muscarinic antagonists
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
54 Terms
identify where muscarinic receptors are found
1. modulatory/auto receptors= postganglionic cell body and terminal on BOTH para and symp neurons
2. effector cells: parasymp (glands/smooth muscle) and symp (sweat glands)
3. vascular endothelial cells (but NOT innervated)

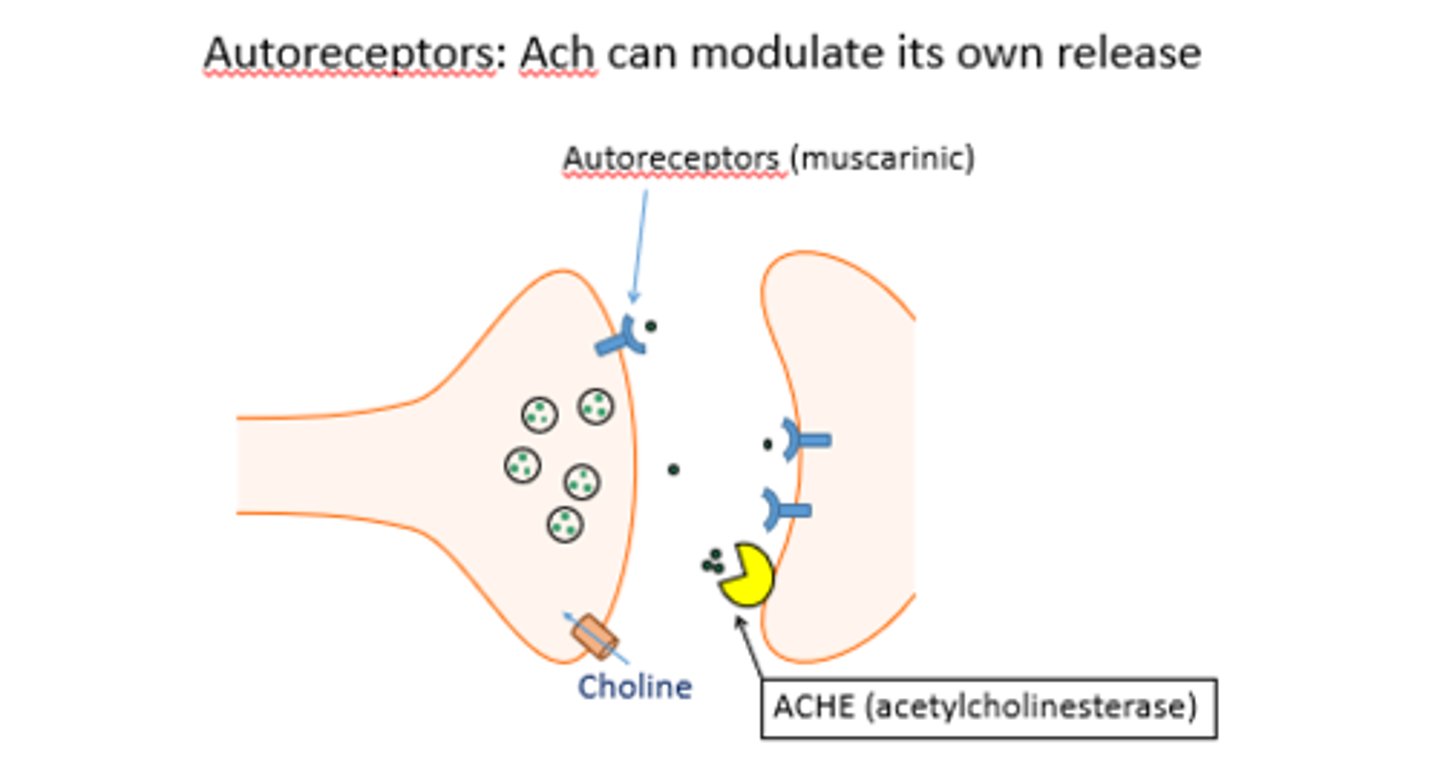
what are muscarinic auto receptors
receptors found on the pre-synaptic nerve terminal that modulate how much ACh is released from that same neuron
ex: if theres A LOT of ACh release, then it will land on both the effector receptor but also on the muscarinic receptor on that same neuron and have an inhibitory effect= less ACh release
which muscarinic receptors are found in the CNS? PNS?
CNS= M1-M5
PNS= M1-M3
what provides predominant tone in the heart?
vagus-> parasympathetic
(less tone in infants and elderly)
what is the prototypical muscarinic antagonist
Atropine (naturally occuring alkaloid)
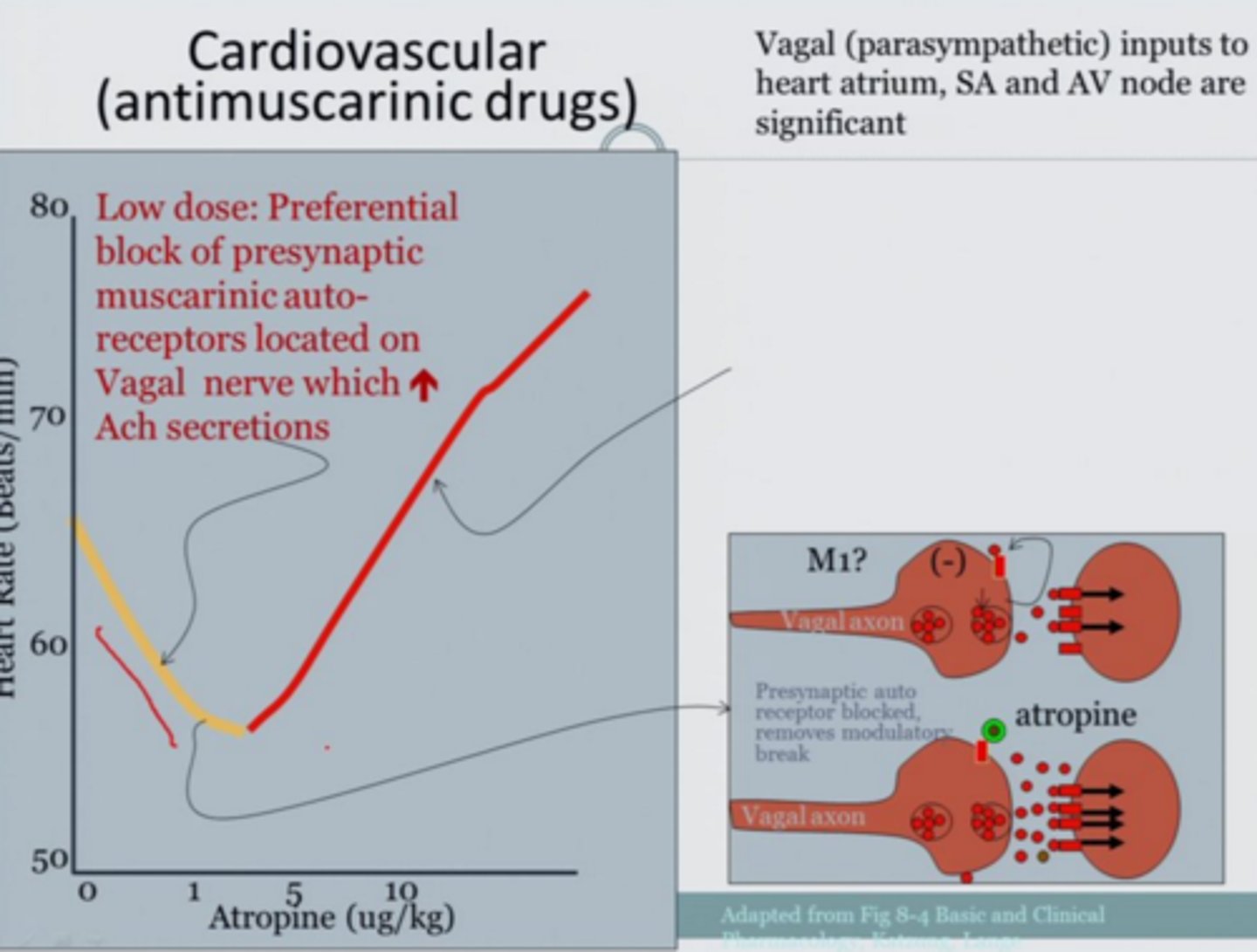
what are the effects of a low dose of atropine on the heart? high dose? why?
low dose= slight BRADYcardia. atropine targets autoreceptor causing more ACh stimulation of SA node
high dose= mild TACHYcardia. atropine targets receptor on SA node, blocking effect of ACh
t/f: as the dose of atropine increases, greater xerostomia is seen
true. dry mouth as a result of muscarinic antagonism
describe what happens to the pupil as more atropine is given
greater mydriasis (dilation)
which physiological responses are seen in smaller doses of atropine? greater doses?
small doses= heart (brady-> tachy switch at high), dry mouth, less sweating
large dose=tachy, hot and dry skin, very blurred vision, urination difficulty, GI reduction
describe the mech as to how muscarinic antagonists can lead to less sweating and hot/dry skin
1. blocks muscarinic auto receptors on symp ganglia
2. blocks muscarinic receptors on sweat glands
3. blocks NONinnervated musc receptors on vasc endothelial muscles (less vasodilation= less heat released)
describe how muscarinic receptors lead to vasodilation under normal conditions
-ACh binds to M3 receptors on NONinnervated vascular endothelial cells= activates a signaling pathway that leads to the production of nitric oxide.
-NO diffuses to the underlying smooth muscle cells= vasodilation
t/f: muscarinic antagonists are usually smaller than muscarinic agonists
false. musc antagonists are bigger/bulkier
(think of a big bully antagonizing the agonists)
would a muscarinic antagonist be more effective in blocking bethanechol or endogenous acetylcholine? why?
bethanechol bc it is exogenous agonist.
ACh is released directly at the synapse= high local concentrations in a very short time (more challenging for antagonists to outcompete it)
-exogenous agonists like bethanechol are administered systemically and diffuse to the receptors rather than being released in a focused, high-concentration burst
t/f: an AChE inhibitor may be used for atropine poisoning
true. an example is physostigmine.
AChE inhibitor would stop ACh degradation, and help ACh outcompete the atropine
describe atropine selectivity
non-selective: targets all M1-M5 receptors
- BUT differs in which tissues it reaches
which stimuli can cause reflex vagal activity that triggers bradycardia? how does atropine affect this?
irritant vapors (ex:smoke), pressure on eyeball, and peritoneal stimulation can all lead to a vagal reflex that lowers bp
atropine would block vagal tone and stop the heart from slowing
t/f: at low doses, atropine affects pre- more than post-synaptic receptors due to tissue differences
true (not bc of receptor selectivity)
why does atropine have almost no effect on bp in therapeutic dose ranges
- blood vessels are mainly controlled by sympathetic stimulation for vasodilation and vasoconstriction
- there are NONinnervated M3 receptors on vasc endothelial cells that cause vasodilation via NO but they rely on circulating ACh so atropine doesnt really have an effect
(most of atropine's cardio effect is via heart SA node)
effect of atropine on respiratory system
- directly blocks bronchospasm/constriction and mucus secretion via ACh antagonism
indirect effect of atropine on histamine/bradykinin/eicosanoid vasodilation effects
indirectly blocks the effects of histamine, bradykinin, and eicosanoids (even if histamine, bradykinin, or eicosanoids cause vasodilation, the body can't respond with reflex vagal-induced bradycardia because atropine blocks M receptor on SA)
describe why atropine may be used to treat allergic rhinitis and NAR. side effects?
- blocks resp effects of ACh= dries mucus membranes and inhibits secretions from nose/mouth/pharynx
= may form mucus plugs, side effects from systemic distribution
examples of quaternary ammonium antimuscarinic agents:
used for?
CNS effect?
-ipratropium and tiotropium
-block bronchoconstriction
-local effect bc inhaled and do NOT cross BBB= less CNS effects
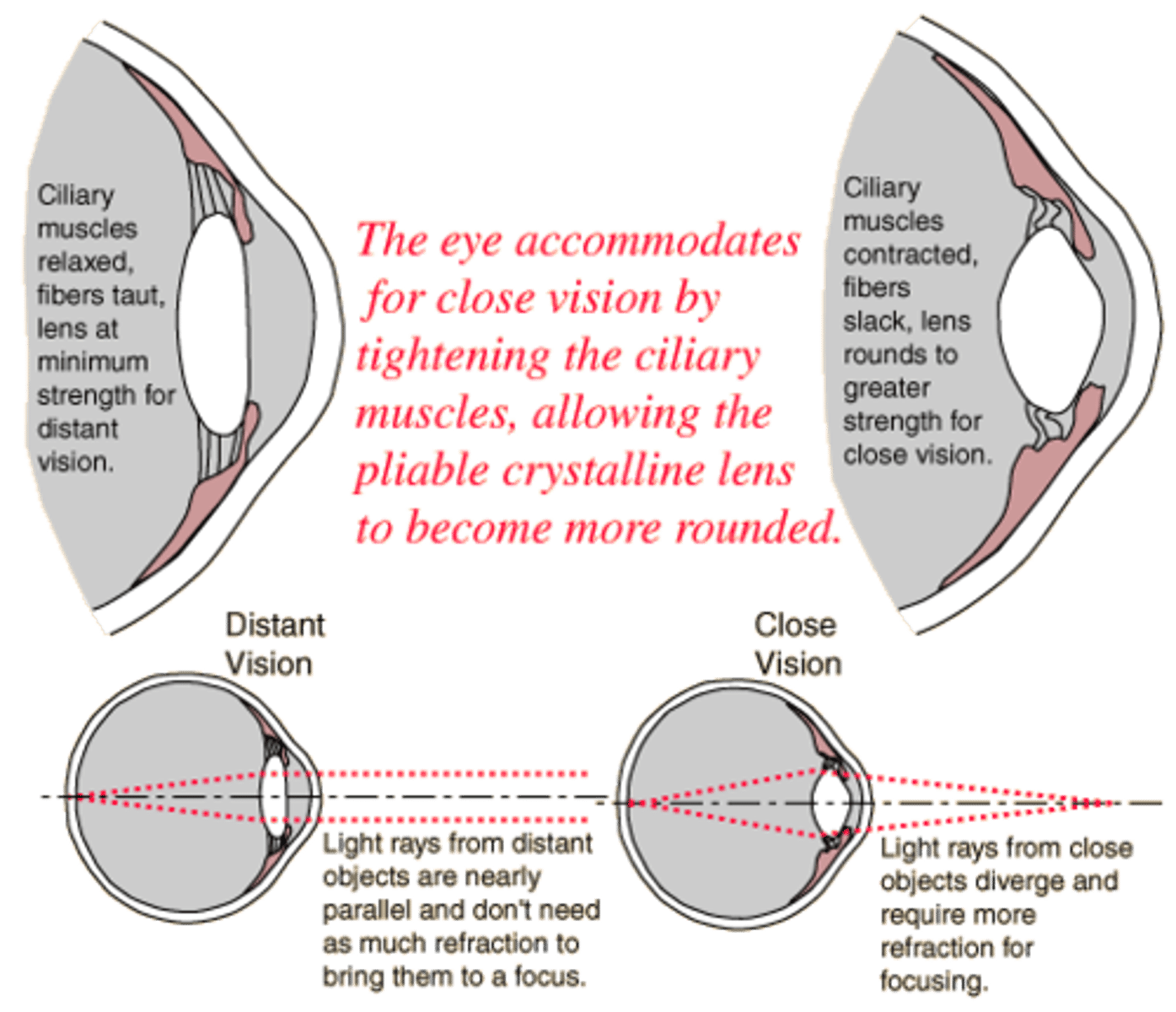
effects of atropine on the eye
- block M receptor on circular muscle= mydriasis (dilation)
=pupil reflex to light is blocked
- blocks M receptor on ciliary muscle= lens cannot accommodate when object is near= blurry
atropine cause pupillary ___________ and an object that is ____(near/close?)___ would appear blurry
dilation; near
compare scopolamine vs atropine potency on the eye
scopolamine is more potent (also crosses BBB easier than atropine)
explain why atropine does not completely inhibit GI responses
GI is not only controlled by parasymp stimulation, but by enteric nervous system and GRP(gastrin) too
cycloplegia
paralysis of the ciliary muscle (lens cannot accommodate)
- side effect of muscarinic antagonists
t/f: scopolamine has more of an effect on the CNS than atropine due to BBB penetration
true
effect of toxic doses of atropine on the CNS
CNS excitation, restlessness, irritability, disorientation, delirium
effect of therapeutic doses of scopolamine on CNS
CNS depression, drowsiness, fatigue, amnesia, reduced REM sleep
(opposite of atropine which excites CNS)
how do ipratropium and tiotropium affect the respiratory system? what is different between them?
- cause bronchodilation without lessening mucus clearance (unlike atropine); less effective against 5HT and luekotrienes
- ipratropium is non selective while tiotropium has higher affinity for postsynaptic M1 and M3
t/f: tiotropium is non selective while ipratropium has higher affinity for postsynaptic M1 and M3
false. ipratropium is non selective while tiotropium has higher affinity for postsynaptic M1 and M3
how can muscarinic antagonists worsen closed angle glaucoma
-Blocking ciliary muscle contraction, which impairs aqueous humor outflow and increases intraocular pressure.
-inducing mydriasis, which narrows the anterior chamber angle, exacerbating the blockage of aqueous humor drainage
(but generally safer in open angle glaucoma)

oxybutynin, tolterodine/fesoterodine, solifenacin/darifenacin, and trospium chloride are all used for
musc antagonists used for overactive bladder
- relax detrusor, decrease pressure in bladder, increase bladder capacity
compare oxybutynin to tolterodine selectivity
oxybutynin= non-selective (m1-m3)
- causes sedation via M1 stimulation
- blocks spasms by blocking Ca channels
tolterodine= M2 and M3 SELECTIVE
- NO sedation
the blockage of which muscarinic receptor may cause sedation
M1 in CNS (ex: oxybutynin)
cyclopentolate
Muscarinic antagonist
mydriasis + loss of accommodation for close vision
tropicamide
muscarinic antagonist
mydriasis + loss of accommodation for close vision
presynaptic muscarinic receptors can be found in
a. postganglionic parasymp neurons
b. postganglionic symp neurons
c. all of the above
c. all of the above
when _________ binds to presynaptic muscarinic receptors it ______ Ach release
a. atropine, inhibits
b. bethanechol, stimulates
c. ACh, inhibits
d. methacholine, stimulates
e. two of the above are true
c. ACh, inhibits
(autoreceptor function)
a high dose of atropine is most likely to cause
a. bradycardia
b. loss of accommodation/ blurring
c. micturition difficulty
d. dry hot skin
e. two of the above
f. three of the above
f. three of the above
[a= incorrect. would be tachycardia
b= true
c= true
d= true]
t/f: musc antagonists are less effective at blocking exogenous agonist than parasympathetic nerve stimulation
false. more likely to block exogenous than endogenous source
t/f: atropine can block the slowing of the heart caused by pressure on the eyeball
true. blocks vagal reflex
t/f: atropine can indirectly block some of the effects of bradykinin by limiting the effects of increased vagal tone
true
t/f: a therapeutic dose of atropine would be expected to increase vascular resistance and BP
false. atropine is a muscarinic antagonist. arterioles are not parasympathetically innervated, so blocking the M3 receptors would not affect arterioles
the best agent to use to treat motion sickness
a. atropine
b. scopolamine
c. ipratropium
d. titotropium
b. scopolamine
the agent least likely to cross the BBB
a. atropine
b. scopolamine
c. ipratropium
c. ipratropium
it is charged, wont cross BBB
the best therapeutic agent for treating COPD would be
a. scopolamine
b. atropine
c. tiotropium
d. methacholine
c. tiotropium
t/f: the degree of bronchodilation elicited by ipratropium is dependant on basal vagal tone
true. vagal tone causes bronchoconstriction, so blocking it causes relaxation
t/f: the degree of bronchodilation elicited by a beta-2 agonist is dependant on basal sympathetic tone
false
parietal cell acid secretion is stimulated by
a. ACh
b. histamine
c. gastrin
d. 2 of the above
e. all of the above
e
atropine is not considered to be an effective treatment for peptic ulcer bc
a. does not block effects of gastrin releasing peptide
b. stimulates H2 receptors
c. has many side effects at large doses
d. 2 of the above
e. all of the above
d. 2 of the above (a and c)
t/f: muscarinic antagonists are more likely to aggravate open-angle glaucoma than angle-closure glaucoma
false
t/f: muscarinic receptors stimulate histamine release. since atropine blocks this, no HCl will be produced in parietal cells.
false. it does block histamine release but parietal cell secretion is not only dependant on histamine, but on ACh and gastrin as well (endocrine system plays a role)