Foundations of Health/Self Care & PPCP, Pathophysiology of Heartburn, and Heartburn
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
59 Terms
Self-care is defined as the "independent act of __________, __________, and ________ one’s illnesses with or without seeking professional advice”
preventing, diagnosing, and treating
Seven Pillars of Self-Care
1.) Knowledge and Health Literacy
2.) Mental well-being and self-awareness
3.) Physical Activity
4.) Healthy Eating
5.) Risk Avoidance
6.) Good Hygiene
7.) Rational Use of Products and Services
The basic function of the GI tract is to take in foods, process them into nutrients that can be used by the body, and eliminate wastes. This function depends on the following physiological processes.
- Secretion
- Motility
- Digestion
- Absorption
- Defense & Immunity
Motility is the coordinated GI __________________ that moves the content from the mouth to the anus.
smooth muscle contraction and relaxation
Digestion is the physical and chemical process of ___________________ that can be absorbed by cells of the __________________.
converting nutrients in foods to products, mucosa
Absorption is the process of _____________________ (amino acids, small peptides, monosaccharides, fatty acids) into the body.
transporting the products of digestion
The GI tract wall has four functional layers:
1.) Mucosa
2.) Submucosa
3.) Muscularis
4.) Serosa
Gastric secretion from gastric glands in the wall of the stomach and surface mucous cells contains the following:
- hydrochloric acid
- intrinsic factor
- pepsinogen and lipase
- mucus and bicarbonate
Hydrochloric acid is secreted from _________________ for ________________. Hydrochloric acid is pumped into the stomach lumen by ____________________
parietal cells for food sterilization and dietary protein hydrolysis
H+, K+-ATPase (a proton pump).
Parietal cells secrete _________________________
hydrochloric acid and intrinsic factor
Intrinsic factor is secreted from _______________________
parietal cells for the later absorption of vitamin B12.
Pepsinogen and lipase are secreted from ______________________
chief cells for initiating protein and fat digestion.
Mucus and bicarbonate are secreted from ________________________ to ______________________
mucous cells to protect the stomach from self-digesting
Gastric secretion can be stimulated during two phases:
the cephalic phase (before foods enter the stomach) and the gastric phase (after foods enter the stomach).
The Cephalic Phase is triggered by vagal input before food reaches the stomach. ________________________ stimulate G cells to release gastrin, promoting secretion. Gastrin release is inhibited by ___________________.
Gastrin-releasing peptide (GRP) and acetylcholine
somatostatin (SST) when acidity is high
The Gastric Phase is triggered by food in the stomach. ________________________ activate G cells, and reduced acidity inhibits _____________________ release, promoting gastrin-mediated secretion.
Stretch receptors, somatostatin (SST)
Acid-peptic disorders include ____________________
- gastroesophageal reflux disease (GERD)
- peptic ulcer disease (PUD)
- stress-related mucosal injury
Peptic ulcer disease is caused by __________________, and can therefore be treated with _____________________
H. pylori, antibiotics
GERD occurs due to the _______________________, leading to injuries. Frequent heartburn leads to GERD.
reflux of gastric acid and pepsin into the esophagus
Symptoms of GERD include __________________ and is common in the ________________________
heartburn
elderly, smokers, obese individuals, and during pregnancy.
Risk factors for GERD include
Obesity, pregnancy, alcohol, caffeine, and certain medications (e.g., antihistamines, painkillers).
pharmacologic therapy for heartburn and dyspepsia / medications that can reduce intra-gastric acidity include:
- Antacids
- Histamine Type 2 Receptor Antagonists (H2RAs)
- Proton pump inhibitors (PPIs)
Heartburn is a.k.a. _______________________
acid regurgitation, sour stomach, bitter belching
Clinical Presentation of Heartburn
- Burning sensation in the stomach or lower chest that extends up
- Reflux (bitter acidic fluid in the back of the throat)
- Less common: burping, hiccups, nausea, and vomiting
- Symptoms occur within ~1 hour of eating/drinking
Clinical Presentation of Dyspepsia (indigestion)
- Early satiation (the feeling of fullness after eating a small amount of food)
- Epigastric pain/burning
- Other symptoms: bloating, nausea, vomiting, or belching (burping)
Complications of Untreated GERD
- Erosive esophagitis/ulcers
- Esophageal stricture (build-up of collagen that narrows the esophageal lumen)
- Esophageal cancer
- Barrett's esophagus (epithelial changes that indicate chronic heartburn and is a risk factor for strictures and cancer)
a myocardial infarction (heart attack) is the blockage of coronary ______________________, resulting in muscle death
Chest pain/discomfort ("squeezing, tightness, pressure, constriction, crushing, or heavy weight on chest") that has a gradual onset that comes and goes, is called __________________
arteries, which supply oxygen to the heart muscles
angina
Blockage of coronary arteries (supply ________ to ___________), resulting in ______________
oxygen, heart muscles, muscle death
When assessing a patient with heartburn or dyspepsia, these are the alarm symptoms to look out for, in which urgent diagnosis is required
- Unexplained weight loss
- Dysphagia (difficulty swallowing)
- Odynophagia (painful swallowing)
- Vomiting
- GI bleeding (vomiting blood or black tarry stools)
When assessing a patient with heartburn or dyspepsia, these are the atypical symptoms to look out for, in which urgent diagnosis is required
- chronic hoarseness, wheezing, coughing
- nocturnal heartburn
symptoms of a heart attack include
chest pain with sweating, radiating pain to one/both arms, and shortness of breath
Exclusions for self-treatment of heartburn and dyspepsia in which medical referral/higher-level care is required
- alarm/atypical symptoms
- heart attack symptoms
- frequent heartburn for more than 3 months
- infectious cause (continuous nausea, vomiting, or diarrhea)
- severe heartburn/dyspepsia
- heartburn/dyspepsia that continues after 2 weeks of treatment with nonprescription H2RA or PPI
- adults over the age of 45 years with new-onset dyspepsia
age restrictions for the use of certain medications for heartburn and dyspepsia
- Children under 2 years should not use antacids
- Children under 12 years should not use H2 receptor antagonists (H2RAs)
- Children under 18 years should not use proton pump inhibitors (PPIs)
Non-pharmacologic therapy for heartburn and dyspepsia
- Weight loss (if obesity or recent weight gain is present, 10% of body weight loss is meaningful)
- Avoid eating within 2-3 hours of bedtime (empty stomach)
- Avoid lying down after eating
- Sleeping on the left side with the head elevated by 6-8 inches
- Smoking cessation
- Avoiding "trigger" foods/drinks
- Discussing potential causative medications with prescribers (consider discontinuation)
ingredients, indications, and MOA of antacids
Ingredients: sodium bicarbonate, calcium bicarbonate, magnesium (hydroxide, carbonate, or trisilicate), or aluminum (hydroxide or phosphate)
Indications: heartburn, GERD, calcium supplementation (calcium-containing)
MOA: directly neutralizes gastric acid in the stomach
efficacy, onset, and duration of antacids
- Efficacy: determined by acid-neutralizing capacity (ANC); may repeat the dose in 1-2 hours, but not more than products-specific daily limits
- Onset: <5 minutes
- Duration: 20-60 min (empty stomach), 1-3 hours (after a meal)
Safety concern of antacids
Patients who are frequently using calcium-containing antacids will need to monitor their calcium levels, especially those with renal impairment
Safety concern for patients with renal impairment
- Avoid magnesium containing products (levels may build up)
- Monitor for calcium, phosphate, or aluminum toxicity in severe disease
Tolerability / side effects of antacids
- well tolerated
- Magnesium-containing antacids can cause diarrhea
- Aluminum-containing antacids can cause constipation
- Calcium carbonate-containing antacids can cause CO2 production (gas) and constipation
Drug Interactions with antacids
- Metal cations can bind to certain medications (chelation)
- Enteric-coated medications that need a lower pH will have reduced absorption due to increased gastric pH by the antacid.
Key counseling points of antacids
- when to take them (as soon as symptoms start !)
- awareness of drug interactions with current prescriptions or supplements
- choosing a formulation: chewable tablets or gummies, dissolvable tablets, liquid
ingredients, indications, and MOA of Histamine Type 2 Receptor Antagonists (H2RAs)
Ingredients: famotidine, ranitidine, cimetidine, etc.
Indications: GERD, peptic ulcer disease, hypersecretory conditions
MOA: competitively inhibits histamine at H2 receptors, which inhibits stimulation of H+ secretion from gastric parietal cell H+/K+ATPase pumps
efficacy, onset, and duration of Histamine Type 2 Receptor Antagonists (H2RAs)
Efficacy: can reduce stomach acid by about 70%; however with repeated dosing within 3 days, tachyphylaxis can occur (rapidly diminishing response to successive doses of a drug)
Onset: 15-45 minutes
Duration: 4-12 hours
Safety concern of Histamine Type 2 Receptor Antagonists (H2RAs)
- can cause thrombocytopenia (low platelet levels in the blood)
- dose is adjusted by prescriber for patients with chronic kidney disease (CKD)
Tolerability / side effects of Histamine Type 2 Receptor Antagonists (H2RAs)
- well tolerated
- Mild headache, fatigue, dizziness, and constipation/diarrhea
Drug interactions with Histamine Type 2 Receptor Antagonists (H2RAs)
- Cimetidine inhibits CYP enzymes significantly more than other H2RAs
- Slight increase in blood alcohol concentration when taken with alcohol
Key counseling points of Histamine Type 2 Receptor Antagonists (H2RAs)
it is most effective to take about 30 minutes before a meal where the patient is anticipating to get heartburn symptoms, or as needed (up to twice daily) when symptoms arise
ingredients, indications, and MOA of Proton Pump Inhibitors (PPIs)
Ingredients: omeprazole, esomeprazole, lansoprazole
Indications: GERD, H. pylori eradication, peptic ulcer disease treatment and prevention, stress ulcer prophylaxis
MOA: Absorbed into stomach parietal cells as a prodrug, then activated in acid secretory channels, then binds to H+/K+ATPase pumps, irreversibly inactivating acid secretion until new pumps are created
efficacy, onset, and duration of Proton Pump Inhibitors (PPIs)
Efficacy: Best absorbed on an empty stomach, since there will be more H+/K+ATPase pumps available at that time
Onset: 1-3 hours, complete relief in 1-5 days
Duration: 24 hours
safety concern of Proton Pump Inhibitors (PPIs)
- Enteric infections, vitamin B12 deficiency, hypomagnesemia, and reduced calcium absorption/decreased bone mineral density
Tolerability / side effects of Proton Pump Inhibitors (PPIs)
- well tolerated
- may cause headache, diarrhea, nausea, and abdominal pain
Drug interactions with Proton Pump Inhibitors (PPIs)
May inhibit CYP450 enzymes, which metabolize other drugs for clearance
Key counseling points of Proton Pump Inhibitors (PPIs)
- take on an empty stomach 30 minutes before breakfast
- Delayed release tablets (or pellets in capsules) should not be crushed/chewed/split
- With chronic use, rebound acid secretion can occur for a few days
- should only be used for 2 weeks once every 4 months. May be used longer or more frequently with supervision by your medical provider
Antacids, H2RAs, and PPIs all increase
gastric pH
Medications that are risk factors for heartburn/GERD and dyspepsia
- Calcium channel blockers
- Iron
- NSAIDs
- Oral contraceptives
Medications that are risk factors just for heartburn/GERD
- anticholinergics
- potassium
Medications that are risk factors just for dyspepsia
- antibiotics
- opioids
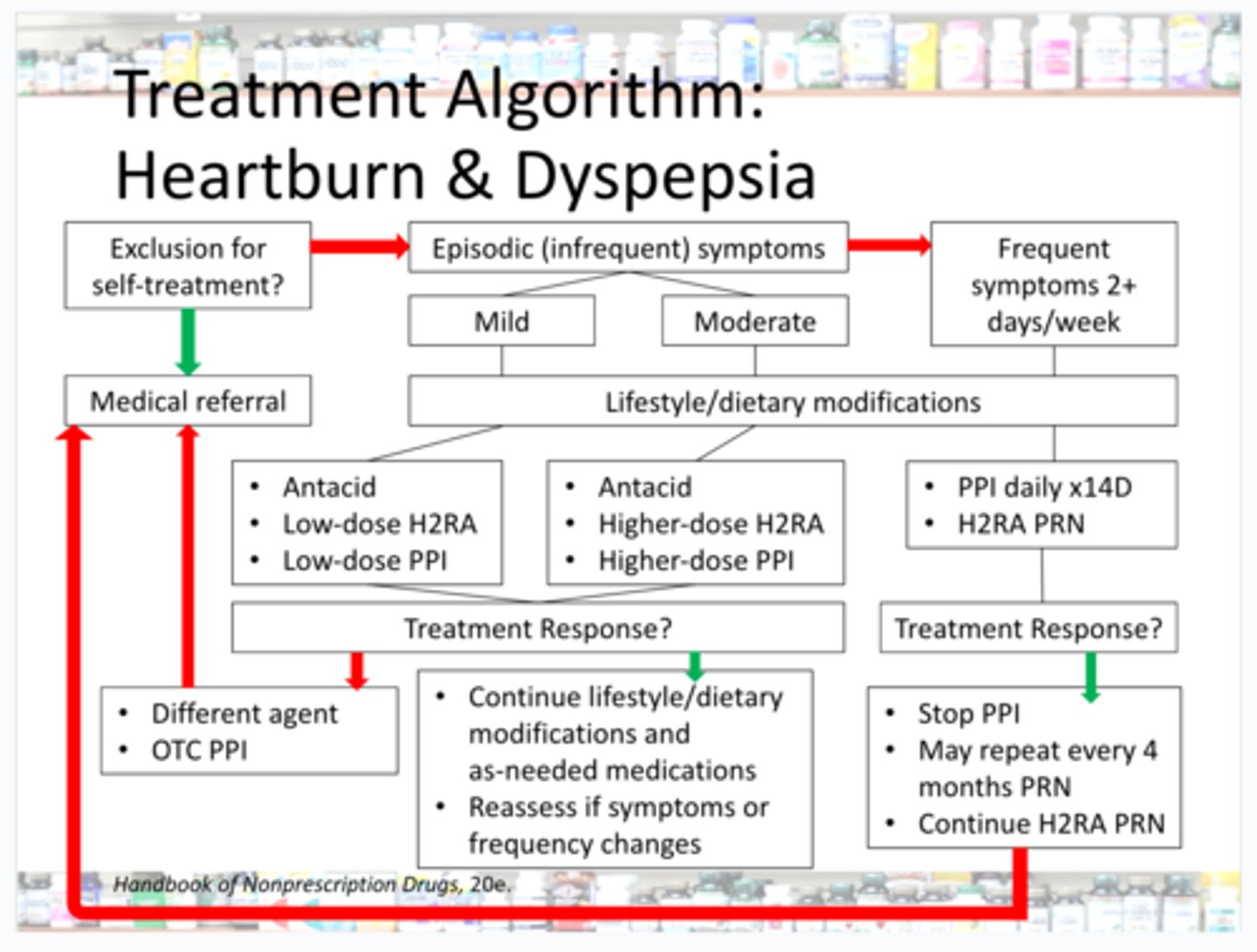
Treatment Algorithm: Heartburn & Dyspepsia
Examples of brand name drugs that are antacids, H2RAs, and PPIs
Antacids = Tums®
H2RAs = Zantac 360®, Pepcid®
PPIs = Prilosec®