Forum 1: reparing for your patient and subjective assessment
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
Primary Function of the Respiratory System
Supply the body tissues with oxygen
Dispose of carbon dioxide
What system is the airway innervated by?
The autonomic nervous system
Central centers in the brain stem
Inspiratory center (medulla)
Expiratory center (medulla)
Pneumotaxic center (pons)
Apneustic center (pons)
What does the nose contain?
Respiratory mucus- goblet cells
What does the Pharynx contain?
Nasopharynx (air)
Oropharynx (food and air)
Larynggopharyx (food and air)
bifurcates into larynx
and oesophagus
larynx protected by epiglottis
What does the Larynx contain?
vocal cords
What does the Trachea contain?
Trachea
anterior to the oesophagus
‘wind-pipe-
cartilaginous rings
right vs left bronchus
trachea bifurcates into left and right main bronchus = carina
right main bronchus - 20-30 degrees
left main bronchus - 45-55 degrees
how many divisions of airway in the human lung?
approx. 23 divisions
Lung Lobes
Right = 3 (upper, middle, lower)
Left = 2 (upper and lower)
Separated by fissures
right horizontal and oblique
left oblique
lung segments
10 right
8 left
anatomically and functionally separate unit of lung
own artery, vein and segmental bronchus
Pleura
Parietal Pleura- outer layer which connects to the chest wall
has nerve innervation (pleuritic pain)
Visceral Pleura- inner layer which covers the lungs
Pleural fluid
Allows pleura to slide during ventilation
negative pressure which counteracts the tendency of the lungs to recoil
clear, straw-like colour
produced and absorbed at a constant rate
if excess pleural fluid, there is decreased room for the lungs to expand
Principal muscles of respiration
Intercostals
Diaphragm
Diaphragm
Main muscle of inspiration
Separates thorax from abdomen
Large dome shaped muscle
Higher anteriorly
Sits 1-2cm higher on the right due to the liver
Intercostals
Pass between adjacent ribs
3 layers - external, internal and innermost
Accessory muscles of respiration (inspiration)
Scalenes (elevation of rib cage)
SCM (elevation of rib cage)
Pec major
Pec minor
Muscles of active expiration
Abdominal muscles
Internal intercostals
Openings of diaphragm
3 structures pass through:
Oesophagus
Aorta
Vena cava
Quiet breathing
Quiet breathing- expiration results from passive recoil of lungs
Active expiration
Internal intercostals - expect interchondral part
Abdominal muscles (depress lower ribs, compress abdominal contents)
Rectus abdominis
External oblique
Internal oblique
Transversus abdominis
What must happen to the thorax for respiration?
The dimensions must change
2 movements
pump handle
bucket handle
Pump Handle
Increasing anterior-posterior diameter
Elevation sternum and ribs 2-5 with inspiration
Bucket Handle
Increase transverse diameter of thorax
Anterior ends of ribs 8-10 move upwards and outwards
3 steps of gas exchange at the alveoli
oxygen inspired through conducting zone into respiratory zone of bronchial tree
alveolar gas contains a mixture of fresh gas and some expired CO2
oxygen moves across the alveolar-capillary membrane via diffusion
Diffusion is dependent on:
surface area of alveolar membrane
concentration / pressure gradient
gas solubility n
thickness of alveolar membrane
ventilation / perfusion coupling
3 functions of mucociliary clearance
to act as a mechanical barrier to trap organisms
is a chemical screen with anti-oxidant properties
biological barrier interacting with organisms and inflammatory cells
3 main components of mucociliary clearance
cilia
aqueous (sol) layer
viscous (gel) layer
Mucociliary clearance is affected by
Quantity of mucous (increased obstruction)
Viscosity of mucous (hyper-viscous secretions impede movements, airway dehydration- cilia unable to stretch into gel layer as bent over by weight of dehydrated muscous)
Cliliary beat frequency (impaired in diseases such as primary ciliary dyskinesia and immotile cilia syndrome)
Collateral ventilation
Provides an alternate route of ventilation when peripheral airways are obstructed
breathing
the process of moving air into and from the lungs to facilitate gas exchange
respiratory system requires all the following for effective gas exchange:
nose and mouth
trachea and airways
lungs including alveoli
respiratory muscles
blood vessels
biomechanical and physiological process
Airway structure and function
Trachea- C shaped rings
Branching Bronchi - semi-circular cartilaginous rings
Small airway
Small Airways
Lie interwoven with lung parenchyma
Have muscular walls
Are vulnerable to bronchial disorder (spasm, oedema, hypersecretion)
Repeated coughing can weaken airway walls
Become floppy/collapsible
Conducting Zone
Conducting airways brings gas to the respiratory zone
Begin at the nose all the way to terminal bronchioles
Respiratory Zone
Where gas exchange takes place
Respiratory bronchioles and alveoli
Anatomical dead space
The air left within the conducting zone each breath
Anatomical dead space
The air left within the conducting zone each breath
~150ml tidal volume
Alveolar dead space
Inspiratory gas reaching the alveoli but not participating in gas exchange due to insufficient blood supply
In health this is almost 0
Physiological dead space
Sum of all parts of tidal volume breath which does not participate in gas exchange (anatomical and alveolar dead space)
Atmospheric Pressure
Pressure exerted by gases in the air
Intra-Abdominal Pressure
Always positive
Generally higher-pressure system
Helps with core stability
Intra-Thoracic Pressure
Negative pressure during inhalation, positive during exhalation
Generally low-pressure system
Intrapulmonary Pressure
Pressure within the alveoli
Intrapleural Pressure
Pressure within the pleural cavity
Transpulmonary Pressure
The difference between the intrapulmonary and intrapleural pressures
Mechanics of Ventilation
Mechanical process that depends on volume changes within the thorax
VOLUME CHANGES —> PRESSURE CHANGES —→ GAS FLOW
Inspiration
Increase thoracic cage diameter and lung volume
Fall in intrapulmonary pressure so gas flows down pressure gradient
Air flow ceases when intrapulmonary pressure becomes equal to atmospheric pressure
Respiratory Compliance
Measure of stiffness/stretchiness of the lung
Lung Compliance
Distensibility of lung
Chest wall compliance
Distensibility of chest wall
respiratory compliance can be altered or influenced by disease
Respiratory disease- reduced total lung compliance is classified as restricted disease- patients have difficulty breathing in
leads to:
increased respiratory load- increased work of breathing
accessory muscle use
Reduced respiratory compliance
makes the generation of larger pressures necessary to change volume
low lung volumes (atelectasis, post surgery, prolonged recumbency in supine)
high lung volumes (hyperinflation, aging)
reduced pulmonary surfactant
pulmonary oedema
consolidation
interstitial fibrosis
pleural effusion
Reduced chest wall compliance
Lungs are normal but inspiration reduced to chest wall compliance
thoracic deformity (kyphosis, scoliosis, sternal deformity)
circumferential thoracic burn
obesity
supine position
raised intra-abdominal pressure (abdominal distension, post-surgery, pregnancy)
aging
Ventilation
Air which reaches the lungs
Distribution of ventilation will be influenced by part of lung, position of patient airflow resistance
occurs optimally in lower 1/3 of lung- partially expanded but large capacity for volume change
Diffusion
Transfer of gases across alveolar-capillary membrane
Perfusion (Q)
Blood flow available to participate in gas exchange
Distribution of perfusion
increases down the healthy upright lung
Ventilation- Perfusion
Vital to maintain VQ matching to achieve adequate gas exchange
In the presence of respiratory disease, autoregulatory mechanisms employed:
Hypoxic pulmonary vasoconstriction
if low PaO2 then arterioles constrict to redistribute blood flow
Chronic in COPD - lead to heart failure
Pulmonary capillary recruitment
If good ventilation, additional arterioles recruited to optimise VQ matching
Oxygen Transport
Immediately bound to haemoglobin (Hb) (98%)
Physically dissolved in the plasma (2%)
Carbon Dioxide Transport
Carried in blood entirely as solution - mostly bicarbonate
oxygen dissociation curve
relationship between partial pressure of O2 (either alveoli or tissues) and the degree to which Hb is saturated with O2
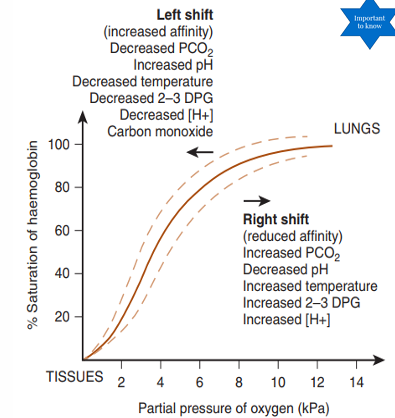
Factors which shift the curve
All of the following shift the curve to the R and down
decreased pH
increase in PCO2
increased temp.
increased 2,3-diphosphoglcerate (DPG) (by product of glycolysis, increased in pregnancy)
A shift to the right reduces oxygen’s affinity for Hb (to allow delivery to tissues)
Haldane Effect
In the presence of hypoxaemia, CO2 bind to Hb to be transported back to the lung
Bohr Effect
Shift to the right of oxygen equilibrium curve caused by a drop in pH, reducing the Hb’s affinity for O2
Allows for better oxygen unloading in metabolically active peripheral tissues like skeletal muscle during exercise. Increased skeletal muscle activity causes localized increases in carbon dioxide partial pressure, which lowers the local blood pH.
Goals of a respiratory assessment
Establishing the patient’s main problems at presentation
Identifying any relevant co-morbidities
Identifying precautions or contraindications to treatment
Formulating a treatment plan
Identifying outcome measures that can be used to determine effectiveness/responses to treatment
Identifying patients for whom treatment will not be beneficial
Sources of information
the medical chart (blood tests, chest x-rays, pulmonary function tests, arterial blood gas analysis)
observation charts- particularly for vital signs, medications, and clinical pathways
medical and nursing staff involved
the patient and/or their family/carers
Content gathered from inpatient chart
history of presenting condition (HPC)
past medical history
investigations
blood
scans
current condition
attachments
other allied health input
HAIDET
A way to remember meeting a pt the first time
Hand Hygiene
Acknowledge
Introduce
Duration
Explanation
Thank you
Subjective Assessment- Purpose
Confirm or elaborate on information gained from chart
Establish rapport with patient
May lessen anxiety
Respiratory Assessment
Shortness of breath
Wheeze
Cough
Sputum
Smoking History
SOB Questions
Do you feel short of breath?
At rest or with exertion?
What activities make you short of breath?
How long to recover?
Wheeze Questions
Do you experience a wheeze?
What provokes it?
What relieves it?
Cough Questions
Have you been coughing?
Is this usual for you or different? (current vs. usual for patient)
Productive or non-productive?
Any difficulties clearing your sputum?
When and how often?
Sputum Questions
Have you been producing any sputum? (current vs usual for patient)
Volume? Colour? Consistency? Haemoptysis?
Smoking history Questions
How much?
For how long?
Respiratory Subjective- pre-existing respiratory conditions
How do they usually manage it?
physio? meds?
Frequency of exacerbations
how are they managed?
do they have an action plan?
Other current status questions
what have they done today
Functional history
exercise
social history
medication
tests
Clinical Reasoning Example Form
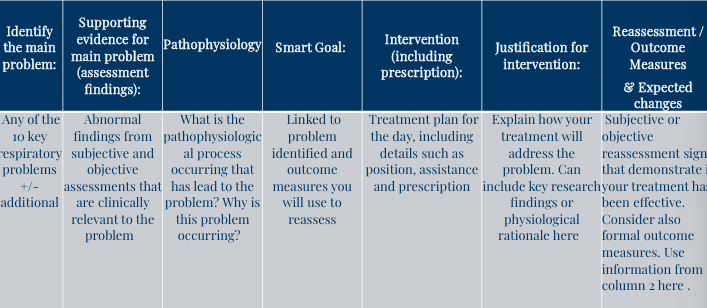
Clinical Reasoning Process
Identify significant information from subjective and objective assessment
Combine with knowledge of normal anatomy and physiology and knowledge of pathophysiology and clinical manifestations and clinical course/prognosis of disease
Put puzzle pieces together to identify the key problems amenable to physiotherapy
Utilise knowledge of evidence based interventions to best address the identified key problem for that individual
Clinical Reasoning step 1
Identify significant information from subjective and objective assessment
Clinical Reasoning step 2
Combine with knowledge of normal anatomy and physiology and knowledge of pathophysiology and clinical manifestations and clinical course/prognosis of disease
Clinical Reasoning step 3
Put puzzle pieces together to identify the key problems amenable to physiotherapy
Clinical Reasoning step 4
Utilise knowledge of evidence based interventions to best address the identified key problem for that individual