Unit 7: Hormonal control in plants and animals
1/140
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
141 Terms
local regulators
chemical signaling molecule that acts on nearby cells through diffusion, such as cytokines and neurotransmitters
hormones
secreted molecule that circulates throughout the body and stimulates specific cells.
exocrine gland
a gland that secretes substances into a body cavity or onto the body surface.
sweat and digestive juices
endocrine gland
a gland that secreates subtances that control growth and metabolism into the blood stream to be transported to other parts of the body
what are most hormones derived from
amino acids, polypeptides, or steroids.
steroid hormones need what to travel through blood
need to bind to transport proteins (also known as carrier proteins or binding globulins) to travel through the bloodstream.
polypeptide based hormones need what to go through blood
can travel through blood freely
what are the hormones secreted by the adrenal cortex and gonads compared to everyother endocrine gland
steroids,
all others secrete hormones derived from proteins or amino acids
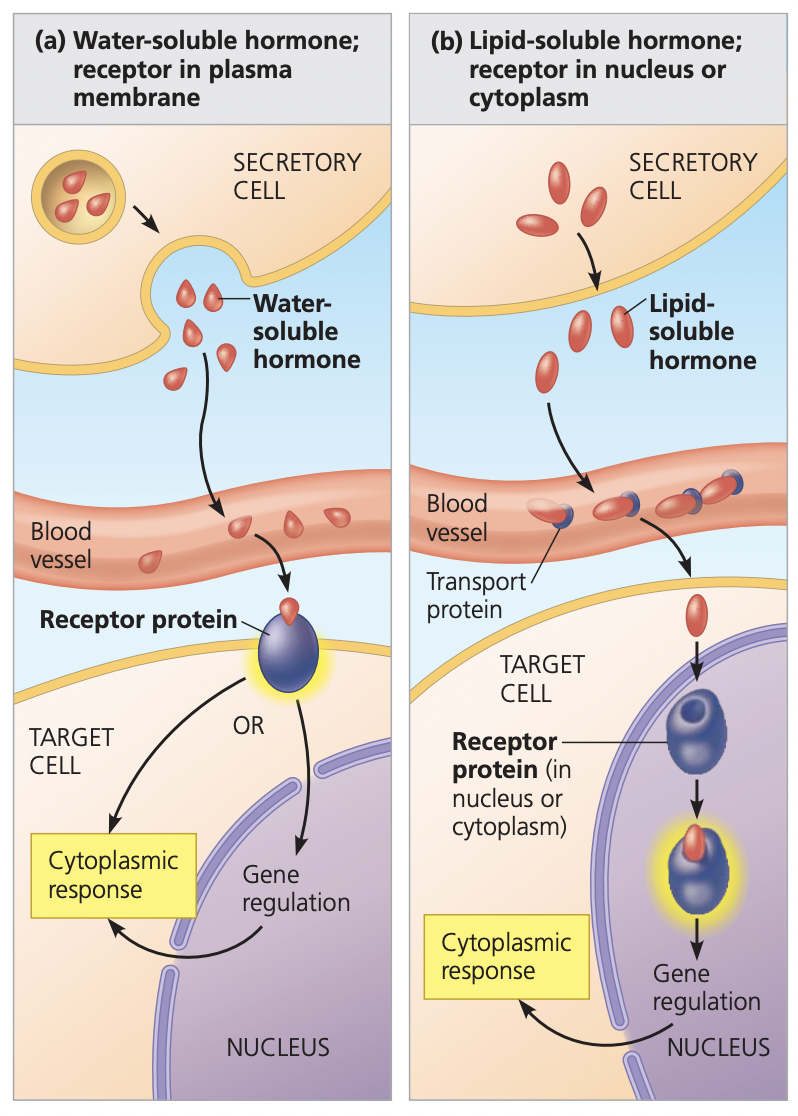
How do steriod hormones act
they are lipid soluble and hydrophobic so they can enter target cells and bind with intracellular receptors that elicit a response
how do polypeptide hormones act
they are water soluble and hydrophilic bind to specific receptors on the outside of the cell membrane to initiate a signal transduction pathway
What feature of a hormone determines whether it will initiate a signal transduction pathway or regulate gene expression
whether it is a steroid or polypeptide-based hormone.
Steroid-based hormones are hydrophobic, which allows them to enter the cell and regulate gene expression
Polypeptide-based hormones are hydrophilic and must interact with a cell-surface receptor protein, which creates a signal transduction pathway
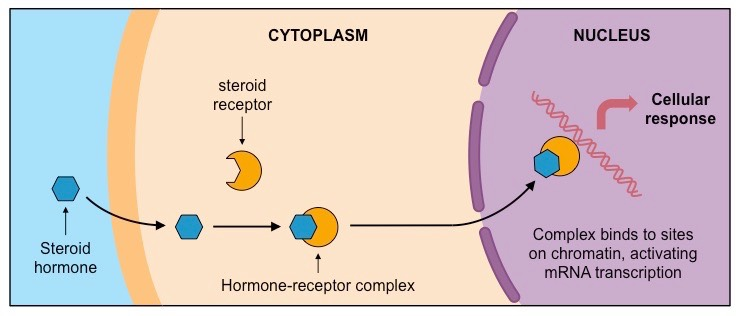
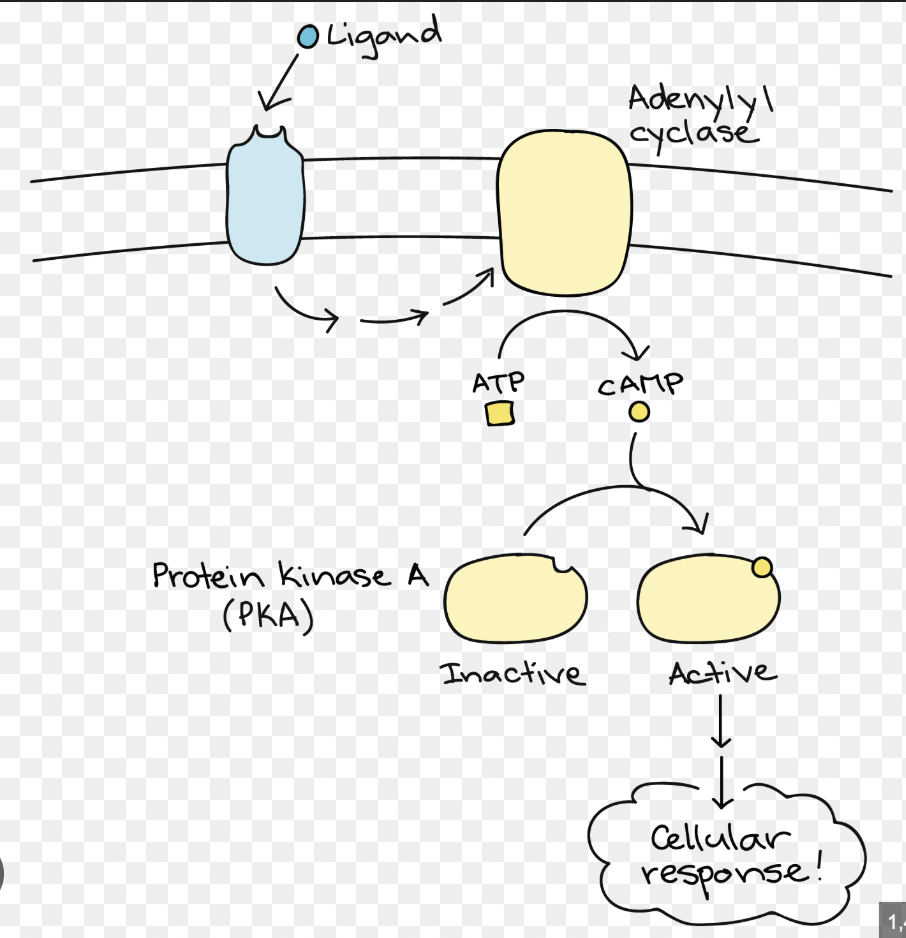
how does the signal transduction model work
A water-soluble hormone binds to an extracellular protein receptor
signal travels to adeline cyclase to create cAMP with ATP
The cAMP is used as a secondary messenger and activates an inactive protein
activated protein conducts a cellular response
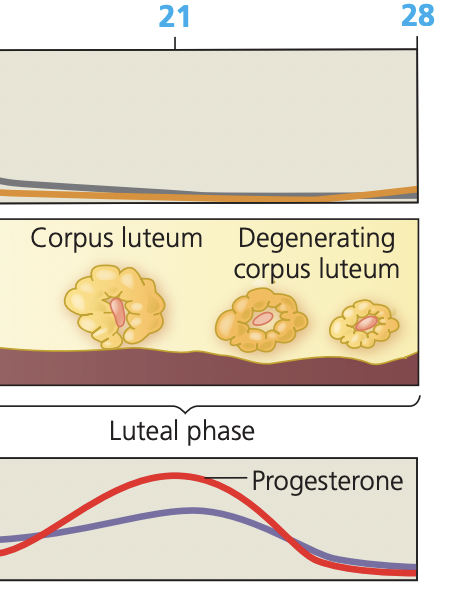
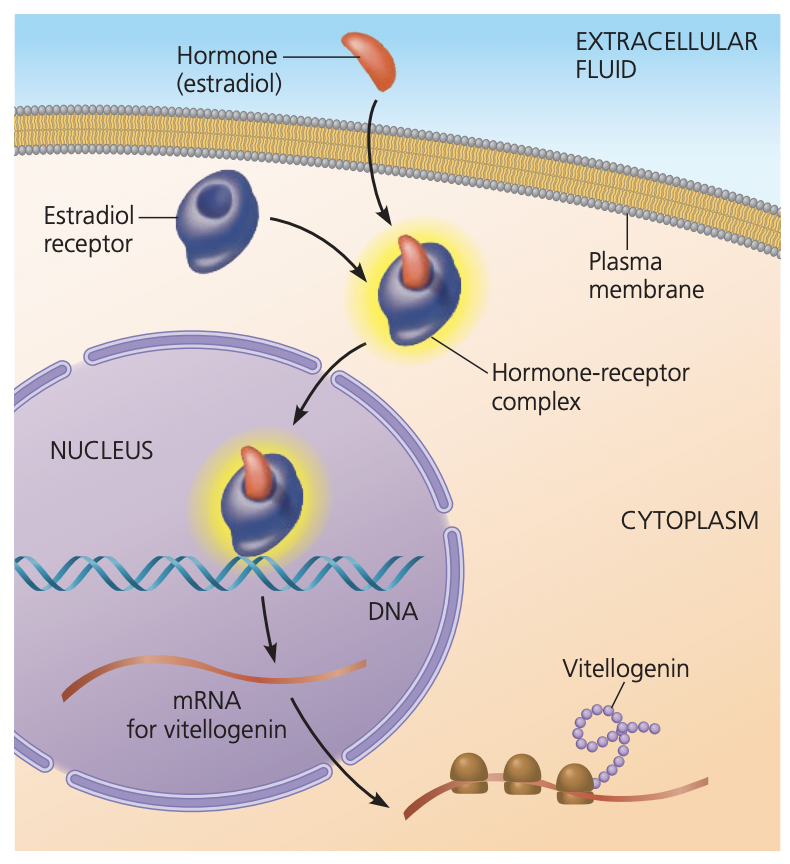
Explain the general mechanism by which lipid-soluble (hydrophobic) steroid hormones affect target cells
A steroid hormone goes through the cell membrane
binds to a steroid hormone receptor located in the cytosol, creating a hormone receptor complex
Complex moves into the nucleus, where it interacts with DNA
This then activates certain transcription and gene expression
cell's response to stimulation by a polypeptide hormone
Is it rapid or slow, short-lived or long-lived?
rapid and short-lived
Rapid: effects begin within seconds to minutes because existing proteins or enzymes are modified (no need to make new ones).
Short-lived: once the hormone is degraded or signaling stops and effect fades.
cell's response to stimulation by a steroid hormone
Is it rapid or slow, short-lived or long-lived?
slow and longlived
Slow: it takes time (minutes to hours) for transcription and translation of new proteins to occur.
Long-lived: newly synthesized proteins remain active even after the hormone is gone, so effects can last hours to days.
The particular proteins that a cell possesses determine what
the signal molecules it responds to and the nature of the response
target specificity of hormones in terms of receptors
hormone’s target specificity is determined by the presence of specific receptors on target cells that only hormones can bind to
Why does epinephrine in a liver cell cause that cell to hydrolyze glycogen to glucose, whereas epinephrine in skeletal muscle causes it to dilate?
though epinephrine is the same hormone, it will create a different effect with different target cells
this is due to the cells haveing different transduction pathways and different receptors
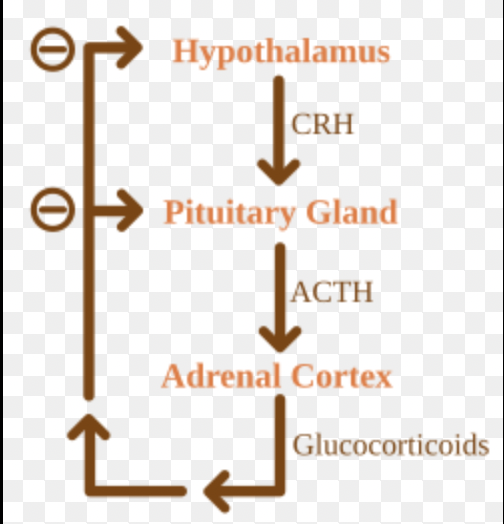
how is the endocrine system regulated
negative feedback loops
direct negative feedback loop
a regulatory pathway where the final product in a single chain directly inhibits its own production
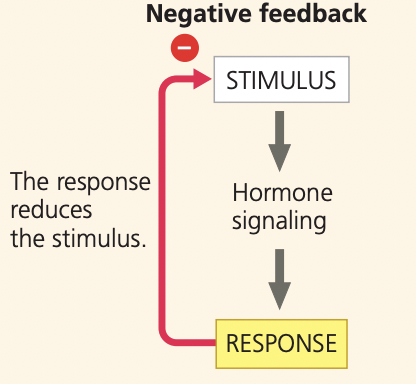
indirect negative feedback loop
Involves multiple hormone levels in a regulatory chain. The final hormone in the pathway feeds back to inhibit the earlier glands (often the hypothalamus and/or pituitary).
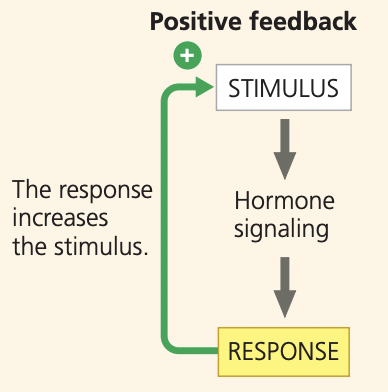
positive feedback
When the final product in a chain increases, the production of the product
What are tropic hormones
hormones that stimulate other endocrine glands to produce and release their hormones
The hypothalamus produces TRH so that the anterior pituitary can produce TSH
why is it good to have a pair of hormones that have opposite effects
they work together to fine tune a response
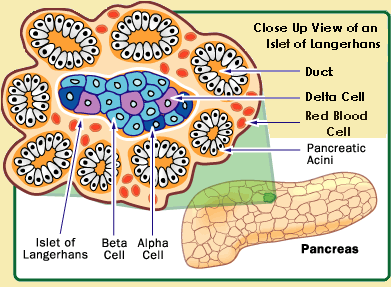
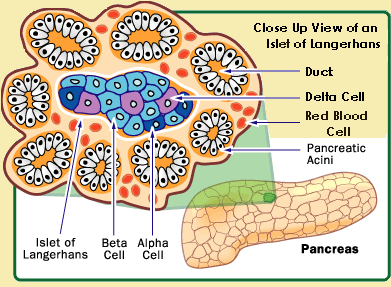
What type of cell in the pancreas synthesizes insulin
Beta cells: the majority of cells within the islets of Langerhans
insulin
Lowers blood glucose level
peptide hormone
What type of cell in the pancreas synthesizes glucagon
Alpha cells: found in the islets of Langerhans
Glucagon
Raises blood glucose level
peptide hormone
Where is the pancreas located in relation to the stomach and small intestine?
the pancreas is posterior to the stomach and supperior to the small intestins
connects via the duodenum
How does insulin affect the uptake of glucose into muscle and adipose tissue?
Insulin increases glucose uptake in muscle and adipose tissue
how does insulin affect the synthesis (stimulate or inhibit) and degradation (stimulate or inhibit) of fats
fat synthesis (lipogensis): stimluated
fat degradation (lipolysis): inhibited
insulin is responsible for the uptake and storage of glucose
How does insulin affect the synthesis (stimulate or inhibit) and degradation (stimulate or inhibit) of protein
Protein synthesis: stimulated
Protein degradation: inhibited
insulin promotes the building of muscles
How does insulin affect the synthesis (stimulate or inhibit) and degradation (stimulate or inhibit) of glycogen
glycogen synthesis: stimulated
glycogen degradation: inhibited
insulin wants to increase storage of sugar
How is the blood sugar level regulated and maintained after a meal high in carbohydrates is eaten
After a meal high in carbs, the blood glucose levels are going to be high
Insulin is released to reduce blood sugar levels by
stimulating glucose uptake
glycogen formation
muscle growth
inhibit alpha cells
stimulate beta cells
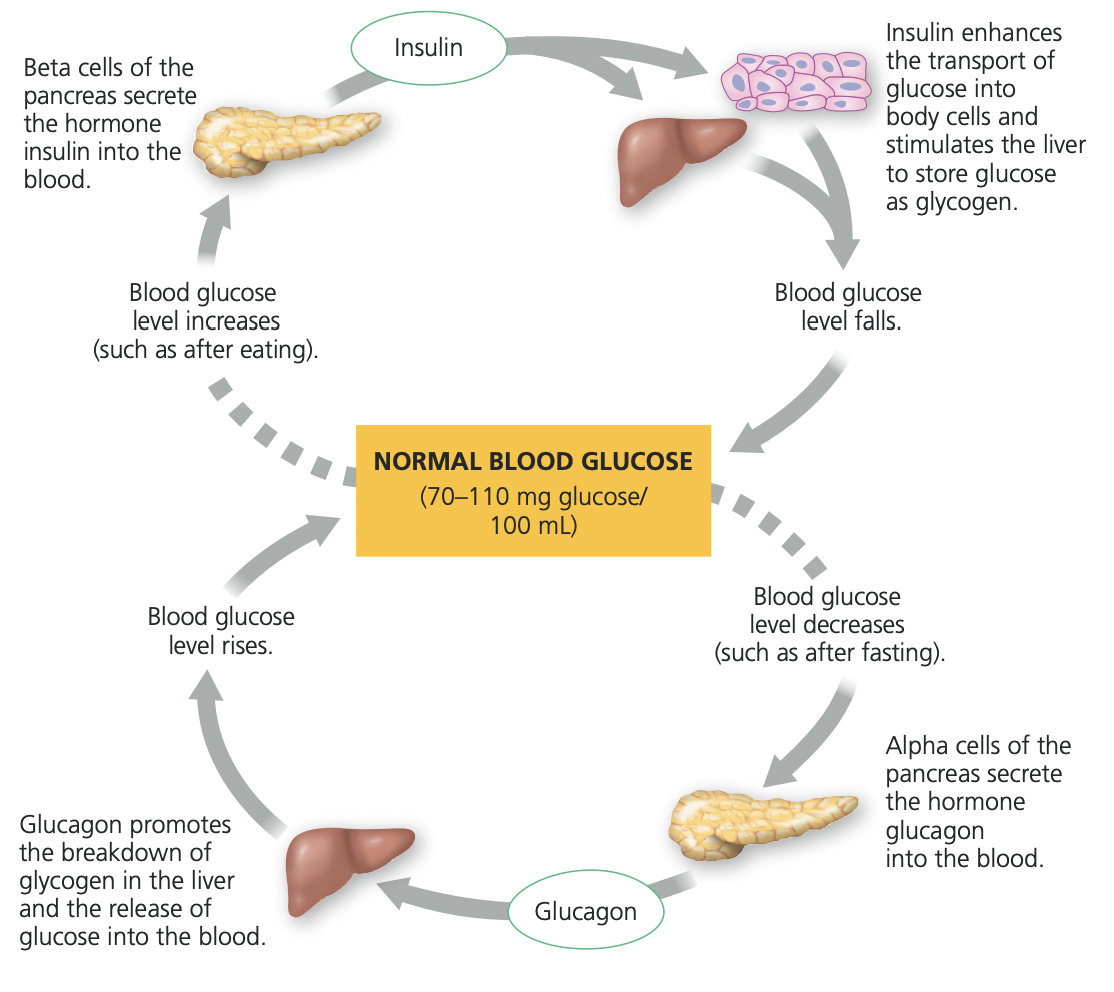
How is the blood sugar level regulated and maintained several hours after a meal high in carbohydrates is eaten
Between meals, glucose levels decrease
Glucagon is released to increase blood sugar levels
works mainly in the liver
stimulate glycogenolysis
stimulates gluconeogenesis
inhibit beta cells
stimulate alpha cells
Diabetes mellitus has been described as "starvation in the midst of plenty." Explain the meaning of this statement
It describes how, despite high levels of sugar (glucose) in the blood, the body's cells are unable to use it for energy
juvenile-onset or insulin dependent Type 1 diabetes
autoimmune disorder in which the immune system destroys the beta cells of the pancreas and thus no insulin is produced
Adult-onset or non-insulin-dependent diabetes
Type 2 diabetes
When the target cells are unable to take up glucose despite insulin being produced. The receptors get desensitized to the amount of insulin and stop working
one major symptom of Type 1 diabetes and how it relates to the function of insulin
one major symptom is sweet and excessive urine. This is due to the fact that since no glucose is being taken up the kidneys need to filter out all of the excess sugar in the blood, which pulls water with it.
In a normal individual, what happens to insulin secretion when the blood glucose level is high? ...low?
High: insulin secreation increases
low: insulin secreation decreases
parts of the pituitary gland
Anterior Pituitary
Posterior Pituitary
Completely seperate systems
anterior pituitary
endocrine gland that synthesizes and secretes hormones in response to hormones from the hypothalamus
posterior pituitary
stores and secretes hormones synthesized in the hypothalamus.
extension of the hypothalamus
What is the function of the hormones of the anterior pituitary and hypothalamus
They have master regulating roles,
orchestrate the action of several glands through complex negative feedback loops.
Describe the structural and functional relationships between the hypothalamus and the pituitary
The hypothalamus acts as the command center which regulates how much master hormones are produced from the pituitary
Describe the relative location of the hypothalamus and pituitary gland within the skull
The hypothalamus is superior to the pituitary
where is oxytocin and ADH are synthesized and where they are stored.
They are synthesized from neurosecretory cells of the hypothalamus
stored in the posterior pituitary gland
Neurosecretory cells of the hypothalamus
produce neurohormonse and are alink between the nervous and endocrine system
Oxytocin
has functions related to reproduction.
controls milk secretion by the mammary glands
regulates uterine contractions during birthing
maternal care
pair bonding
sexual activity
peptide hormone
ADH
vasopressin
regulates kidney function
ADH increases water retention in the kidneys, helping maintain normal blood osmolarity
has a role in social behavior
peptide hormone
What is the effect of ADH on urine volume
decreases, ADH promotes water retention in the kidneys
Describe the role of releasing hormones produced in the hypothalamus for hormones produced by the anterior pituitary.
Hormones from the hypothalamus control the amount of release of hormones produced in the anterior pituitary
Describe the special arrangement of blood vessels in the hypothalamus and anterior pituitary (portal system)
a specialized blood vessel network connecting the hypothalamus and the anterior pituitary gland
ensures that inhibiting hormones secreted by the hypothalamus reach the anterior pituitary quickly and in high concentration
2 capillary beds
Thyroid-stimulating hormone
(TSH)
site of synthesis
major role
site of synthesis
anterior pituitary gland
major role
stimulate the thyroid gland to produce and release thyroid hormones (T3 and T4)
Gonadotropic hormones (FSH and
LH)
site of synthesis
major role
site of synthesis
anterior pituitary gland
major role
regulate gametogenesis (the formation of sperm and eggs)
steroidogenesis (production of sex hormones: estrogen and testosterone)
Adrenocorticotropic hormone (ACTH)
site of synthesis
major role
site of synthesis
anterior pituitary gland
major role
stimulate the adrenal cortex to produce and release cortisol
Prolactin (PRL)
site of synthesis
major role
site of synthesis
anterior piruitary gland
major function
stimulate milk production in the mammary glands after childbirth
Growth hormone (GH)
site of synthesis
major role
site of synthesis
anterior pituitary gland
major role
Promoting linear growth in children and adolescents
Gonadotropic-releasing hormone
(GnRH)
site of synthesis
major role
site of synthesis
hypothalamus
major function
regulate the reproductive system by controlling the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland
why is the pituitary gland called the master gland
it controls the functions of many other endocrine glands by releasing hormones that stimulate them
does the pituitary gland control all endocrine glands
no, it controls most
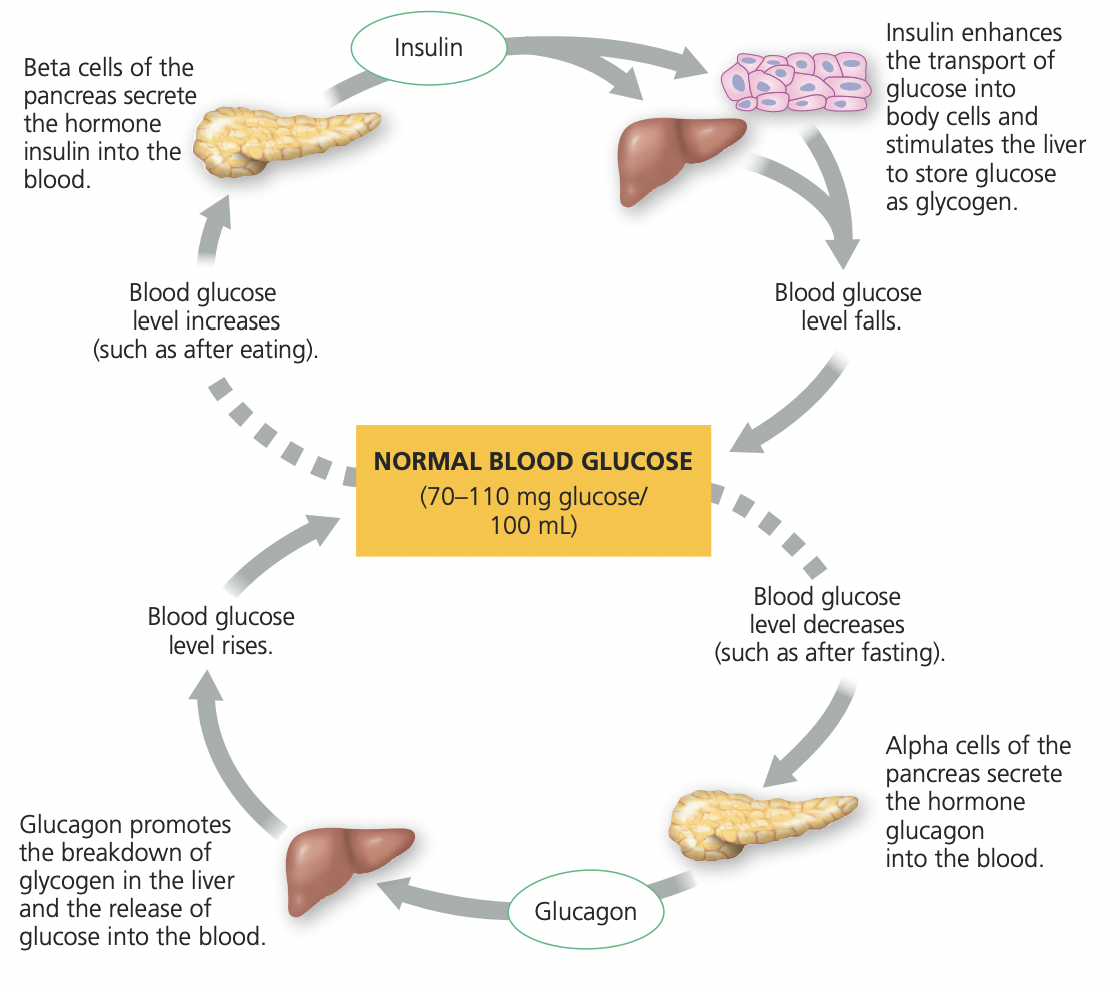
describe the negative feedback control of thyroid hormone secretion. Is this a direct or indirect negative feedback loop?
thyroid hormone levels drop below the normal range
detected by sensory neurons, which send a signal to neurosecretory cells in the hypothalamus.
Neurosecretory cells secrete thyrotropin-releasing hormone (TRH ) into the portal system to the anterior pituitary gland
TRH causes the anterior pituitary to secrete thyroid-stimulating hormone (TSH, also known as thyrotropin) into the circulatory system.
TSH stimulates endocrine cells to release T3 and T4 into the blood
Thyroid hormone levels return to normal, and excess thyroid hormones block TRH release in the hypothalamus
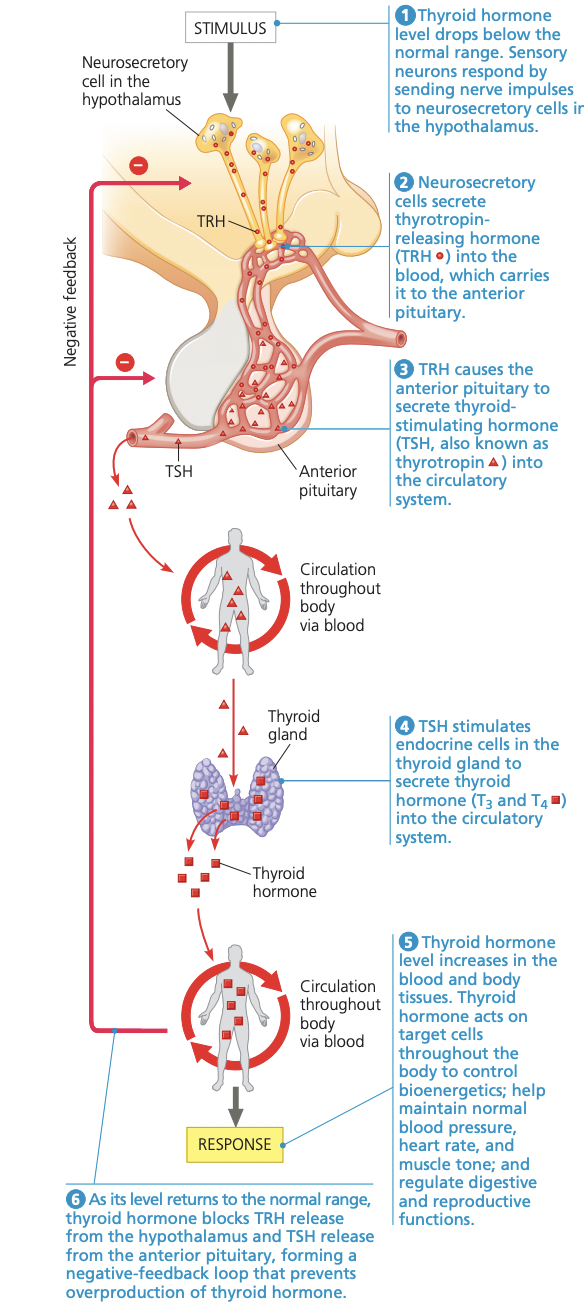
is the thyroid hormones (T3 and T4) hydrophilic or hydrophobic
hydrophobic
how does T3 and T4 initiate the response pathway
acting on target cells through nuclear receptors to alter gene expression
The thyroid hormones are derived from what molecule?
the amino acid tyrosene
What effect do T3 and T4 have upon growth and development?
promotes normal growth in the body, particularly in the brain and skeleton
What happens to individuals with a congenital (from birth) deficiency of T3 and T4? And what is it called
hypothyrodism
weight gain, lethargy, and intolerance to cold in adults
What happens to individuals with a congenital (from birth) overproduction of T3 and T4? And what is it called
hyperthyroidism
high body temperature, profuse sweating, weight loss, irritability, and high blood pressure
State the effect of T3 and T4 upon homeostasis, particularly the rate of cellular metabolism
T3 and T4 increase the basal metabolic rate (BMR) by stimulating cells to produce more ATP.
They increase the number and activity of mitochondria
leads to higher oxygen use and energy output.
This raises body temperature
helping maintain thermal homeostasis.
More T₃/T₄ → Faster metabolism → More ATP and heat production
Less T₃/T₄ → Slower metabolism → Less ATP and heat production
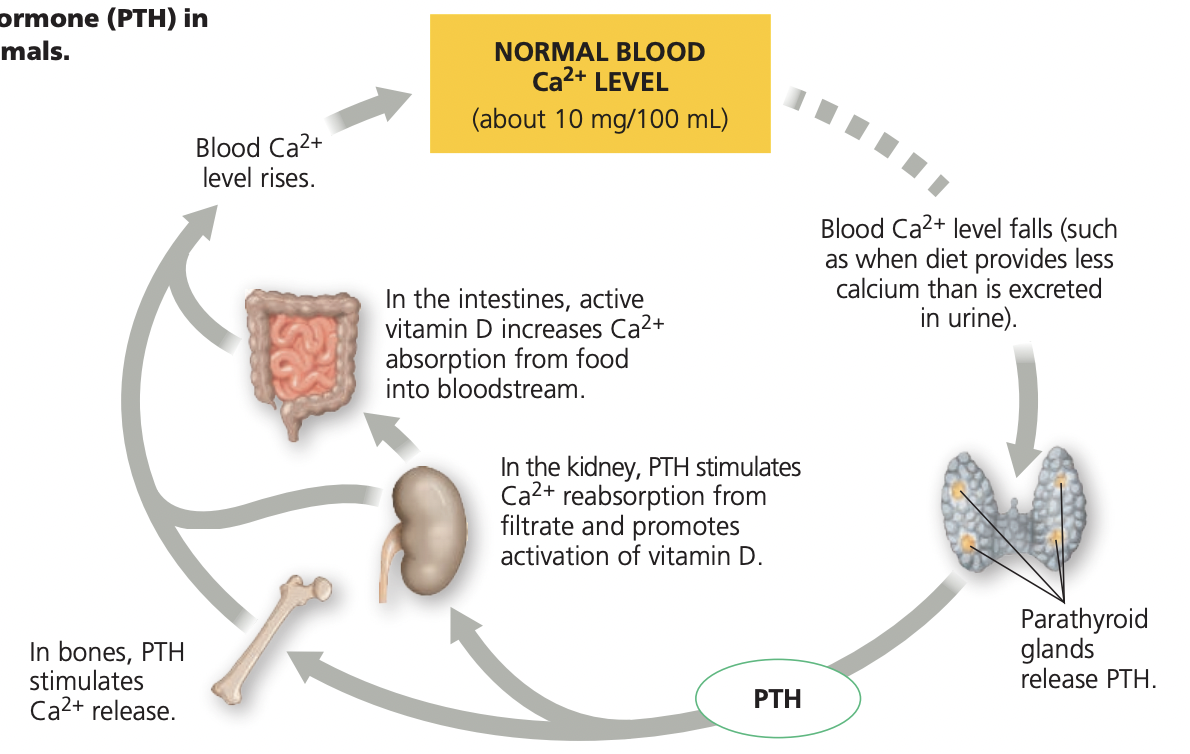
Describe how parathyroid hormone (PTH) regulates blood calcium ion levels.
blood calcium levels fall below average
Parathyroid glands release PTH in response
PTH goes to the bone and stimulates Ca2+ release
In the kidney, PTH stimulates
Ca2+ reabsorption from
filtrate and promotes
activation of vitamin D
The activated vitamin D causes the small intestines to reabsorb more Ca2+ from food
Ca levels in blood rise
place where Ca2+ is highest in a cell. By what process is Ca2+ accumulated in these structures?
endoplasmic reticulum of the cell
active transport via Ca2+ pump
What is the direction Ca2+ ions move when the channel is open
from the ERs to the cytoplasm
the importance of Ca2+ in cell function
Calcium ions act as a universal intracellular signal
a kind of “on switch” for many biological processes.
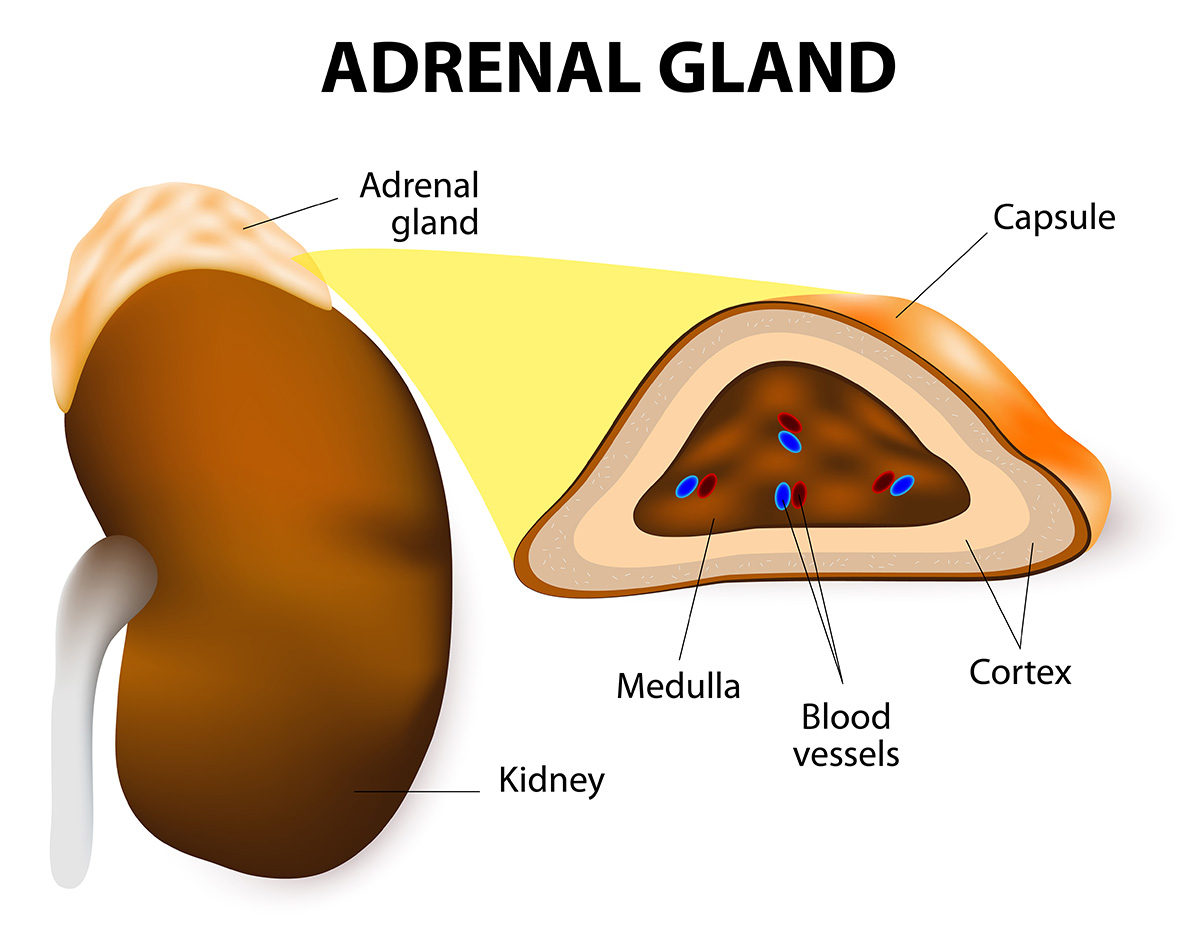
adreanal gland parts
cortex and medulla
these parts are seperate
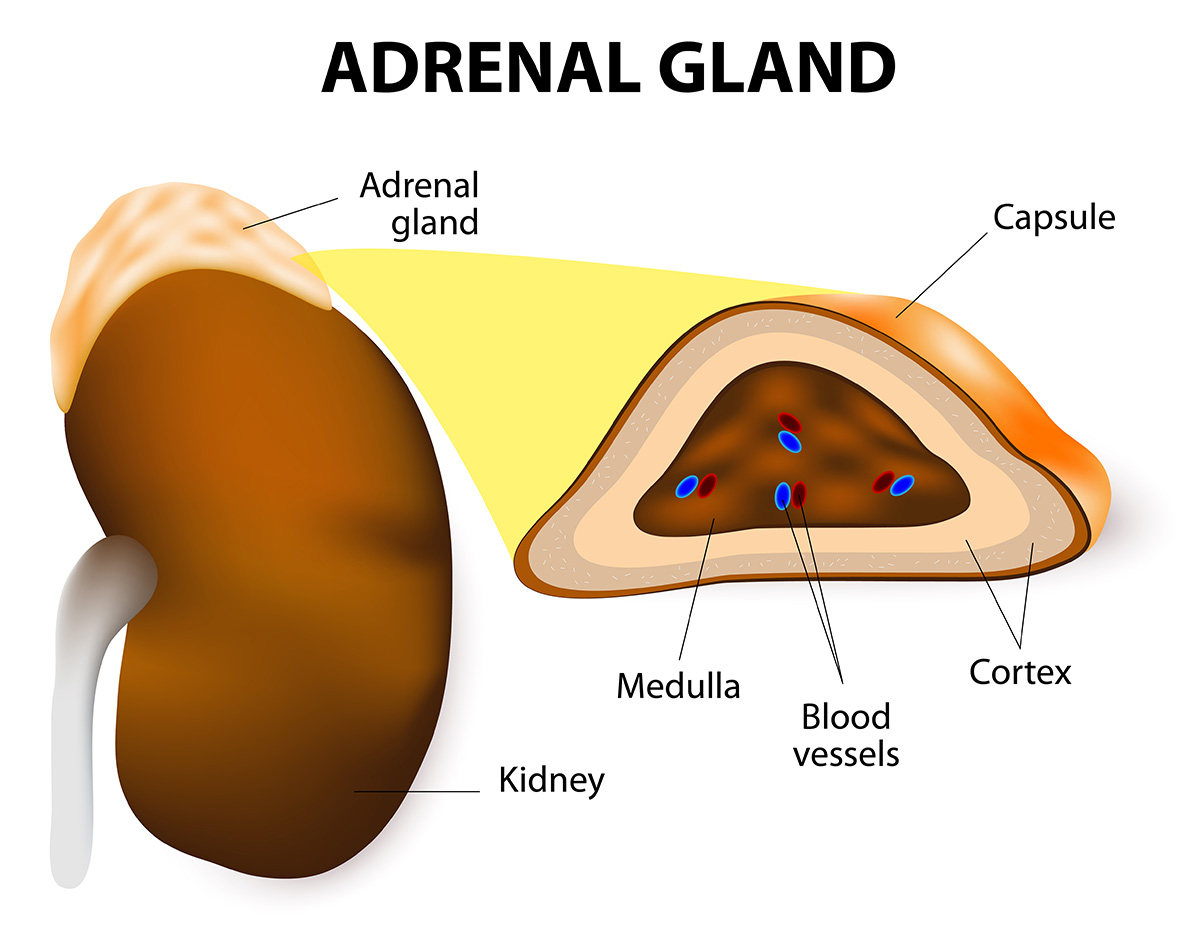
which organ is the adrenal gland associated too
Kidneys
what are catecholamines
a collection of hormones and neurotransmitters that are involved in regulating the body’s fight or flight response
epinephrine
norepinephrine
dopamine
where are catecholamines produced
adrenal medulla and the inner part of the adrenal glands
How do catecholamines function in maintaining homeostasis with respect to blood sugar?
They increase glucose availability to meet immediate energy demands,
stimulate the liver to produce and release glucose through glycogenolysis and gluconeogenesis
How do catecholamines compare to insulin?
they have opposite effects
how does epinephrine effect blood pressure
Increases BP
Epinephrine causes vasoconstriction (narrowing) of some blood vessels, increasing overall blood pressure.
allowing for more rapid oxygen and nutrient delivery to vital organs
how does epinephrine effect heartbeat
Increases
Stimulates the SA node and heart muscle, increasing both rate and strength of contractions.
This raises cardiac output, sending more blood (and oxygen) to active tissues.
how does epiephrine effect the rate of conversion of glycogen to glucose
Increases
Stimulates glycogenolysis in the liver and muscles
provides quick energy source (ATP) for muscles and the brain.
how does epinephrine effect the rate of oxygen consumption by cells
Increases
to meet the sudden energy demand the cells will need oxygen
how does epinephrine effect the rate of blood supply to skeletal and heart muscle
Increases (vasodilation)
Blood vessels in skeletal and cardiac muscles dilate, ensuring more oxygen and glucose are delivered where energy demand is highest.
how does epinephrine effect the rate of blood supply to skin, digestive tract, and kidneys
Decreases (vasoconstriction)
Blood is redirected away from non-essential organs during emergencies to conserve energy and supply vital organs (muscles, heart, brain).
This is why skin may appear pale and digestion slows under stress.
how does epiephrine effect peristalsis of the intestine
Decreases (inhibited)
Smooth muscle contractions in the digestive tract slow down or stop, conserving energy for critical systems like the heart and muscles.
What are the two primary types of corticosteroids?
glucocorticoids
mineralocorticoids
What is the primary effect of glucocorticoids, such as cortisol?
increase blood glucose levels and mobilize energy reserves to help the body cope with long-term stress.
how do the effects of glucocorticoids compare to that of insulin
they have opposite effects
What is the primary effect of mineralocorticoids like aldosterone?
they increase Na⁺ reabsorption and K⁺ secretion in kidneys
Results in an increase in water retention, blood volume, and blood pressure
Name the three glands that produce steroid hormones.
Adrenal cortex
Gonads
Placenta
Hormones of the adrenal cortex
Glucocorticoids
Cortisol
Mineralocorticoids
Aldosterone
Androgens
DHEA
Androstenedione
Compare and contrast the functions of the hormones FSH and LH in the human male
FSH Males
stimulate Sertoli cells, located within the seminiferous tubules, to nourish developing sperm
LH Males
Stimulates Leydig cells to produce testosterone, which supports sperm production and secondary sexual characteristics.
Compare and contrast the functions of the hormones FSH and LH in the human female
FSH females
Stimulates growth and maturation of ovarian follicles
Promotes estrogen secretion from the growing follicle
LH females
Triggers ovulation (release of the egg from the mature follicle).
Stimulates formation of the corpus luteum, which secretes progesterone and estrogen to maintain the uterine lining.
How are testosterone levels regulated in the human male.
through negative feedback
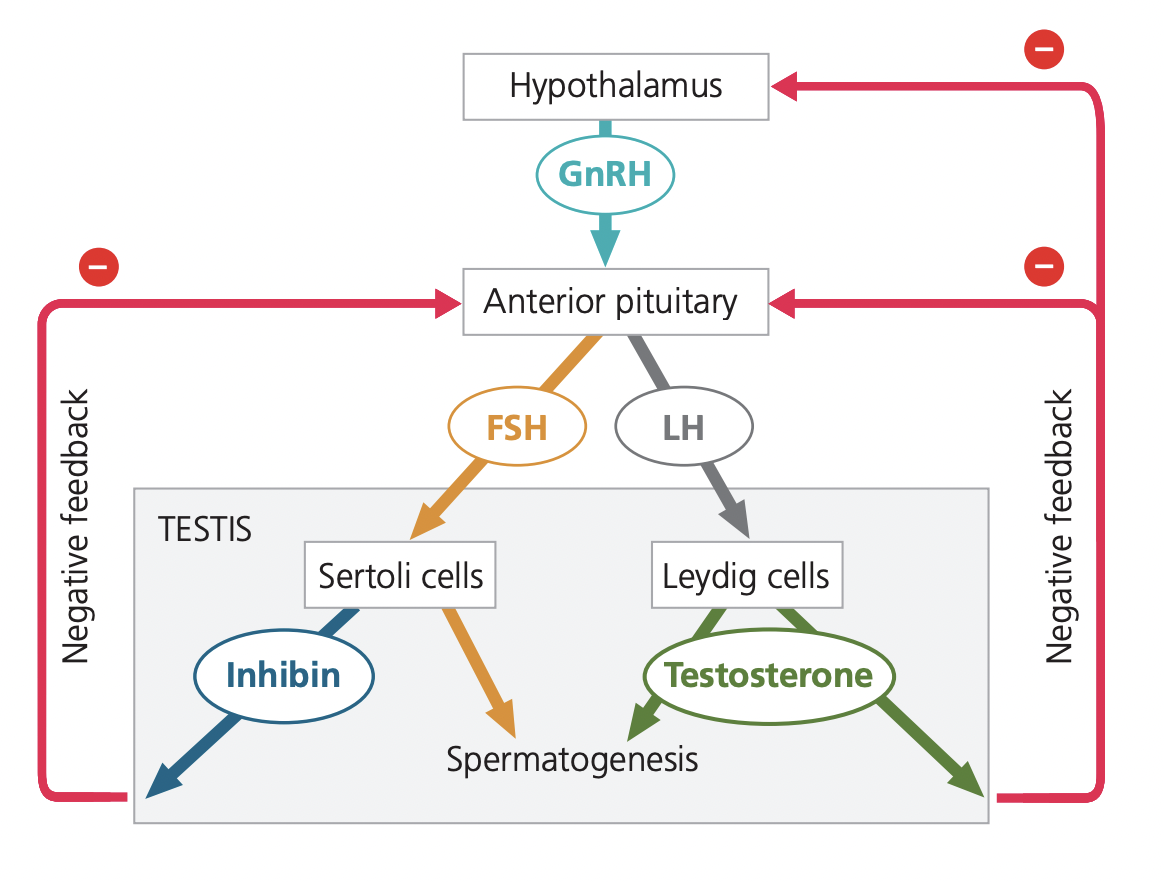
What would be the effect on the hormonal system if a male takes anabolic steroids, which are testosterone analogs?
Taking anabolic steroids shuts down the body’s own testosterone production through negative feedback on the hypothalamus and pituitary, leading to reproductive and hormonal imbalances.
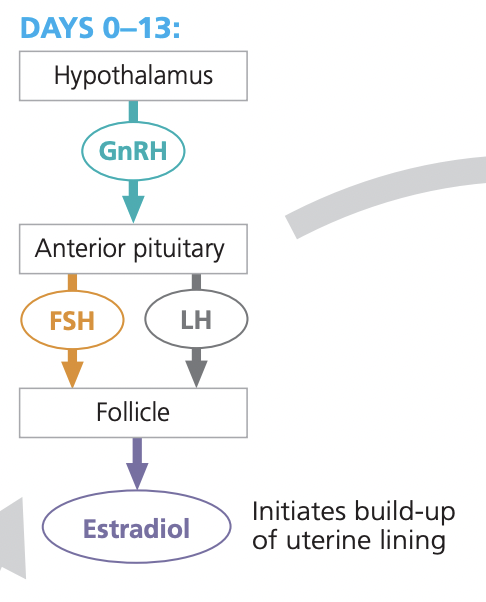
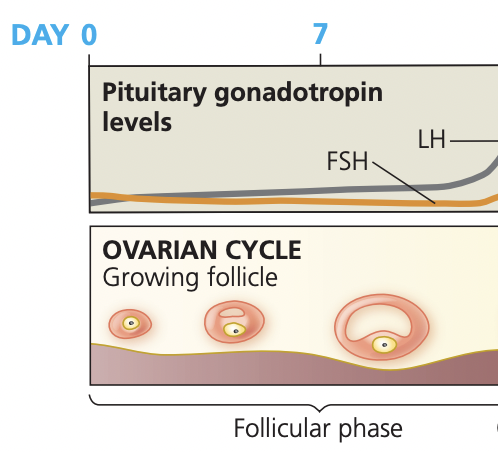
Ovarian cycle in females
Follicular phase
Ovulation
Luteal phase
Follicular phase
Days
Main Hormones (increase or decrease)
Ovarian Events
Uterine Effects
1–14 days
hypothalamus: secreates GnRH → stimulates the anterior pituitary to release FSH and LH
from this estradiol production is stimulated
FSH promotes the growth and maturation of several ovarian follicles.
The granulosa cells of these follicles secrete estriol as they grow.
Estriol stimulates endometrial thickening (proliferative phase of the uterine cycle).
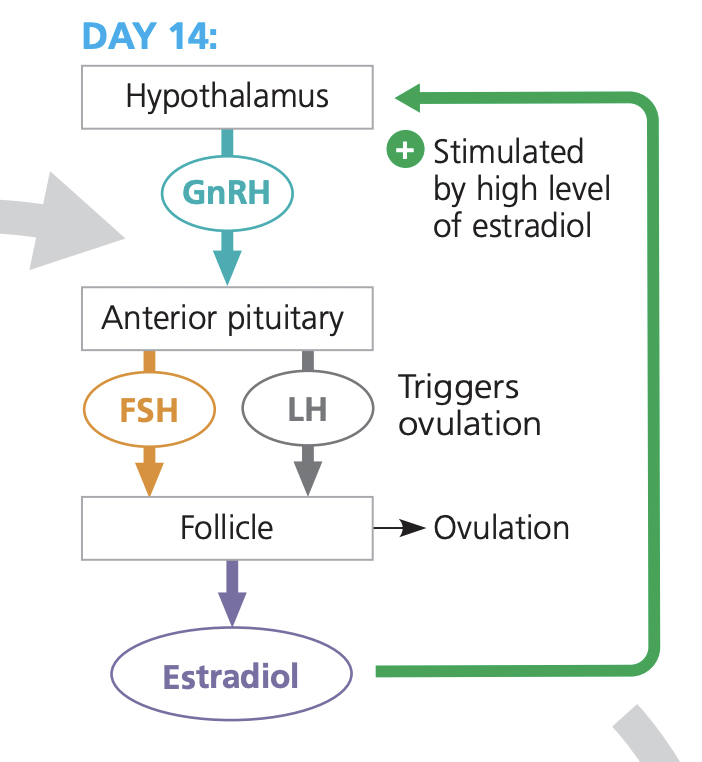
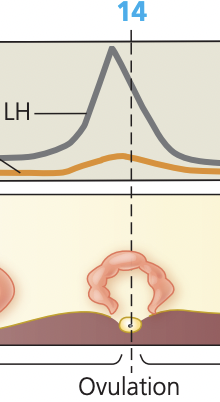
Ovulation phase
Days
Main Hormones (increase or decrease)
Ovarian Events
Uterine Effects
~14
LH surge, estriol creates a positive feedback loop with the hypothalamus
The LH surge triggers the mature follicle to rupture, releasing the egg (ovum) from the ovary into the fallopian tube. (ovulation)
The endometrium continues to thicken in case of implantation
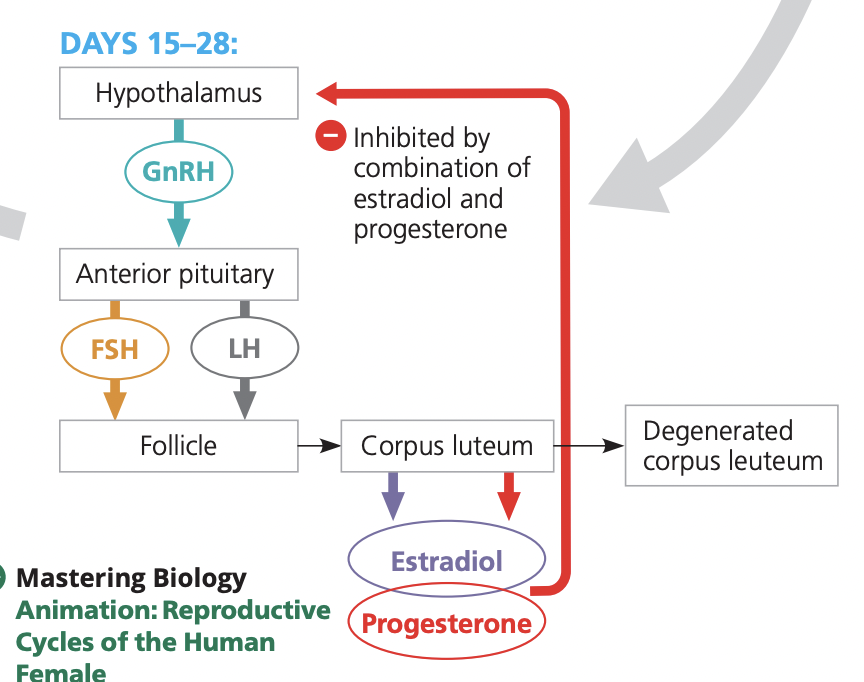
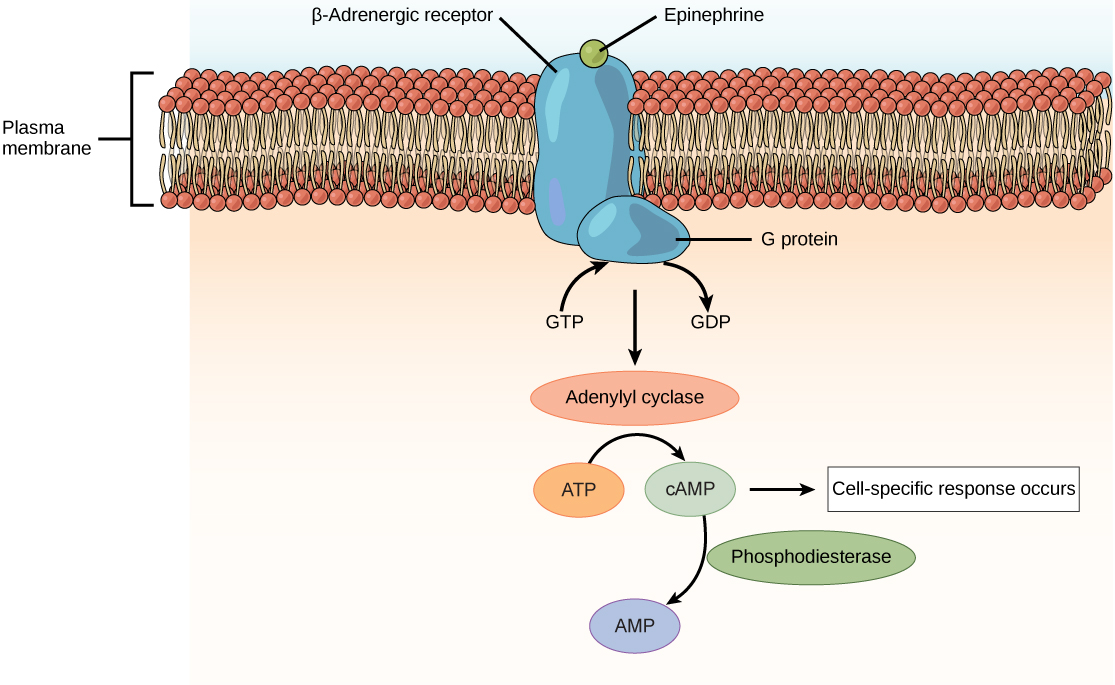
Luteal phase
Days
Main Hormones (increase or decrease)
Ovarian Events
Uterine Effects
15–28
↑ Progesterone, ↑ Estrodiol
The corpus luteum forms and secretes high levels of progesterone and some estradiol
progesterone maintains and further develops the endometrial membrane
Exerts negative feedback on the hypothalamus and anterior pituitary, suppressing GnRH, LH, and FSH secretion.
Endometrium maintained; if no fertilization → menstruation