Transfusions fusion Hazards & Safety – Ultimate Flashcards (20)
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
What is the primary purpose of the SHOT scheme?
To collect data on Serious Hazards of Transfusion (including near misses) to improve patient safety standards in the UK.
. What does Landsteiner’s Law state regarding blood compatibility?
Individuals produce antibodies against antigens they lack on their own red blood cells
(e.g. Group A individuals have Anti-B antibodies).
. Which blood group is the “universal donor” for red cells vs plasma?
Red cells: Group O (no A or B antigens)
Plasma: Group AB (no Anti-A or Anti-B antibodies)
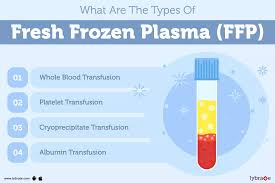
What are the clinical indications for Fresh Frozen Plasma (FFP)?
Replacement of clotting factors (e.g. DIC, liver disease, massive haemorrhage).
What is the specific use of cryoprecipitate?
Concentrated source of fibrinogen, used when fibrinogen is low (< 1.5 g/L).
What is the “two-sample rule” and why does it exist?
Requirement for two separately taken blood samples to confirm blood group before issuing red cells.
Purpose: Prevents WBIT (Wrong Blood in Tube) errors.
What is the most common cause of ABO-incompatible transfusions?
Human error, particularly failure of positive patient identification at the bedside.
What defines an Acute Haemolytic Transfusion Reaction (AHTR)?
Recipient a occurs within 24 hours, when recipient antibodies (usually IgM anti-A/anti-B) destroy donor red cells, causing rapid intravascular haemolysis, fever, and shock.
What defines a Delayed Haemolytic Transfusion Reaction (DHTR)?
Occurs days to weeks later.
Caused by IgG alloantibodies that were undetectable pre-transfusion but rise after re-exposure (anamnestic response).
What is Transfusion-Associated Circulatory Overload (TACO)?
Pulmonary oedema due to excessive or rapid transfusion.
Key signs: Hypertension, raised JVP, improves with diuretics.
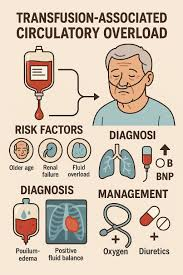
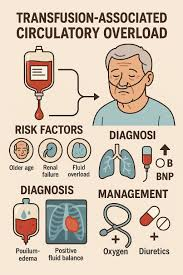
How is TACO prevented in high-risk patients?
TACO prevention in high-risk patients includes careful risk assessment, weight-adjusted transfusion volumes, and slow transfusion rates (with close monitoring).
. What is Transfusion-Related Acute Lung Injury (TRALI)?
Acute hypoxia caused by donor plasma antibodies activating recipient neutrophils in the lungs.
Key signs: Hypotension, fever, no response to diuretics.
How is the risk of TRALI reduced?
Use of male-only plasma (females more likely to have antibodies from pregnancy).
What is Transfusion-Associated Graft-versus-Host Disease (TA-GvHD)?
A usually fatal condition where donor T-lymphocytes attack recipient bone marrow and tissues.
Which patients require irradiated blood components?
Immunocompromised patients (e.g. Hodgkin lymphoma, stem cell transplant recipients) to prevent TA-GvHD.
What is a Febrile Non-Haemolytic Transfusion Reaction (FNHTR)?
Temperature rise ≥ 1 °C during transfusion due to cytokines or recipient antibodies against donor white cells.
What causes Post-Transfusion Purpura (PTP)?
Recipient antibodies against human platelet antigens (HPA), destroying both transfused and own platelets 5–12 days post-transfusion.
Which patients require CMV-negative blood products?
Pregnant women (especially intrauterine transfusions) and neonates.
What is the main long-term risk for transfusion-dependent patients?
Iron overload (haemosiderosis), requiring iron chelation therapy.
What is the immediate management of any suspected severe transfusion reaction?
Stop the transfusion immediately
Maintain IV access with saline
Re-check patient identity and blood unit labels