4/5- solute + water handling
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
47 Terms
what’s the most important contributor to the body’s extracellular fluid (ECF)
Na+
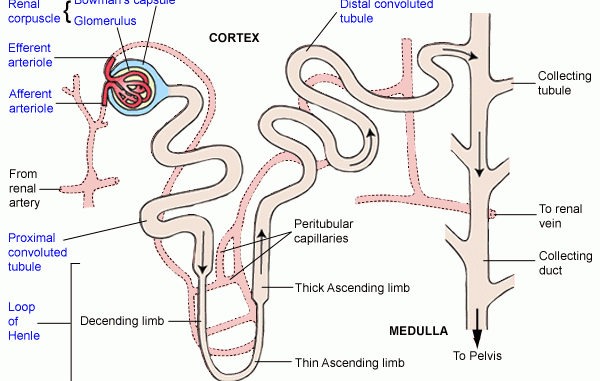
4 parts of the nephron that reabsorbs filtered Na+
proximal tubule: ~67%
thick ascending loop of Henle (TAL): ~25%
DCT + cortical collecting tubule: ~5%
medullary collecting duct: ~3%
Na+ reabsorption involves which 2 things
apical ENaC (epithelial Na+ channel)
basolateral Na-K pump
in the 1st ½ of proximal tubule, Na+ is reabsorbed w/
HCO3− + other solutes (e.g., glucose, amino acids, Pi, lactate)
in the 2nd ½ of proximal tubule, Na+ is reabsorbed w/
Cl-
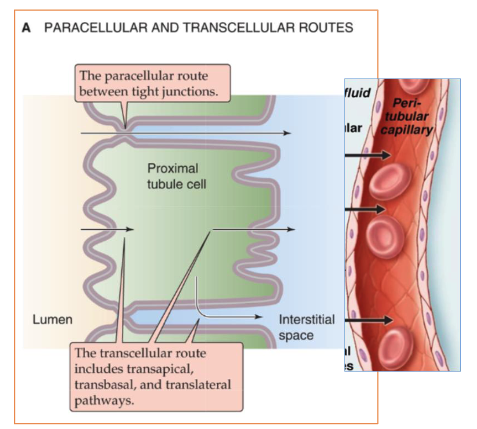
2 mechanisms the proximal tubule reabsorbs Na+ + Cl-
transcellular: crosses apical + basolateral membranes before entering blood
paracellular: move through tight junctions between cells
T/F: proximal tubule is permeable to water
true
what happens when the 1st ½ of the proximal tubule doesn’t work
Fanconi syndrome: renal disease from inability to reabsorb HCO3−, Pi, amino acids, glucose, low-molecular-weight proteins
2 drugs that target the proximal tubule
mannitol
carbonic anhydrase inhibitors (acetazolamide)
mannitol mechanism of action
osmotic diuretic that’s filtered into proximal tubular space where it increases tubular fluid osmolality → impaired reabsorption of fluid + increased excretion of water
carbonic anhydrase inhibitors (acetazolamide) mechanism of action
inhibits carbonic anhydrase, which normally facilitates HCO3- reabsorption
leads to metabolic acidosis
used to treat glaucoma
how is Na+ reabsorbed in the thick ascending loop of Henle (TAL)
Na/K/Cl cotransporter (NKCC2):
NHE3
T/F: TAL is permeable to water
false, it’s impermeable so it’s called the “diluting segment”
where can you find the most diluted urine in the nephron
end of TAL/tip of thin descending loop
how is Na+ reabsorbed in the DCT
Na/Cl cotransporter
T/F: DCT is permeable to water
false, it’s impermeable
how is Na+ reabsorbed in the cortical collecting tubules (CCT)
via principal cell: Na+ crosses the apical membrane of principal cell through epithelial Na channels (ENaC)
what can modulate # of open ENaCs
changing levels of aldosterone or AVP/ADH
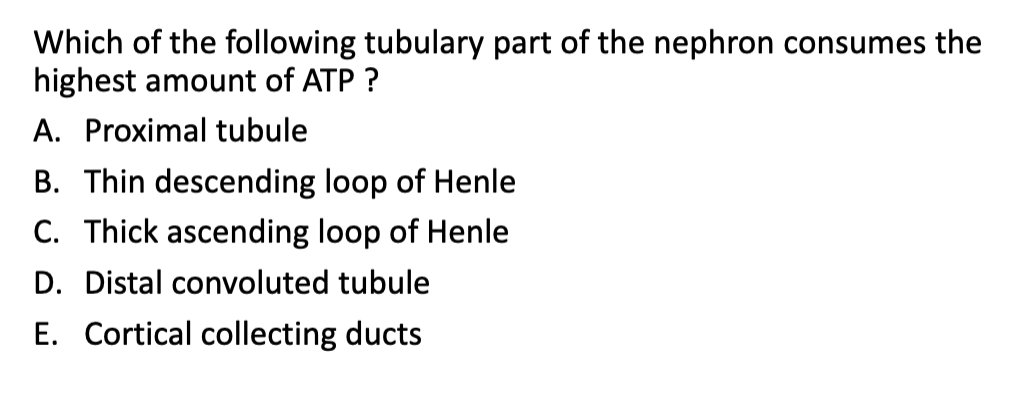
A. proximal tubule
kidneys have a high O2 consumption because
Na+ reabsorption is dependent on ATP-driven Na-K pump
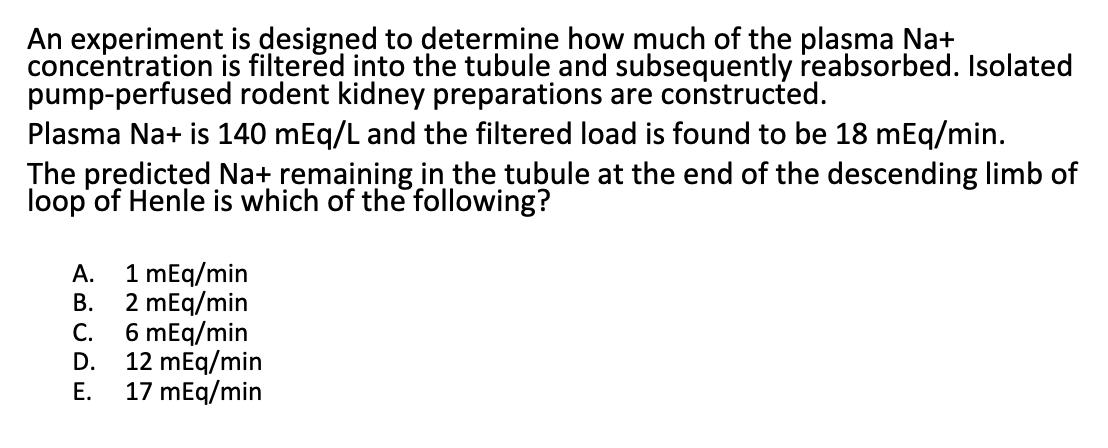
C because proximal tubule absorbs ~67% so multiply 0.67 w/ 18 mEg/min = 12 → 18-12 = 6 mEq/min

B because osmolality of Na does not change
when would the osmolality of Na change
osmotic diuresis: poorly permeable substances are present in the plasma + glomerular filtrate (ex: infusion of sucrose + mannitol, untreated diabetes mellitus)
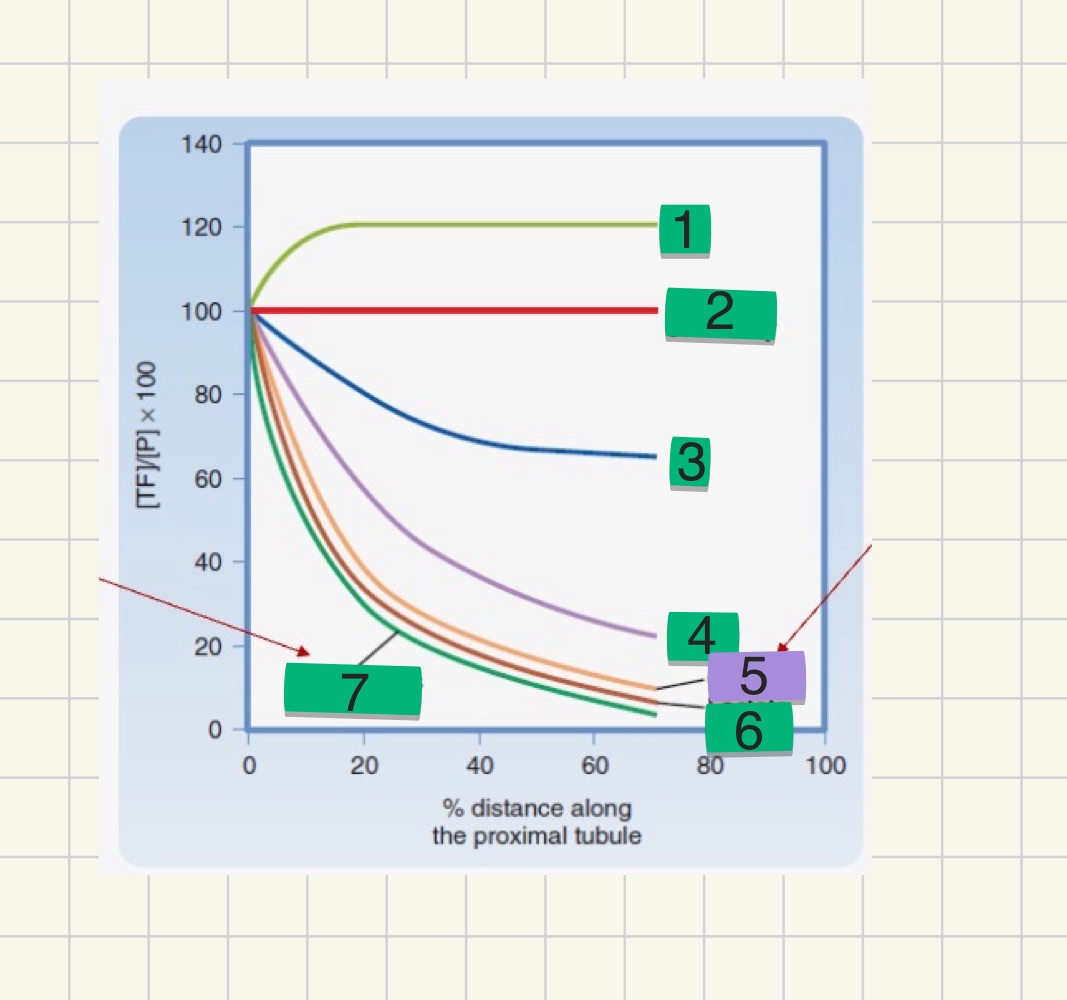
what are the numbers
Cl-
Na+ osmolality
Pi
HCO3-
glucose
lactate
amino acids
in the absence of AVP, _____ have relatively low water permeability
TAL + all downstream segments
3 things that increase Na+ reabsorption
renin-angiotension aldosterone
AVP/ADH
sympathetic activity
4 things that decrease Na+ reabsorption
ANP
prostaglandin
bradykinin
dopamine
what’s the glomerulotubular (GT) balance
causes fractional Na+ reabsorption by modulating rate of NaCl reabsorption in proximal tubule
what’s Bartter syndrome
autosomal recessive disease that inactivates the gene coding for Na/K/Cl symporter → decreased NaCl + K reabsorption → decreased ECFV, hypokalemia, metabolic alkalosis, hyperaldosteronism
which organ produces urea
liver, produces it from ammonia
kidneys regulate blood urea nitrogen (BUN) to what levels
7-18 mg/dL
what causes urea retention
renal disease → decreased GFR → urea retention + increased BUN
what happens to glucose in the nephron
proximal tubule reabsorbs almost all of filtered glucose via Na/glucose cotransporter (SGLT)
glucose should not be in urine (zero clearance) as long as blood glucose level is below
~180 mg/dL
rate of glucose reabsorption plateaus at what value
~400 mg/min → SGLT1 + SGLT2 cotransporters become saturated
what’s Hartnup disease
autosomal recessive disease → neutral + ring structured amino acids not absorbed + excreted through urine
what’s the safety mechanism when a protein is not reabsorbed
reabsorbed via clathrin coated endosomes
what’s urate + how much of it is reabsorbed
it’s the end product of purine catabolism + proximal tubule reabsorbs 90% of it
uricosurgic agents are used to
inhibit urate transporters to treat gout (elevated urate level)
luminal pH affects the clearance of what
weak acids: decreased luminal pH → reabsorption of neutral weak acids + secretion of neutral weak bases
how do we combat decreased luminal pH aka salicylate (aspirin) toxicity
alkalinizing urine w/ HCO3-
increasing urine flow w/ diuretics
T/F: some phosphate excretion occurs even at normal levels
true, therefore a small increase in phosphate level → significant acceleration of phosphate excretion
what’s the key promotor of phosphate excretion
parathyroid hormone (PTH), inhibits sodium/phosphate uptake
what’s the most important regulator of renal Ca2+ reabsorption
PTH + vitamin D stimulate calcium reabsorption
where in the nephron does PTH stimulate Ca2+ reabsorption
TAL + DCT
what drug is used to treat hypocalcemia (low calcium blood level)
loop diuretic, furosemide
Mg2+ behaves like which ion
Ca2+