8. Vascular Disorders & Thrombosis: Mechanisms of Edema
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
What is an important key to life?
water
What percent of body weight does water constitute?
60%
What amount of water is intracellular?
2/3
What amount of water is extracellular?
1/3
What compartments is extracellular water broken down into?
I
P
interstitium
plasma
What percent of water is extracellular in the interstitium?
80%
What percent of water is intravascular in the plasma?
20%
how water shifts from the different compartments and into and out of the cell
concentration gradient
What is water distribution between plasma and the interstitium determined mainly by?
osmotic and hydrostatic pressure differentials between the compartments
difference between the pressure within the capillaries and the pressure within the interstitium
hydrostatic pressure
Electrolytes make up roughly what percent of plasma osmolality? What can be said about their concentration between the intravascular compartment and the interstitium?
84%; due to their relatively free movements through the pores in the endothelium, their concentration remains relatively even
Plasma proteins make up roughly what percent of the osmolality? What do they represent the majority of? Why?
1%; oncotic pressure gradient; there is a vast difference in the concentration of these proteins between the interstitium and plasma
most important plasma protein responsible for the oncotic pressure gradient
albumin
The concentration of albumin is much greater in ________ than in the ________, typically which helps to pull fluid from the ________ into the ________ compartment.
plasma; interstitium; interstitium; intravascular
major oncotic protein within the interstitium
glycoproteins
What will alterations in any of the factors which regulate normal fluid distribution resulting in fluid accumulation in the interstitium result in?
edema
What are the mechanisms of edema?
I
I
D
D
increased microvascular permeability
increased intravascular hydrostatic pressure
decreased oncotic pressure (or osmotic pressure)
decreased lymphatic drainage
With increased microvascular permeability, ________ results in the release of ________ to cause ________. This results in the ________ of the interendothelial gaps. Water moves from the ________ ________ into the ________. This is the tissue ________ often seen in ________.
inflammation; mediators; vasodilation; widening; intravascular space; interstitium; swelling; inflammation

What is this an example of?
increased microvascular permeability (atopic dermatitis)
The edema due to increased microvascular permeability can be ________ or ________.
localized; systemic

What is this showing?
generalized edema due to septicemia
What are the mechanisms involved in increased intravascular hydrostatic pressure?
I
P
I
increased blood flow (hyperemia)
passive accumulation of blood (congestion)
increased blood volume
How does an increase in blood flow lead to edema?
pressure within the capillary is higher, so the fluid will move out
How does passive accumulation of blood lead to edema?
more blood pooling means more fluid will move out
How does increased blood volume lead to edema?
more blood means more distended which means more pressure and more ability for fluid to move out
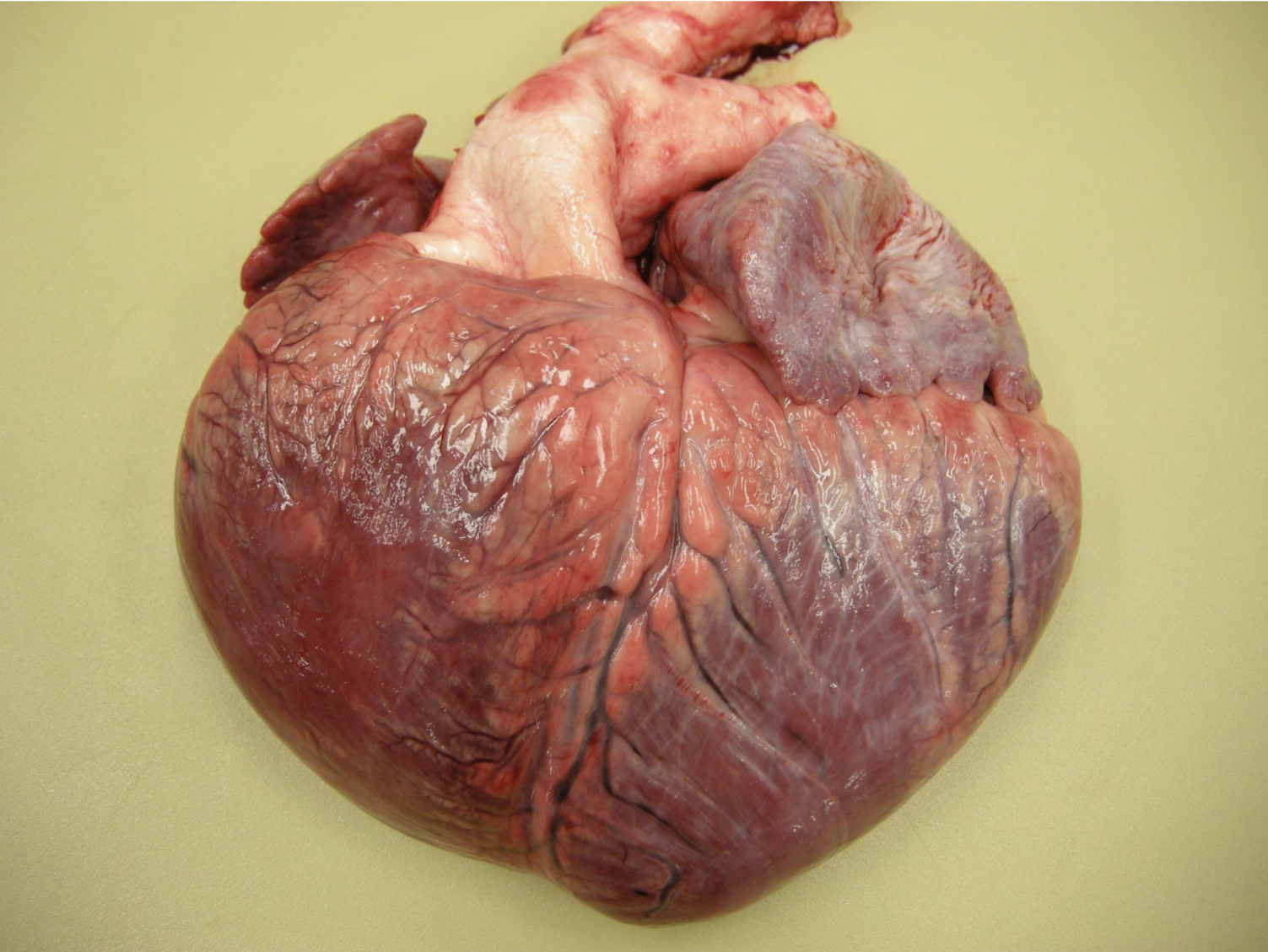
What is this an example of?
increased intravascular hydrostatic pressure
What is this an example of?
increased intravascular hydrostatic pressure (atrial septal defect causes dilation of the right side)
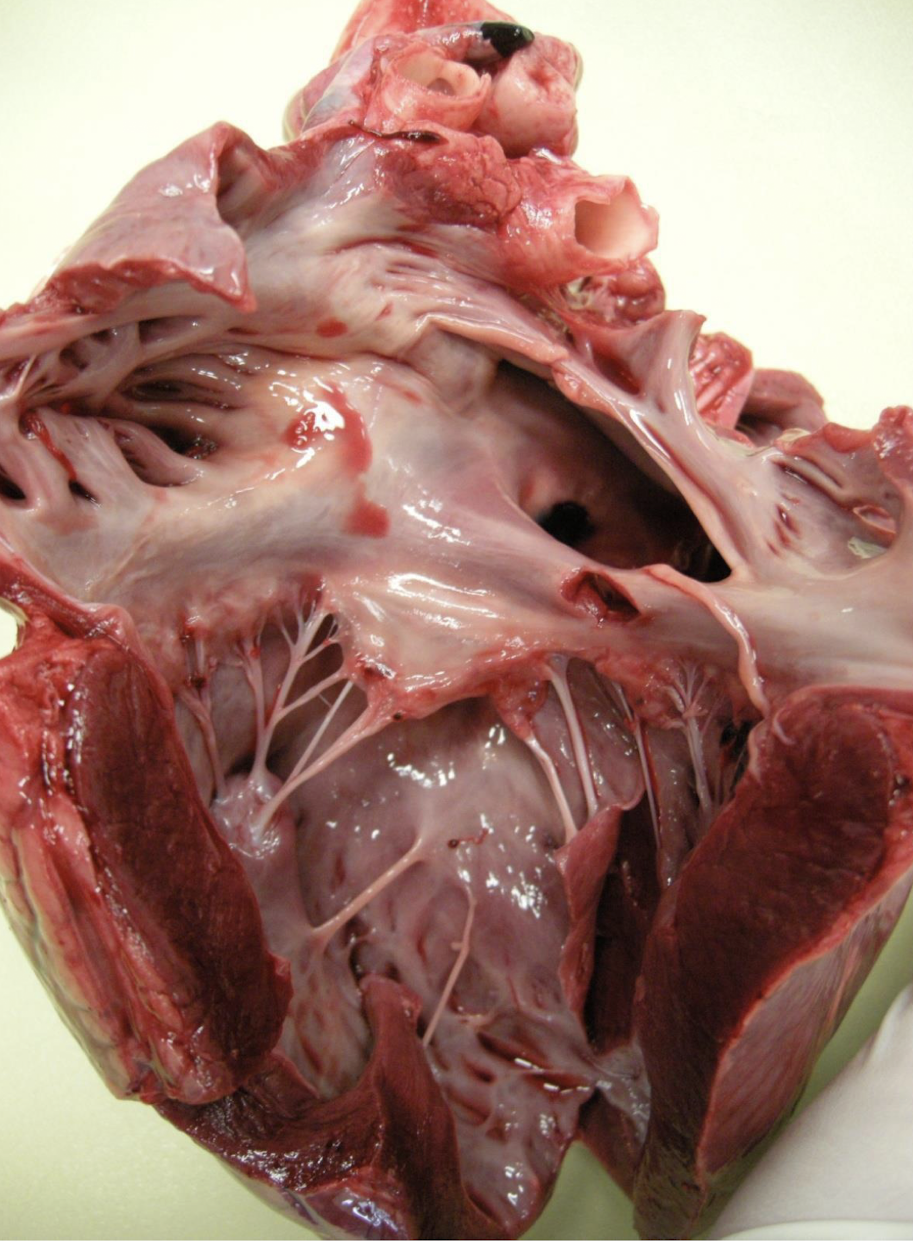
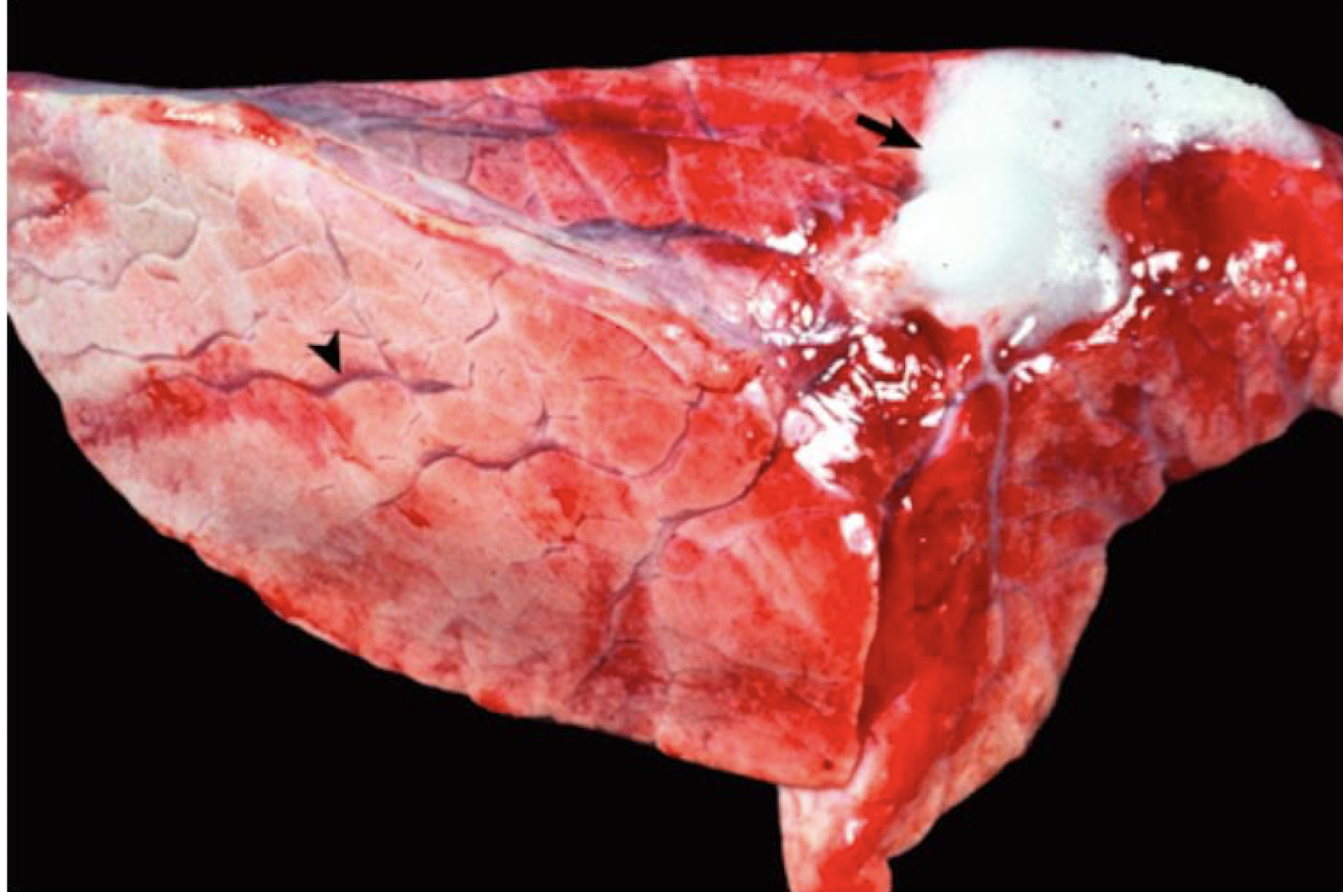
What does tracheal froth tell you?
that the lungs are edematous (indicative of pulmonary edema)
Which side of the heart with heart failure causes this?
left sided heart failure
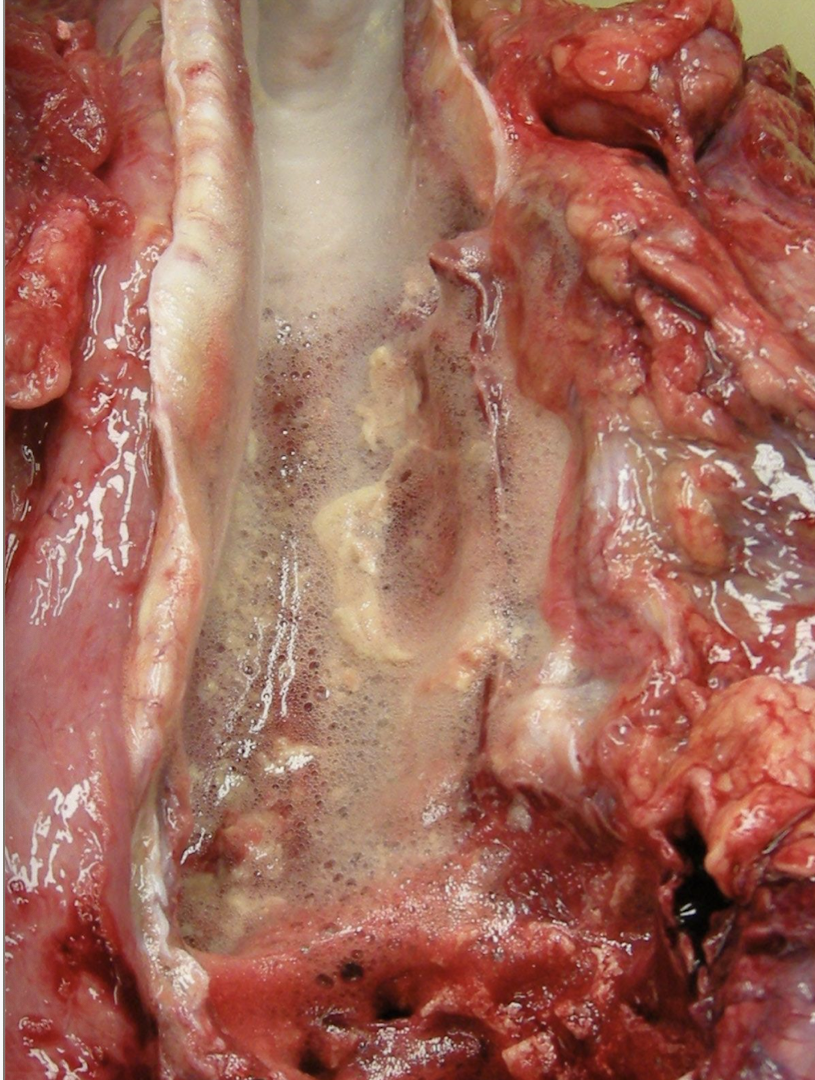
What is this showing?
tracheal froth
What will chronic passive hepatic congestion cause?
yellow tinged fluid found in the abdominal cavity
Which sided heart failure causes chronic passive hepatic congestion?
right sided heart failure
With a liver suffering from chronic passive hepatic congestion, what will it look like on a cut surface? How would it feel?
reticular pattern and “Nutmeg” liver; firm
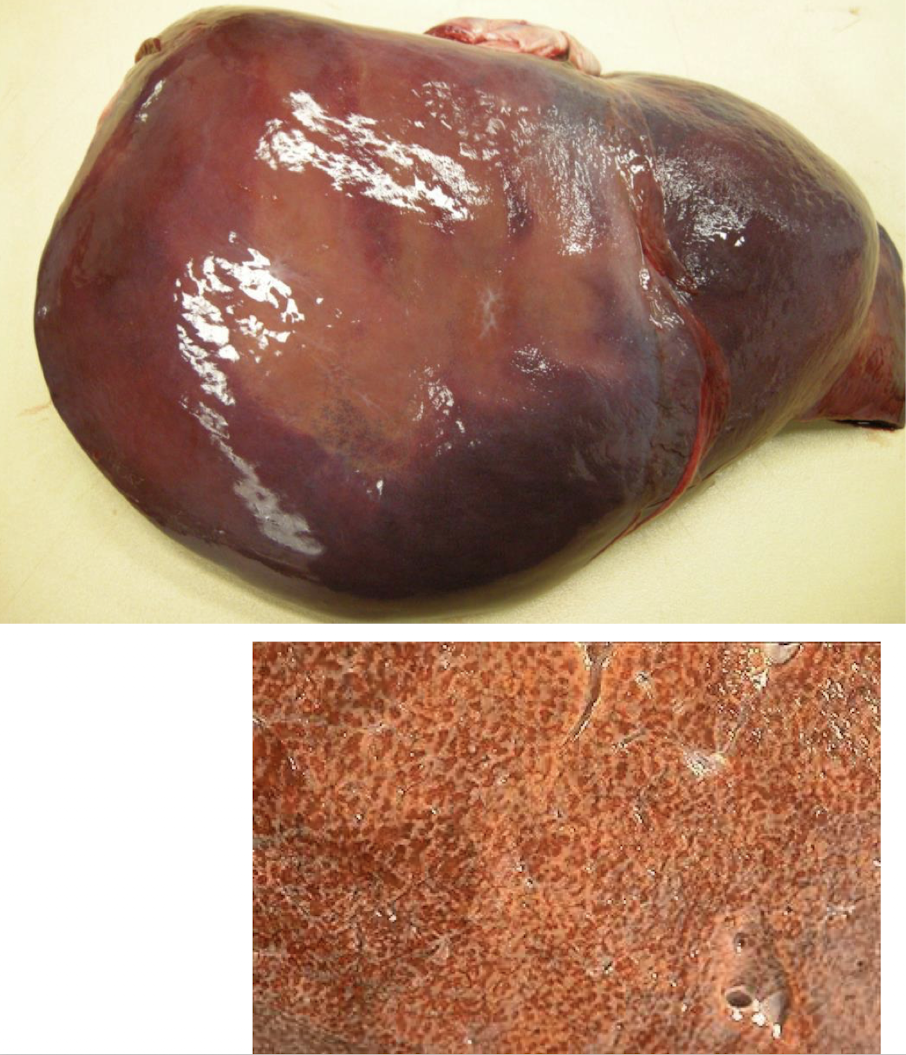
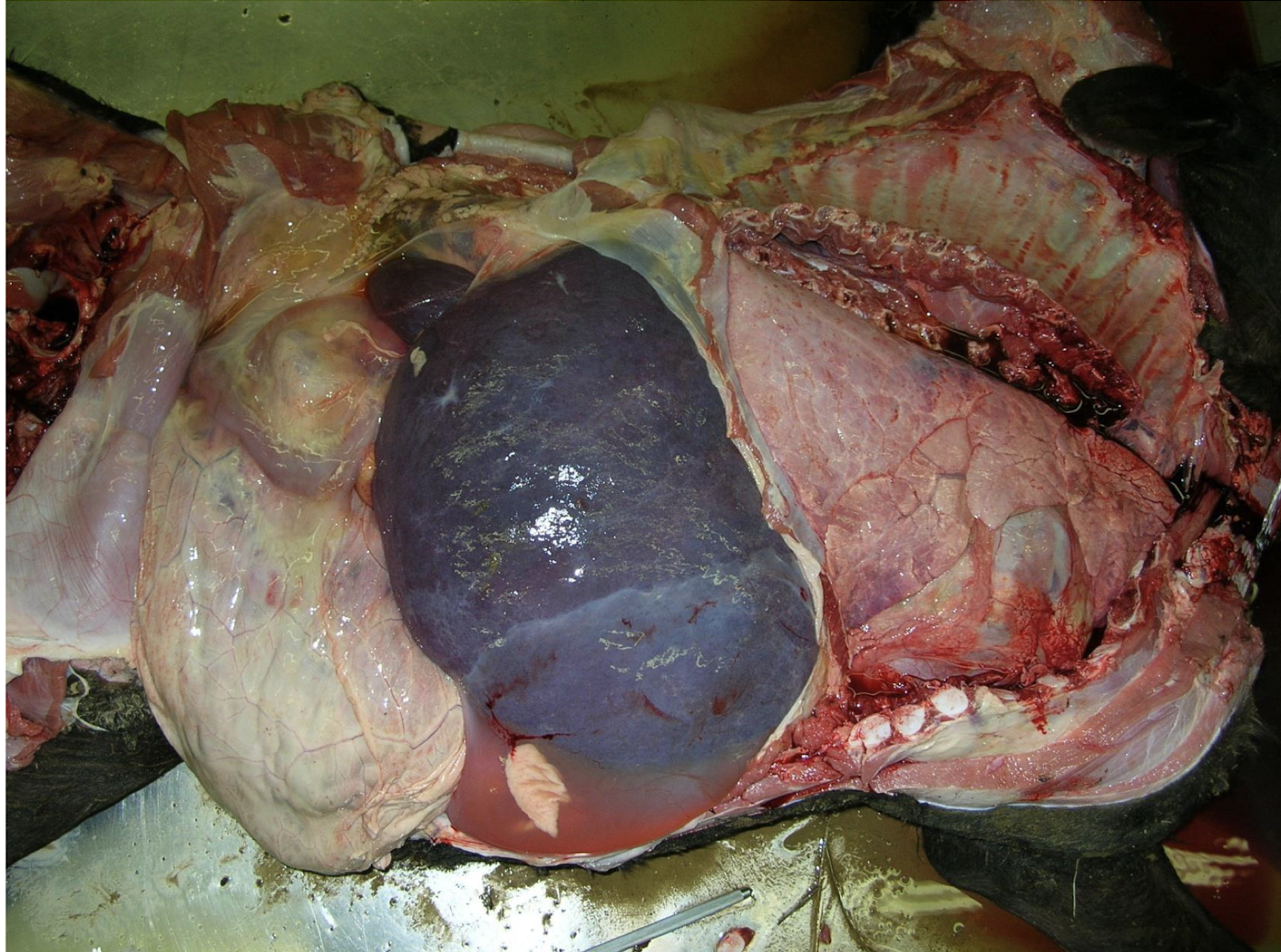
What is this showing?
chronic passive hepatic congestion
What is decreased oncotic pressure (or osmotic pressure) overwhelmingly most often due to? Which one specifically?
decreased plasma proteins; hypoalbuminemia
What are mechanisms of hypoalbuminemia that result in edema?
S
P
P
S
L
P
severe blood loss
protein losing enteropathy
protein losing nephropathy
severe burns
loss of hepatic functional mass
profound malnutrition (emaciation)

What is this an example of?
decreased oncotic pressure

Which mechanism of edema is responsible from bottle jaw caused by the barber pole worm?
decreased oncotic pressure
What is this image showing?
pulmonary edema
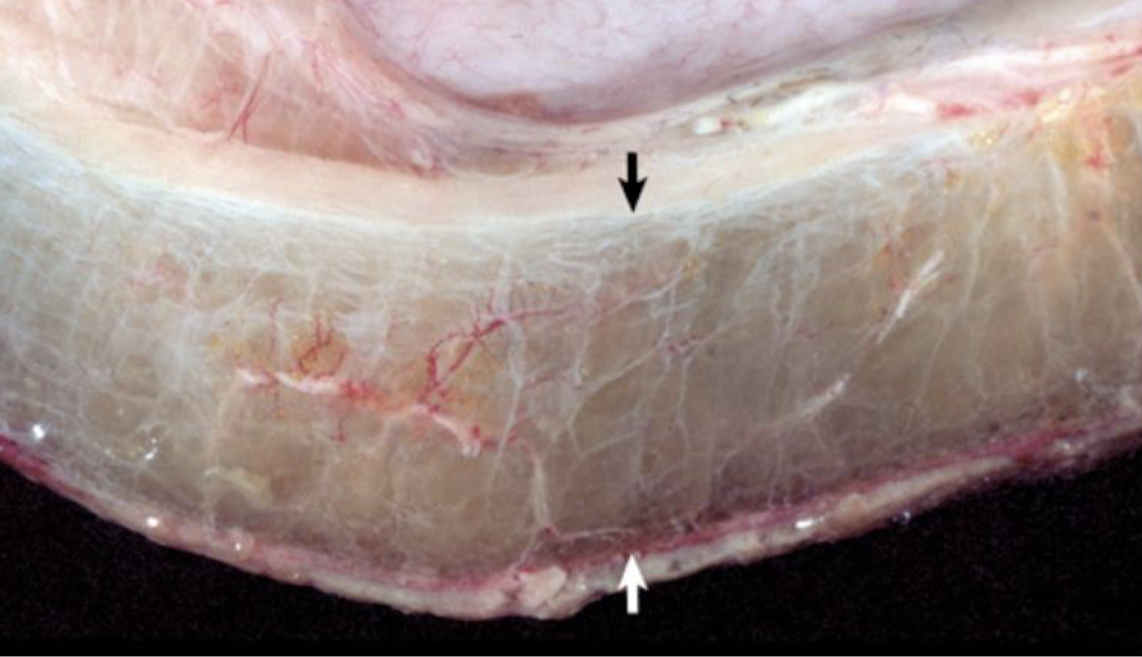
What is this image showing?
intestinal edema of the submucosa
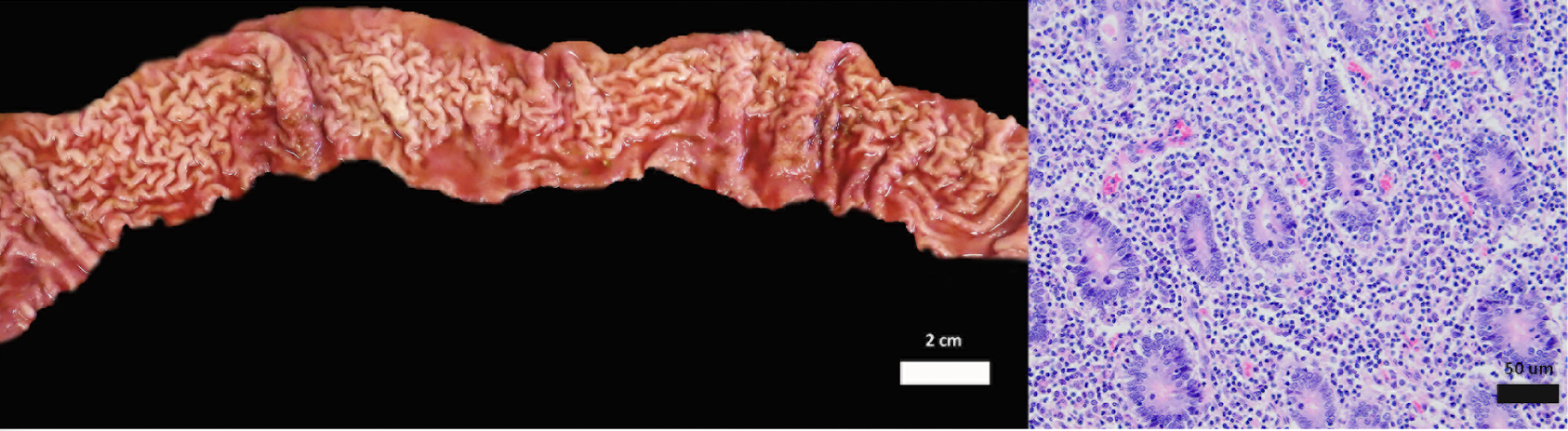
What is this an image of?
equine GI lymphoma
What is the effect of hepatic cirrhosis in equines? What about in dogs and cats? What about in all 3?
liver gets giant; gets smaller; gets fibrous
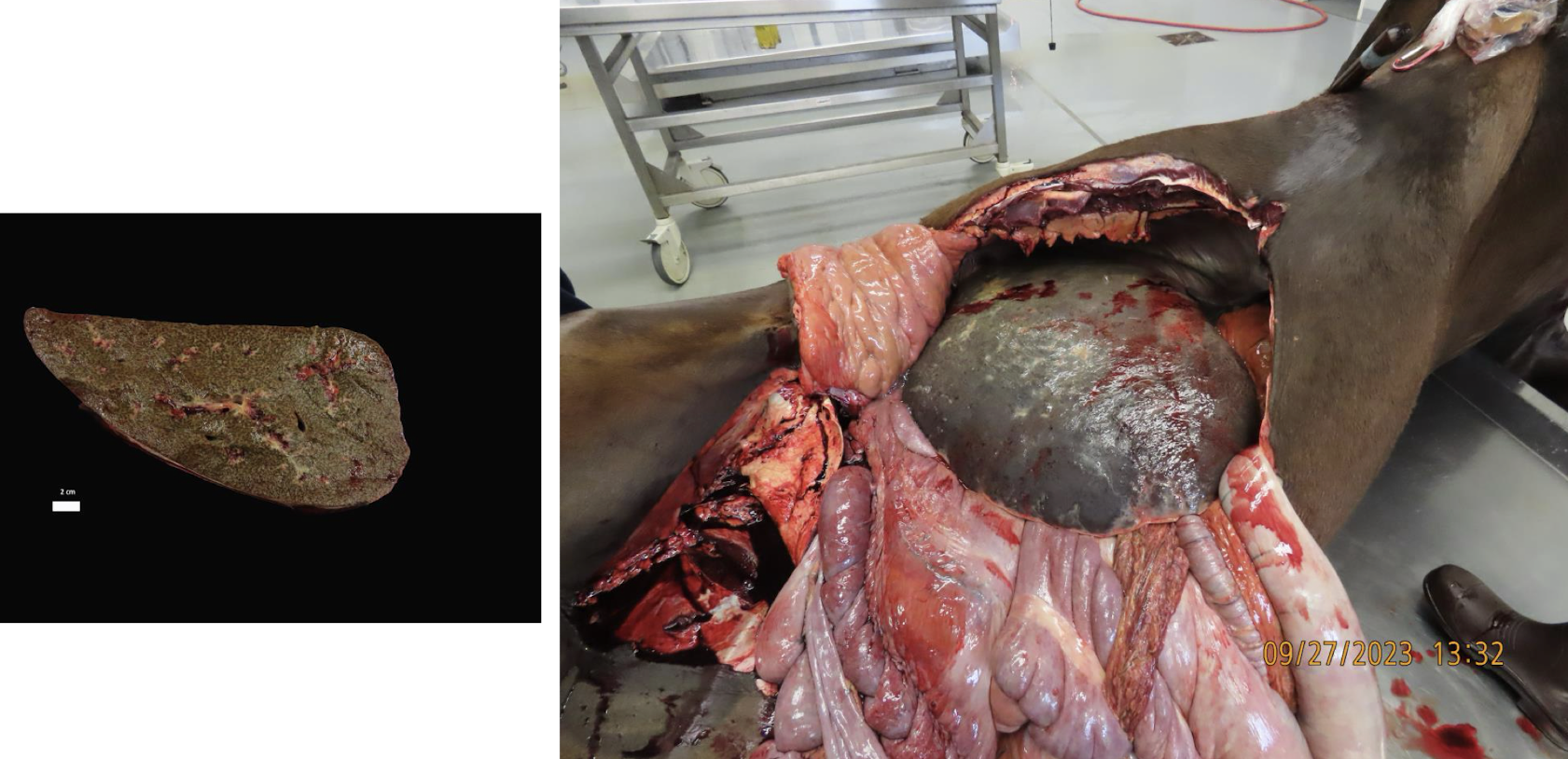
What is this showing?
equine hepatic cirrhosis
reduced ability of the lymphatic system to remove excess fluid
decreased lymphatic drainage
What are causes of decreased lymphatic drainage?
L
L
L
lymphatic vessel compression (neoplasia or inflammation)
lymph vessel constriction (from fibrosis)
lymph vessel blockage (thrombus or embolus)
What is this showing?
puppy with congenital lymphedema

In congenital lymphoma, the lymphatic vessels are either ________ or ________.
hypoplastic; aplastic
condition in which all tissues are edematous
anasarca

What is this showing?
fetal congenital edema (anasarca)
when fluid accumulates in a body cavity (abdomen, thorax, pericardial sac)
effusion
What are different examples of effusion>
A
T
P
abdominal effusion
thoracic effusion
pericardial effusion
What are the three categories of effusions?
pure transudate
modified transudate
exudate
type of effusion with low protein and low cellularity
pure transudate
Pure Transudate:
protein = ________
cellularity = ________
________ fibrinogen
generally ________, ________, to ________ colored fluid
< 2.5 g/dL
< 1500 cells/uL
low
translucent; clear; straw
type of effusion that is high protein and high cellularity
exudate
Exudate:
protein = ________
cellularity = ________
________ therefore ________ fibrinogen
generally ________ or ________
> 2.5 g/dL
> 5000 cells/uL
inflammatory; high
cloudy; opaque
type of effusion that does not fit into the other categories
modified transudate
Modified Transudate:
category in between which is either ________ protein or ________ cellularity or a ________ thereof
protein = ________
cellularity = ________
low; low; combination
> 2.5 g/dL
< 5000 cells/uL
Transudative effusions are generally a result of one of which two mechanisms?
I
D
increased intravascular hydrostatic pressure
decreased oncotic pressure (or osmotic pressure)

What is this an image of?
ascites
thoracic transudative effusion
hydrothorax
pericardial transudative effusion
hydropericardium
abdominal transudative effusion
hydroperitoneum or ascites
True or false: “Hydro” is not used for modified transudate or exudate.
true
What is this showing?
ascites
What are exudative effusions generally a result of?
increased vascular permeability due to inflammation
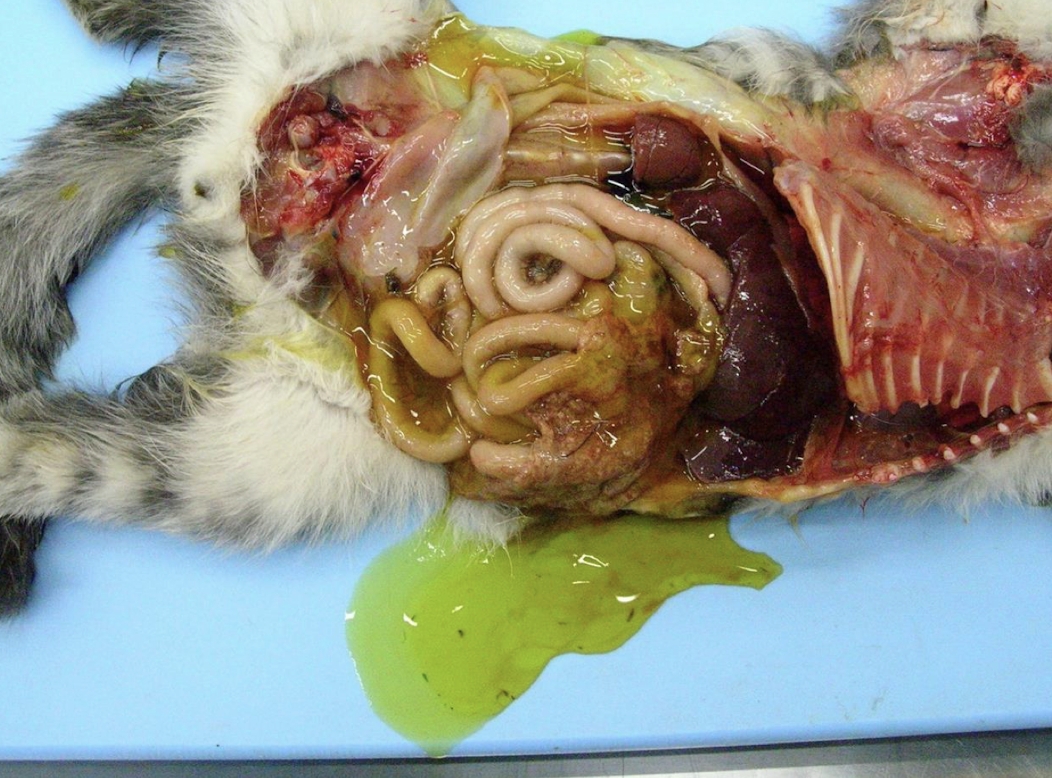
What is this showing?
exudative effusions due to FIP
specific type of effusion (typically thoracic) due to obstruction of the thoracic duct where there is lymph in the thoracic cavity itself that is an opaque white to pink tinged fluid
chylous effusions
What is the protein level in chylous effusions? What can be significant about the protein?
> 2.5 g/dL; may be artifactually increased due to large lipoproteins int he sample increasing the refractive index
What is the cellularity level of chylous effusions?
variable, but usually > 3000 cells/uL
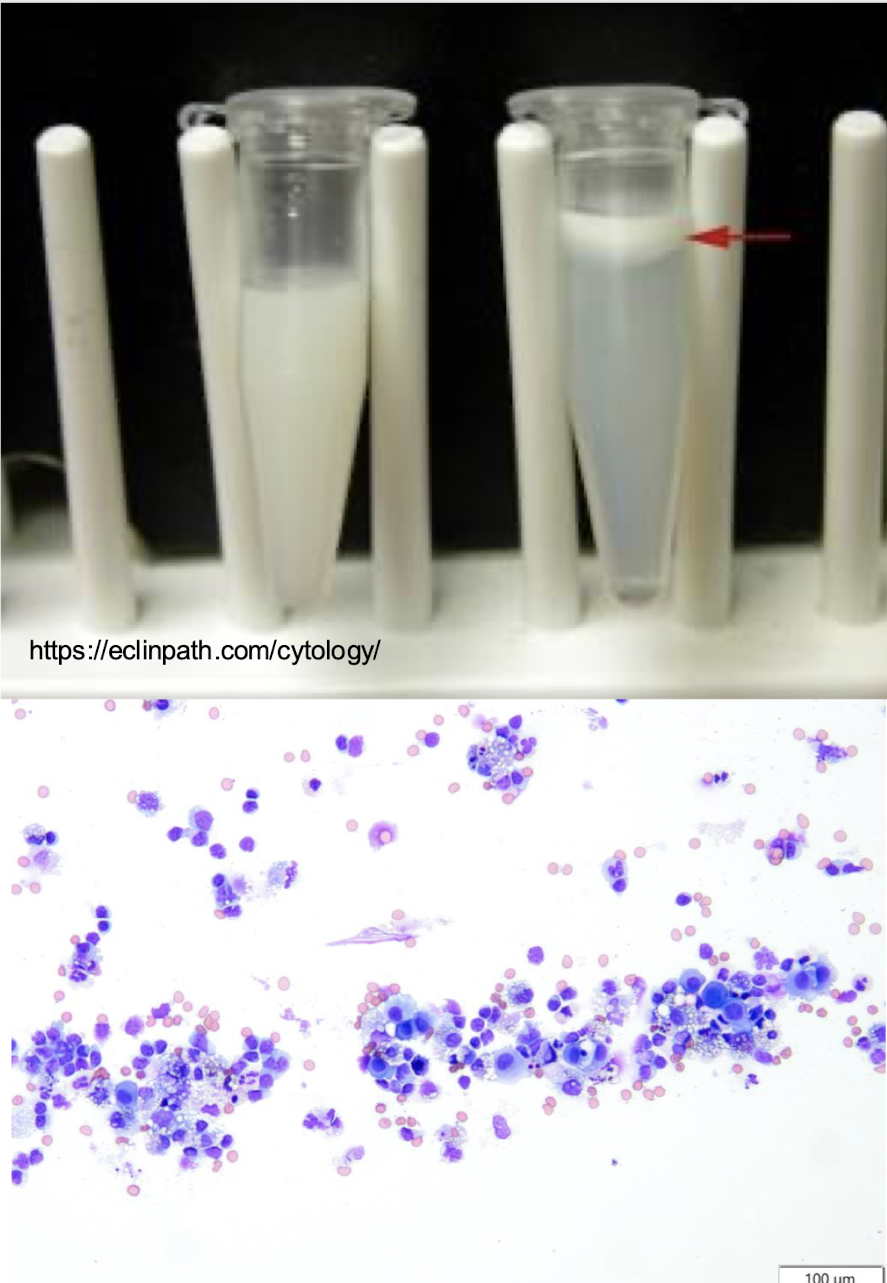
What is this showing?
chylous effusions