Ella Kulman Cardiovascular
1/284
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
285 Terms
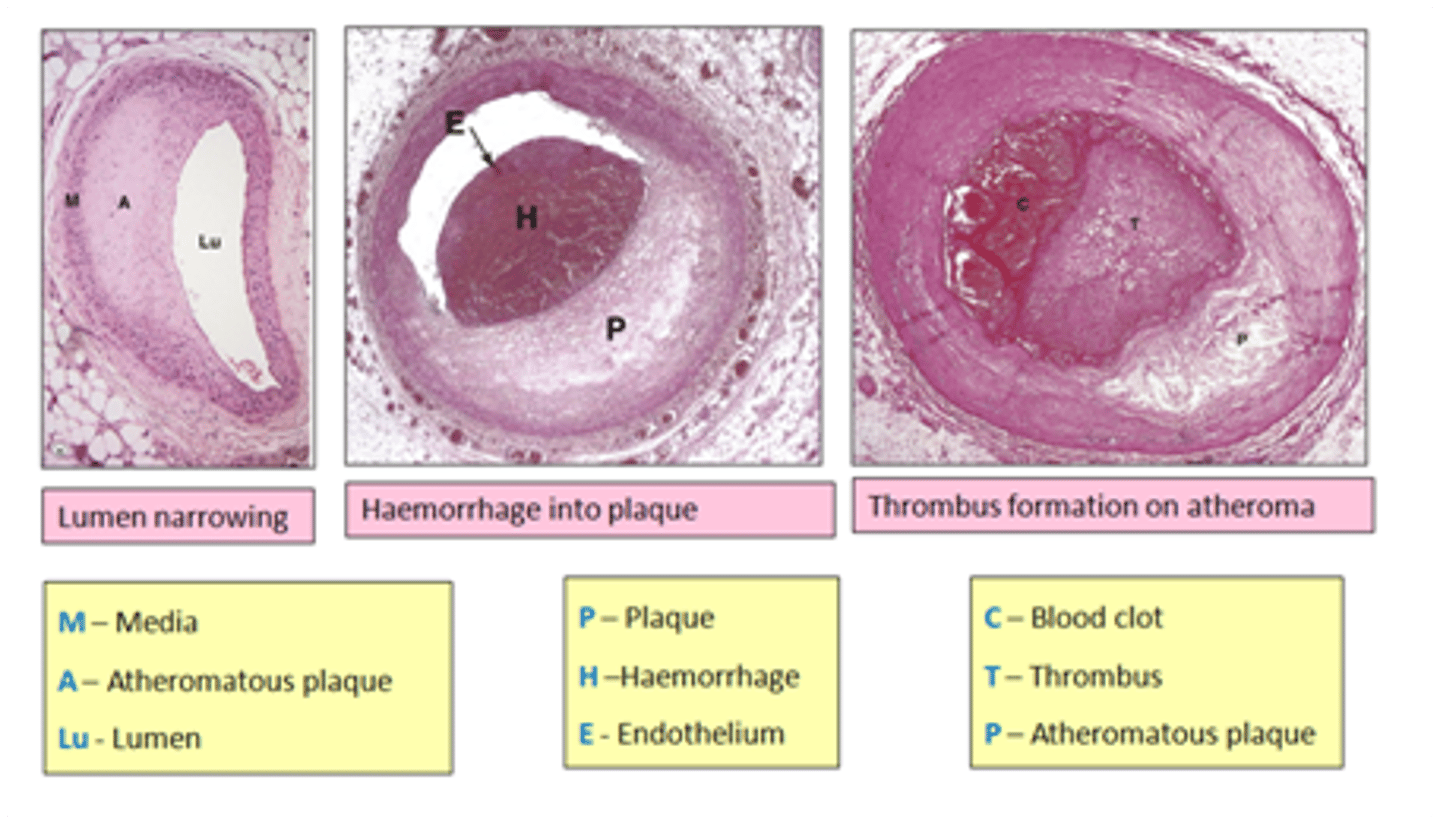
3 things an atherosclerotic plaque can cause
1. Heart attack
2. Stroke
3. Gangrene
Give up to 7 risk factors of atherosclerosis
1. Family history
2. Increasing age
3. Smoking
4. High levels of LDL's
5. Obesity
6. Diabetes
7. Hypertension
In which arteries are you most likely to find an atheromatous plaque?
peripheral + coronary arteries
which histological layer of the artery may be thinned by an atheromatous plaque?
media
what is the precursor for atherosclerosis?
fatty streak
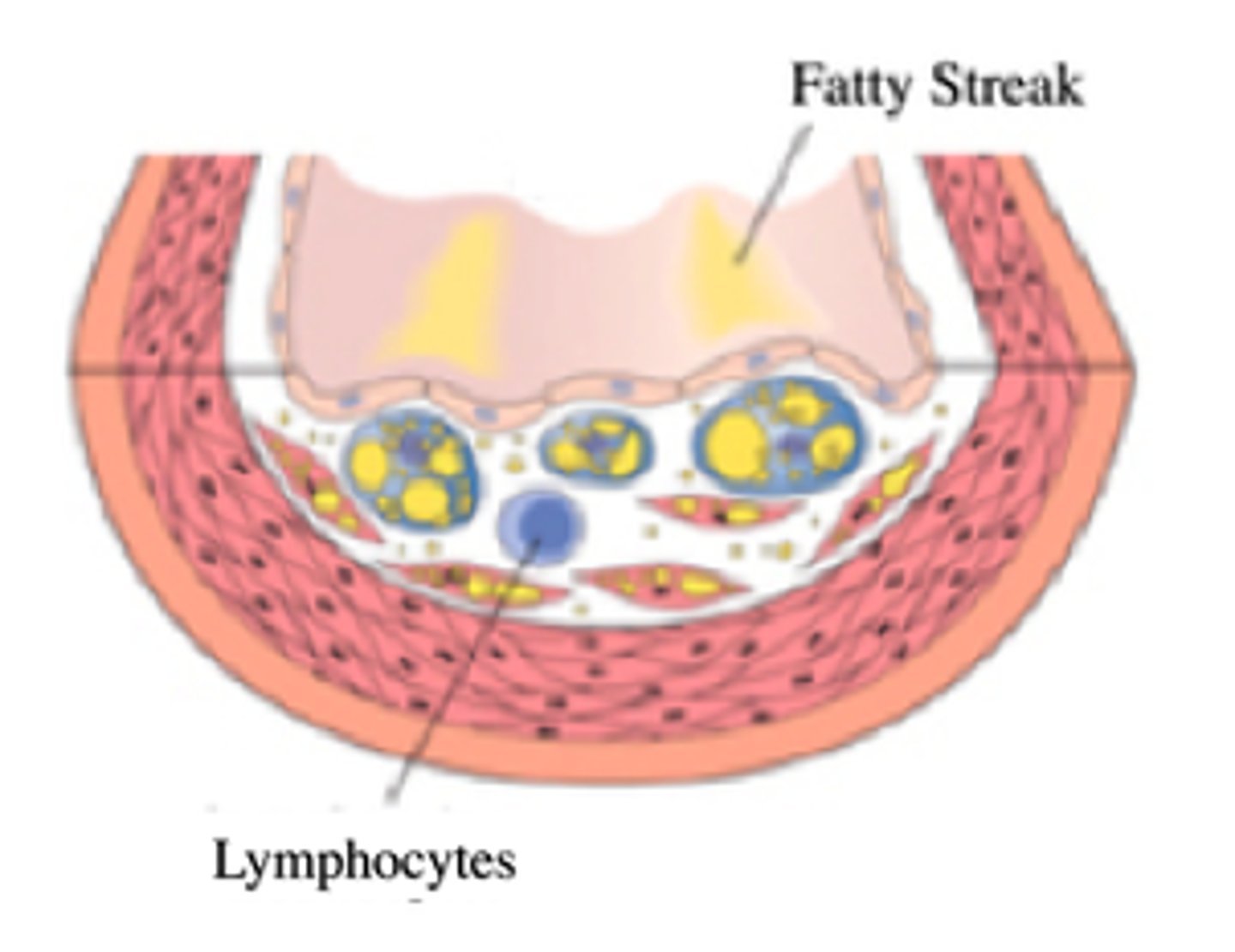
What can cause chemoattractant release?
a stimulus such as endothelial call injury
what are the functions of chemoattractants?
chemoattractants signal to leucocytes
leukocytes then accumulate and migrate into vessel walls → cytokine release → inflammation
Describe in 5 steps the progression of atherosclerosis
1. Fatty streaks
2. Intermediate lesions
3. Fibrous plaque
4. Plaque rupture
5. Plaque erosion
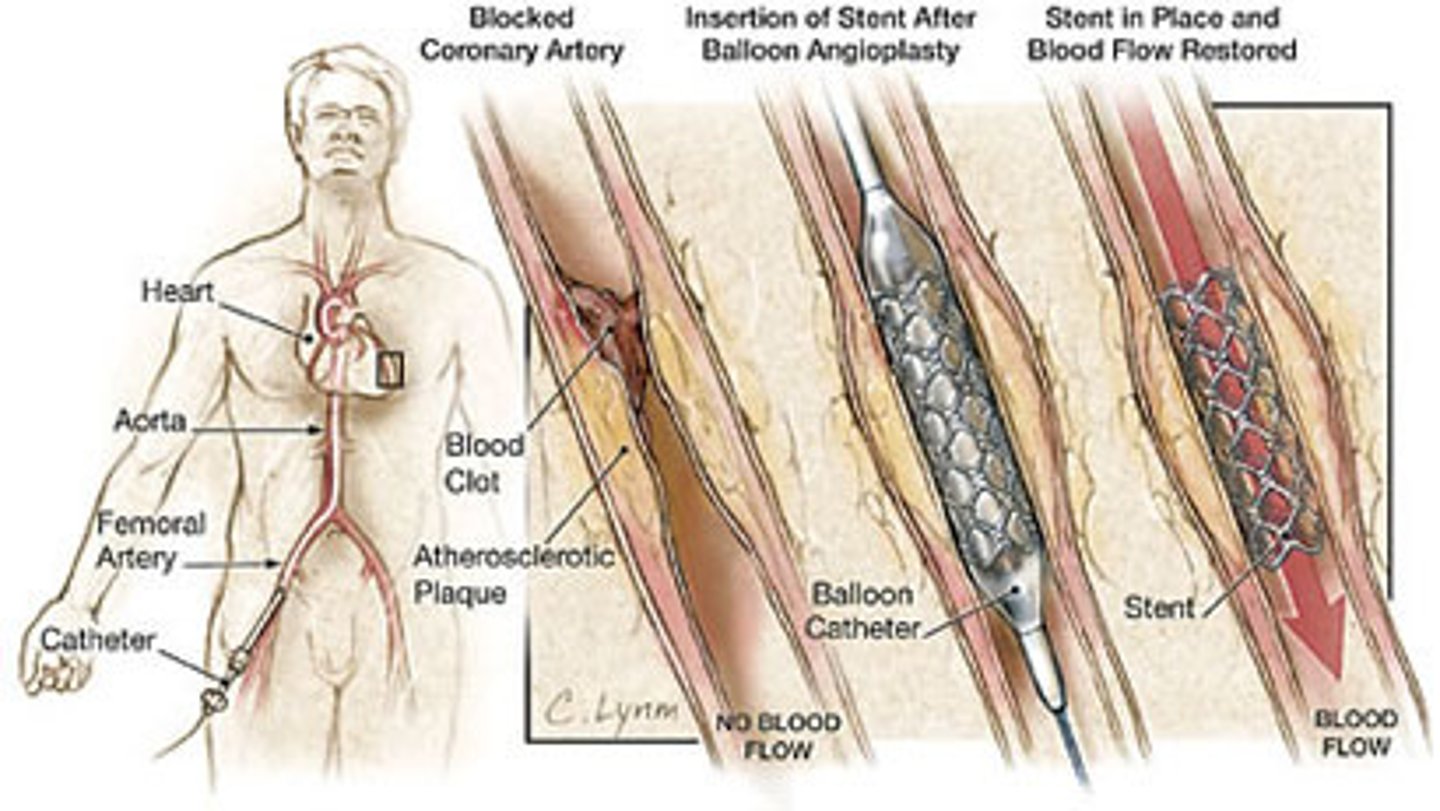
What is the treatment for atherosclerosis?
percutaneous coronary intervention (PCI)
*an umbrella term
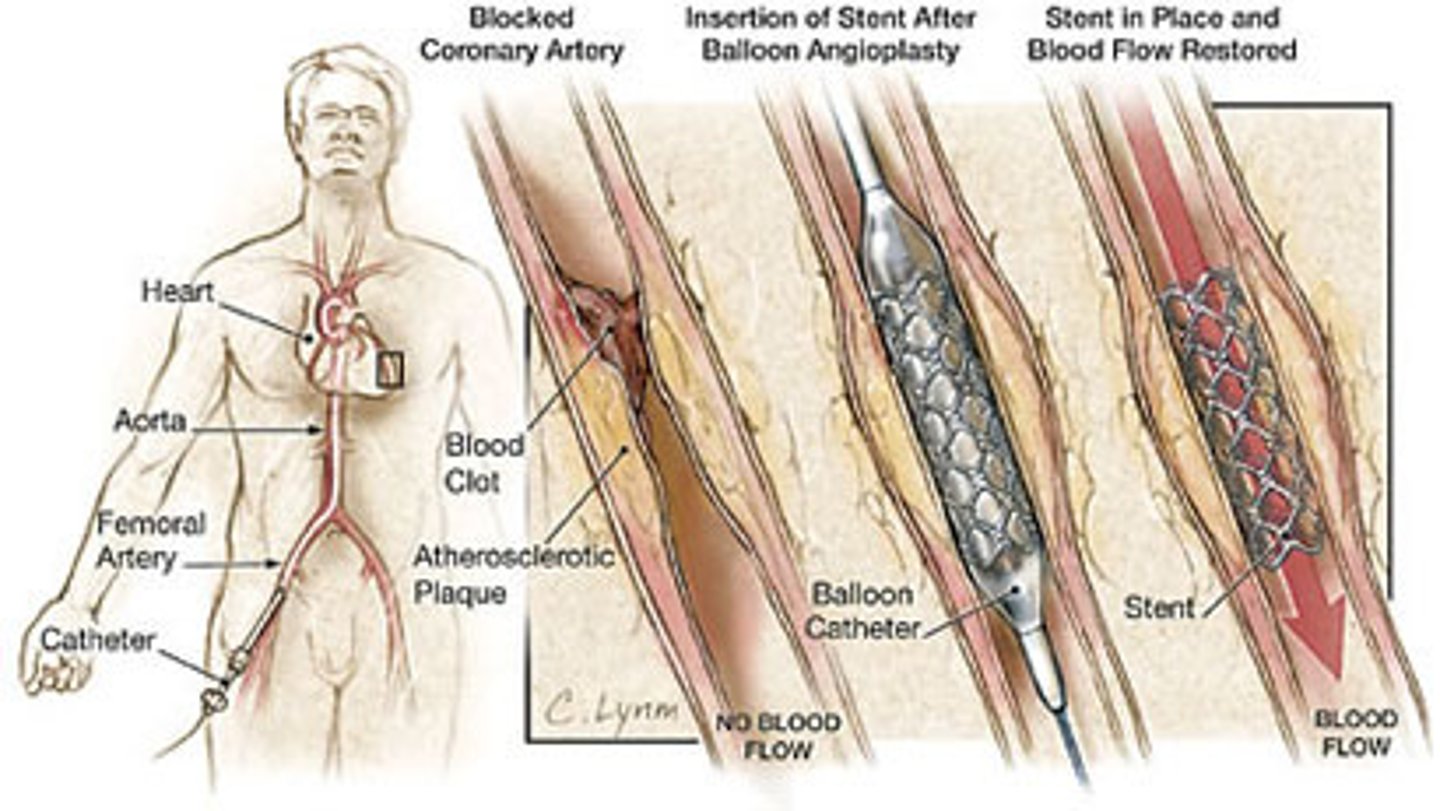
What is the major limitation of PCI?
restenosis
How can restenosis be avoided following PCI?
drug eluting stents: anti-proliferative and drugs that inhibit healing
Describe atherogenesis
the development of an atherosclerotic plaque
Define angina
a type of IHD, it's a symptom of O2 supply/demand mismatch to the heart experienced on exertion
What is the most common cause of angina?
narrowing of the coronary arteries due to atherosclerosis
Give 5 possible causes of angina
1. Narrowed coronary artery = impairment of blood flow e.g. atherosclerosis
2. Increased distal resistance= LV hypertrophy
3. Reduced O2 carrying capacity e.g. anaemia
4. Coronary artery spasm
5. Thrombosis
Give 5 modifiable risk factors for angina
1. Smoking
2. Diabetes
3. High cholesterol (LDL)
4. Obesity/sedentary lifestyle
5. Hypertension
Give 3 non-modifiable risk factors for angina
1. Increasing age
2. Gender, male bias
3. Family history /genetics
Briefly describe the pathophysiology of angina that results from atherosclerosis
on exertion there is increased O2 demand, wrovary blood flow is obstructed by an atherosclerotic plaque → myocardial ischaemia → angina
Briefly describe the pathophysiology of angina that results from anaemia
On exertion there is increased O2 demand, in someone with anaemia there is reduced O2 transport → myocardial ischaemia → angina
Why are blood vessels unable to compensate for increased myocardial demand in someone with CV disease?
in CVD epicardial resistance is high, meaning microvascular resistance has to fall at rest to supply myocardial demand at rest. when this person exercises, the microvascular resistance can't drop anymore and flow can't increase to meet demand = angina
How is chest pain in angina often described?
Crushing chest pain - heavy and tight
patient will often make a fist shape to describe it
Give 5 signs/symptoms of angina
1. Crushing central chest pain
2. The pain is relieved at rest or using a GTN spray
3. The pain is provoked by physical activity
4. The pain might radiate to the arms, neck or jaw
5. Breathlessness
what investigations might you do in someone you suspect to have angina?
1. ECG - usually normal
2. Echocardiogram
3. CT angiography - has a high NPV and is good at excluding disease
4. Exercise tolerance test- induces ischaemia
5. Invasive angiogram - tells you FFR (pressure gradient across stenosis)
Primary prevention (2) of angina
1. Risk factor modification
2. Low dose aspirin
Secondary prevention (3) of angina
1. Risk factor modification
2. Pharmacological therapies for symptom relief and to reduce the risk of CV events
3. Interventional therapies e.g. PCI
Name 3 symptom relieving pharmacological therapies that might be used in someone with angina
1. Beta blockers
2. Nitrates e.g. GTN spray
3. Calcium channel blockers
Describe the action of beta blockers
They are beta 1 specific. They antagonise sympathetic activation and so are negatively chronotropic and ionotropic. Myocardial work is reduced and so is myocardial demand = symptom relief
Give 3 side effects of beta blockers
1. Bradycardia
2. Tiredness
3. Erectile dysfunction
4. Cold peripheries
when might beta blockers be contraindicated?
In someone who has asthma/is bradycardic
Describe the action of nitrates
e.g. GTN spray are venodilators
venodilators → reduced venous return → reduced pre-load → reduced myocardial work/demand
Describe the action of Ca2+ channel blockers
they are arterodilators → reduced BP → reduced afterload → reduced myocardial demand
Name 2 drugs that might be used in someone with angina or in someone at risk to improve prognosis
1. Aspirin
2. Statins
What are statins used for?
reduce the amount of LDL's in the blood
Name 2 types of revascularisation
1. PCI
2. CABG
Give 2 advantages and 1 disadvantage of PCI
1. Less invasive
2. Convenient and acceptable
3. High risk of restenosis
Give 1 advantage and 2 disadvantages of a CABG
1. Good prognosis after surgery
2. very invasive
3. Long recovery time
What are acute coronary syndromes? (ACS)
encompasses a spectrum of acute cardiac conditions including unstable angina, NSTEMI, STEMI
what is the most common cause of ACS?
rupture of an atherosclerotic plaque and subsequent arterial thrombosis
What are uncommon causes of ACS?
1. Coronary vasospasm
2. Drug abuse
3. Coronary artery dissection
Describe type 1 MI
Spontaneous MI with ischaemia due to plaque rupture
Describe type 2 MI
MI secondary to ischaemia due to increased O2 demand
Why do you see increased serum troponin in NSTEMI and STEMI
the occluding thrombus causes necrosis of calls and so myocardial damage. Troponin is a sensitive marker for cardiac muscle injury and so is significantly raised to reflect this
Give 3 signs of unstable angina
1. Cardiac chest pain at rest
2. Cardiac chest pain with crescendo patterns; pain becomes more frequent and easily provoked
3. No significant rise in troponin
Give 6 signs/symptoms of MI
1. Unremitting and usually severe central cardiac chest pain
2. Pain occurs at rest
3. Sweating
4. Breathlessness
5. Nausea/vomiting
6. 1/3 occur in bed at night
Give up to 7 potential complications of MI
1. Heart failure
2. Rupture of infarcted ventricle
3. Rupture of interventricular septum
4. Mitral regurgitation
5. Arrhythmias
6. Heart block
7. Pericarditis
What investigations would you do on someone you suspect has ACS?
1. ECG
2. Blood tests; look at serum troponin
3. Coronary angiography
4. Cardiac monitoring for arrhythmias
What might the ECG of someone with unstable angina show?
normal or T wave inversion/ST depression
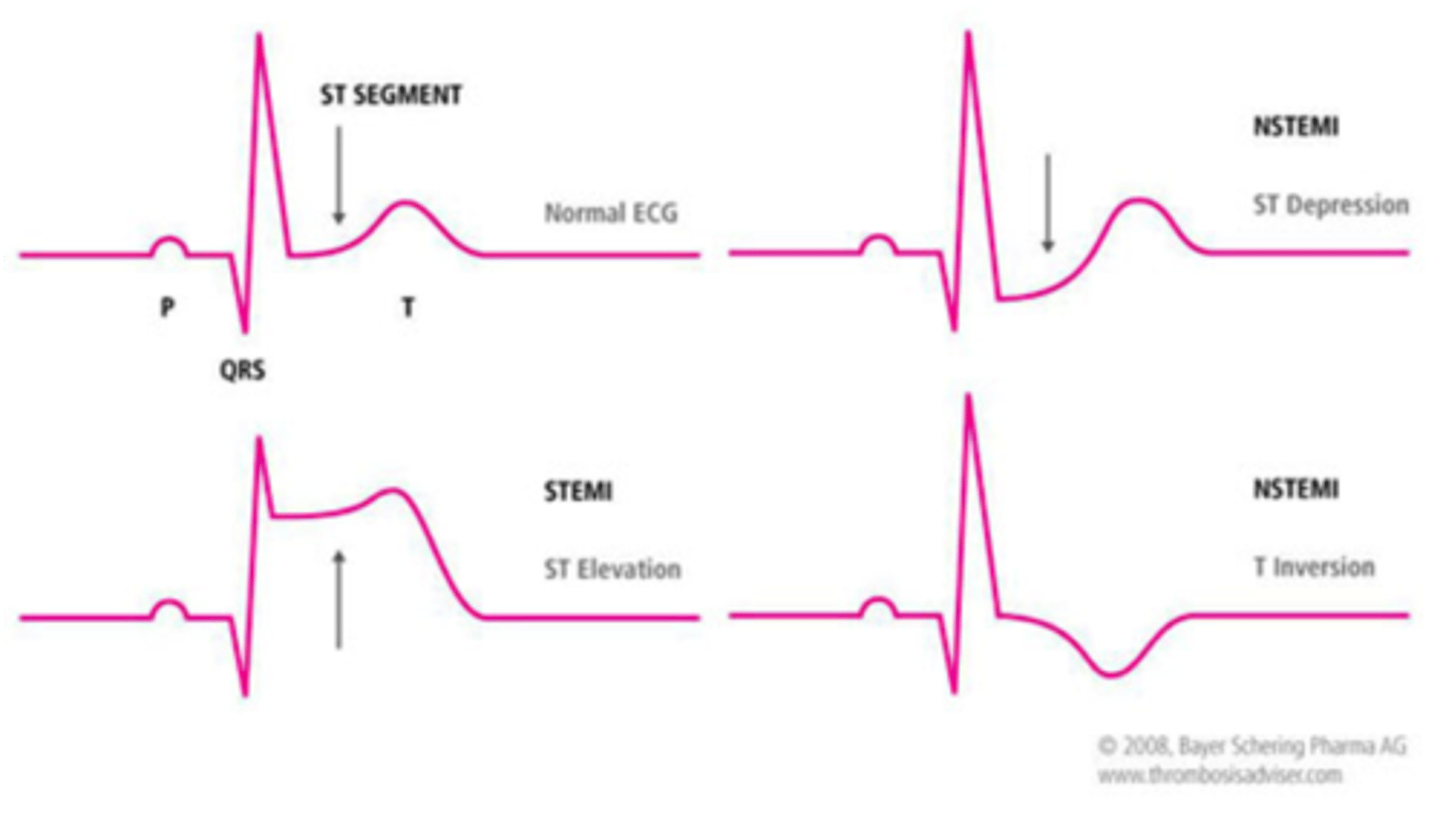
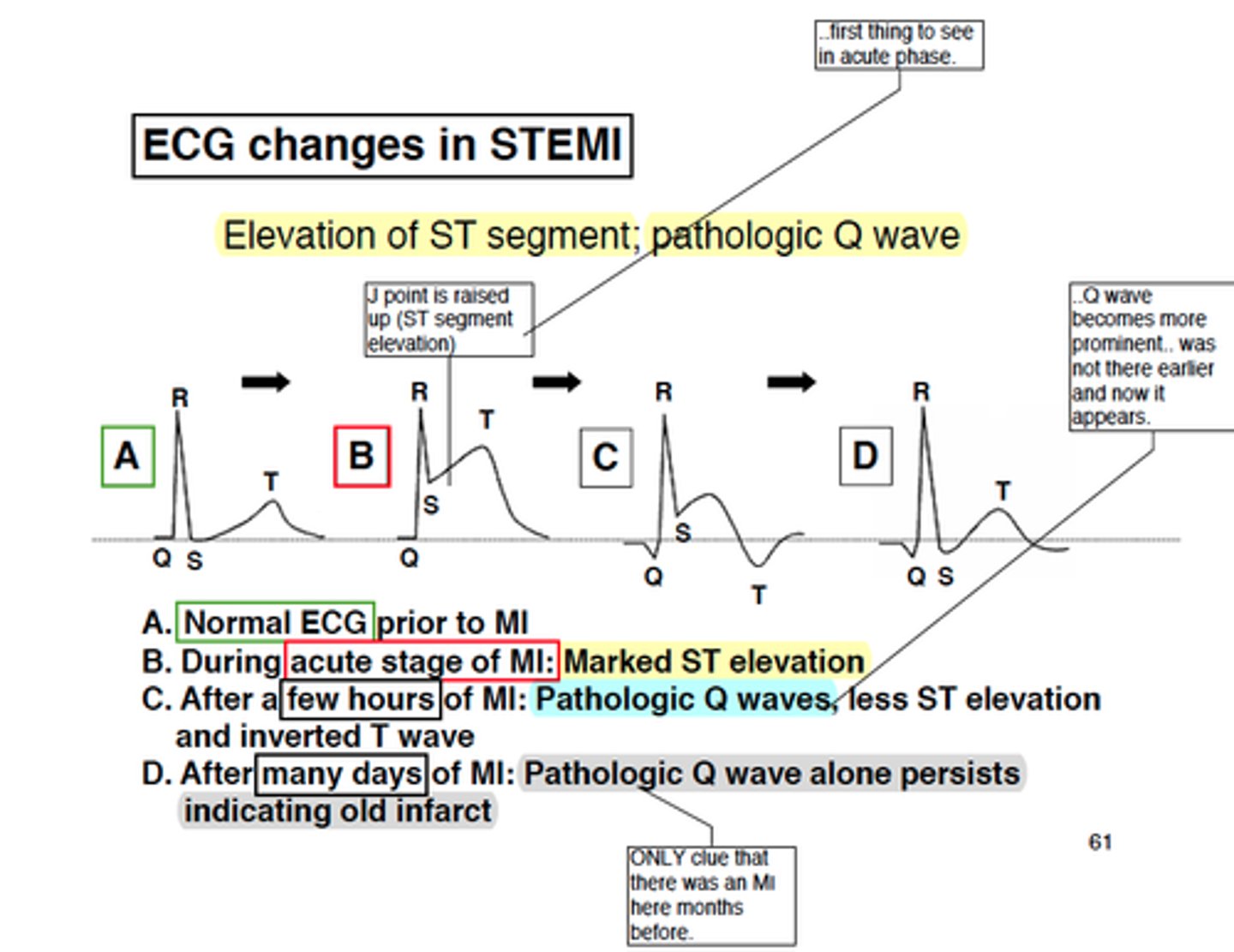
What might the ECG of someone with STEMI show?
ST elevation in the anterolateral leads. After a few hours, T waves invert and deep, broad, pathological Q waves develop
what would serum troponin levels be like in someone with unstable angina?
normal
what would serum troponin levels be like in someone with NSTEMI/STEMI?
significantly raised
Why might someone with mitral stenosis be breathless? (use Sterling's law)
mitral stenosis means ventricles don't fill completely → reduced EDV → reduced ESV → reduced CO and so breathlessness
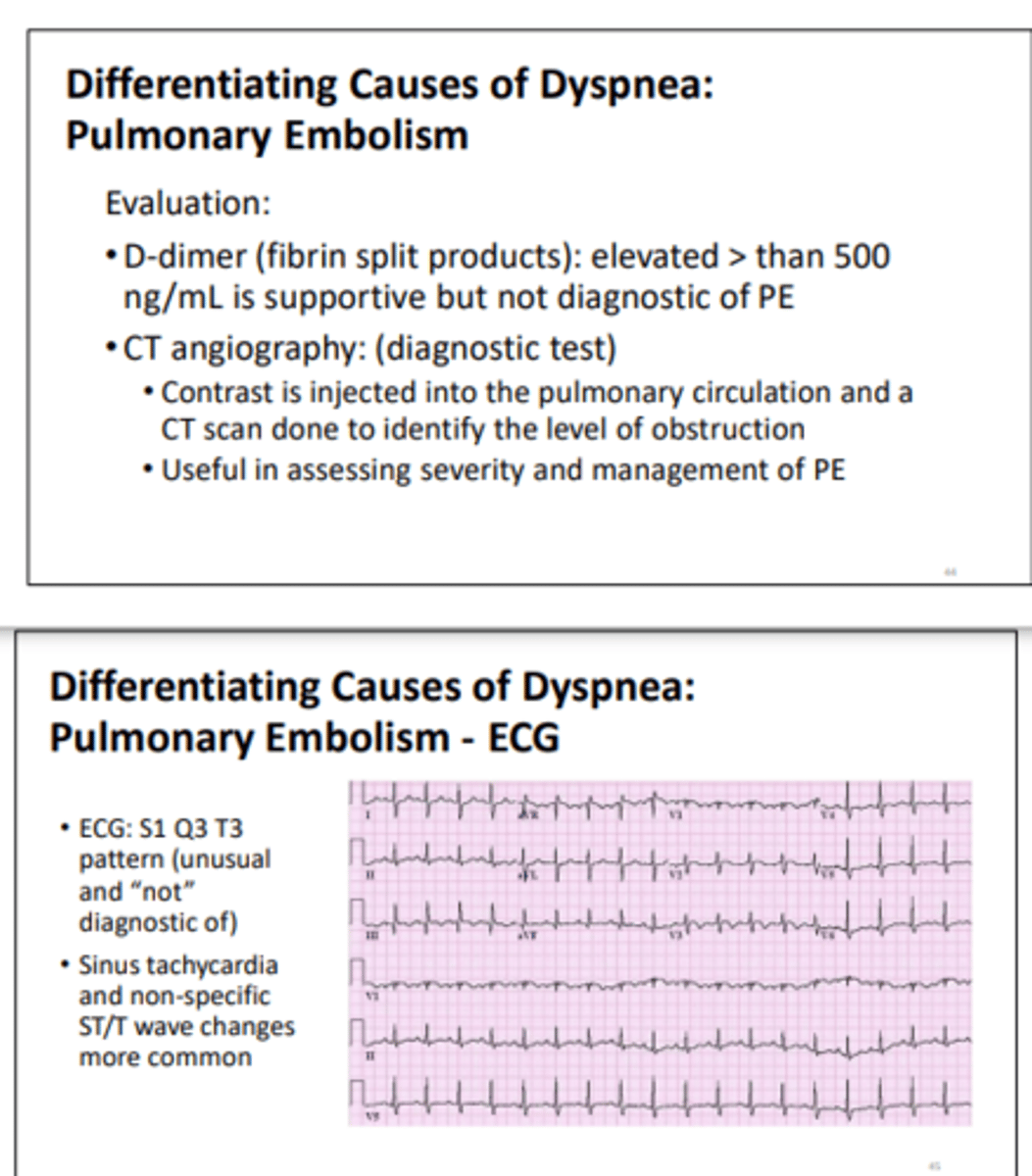
Give 2 ECG signs of PE
1. Sinus tachycardia
2. Atrial fibrillation
Name 2 diseases caused by moderate ischaemia
1. Angina
2. Intermittent claudication
Name a disease caused by severe ischaemia
critical limb ischaemia
Give 2 signs of RHF
1. Raised JVP
2. Ascites

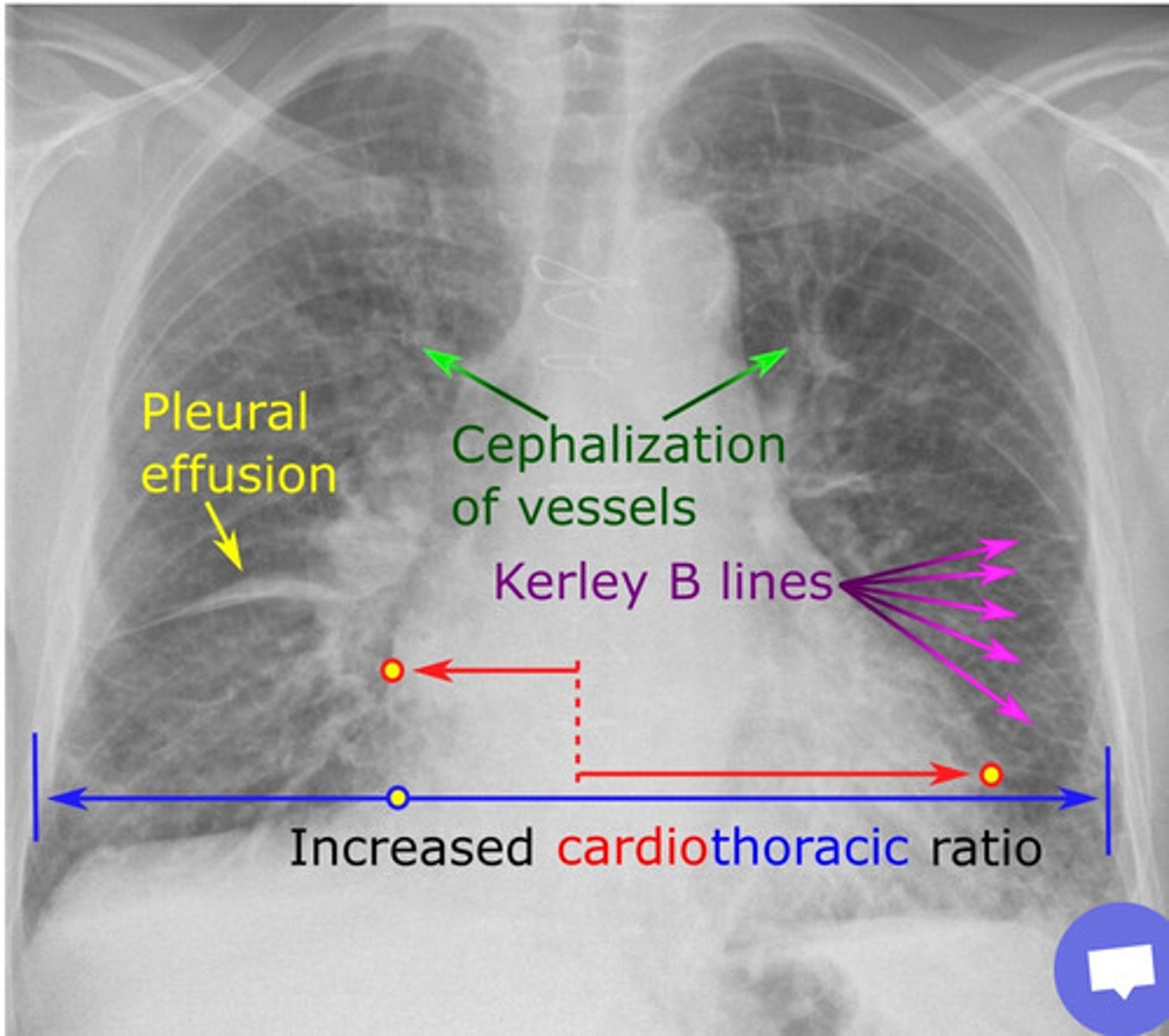
Give 5 signs you might see on a CXR taken from someone with heart failure
1. Pleural effusion
2. Dilated pulmonary arteries
3. Kerley B lines
4. Bat's wings
5. Cardiomegaly
Why might someone with HF feel breathless when lying down?
due to pulmonary oedema
Why might someone with HF have peripheral oedema?
1. Deceased venous pressure
2. RAAS activation → sodium and H2O retention
Give 6 signs of anaphylactic shock
1. Breathlessness
2. Wheeze
3. Rash
4. Swollen lips/tongue
5. Low BP
6. Chest tightness
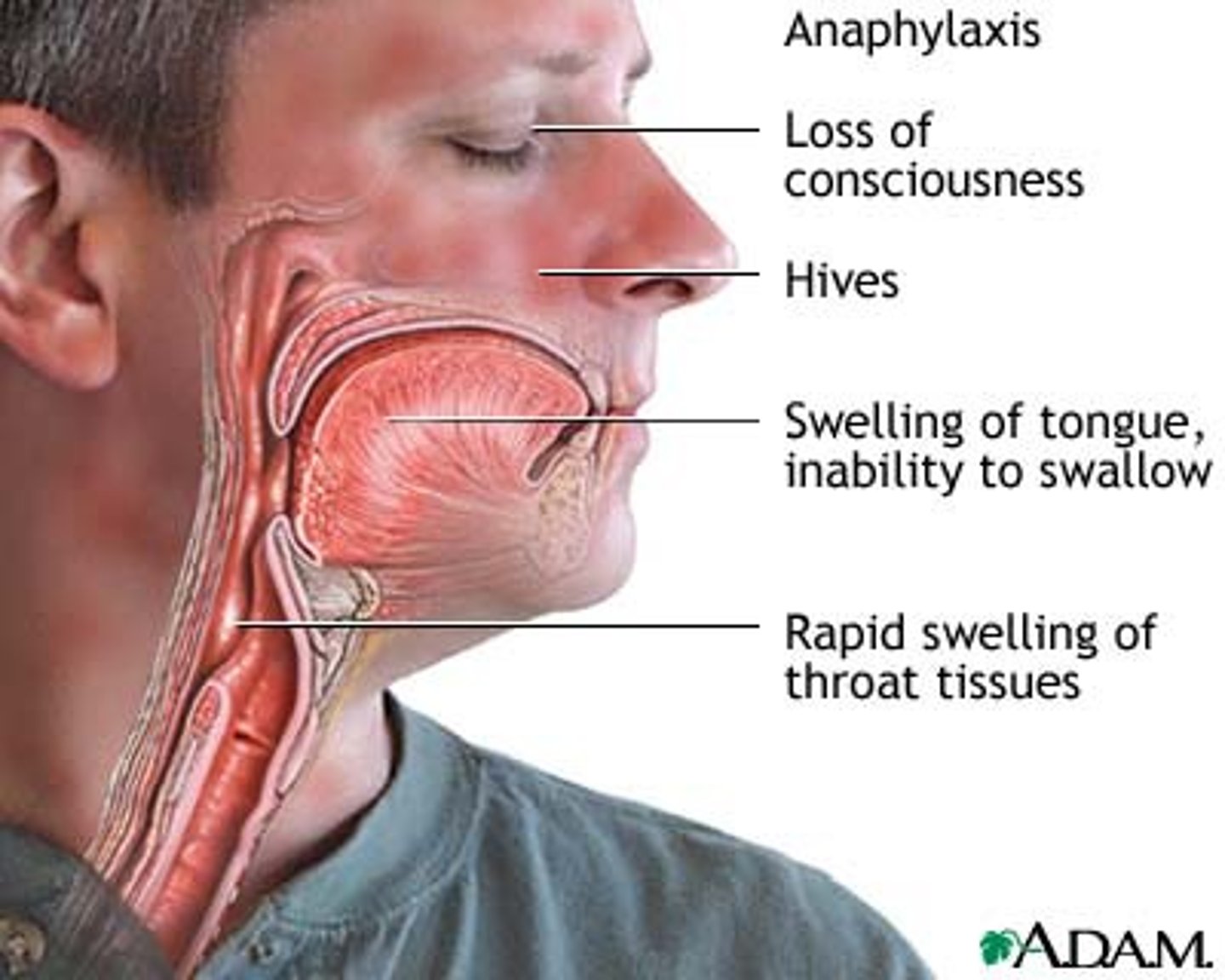
Why might someone with anaphylactic shock have a low BP?
1. Vasodilation
2. Increased vascular permeability
In what other conditions (bar ACS) would you see raised troponin?
1. Gram negative sepsis
2. Pulmonary embolism
3. Myocarditis
4. Heart failure
5. Arrhythmias
Would a baby born with ASD be cyanotic?
no-higher pressure in the LA than the RA so blood is shunted left to right
What is the treatment choice for STEMI?
PCI
Give 5 clinical signs of a large ASD
1. Significant increase in blood flow through the right heart + lungs - pulmonary flow murmur
2. Enlarged pulmonary arteries
3. Right heart dilation
4. SOBOE - shortness of breath on exertion
5. Increased chest infection
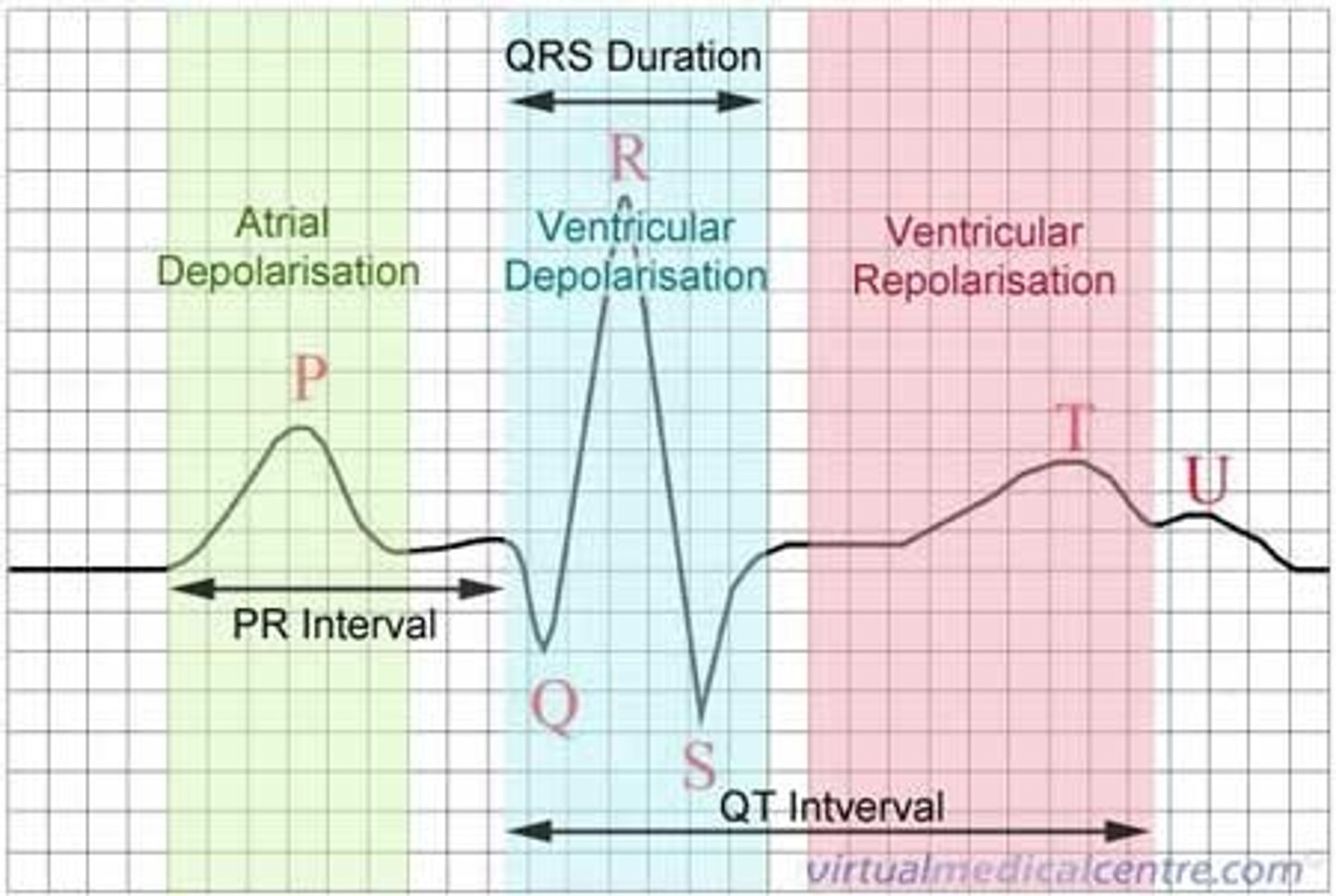
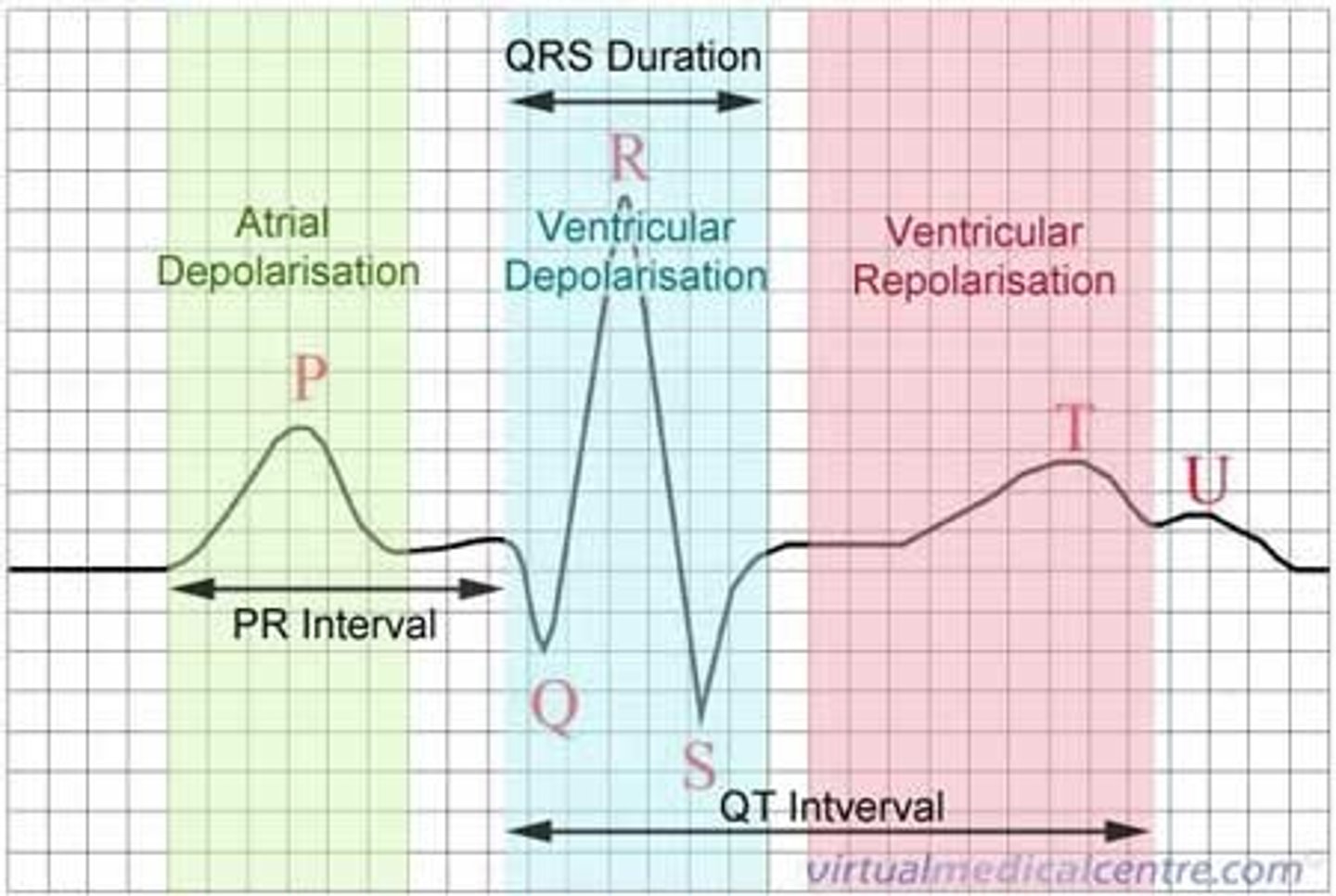
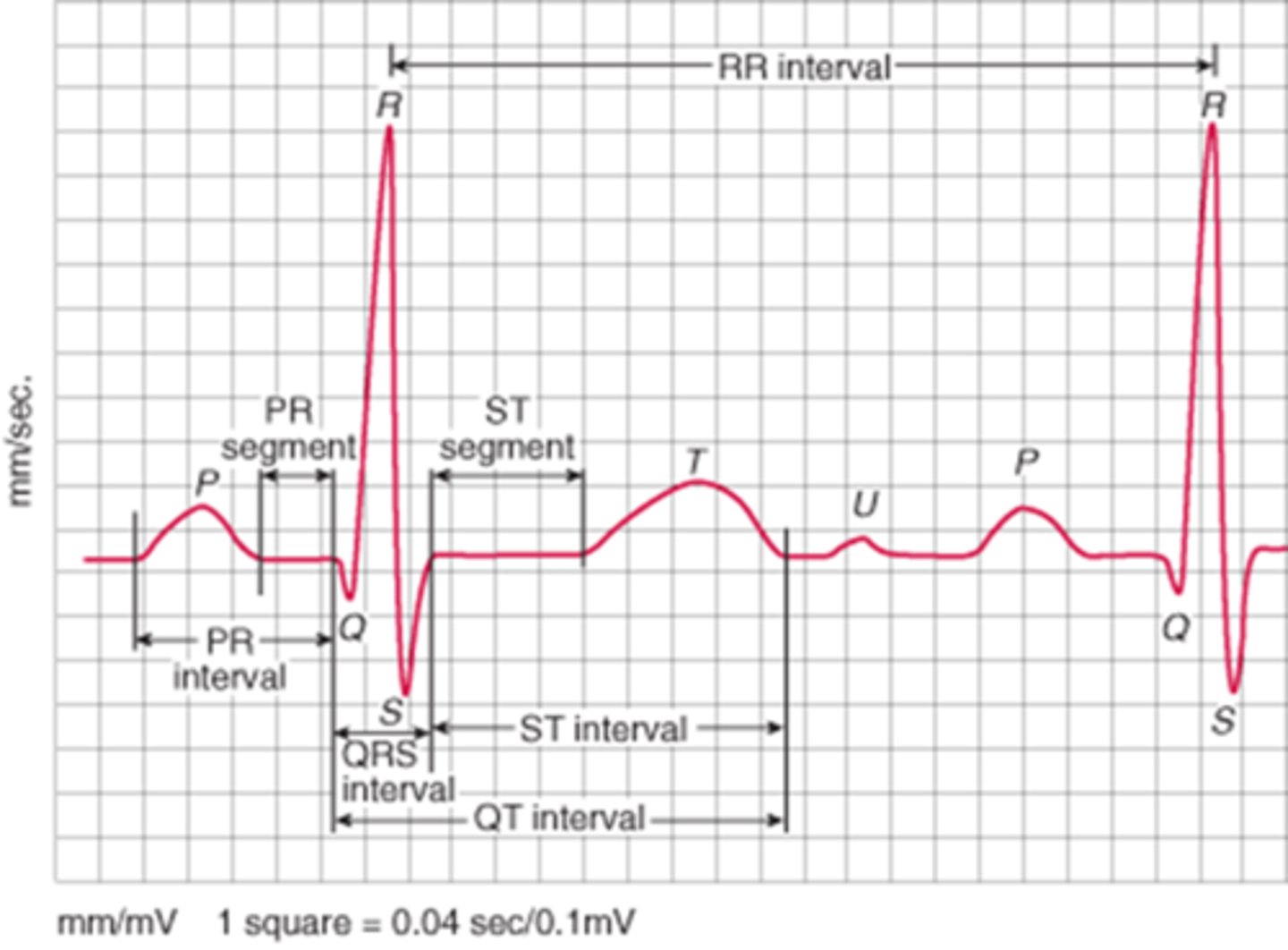
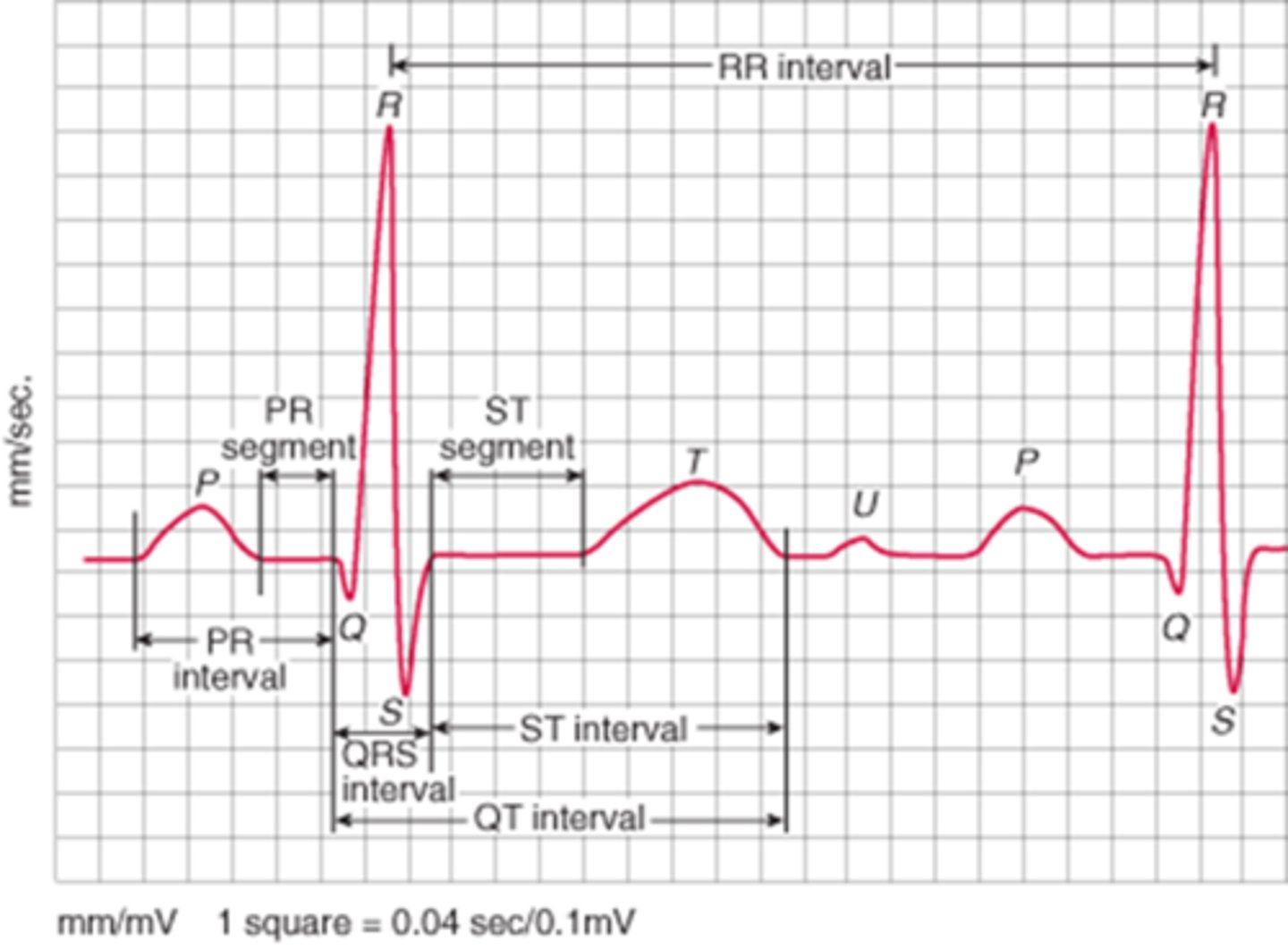
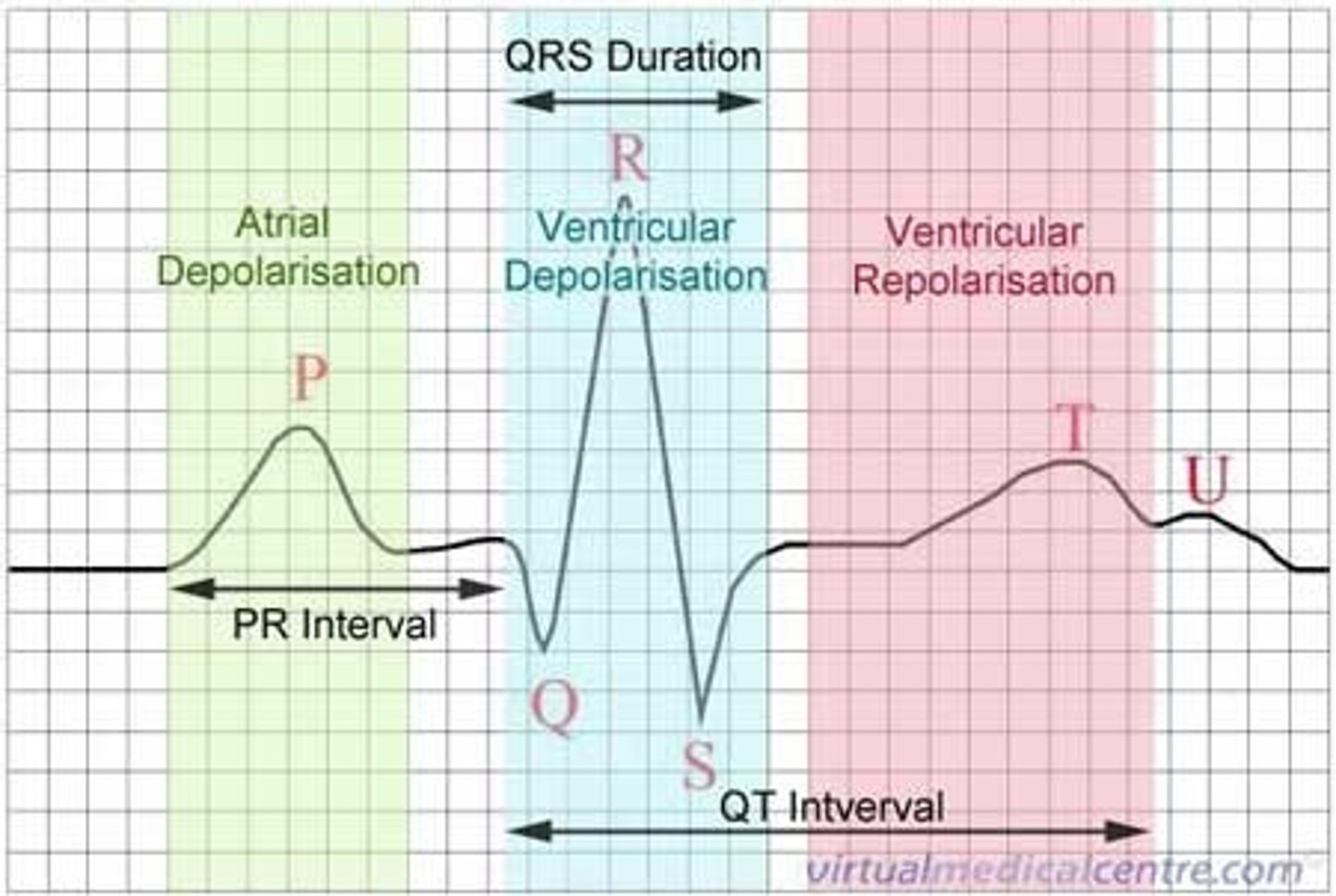
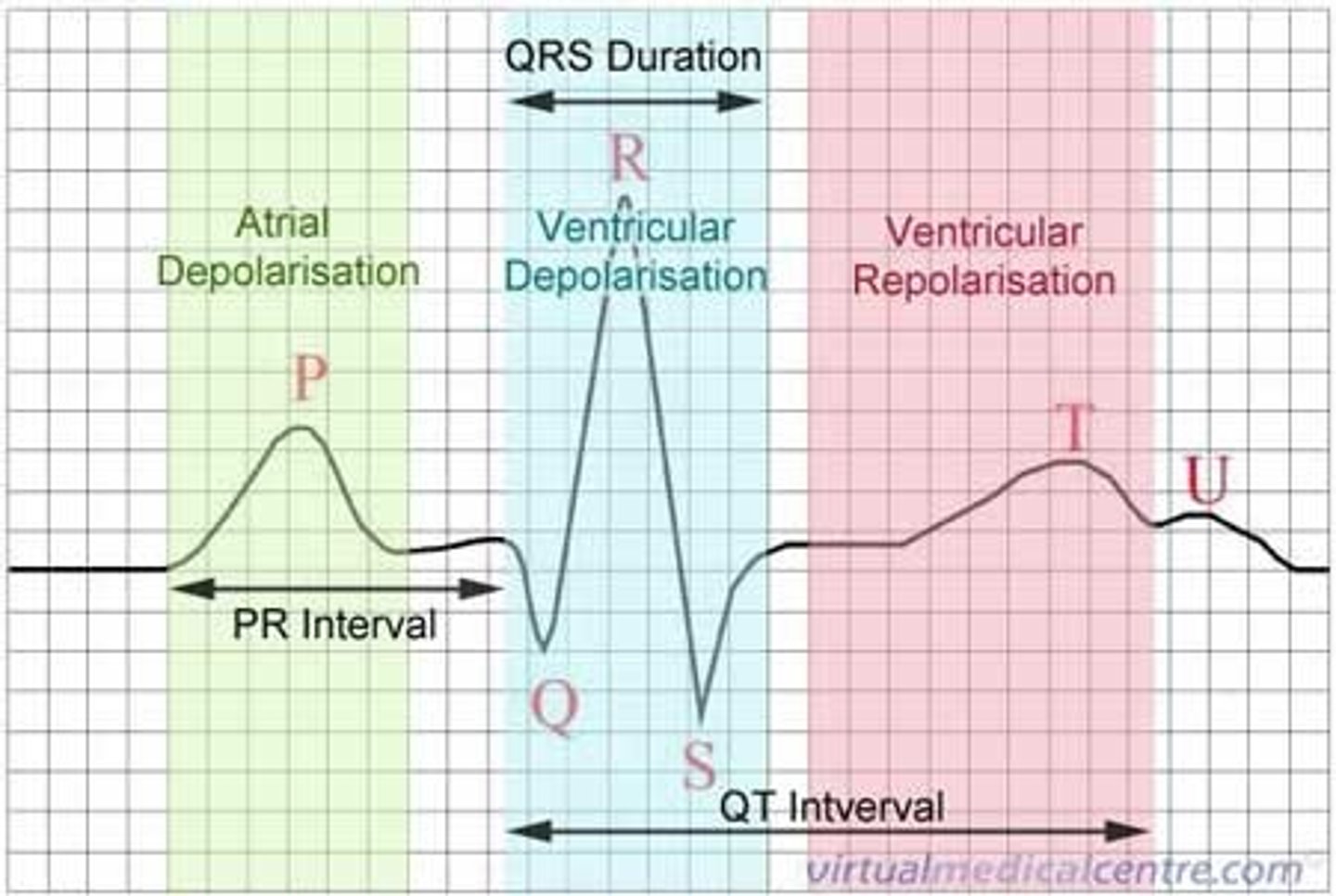
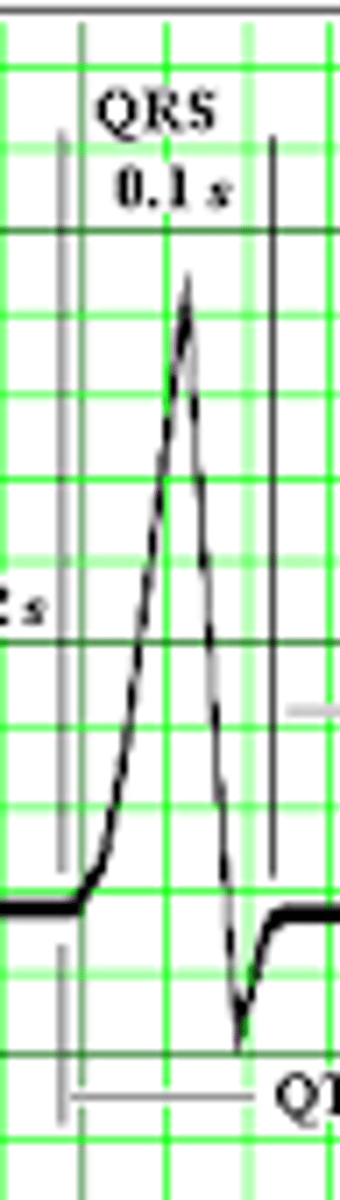
ECG: What is the J joint?
where the QRS complex becomes the ST Segment
What is AVSD?
atrioventricular septal defect -basically a hole in the centre of the heart
ECG: what does the P wave represent?
atrial depolarisation
Give 2 clinical signs of AVSD
1. Breathlessness
2. Poor feeding and poor weight gain
ECG: How long should the PR interval be?
120-200ms
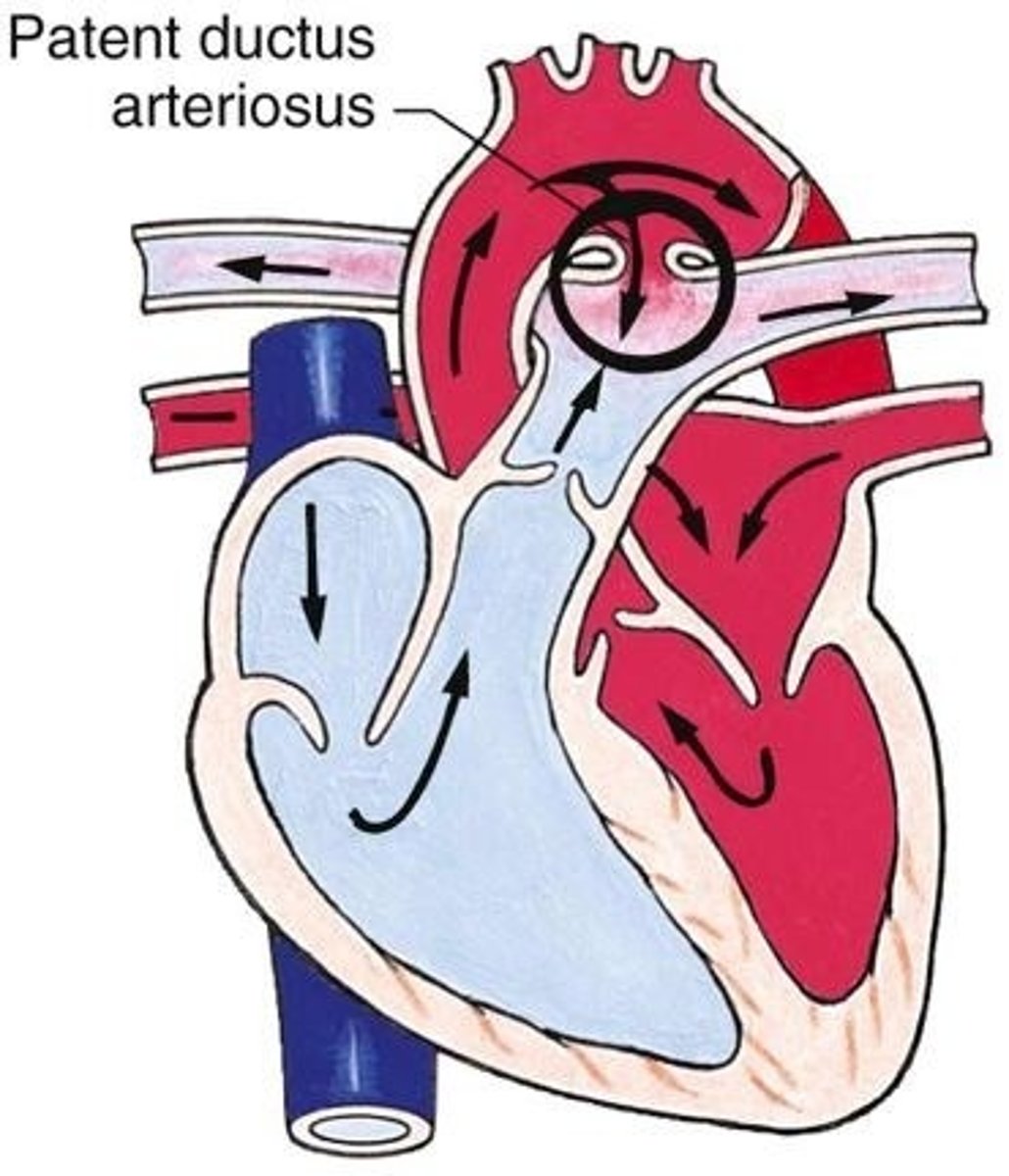
What is PDA?
patent ductus arteriosus
ECG: What might a long PR interval indicate?
Heart block
Give 4 clinical signs of PDA
1. Torrential flow from the aorta to the pulmonary arteries can lead to pulmonary hypertension and RHF
2. Breathlessness
3. Poor feeding, failure to thrive
4. Risk of endocarditis
ECG: How long should the QT interval be?
0.35-0.45s
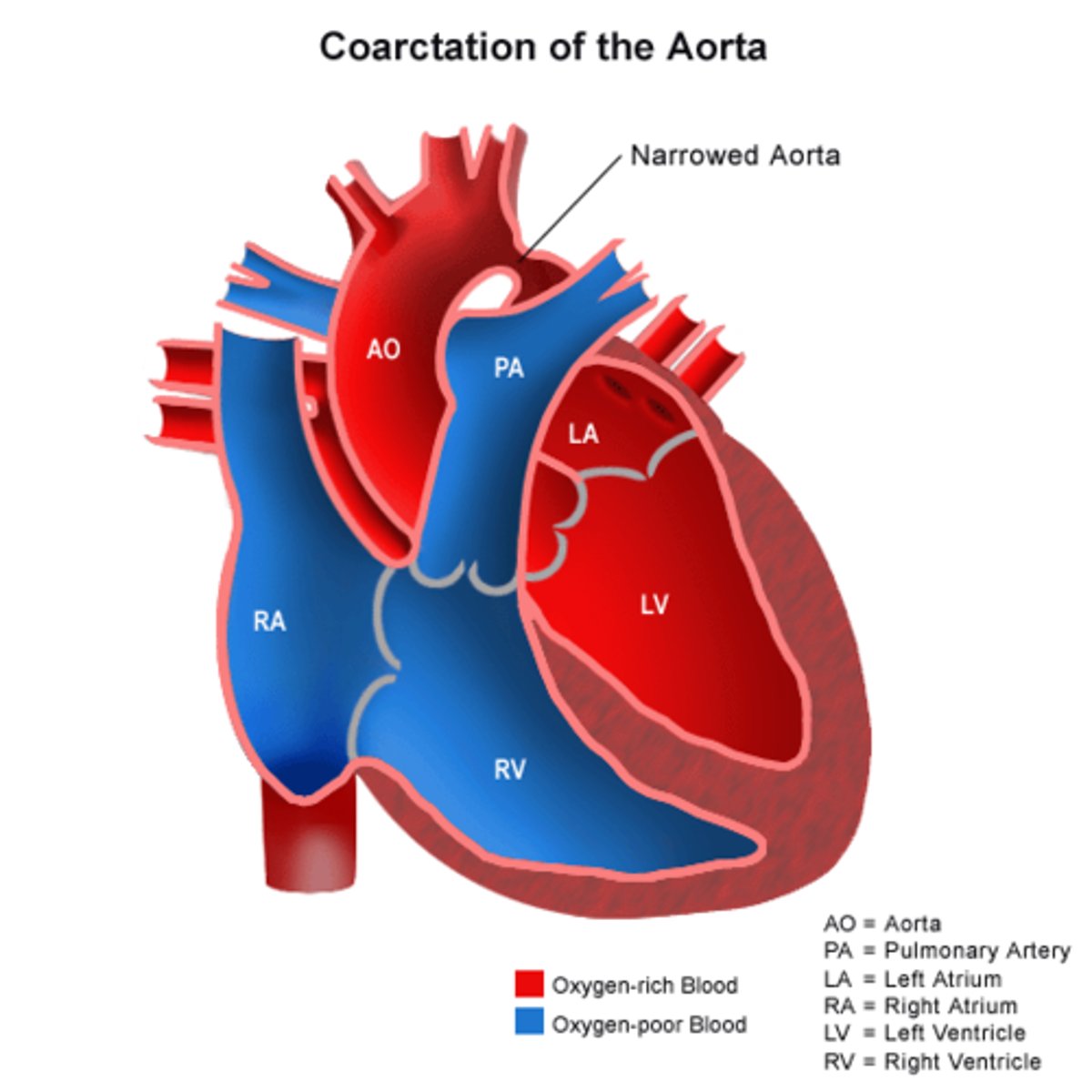
Describe the pathophysiology behind coarctation of the aorta
Excessive sclerosing that normally closes the ductus arteriosus extends into the aortic wall leading to narrowing
ECG: What does the QRS complex represent?
ventricular depolarisation
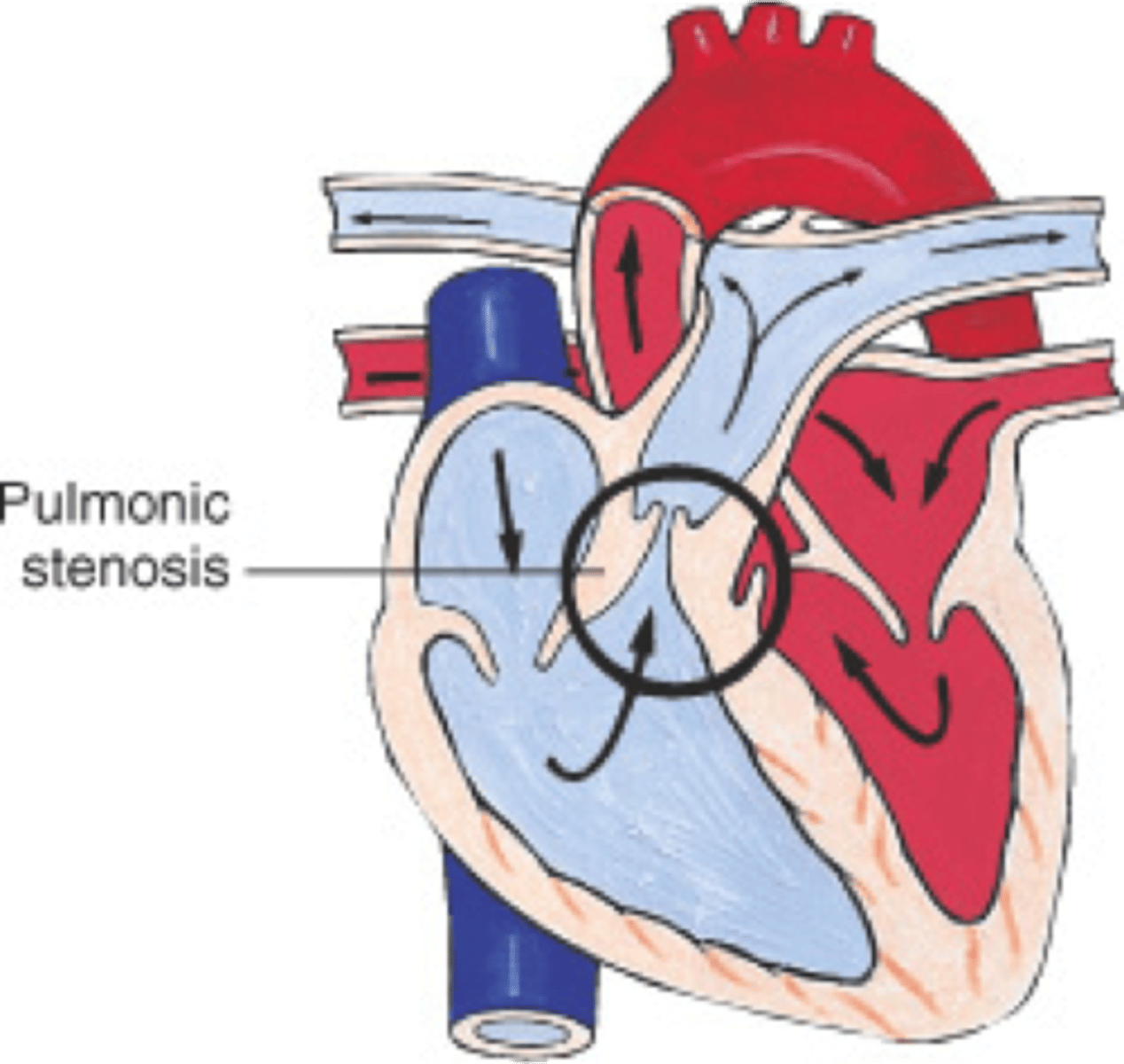
What is pulmonary stenosis?
Narrowing of the RV outflow tract
ECG: What does the T wave represent?
ventricular repolarisation
Define cardiac failure
The inability of the heart to pump blood at the rate required for normal metabolism
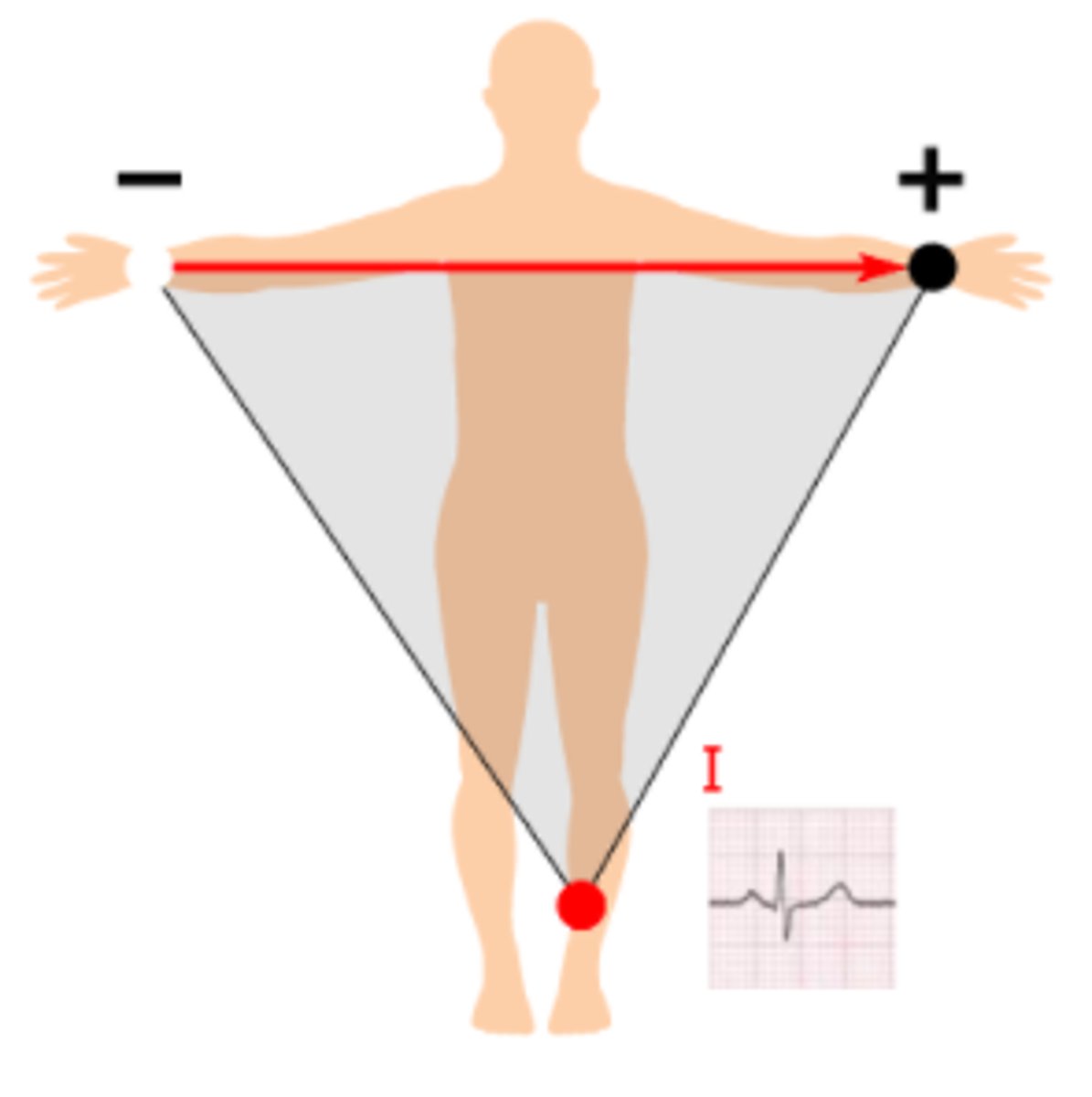
ECG where would you place lead 1?
From the right arm to the left arm with the positive electrode being at the left arm, at 0°
what are the two broad categories for heart failure?
1. Systolic (not pumping effectively)
2. Diastolic (relaxing+ filling abnormally)
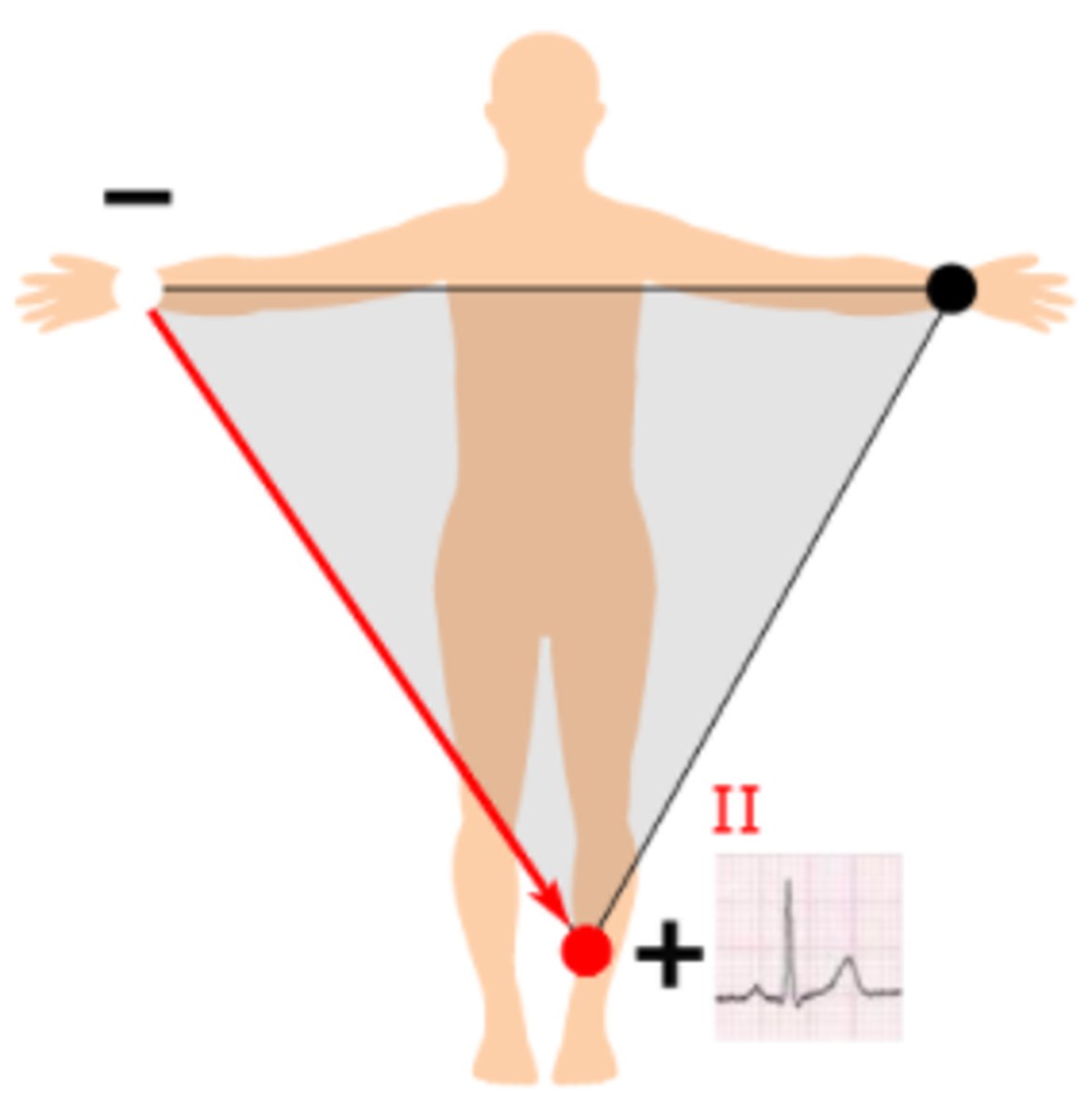
ECG: Where would you place lead 2?
From the right arm to the left leg with the positive electrode being at the left leg, at 60°
Give 5 causes of heart failure
1. IHD (most common)
2. Hypertension
3. Cardiomyopathy
4. Excessive alcohol
5. Obesity
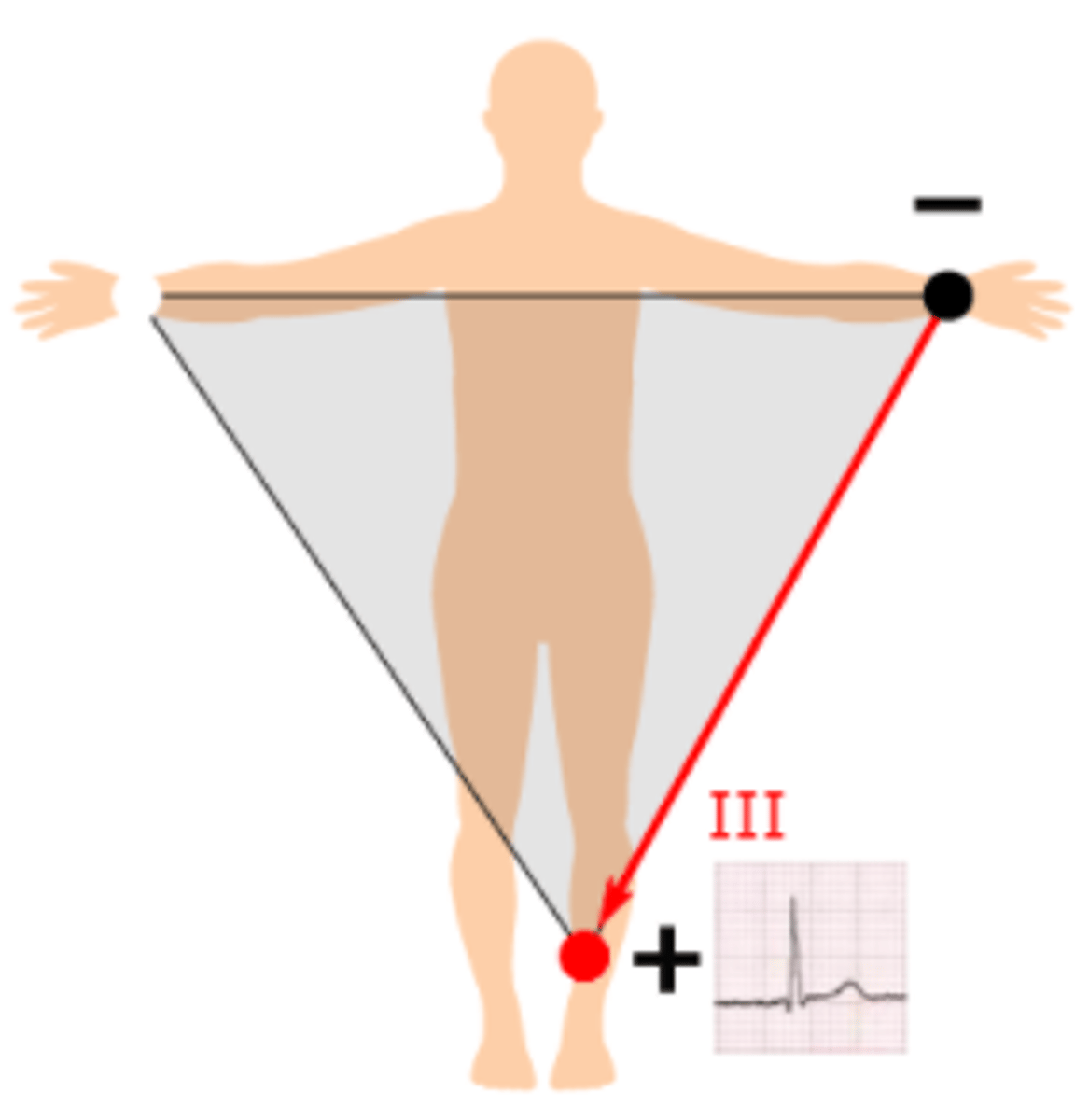
ECG where would you place lead 3?
From the left arm to the left leg with the positive electrode being at the left leg, at 120°
Why are men more commonly affected by HE than women?
women have 'protective hormones'
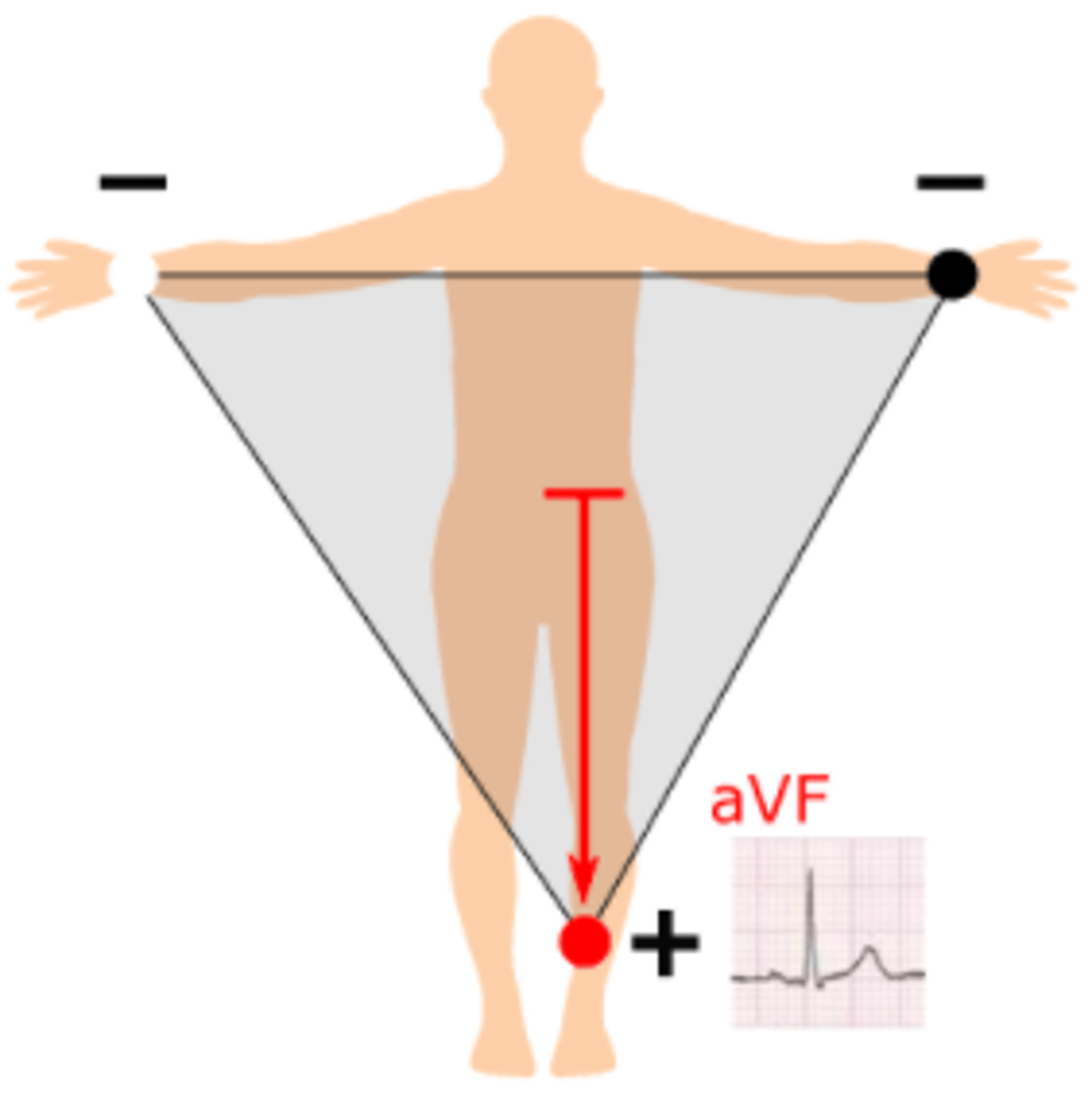
ECG: where would you place lead aVF?
From halfway between the left arm and right arm to the left leg with the positive electrode being at the left leg, at 90°
what are the compensatory mechanisms in HF?
1. Sympathetic system
2. RAAS
3. Natriuretic peptides
4. Ventricular dilation
5. Ventricular hypertrophy
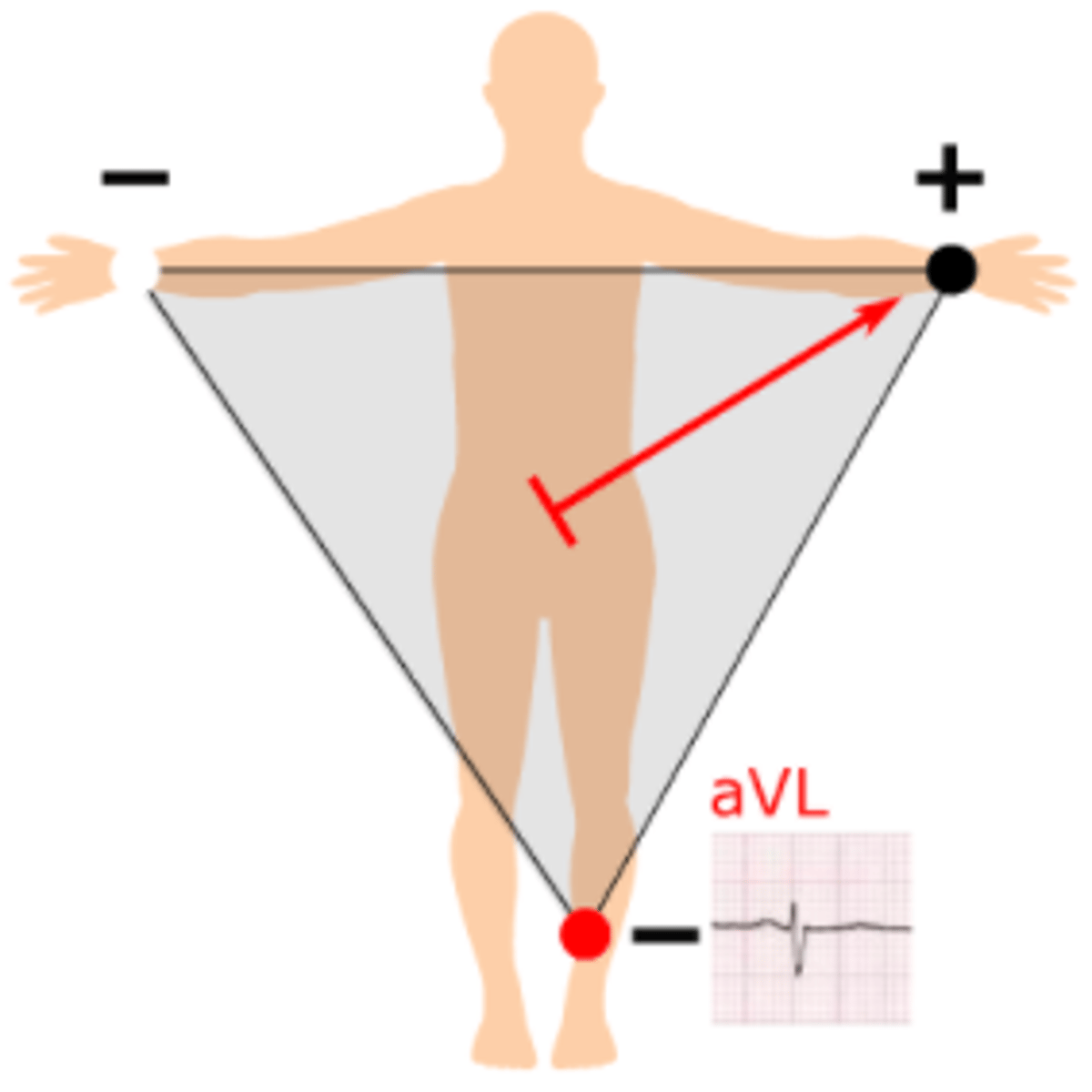
ECG: Where would you place lead avL?
From halfway between the right arm and left leg to the left arm, with the positive electrode being at the left arm at -30°
Explain how the sympathetic system is compensatory in heart failure and give one disadvantage of sympathetic activation
improves ventricular function by increasing HR and contractility = CO maintained
BUT it also causes arterioIar constriction which increases afterload and so myocardial work
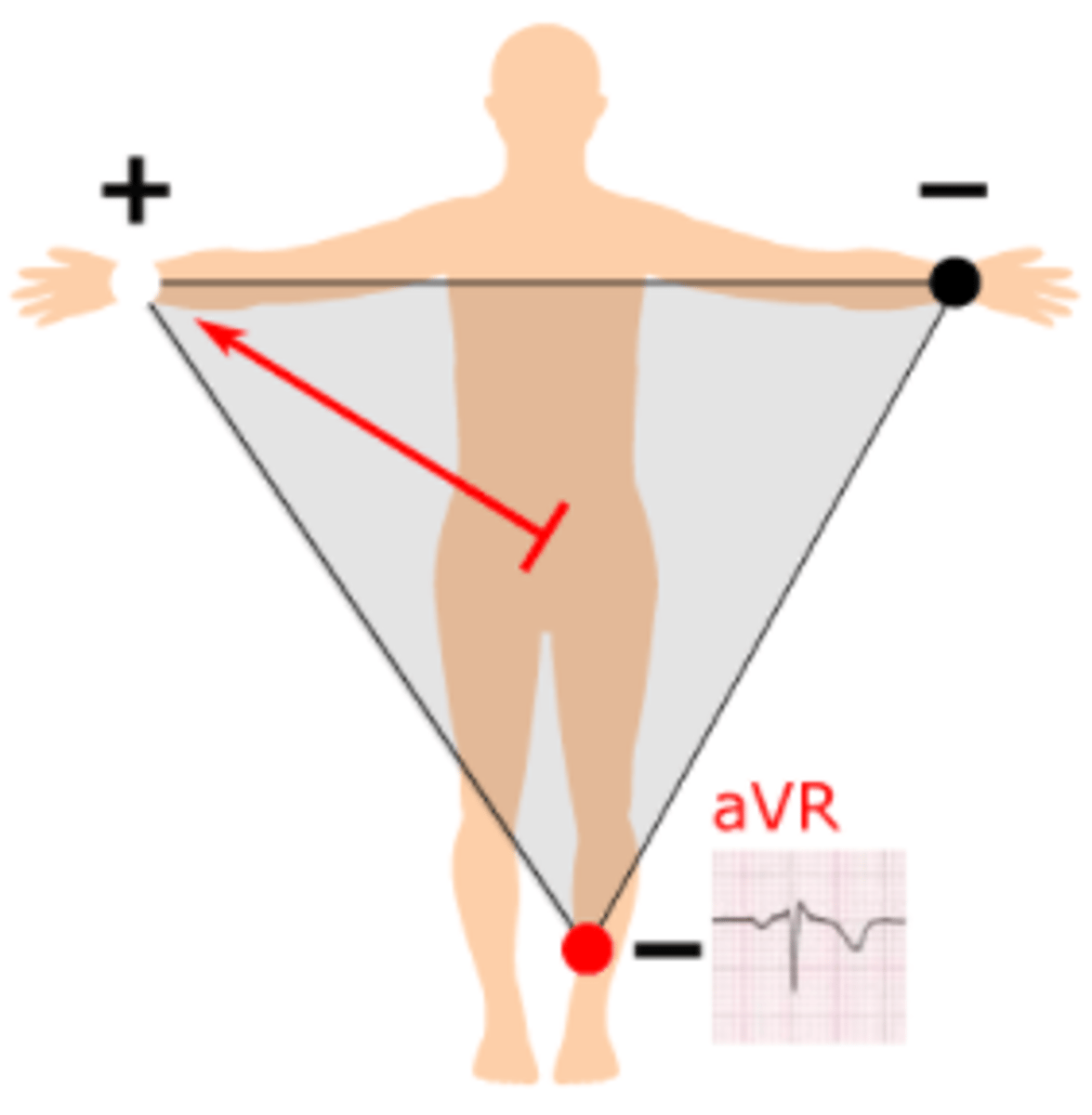
ECG: where would you place lead avR?
From halfway between the left arm and left leg to the right arm, with the positive electrode being at the right arm at -150°
Explain how RAAS is compensatory in HF and give one disadvantage of its activation
reduced CO leads to reduced renal perfusion; this activates RAAS. there is increased fluid retention and so increased preload
BUT it causes arterioIar constriction which increases afterload and so myocardial work
How many seconds does a) small squares and b) large squares represent on ECG paper?
a) 0.04s
b) 0.2s
Give 3 properties of natriuretic peptides that make them compensatory in HF
1. Diuretic
2. Hypotensive
3. Vasodilators
How long should the QRS complex be?
less than 110ms
What are the 3 cardinal symptoms of HF?
1. Shortness of breath
2. Fatigue
3. Peripheral oedema
Give up to 8 potential side effects of beta blockers
1. Fatigue
2. Headache
3. Nightmares
4. Bradycardia
5. Hypotension
6. Cold peripheries
7. Erectile dysfunction
8. Bronchospasm
What is the first line of treatment for a Pt under 55 with hypertension?
ACE inhibitors (eg. Ramipril) or ARB (e.g. candesartan)
What is the first line of treatment for a pt with hypertension who is over 55?
calcium channel blockers ( e.g. Amlodipine)
What is heart failure?
When the heart is no longer able to pump blood to sustain the body's metabolic needs
What is the most common cause of heart failure?
ischaemic heart disease
What hormones does the heart produce?
ANP and BNP (brain natriuretic peptide)