pressure to the inner corner of the eye to reduce systemic absorption
Cholinergic Agents
Examples: Carbachol, Echothiophate, Pilocarpine
Action: Miotics that constrict the pupil and increase aqueous humor outflow
Side Effect: Blurred vision
NCLEX Note: Pilocarpine is a second-line drug for POAG
Client Education: Use good lighting to prevent falls
Adrenergic Agonists
Examples: Apraclonidine, Brimonidine tartrate, Dipivefrin
Action:
Decrease aqueous humor production
Dilate pupils to improve fluid movement
Client Education: Wear sunglasses due to pupil dilation
Beta Blockers
Example: Timolol
First-line therapy for glaucoma
Action: Decrease aqueous humor production
Nursing Considerations:
Can be systemically absorbed
May cause:
Bronchoconstriction (use caution in asthma, COPD)
Hypoglycemia masking (use caution in diabetes)
Bradycardia and hypotension
Carbonic Anhydrase Inhibitors
Examples: Acetazolamide, Dorzolamide, Brinzolamide
Action: Reduce aqueous humor production
Nursing Action:
Assess for sulfa allergy (sulfa-based medications)
Prostaglandin Analogs
Examples: Bimatoprost, Latanoprost
Action: Increase aqueous humor outflow via uveoscleral pathway
Client Education:
Do not use if cornea is not intact
May cause permanent darkening of iris color with long-term use
Systemic Osmotics
Examples: IV mannitol, oral glycerin
Use: Emergency treatment for acute angle-closure glaucoma
Action: Rapidly decreases IOP by osmotic diuresis
Cholinergic Agents
Examples: Carbachol, Echothiophate, Pilocarpine
Action: Miotics that constrict the pupil and increase aqueous humor outflow
Side Effect: Blurred vision
NCLEX Note: Pilocarpine is a second-line drug for POAG
Client Education: Use good lighting to prevent falls
Adrenergic Agonists
Examples: Apraclonidine, Brimonidine tartrate, Dipivefrin
Action:
Decrease aqueous humor production
Dilate pupils to improve fluid movement
Client Education: Wear sunglasses due to pupil dilation
Beta Blockers
Example: Timolol
First-line therapy for glaucoma
Action: Decrease aqueous humor production
Nursing Considerations:
Can be systemically absorbed
May cause:
Bronchoconstriction (use caution in asthma, COPD)
Hypoglycemia masking (use caution in diabetes)
Bradycardia and hypotension
Carbonic Anhydrase Inhibitors
Examples: Acetazolamide, Dorzolamide, Brinzolamide
Action: Reduce aqueous humor production
Nursing Action:
Assess for sulfa allergy (sulfa-based medications)
Prostaglandin Analogs
Examples: Bimatoprost, Latanoprost
Action: Increase aqueous humor outflow via uveoscleral pathway
Client Education:
Do not use if cornea is not intact
May cause permanent darkening of iris color with long-term use
Systemic Osmotics
Examples: IV mannitol, oral glycerin
Use: Emergency treatment for acute angle-closure glaucoma
Action: Rapidly decreases IOP by osmotic diuresis
Glaucoma Therapeutic Procedures
Glaucoma Surgery
Laser trabeculectomy
Iridotomy
Shunt placement
Purpose: Improve aqueous humor outflow by opening a drainage channel
Nursing Action
Emphasize strict medication adherence to prevent optic nerve damage
Client Education
Wear sunglasses in bright environments
Report signs of infection:
Yellow or green drainage
Avoid activities that increase IOP:
Bending at the waist
Sneezing, coughing
Straining
Head hyperflexion
Tight clothing around the neck
Sexual intercourse
Do not lie on the operative side
Report immediately:
Severe eye pain
Nausea or vomiting
Decreased vision
Lid swelling
Bleeding or discharge
Flashes of light or floating shapes
Limit activities:
Tilting head back to wash hair
Housekeeping and cooking
Rapid or jerky movements
Driving or operating machinery
Playing sports
Best vision expected in 4 to 6 weeks after surgery
Glaucoma Complications
Blindness
Potential outcome of untreated glaucoma
Vision loss is irreversible once it occurs
Client Education:
Glaucoma Screening Schedule
Before age 40: Every 2 to 4 years
Ages 40 to 54: Every 1 to 3 years
Ages 55 to 64: Every 1 to 2 years
Ages 65 and older: Every 6 to 12 month