Clinical Chemistry: Carbohydrates Overview and Diabetes
1/214
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
215 Terms
What are the basic building blocks of carbohydrates?
Monosaccharides, which may contain three (trioses), four (tetroses), five (pentoses), or six (hexoses) or more carbon atoms.
Which monosaccharide is the main unit in the body?
Glucose.
What is fructose known for in carbohydrate metabolism?
Fructose skips the first step in glycolysis and, if it is the main source of energy, speeds up ATP production, shifting the body to produce more lipids.
What are disaccharides composed of?
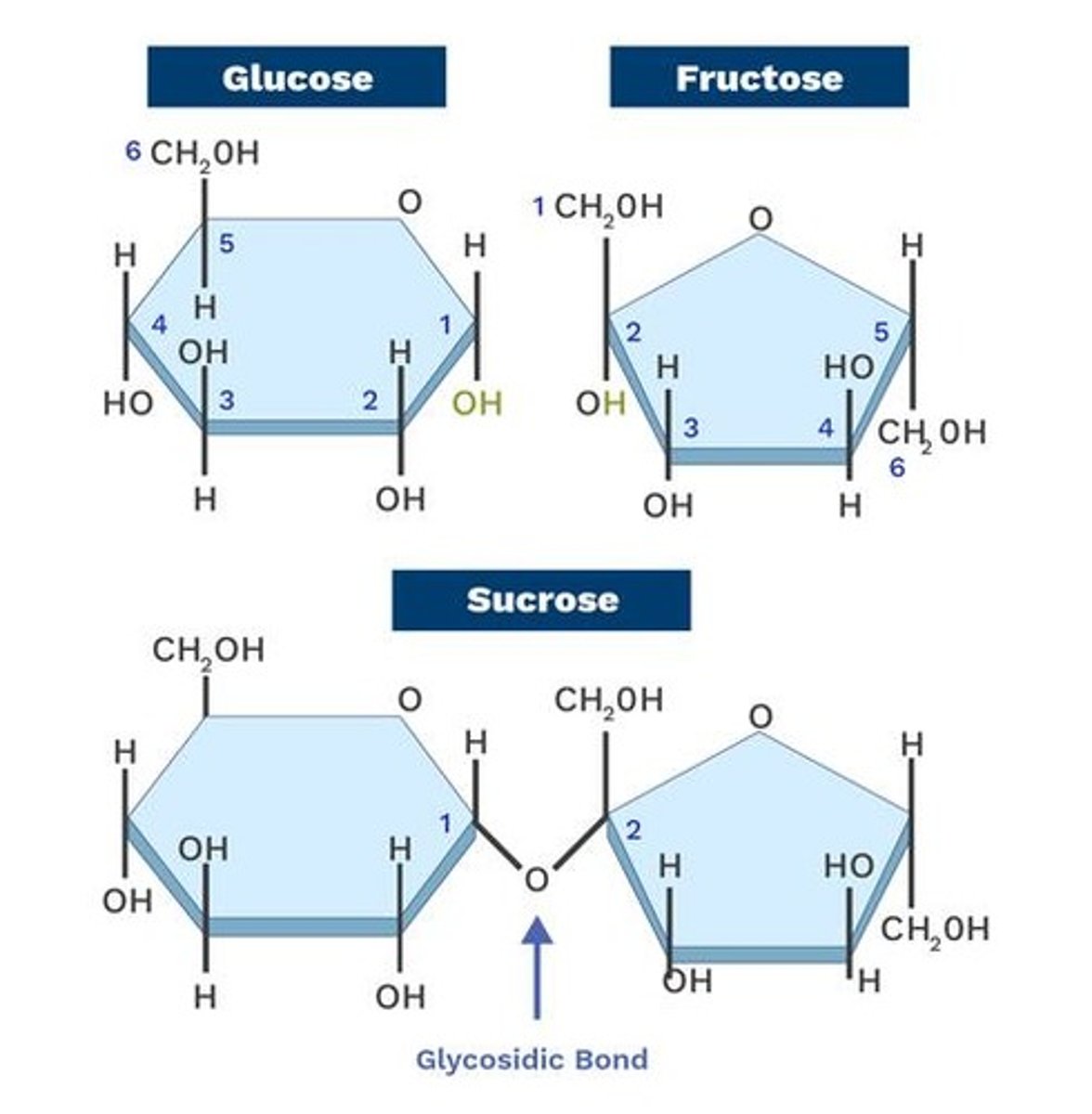
Two monosaccharide units joined by a glycosidic linkage.
What happens to disaccharides upon hydrolysis?
They are split into two monosaccharides by disaccharide enzymes.
Name three examples of disaccharides.
Maltose (2 glucose units), Lactose (1 glucose unit + 1 galactose unit), Sucrose (1 glucose unit + 1 fructose unit).
What is the main source of sugar in the Philippines?
Sugarcane.
What are oligosaccharides?
Polymers of carbohydrates composed of more than 2 sugar units (3 to 10).
Where are oligosaccharides commonly found?
In breastmilk, contributing to good bacterial growth in the GI tract.
What role do polysaccharides play in the body?
They provide energy and are essential for basic biochemical and metabolic processes.
What percentage of the diet should carbohydrates comprise for the Filipino diet?
Approximately 65%.
What is the general formula for carbohydrates?
Cx(H2O)y, indicating they are biochemical organic compounds containing carbon, hydrogen, and oxygen.
What is a common misconception about carbohydrates?
They are referred to as Hydrogenated Carbon, which is a misnomer since carbon cannot be hydrogenated.
What are the primary hormones regulating carbohydrate metabolism?
Insulin, Glucagon, Epinephrine, Cortisol, Growth Hormone, Adrenocorticotropic Hormone, Thyroxine, and Somatostatin.
What is hyperglycemia?
A condition characterized by an excessive amount of glucose in the blood, often associated with Diabetes Mellitus.
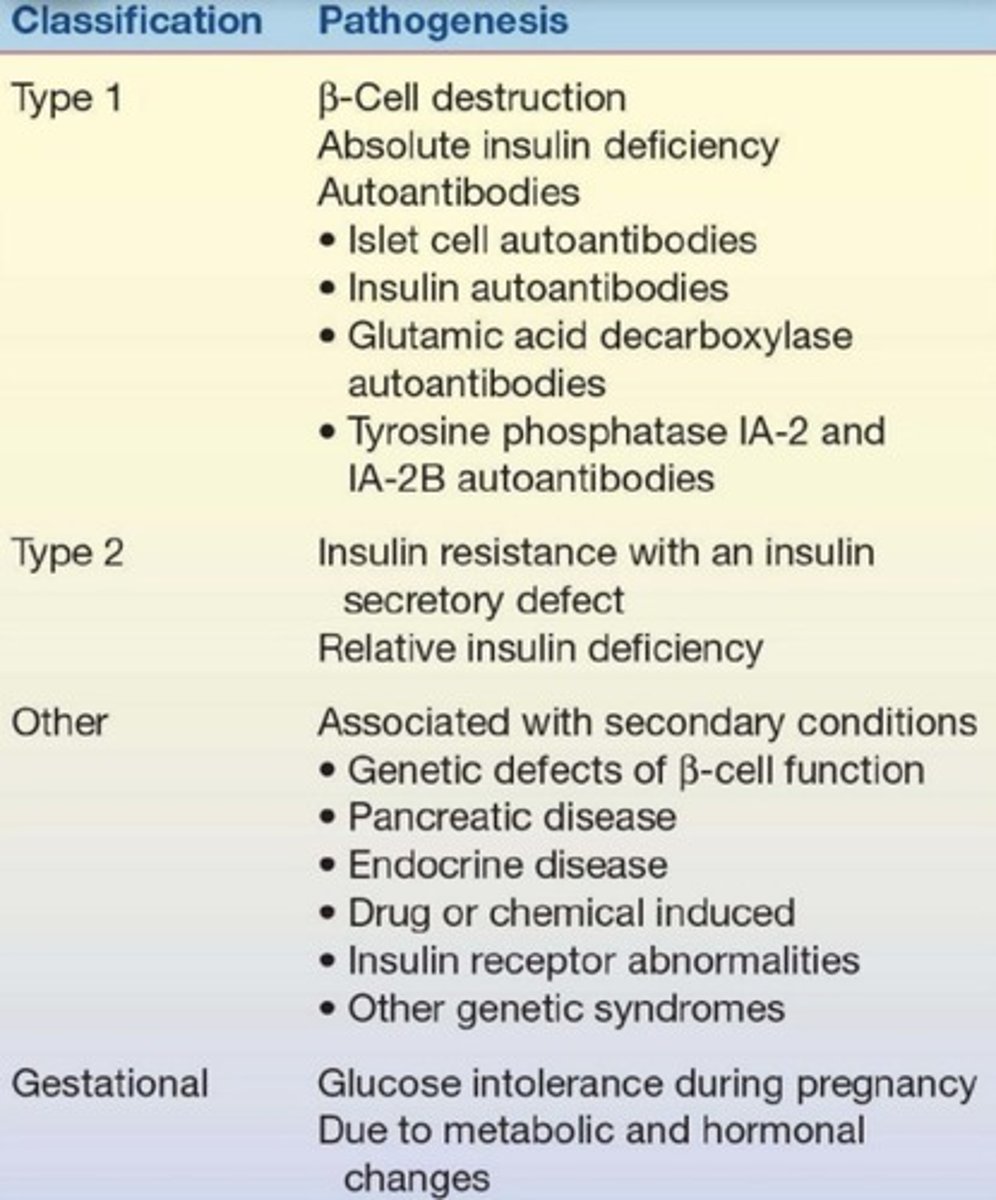
What are the types of Diabetes Mellitus mentioned?
Type I Diabetes Mellitus, Type 2 Diabetes Mellitus, and Gestational Diabetes Mellitus.
What is hypoglycemia?
A condition characterized by abnormally low levels of glucose in the blood.
What is the significance of carbohydrates in the human diet?
They are the primary and most preferred source of energy, especially for the brain.
What is the function of carbohydrates in food component storage?
Their structure allows them to efficiently bind with other carbohydrates to form macromolecules essential for energy storage.
What is the relationship between carbohydrates and energy production?
Carbohydrates are essential for energy production and metabolic processes in the body.
What is the role of insulin in carbohydrate metabolism?
Insulin helps regulate blood sugar levels by facilitating the uptake of glucose into cells.
What are polysaccharides and how are they formed?
Polysaccharides are formed by the linkage of many monosaccharide units through glycosidic bonds and yield more than 10 monosaccharides upon hydrolysis.
What is the most abundant form of carbohydrate in the diet?
Polysaccharides are the most abundant form of glucose-containing carbohydrate foods in the diet.
What are the primary functions of polysaccharides in the body?
Most polysaccharides serve as storage forms of carbohydrates.
Name three examples of polysaccharides and their sources.
1. Starch - found mainly in plants (e.g., rice). 2. Amylose - found in wheat. 3. Glycogen - found mainly in animals and humans, stored in muscles and liver.
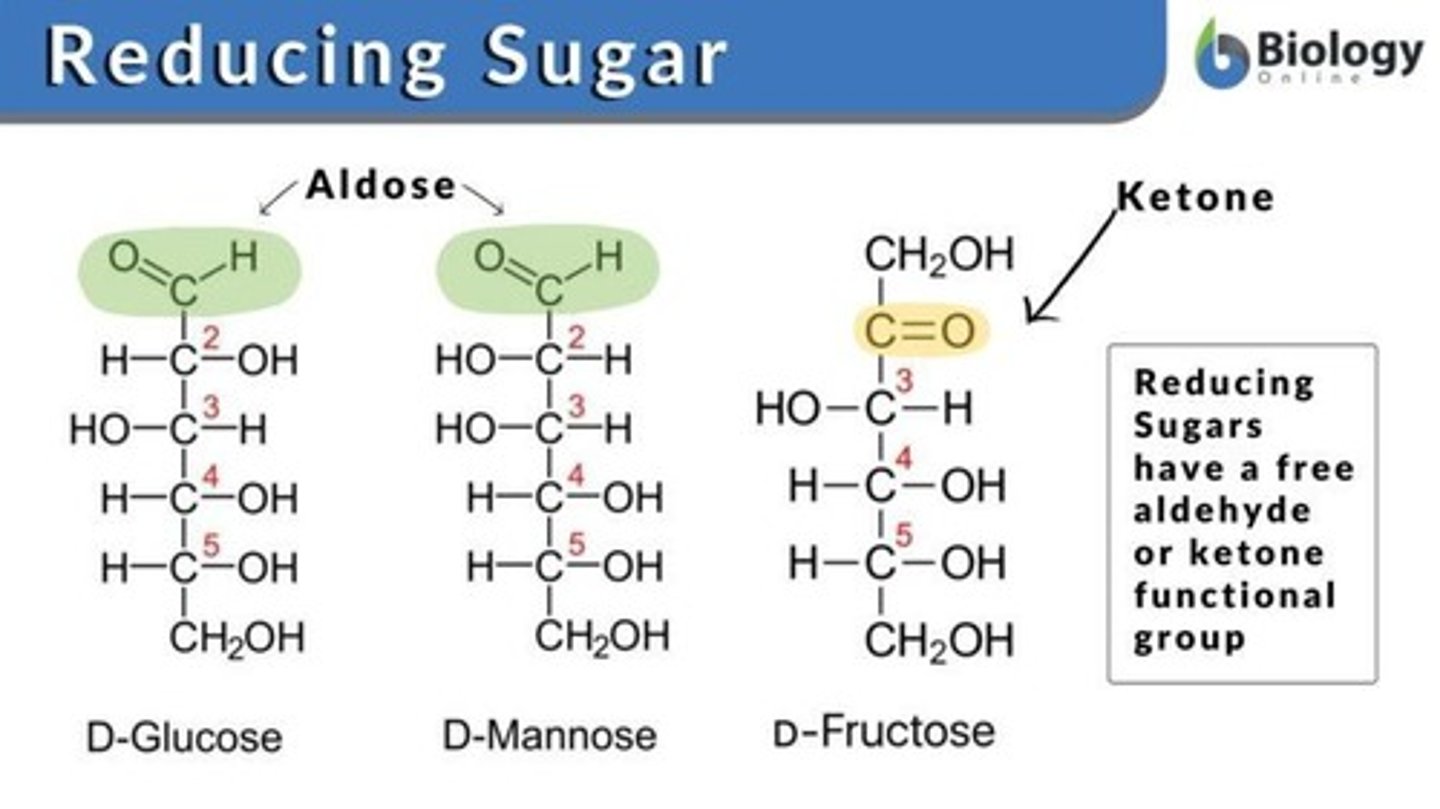
What are the two functional groups present in carbohydrates?
The two functional groups are carbonyl (C=O) and hydroxide (-OH).
How are carbohydrates classified?
Carbohydrates are classified based on four properties: size of the base carbon chain, location of the carbonyl functional group, number and type of sugar units, and stereochemistry of the compound.
What is a reducing agent in the context of carbohydrates?
A reducing agent is a compound that donates electrons, typically containing a free aldehyde or ketone functional group.
Which carbohydrates are examples of reducing sugars?
Examples of reducing sugars include maltose, fructose, lactose, and galactose.
What defines monosaccharides?
Monosaccharides are the simplest form of carbohydrates, consisting of one sugar unit/molecule and cannot be further hydrolyzed.
What are the two types of metabolic processes in carbohydrate metabolism?
The two types of metabolic processes are anabolism (build up) and catabolism (break down).
Which organs are involved in controlling blood sugar?
The liver and pancreas are primarily involved in controlling blood sugar levels.
What processes occur in the liver related to carbohydrate metabolism?
Glycolysis, glycogenolysis, glycogenesis, and gluconeogenesis occur in the liver.
What is the role of insulin in carbohydrate metabolism?
Insulin is the primary hormone responsible for the entry of glucose into cells and decreases plasma glucose levels.
How does insulin affect glucose metabolism?
Insulin increases glucose metabolism by promoting glycogenesis, lipogenesis, and glycolysis while inhibiting glycogenolysis.
What is glucagon and how does it function?
Glucagon is a hormone that raises blood glucose levels by promoting glycogenolysis and gluconeogenesis.
What happens to glycogen stores during a brief fast?
During a brief fast (<24 hours), glycogenolysis occurs, supplying glucose to the extracellular fluid from the liver.
What occurs when glycogen stores are depleted?
When glycogen is depleted, the body turns to other energy sources such as lipids and amino acids.
What is the significance of the anomeric carbon in glycosidic bonds?
The anomeric carbon is crucial in forming glycosidic bonds; if it bonds with another carbohydrate's hydroxyl group, it can result in a non-reducing sugar.
What is sucrose and why is it considered a non-reducing sugar?
Sucrose is composed of glucose and fructose linked by a glycosidic bond, making it a non-reducing sugar because it lacks a free aldehyde or ketone group.
Why is sucrose not measured in blood?
Sucrose is not measured in blood because it is digested before being absorbed, with glucose being the most common monosaccharide in blood.
What is the role of the pancreas in carbohydrate metabolism?
The pancreas produces insulin and glucagon, which regulate blood glucose levels.
What is the relationship between insulin and glucagon?
Insulin and glucagon have opposing actions; insulin lowers blood glucose levels while glucagon raises them.
What is the primary function of insulin in the body?
Insulin's primary function is to facilitate the entry of glucose into cells and regulate glucose levels.
What is the effect of prolonged fasting on carbohydrate metabolism?
During prolonged fasting (>1 day), gluconeogenesis occurs to produce glucose from non-carbohydrate sources.
What happens to the anomeric carbon when a bond is formed with another carbon on a carbohydrate?
The anomeric carbon remains unaltered, and the resulting compound remains a reducing substance with an active ketone or aldehyde group.
What is the primary hormone responsible for increasing glucose levels?
Glucagon.
Where is glucagon synthesized?
In the α-cells of the islets of Langerhans in the pancreas.
What triggers the release of glucagon?
A decrease in body glucose levels.
How does glucagon increase plasma glucose levels?
By promoting glycogenolysis in the liver and increasing gluconeogenesis.
When is glucagon released?
During stress (e.g., trauma, severe infection, bone injury) and fasting states.
What type of agent is glucagon?
A hyperglycemic agent.
What is epinephrine and where is it produced?
Epinephrine is a hormone produced by the adrenal medulla.
How does epinephrine affect plasma glucose levels?
It increases plasma glucose by inhibiting insulin secretion, increasing glycogenolysis, and promoting lipolysis.
When is epinephrine released?
During times of stress, particularly in fight or flight situations.
What is cortisol and where is it released from?
Cortisol is a stress hormone released from the adrenal cortex.
What stimulates the release of cortisol?
Stimulation by adrenocorticotropic hormone (ACTH).
What effects does cortisol have on plasma glucose levels?
It increases plasma glucose by increasing gluconeogenesis, liver glycogenolysis, and lipolysis.
What is Type 2 Diabetes Mellitus?
An acquired condition that can be due to chronic hyperglycemia from high carbohydrate intake.
What was Type 2 Diabetes Mellitus previously referred to as?
Non-insulin-dependent diabetes mellitus (NIDDM).
What is gestational diabetes mellitus (GDM)?
A type of diabetes caused by metabolic and hormonal changes during pregnancy.
When does gestational diabetes typically occur?
During the 2nd or 3rd trimester of pregnancy.
What is the recent classification of diabetes related to Alzheimer's disease?
Type 3 Diabetes Mellitus.
What role does ACTH play in glucose regulation?
ACTH stimulates the adrenal cortex to release cortisol, which increases plasma glucose.
What is thyroxine and how does it affect glucose levels?
Thyroxine is released from the thyroid gland and increases glycogenolysis, gluconeogenesis, and intestinal absorption of glucose.
What is somatostatin and what is its function?
Somatostatin is produced by the δ-cells of the islets of Langerhans and inhibits insulin, glucagon, growth hormone, and other endocrine hormones.
What is hyperglycemia?
A condition characterized by elevated levels of glucose in the blood.
What primarily causes the increase in plasma glucose levels in Type 1 Diabetes Mellitus?
An imbalance of hormones regulating glucose metabolism.
What is the role of insulin in glucose metabolism?
Insulin, produced by the β-cells of the pancreatic islets of Langerhans, enhances glucose availability and alters glucose metabolic pathways.
What happens to β-cells during prolonged hyperglycemia?
They become exhausted, leading to insufficient insulin production.
How can obesity affect insulin sensitivity?
Obesity can cause tissues to become insensitive to insulin, even if sufficient insulin is produced.
What is Diabetes Mellitus characterized by?
Inappropriate hyperglycemia due to pancreatic islet β-cell destruction and a tendency to ketoacidosis.
What is the result of cellular-mediated autoimmune destruction of β-cells?
An absolute deficiency of insulin secretion.
What is the upper limit of normal fasting plasma glucose?
110 mg/dL.
What percentage of diabetes cases does Type 1 Diabetes Mellitus constitute?
10%-20% of all diabetes cases.
What often initiates Type 1 Diabetes Mellitus?
An environmental factor or infection, usually a virus, in genetically predisposed individuals.
What are islet cell autoantibodies?
Markers found in 85%-90% of individuals with Type 1 Diabetes Mellitus, indicating autoimmune activity.
What distinguishes Idiopathic Type 1 Diabetes from other types?
It has no known etiology, is strongly inherited, and lacks β-cell autoimmunity.
What are the insulin requirements in Idiopathic Type 1 Diabetes?
Episodic requirements for insulin, unlike regular requirements in Type 1 DM.
What is a common complication of hyperosmolar coma?
Increased blood osmolarity can lead to neuron shrinkage, causing brain dysfunction, seizures, or death.
What are advanced glycosylated end products?
Products from excessive glucose that can alter vascular structures, leading to complications.
What is Impaired Fasting Glucose (IFG)?
An intermediate stage where fasting glucose is elevated but not at diabetes levels.
What characterizes Impaired Glucose Tolerance (IGT)?
Glucose tolerance values are above normal but below diabetes levels, often measured without fasting.
What is Gestational Diabetes Mellitus (GDM)?
Glucose intolerance that develops during pregnancy, usually normalizing 6-12 months after delivery.
What are common diagnostic criteria for diabetes?
Polydipsia (excessive thirst), polyphagia (excessive hunger), and polyuria (frequent urination).
What happens to the body when it fails to use glucose?
The body turns to fat as an energy source, leading to ketone body production and acidic blood.
What is the relationship between Type 1 Diabetes Mellitus and genetic predisposition?
Type 1 DM is genetically related, often with specific autoantibodies present.
What is the significance of ketone bodies in diabetes?
They are produced during fat metabolism when glucose is not utilized, contributing to acidosis.
What is the impact of chronic hyperglycemia on the body?
It can lead to macrovascular and microvascular complications due to vascular structure alterations.
What are the symptoms of high blood sugar and ketone bodies in diabetes mellitus?
Excessive urination, rapid weight loss, hyperventilation, mental confusion, and possible loss of consciousness.
How does insulin function in a healthy individual?
Insulin helps transport glucose into cells, where it is used for energy.
What happens to glucose in the bloodstream of a person with diabetes mellitus?
Due to abnormal insulin secretion or insensitivity, glucose remains in the bloodstream and cannot effectively enter the cells.
What alternative energy sources do cells use when they cannot access glucose in diabetes?
Cells use glycogen, lipids, or proteins as energy sources, leading to weight loss.
What is the relationship between excess glucose and urination in diabetes?
Excess glucose is excreted in the urine, leading to water loss and further weight loss.
What physiological response occurs due to acidic ketone bodies in diabetes?
The body increases ventilation rate to expel more carbon dioxide and relieve acidity from ketoacidosis.
What effect does high blood glucose have on brain function?
Increased glucose alters osmolarity, causing changes in cellular structure and potentially leading to mental confusion.
What are the microvascular complications associated with diabetes mellitus?
Nephropathy, neuropathy, retinopathy, and increased risk of heart disease.
What are some risk factors for developing Type 2 diabetes mellitus?
Physical inactivity, family history of diabetes, high-risk minority populations, history of gestational diabetes, hypertension, low HDL cholesterol, elevated triglycerides, and A1c ≥ 5.7%.
What is Acanthosis Nigricans and its relation to diabetes?
Acanthosis Nigricans is hyperpigmentation in body crevices due to insulin resistance, characterized by darkened areas around body folds.
What is the significance of a baby weighing more than 4.1 kg in relation to diabetes?
It may indicate maternal hyperglycemia due to excess glucose being transferred to the baby.