clinical psychology and mental health
1/65
Earn XP
Description and Tags
abnormality + disorders
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
66 Terms
how many definitions of abnormality are there?
statistical infrequency
deviation from social norms
failure to adapt adequately
deviation from ideal mental health
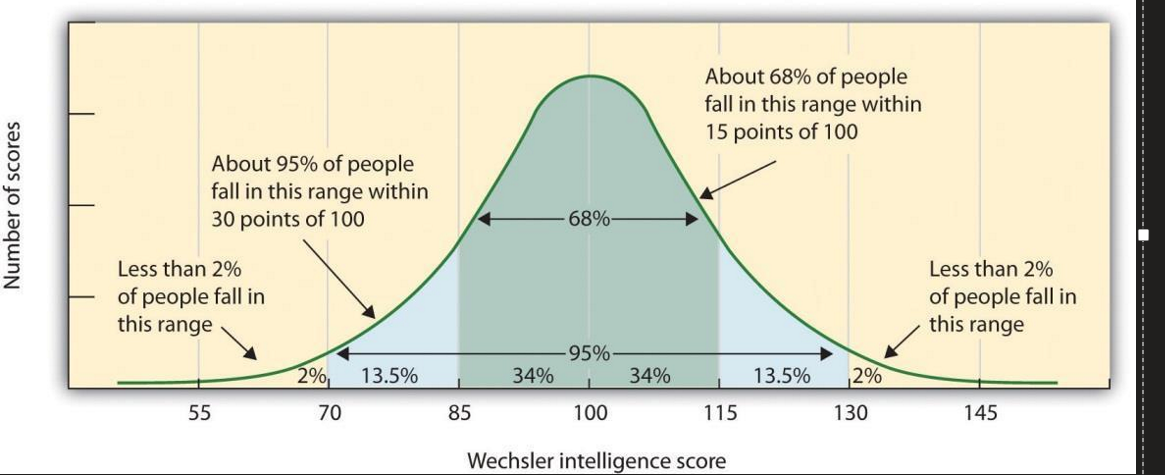
what’s the definition of statistical infrequency
A behaviour is abnormal if its statistically uncommon or rare in society
Based on how behaviours are distributed within a population
normal distribution
Bell-shaped curve.
Middle = range
As you move away from the centre ( + or - standard deviations), fewer people have that score --> more abnormal
Mean = median = mode
if its falls under 2.5% of the population then its considered abnormal
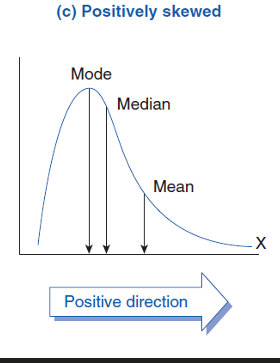
positive skewed distribution
Order: mean< median< mode
The tail is on the right side (positive = right)
Most scores are low, only few are high
Example: a very difficult test (most student get low marks)
Mean is dragged right by the few high scores
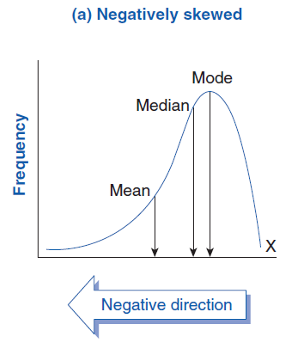
negative skewed distribution
Order: mean>median>mode
The tail is on the left side
Most scores are high, only a few are low
Example: a very easy test (most student got high marks)
Mean is pulled left by the few low scores
evaluation on statistical infrequency
misdiagnosis: some common behaviours could be causing distress but according to this definition its normal e.g. depression
labelling someone who is happy as abnormal could cause low self esteem
Not all abnormal (rare) rates are undesirable, Example: high IQ = rare, but positive
Deviation of social norms
A person is seen as abnormal if their behaviour violates the unwritten rules (social norms) of what is acceptable within a particular society or culture
Real-life example:
Antisocial Personality Disorder (APD): Person is impulsive, aggressive, irresponsible, and lack guilt- behaviour that breaks social and moral standards
Schizotypal Personality Disorder (SPD): Shows eccentric or superstitious beliefs (e.g. seeing things not real), which deviate from cultural norms.
evaluation on deviation from social norms
Cultural relativism: What's "normal" varies across cultures and over time. e.g. in Thailand Karen women wears rings around their neck from young age as a sign of beauty and cultural identity
Historical changes/Hindsight Bias: Norms change over time e.g. in the UK, homosexuality was classed as a mental illness until 1973 → it can also form social control to suppress minority groups (Szasz, 1947)
failure to function adequately
A person is consider abnormal of they are unable to cope with everyday life r meet the demands of daily living-like maintaining relationship, work, or self-care.
→ example: someone with depression may find it difficult to get out of bed, go to work, or communicate with others
Rosenhan and Seligman's criteria
They suggested key sign to identify when someone isn't functioning adequately:
criterion | Description/example |
suffering | Person feels distress (e.g. depression, headaches, exhaustion) |
Maladaptive | Behaviour interferes with everyday goals (e.g. can't go to work) |
Irrationality | Behaviour seems illogical (e.g. panic without reason) |
Observer Discomfort | Makes others feel uncomfortable (e.g. shouting, swearing) |
Vividness' | Behaviour appears strange (e.g. extreme body modification) |
Violation of Moral Codes | Goes against social norms (e.g. paedophilia) |
unpredictability | Behaviour is inconsistent or unexpected |
→ acronym: VIVOUSM
evaluation on failure to function adequately
Individual differences: Two people with same disorder may cope differently, so diagnosis can be inconsistent
Subjective judgement: what count as "failing" can very between observers
Cultural bias: people who live differently (e.g. alternative lifestyles) may be unfair labelled as abnormal
deviation from ideal mental health
Made by Marie Jahoda
Made a criteria that all of them must be achieved to be normal
→ if you don’t meet one of them then you are not normal
Jahoda’s criteria
Positive attitude toward yourself- for ideal mental health, the individual should feel happy with themselves and have a positive attitude about who they are e.g. self-harm, insecurities, depression, social anxiety
Self-actualisation- for ideal mental health, an individual should be able to visualise and reach their potential, this link with Maslow's hierarchy of needs, in the humanistic approach. It refer to a person ability to be content with themselves. e.g. social anxiety, CBA (lost motivation), schizophrenia
Personal autonomy- for ideal mental health, an individual should not have to be dependent on others. This refers to having independence of thought and behaviour, and being able to make your own decisions and look after yourself e.g. depression, OCD, learning disability, ADHD
Jahoda’s criteria (part2)
Resistance to stress- for ideal mental health, an individual should be able to handle stressful situations competently without feeling distress. This refers to the tolerance for stress of an individuals, and their ability to cope with stressful situation. e.g. OCD, anxiety, aggression
Environmental mastery- for ideal mental health, an individual should be able to change their behaviour and attitudes when a change in society or daily life occur. e.g. autism, OCD, ADHD
Accurate perception of reality- for ideal mental health, an individual should interpret the world and environment similarly to others and not disability thinking such as delusions or hallucinations e.g. schizophrenia
evaluation on deviation from ideal mental health
what’s a phobia
A phobia is an anxiety disorder involving an irrational fear of a specific object, situation, or place
what are the three types of phobia
Simple (specific) Phobias
Social Phobias
Agoraphobia
Simple (specific) Phobias:
Fear of one specific object/situation.
Categories of simple phobias
Animal phobias --> spiders (arachnophobia), snakes, dogs
Injury phobias --> blood (hemophobia), injections, needles
Situational Phobias --> flying, lifts, dentists
Natural environment phobias --> water, hights, storms
Social Phobias
Fear of social situations because the person feels judged, embarrassed or inadequate
three types of social phobias
Performance phobia → speaking in public, eating in front of others
Interaction phobia → talking to strangers, answering questions
Generalised social phobia → fear of most social situations (e.g. crowds)
Agoraphobia
Fear of open or public spaces where escape feels difficult.
causes of agoraphobia
Simple phobias (e.g., fear of contamination → avoiding public areas)
Social phobia (fear of people → avoiding open spaces)
behavioural characteristics of phobia
Avoidance: Person a voids the phobic trigger. e.g. social phobias → avoids crowds; arachnophobia → avoids basements
Panic: Crying, shaking, screaming, running away, Extreme panic may trigger freeze (fight-flight-freeze response)
emotional characteristics of phobias
Intense, unreasonable fear
Anxiety + panic when thinking about or facing the phobic object
→ More than what is appropriate for the situation
cognitive characteristics
Selective attention: Hard to look away from the feared object, The person becomes hyper-focused on the threat
Irrational beliefs: e.g. believing "all spiders can kill me" even in the UK where non are deadly
what type of disorder is depression?
mood disorder
two types of depression
Unipolar depression: major depression
Bipolar disorder: (includes mania)
behavioural characteristics of depression
Activity levels: Reduced energy → fatigue → withdrawal from work/social life. In severe cases, unable to get out of bed
Disruption of sleep & eating: Insomnia (difficulty sleeping) or Hypersomnia (sleeping too much) and Appetite changes (loosing or gaining 5% of body weight)
Aggression & self-harm: Irritability and anger towards other. e.g. Self-harm behaviours (cutting) or suicide attempts/thoughts
emotional characteristics of depression
Lowered mood: Intense, persistent sadness. e.g. Feeling "empty" hopeless, worthless.
Anger: Anger may be directed at self or others.
Lowered self-esteem: Feeling of worthlessness, In severe cases: self-harm
cognitive behavioural of depression
Poor concentration: Difficulty focusing, slower decision making e.g. Struggle completing tasks
Selective thinking: Pay more attention to negative event, Their attention become biased toward anything that fits their negative views and ignores positive events
Absolutist thinking: Everything is either completely good or completely bad, Small issues become catastrophes
what is OCD?
OCD is an anxiety disorder with two main components:
Obsessions = intrusive, persistent thoughts
Compulsions = repetitive behaviours used to reduce anxiety
random facts
About 70% of suffers experience both obsessions + compulsions
20% have only obsessions
10% have only compulsion
OCD create a cycle: Obsession → anxiety -→ compulsion → temporarily relief
behavioural characteristics
Compulsions are repetitive: Sufferers feel a strong urge to carry out repetitive behaviours. Common examples:
Repeated hand-washing
Repeated checking (doors/windows locked, appliances off)
Repeating certain rituals
Compulsions reduce anxiety: Compulsions are performed as a direct response to obsessive thoughts
Avoidance: Some sufferers may avoid situations that trigger their obsessions. E.g. avoiding public places to avoid germs
emotional characteristics of OCD
Anxiety and distress: Obsessions are frightening → produce high anxiety
Compulsions relieve anxiety temporarily, but the cycle continues
Accompanying depression
Anxiety + constant interruption of daily life --> low mood and loss of pleasure
Sufferers may feel:
Worthless
Constant sadness
Irritability
Guilt and disgust: Some sufferers experience Guilt and disgust toward themselves or the object of the obsession
cognitive characteristics of OCD
Obsessive thoughts: Intrusive, recurring, uncontrollable thoughts such as:
Fear of contamination
Fear of harming someone
Religious fears
Irrational thoughts: Sufferers hold beliefs that are illogical or disconnected from reality e.g. "if I don’t wash my hands 20 times, or I will get contaminated again"
Cognitive coping strategies: Some sufferers use mental strategies to cope, e.g. Praying repeatedly
Selective attention Sufferers focus only on anxiety-triggering stimuli e.g. A person with contamination fears will constantly notice dirt/germ in the environment
Insight into excessive anxiety: Sufferers are usually aware that:
Their obsessions are irrational
Their compulsions do not logically prevent danger
Despite this insight, they cannot stop the behaviour
behavioural treatments to phobia
→ behaviourists believe phobias are learned, not inherited.
Mowrer (1947) proposed the Two-process model:
1. classical conditioning
operant conditioning
classical conditioning
Phobias first developed when neutral stimulus (NS) becomes associated with fear-producing unconditioned stimulus (UCS)
Process
NS → no fear
UCS (e.g., loud noise) → fear
NS + UCS paired together → fear
NS becomes a conditioned stimulus (CS) producing conditional fear (CR)
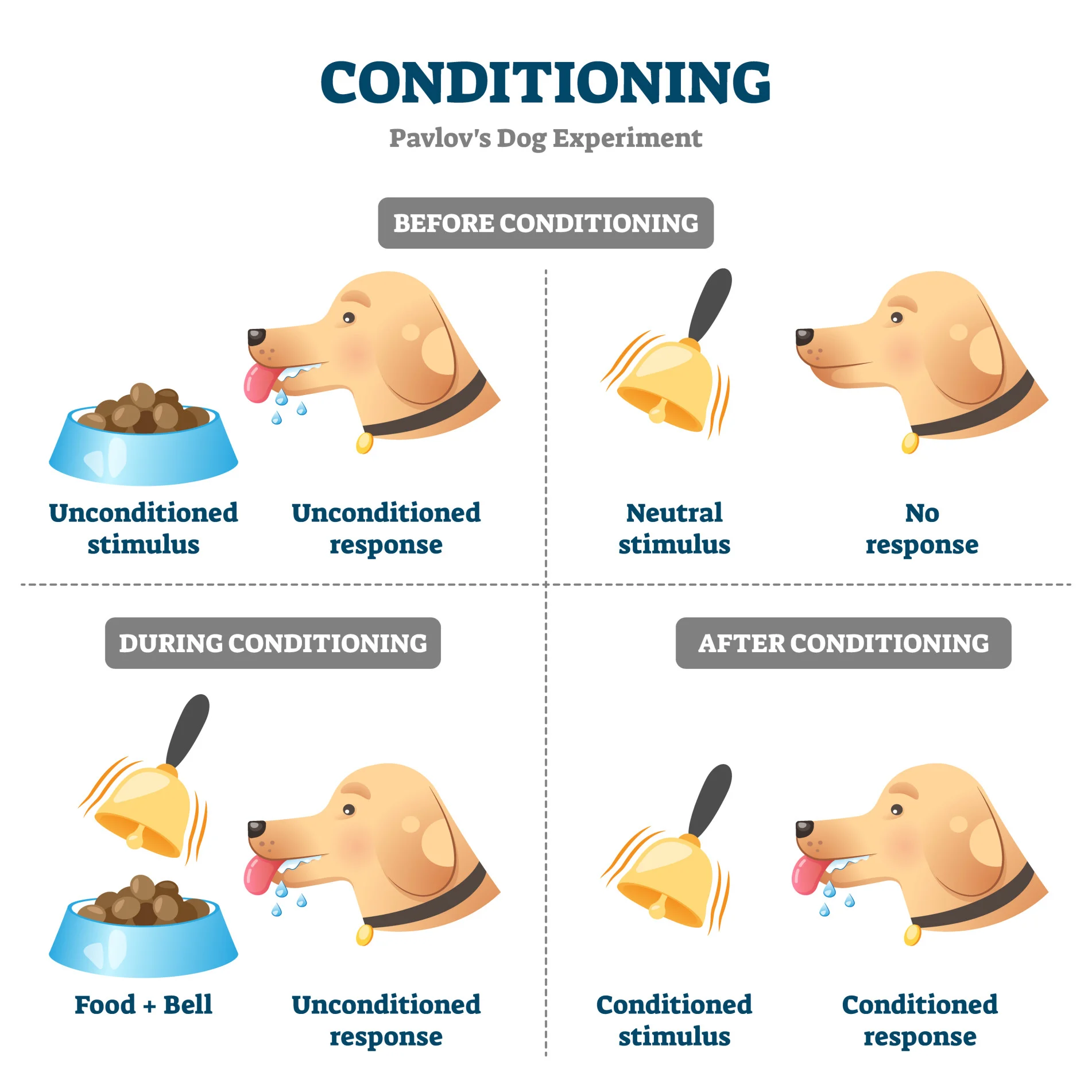
example of classical conditioning
little Albert (Watson & Rayner, 1920)
Albert showed no fear of a white rat (NS)
Loud noise (UCS) paired with rat caused fear
Rat became CS --> Albert cried
Fear generalised to similar white objects (e.g. Santa beard)
operant conditioning
Once the phobias exists, it is maintained through negative reinforcement.
Avoiding the fear situation reduces anxiety
The relief reinforces avoidance behaviour
Parson continues avoiding → phobias maintained long-term
example of operant conditioning
someone with a lift phobias avoids lifts → avoids anxiety → relief → keeps avoiding → phobia stays strong
positive reinforcement
Reinforcement = increases behaviour
Definition: adding something pleasant to increase behaviour
Effect: behaviour is repeated
Example: getting money for good grades
negative reinforcement
Definition: removing something unpleasant to increase behaviour
Effect: behaviour is repeated
Example: seatbelt alarm stops when belt is fastened
→ key point negative reinforcement does not mean punishment
Positive consequences:
Consequence = observed outcomes of behaviour
Definition: behaviour is followed by a reward
Effect: observer is more likely to imitate behaviour
Example: student sees someone rewarded --> imitates action
negative consequence
Definition: behaviour is followed by punishment or disapproval
Effect: observer is less likely to imitate behaviour
Example: student sees someone getting told of --> avoids behaviour
evaluation on classical & operant conditions
Ignores cognition: behavioural theory ignores irrational thoughts yet these often drive phobias
Not all phobias come from trauma: many people with phobias cannot recall a bad experience.
Evolutionary explanation suggests human are naturally predisposed to fear danger (snakes, spiders, heights)
Reductionist: oversimplified phobias to stimulus- response learning and ignores emotions, biology, personality
what are the two behavioural treatment for phobia
Systematic Desensitisation (SD)
flooding
Systematic Desensitisation
Fear hierarchy:
List of situations from least -> most frightening
(e.g., picture of dog -> real dog)
Relaxation training
Berating, muscle relaxation, imagery
Gradual exposure
while relaxed
Move up hierarchy
Based on reciprocal inhibition
(cannot be scared and relaxed at the same time)
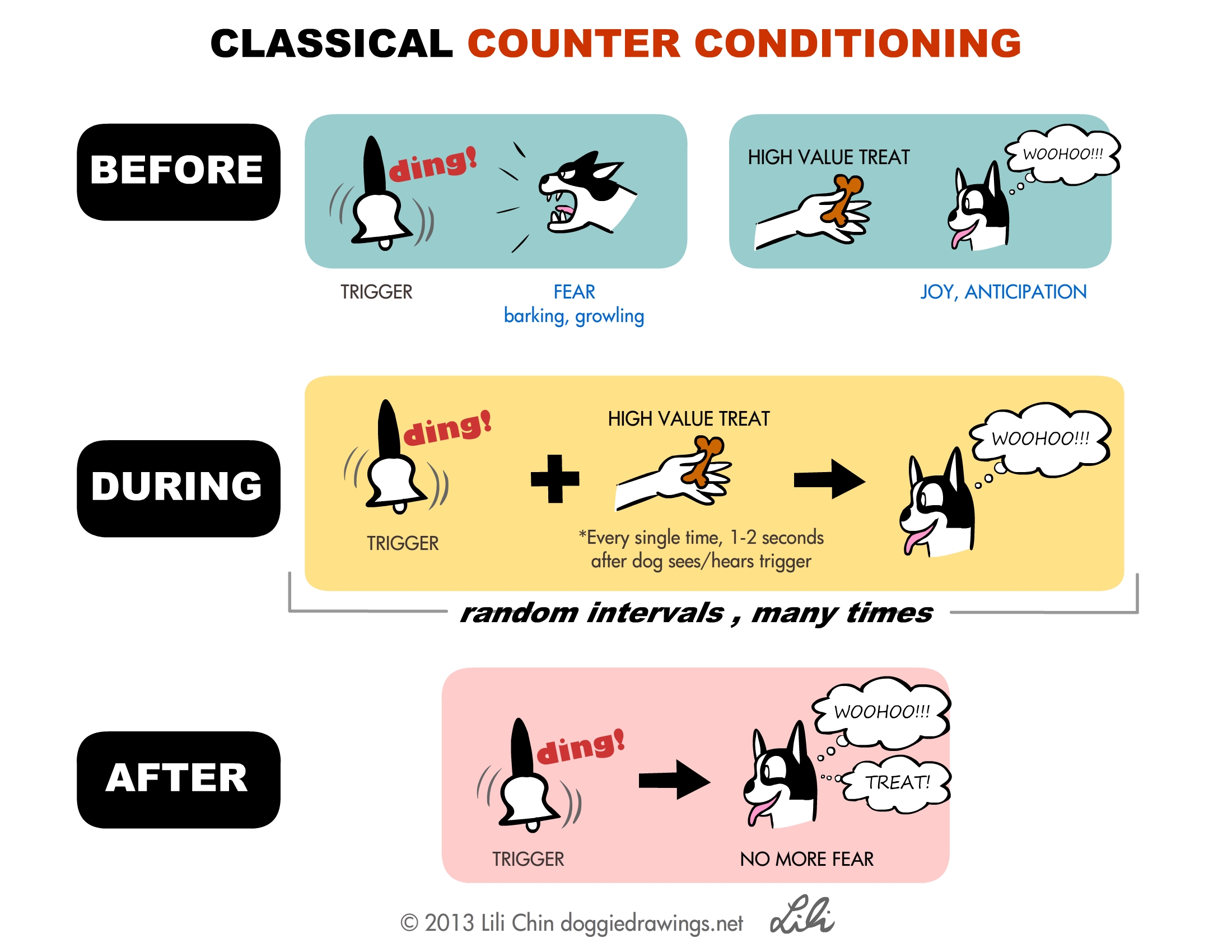
counter-conditioning
CS → fear (CR)
relaxation → calm
CS + relaxation → calm
CS become NS
evaluation on SD
Less effective for complex phobias: social phobias & agoraphobia often caused by irrational thinking, not just learning
Evolutionary phobias harder to treat: some fears may be biologically prepared
flooding
→ immediate, intense exposure to feared stimulus without gradual build-up
How it works:
Person cannot avoid the stimulus
Anxiety peaks -> eventually drops due to exhaustion
No negative reinforcement available
Anxiety decline -> new calm association formed
Extinction occurs (phobic response is unlearned)
evaluation on flooding
Highly traumatic: many patients drop out -> treatment may fail
Not suitable for complex phobias: social phobias need treatments for cognition, not just fear responses
Symptom substitution: removing the phobias may cause another symptom to appear (controversial)
Extension evaluation (issues & debates)
Behavioural approach is reductionist (ignores thinking, biology)
It assumes environmental determinism (no free will)
It uses a nomothetic approach (general laws), ignoring individual differences
Some phobias may have evolutionary advantages (preparedness)
cognitive approach to depression- Beck’s triad
Depression is caused by irrational and negative thinking.
Three types of negative thoughts (the negative triad) :
Negative view of self --> "I'm worthless"
Negative view of the world --> "everyone is against me"
Negative view of the future --> "things will never get better"
what’s a schema
Shema’s = mental "packages" of beliefs.
Depressed people have negative self-schemas, developed from early negative experiences (criticism, bullying)
examples of negative schema’s
Ineptness schema --> "I will fail"
Self-blame schema --> "everything is my fault"
Self-evaluation schema --> constant self-criticism
Cognitive biases
Depressed people distort situations by focusing only on the negatives.
Over-generalisation → making a broad negative conclusions from small events
Catastrophising → exaggerating problems and expecting disasters
absolutist thinking → using “everything” or “everyone” e.g. “everything will go bad if i get out of bed”
Ellis's ABC model (1962)
Depression comes from irrational beliefs, not events themselves:
A- Activating event: Something happens (e.g., friend ignores you)
B- Beliefs: Interpretation of the event:
Rational belief--> "they didn't see me"
Irrational belief--> "they hate me"
C- Consequence: Beliefs create emotional outcome:
Rational --> healthy emotion + coping
Irrational --> depression, anxiety, anger
Cognitive treatment: CBT
CBT is based on the idea that changing irrational thoughts reduces depression
Steps of CBT
Initial assessment --> identify problems
Goal setting
Identify and challenge irrational thoughts by using Beck’s negative triad: fore example, therapist might ask client to look for evidence for and against the thoughts, consider alternative, more realistic explanations
Homework (behavioural experiments)
Ellis REBT treatment
ABCD became ABCDEF:
D -Dispute → challenge irrational beliefs
Logical dispute → "does this belief make sense?"
Empirical dispute → "where is the evidence?"
Pragmatic dispute → “is is good that you're thinking this way"
E -effective beliefs → replace irrational thoughts with rational ones
F -feeling → the new feeling that replaced the old ones
Evaluation (explaining depression)- strength
Practical application → therapies led to CBT and REBT, both effective treatment
Supporting research:
Boury et al → depressed people show more negative thinking
Ates et al → negative thought statements increased depression symptoms
Evaluation (explaining depression)- weaknesses
Cannot explain the origin of irrational thoughts
Biological factors are ignored
Genes, neurotransmitters (e.g. serotonin) also play a role
Drug treatment help --> suggests depression is not purely cognitive
Irrational thoughts may be realistic: "depressive realism", depresses people may have more accurate views of the world
Evaluation (treatment)- strength
Very effective
March et al --> CBT as effective as antidepressants; combination best
No side effects, unlike medication
Evaluation (treatment)- weaknesses
Requires motivation: depressed patients may be too tired/unmotivated to engage
Overemphasises thinking: ignore real-life causes (abuse, poverty)
Success may be due to therapist-client relationship: not the technique themselves (Rosenzweig)
Issue & debates- depression
Nature + nurture --> irrational thinking may be automatic (nature). But can be changed (nurture)
Soft determinism --> we have some control to change thoughts
Scientific? --> uses scientific methods but cannot directly observe thinking