AUBF - Semen Analysis
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
Azoospermia
Absence of Spermatozoa in Semen or Seminal Fluid.
Aspermia
No semen.
Spermatid
Immature/Young Sperm Cells.
Necrospermia
Presence of dead sperm cells.
Oligospermia
Decreased number of sperm.
Asthenozoospermia
Low percentage of progressively motile spermatozoa/sperm cells.
Or may imply a high percentage of either:
Non-progressively motile sperm (e.g., moving in circles or twitching)
Non-motile sperm (no movement at all)
Or both
Teratozoospermia
Low percentage of morphologically normal sperm.
C. Both are True
Seminal Fluid or Semen is a composite solution formed by testes as well as other male reproductive organs.
It consists basically of spermatozoa suspended in seminal plasma.
a. First Statement is True. Second Statement is False.
b. First Statement is False. Second Statement is True.
c. Both are true.
d. Both are false.
Testis → Epididymis → Vas Deferens → Seminal Vesicle → Ejaculatory Duct → Prostate Gland → Bulbourethral Gland → Urethra
Flow of Semen
Testes
Responsible for producing sperm cells, and secreting testosterone. It is also the site of spermatogenesis in the seminiferous tubules. Most important component of the seminal fluid.
Epididymis
It is the site of maturation of sperm, where sperm cells become motile.
Vas Deferens
This propels sperm to the ejaculatory duct.
Seminal Vesicle
A convoluted, pouch-like, that also acts as the transport medium for the sperm and produces an alkaline (7.2 - 8 pH) viscous fluid. This also contains the seminal plasma. This provides nutrients for sperm (fructose) and also contains clotting proteins.
Prostate Gland
A Golf-Ball-Like that produces a slightly acidic fluid (6.5). It contains enzymes that can break down clotting proteins, liquefying semen.
Bulbourethral Gland or Cowper’s Gland
Pea-size part of the male reproductive system that produces a thick alkaline fluid to neutralize the vaginal acidity present in vaginal flora and protects the passing of sperm by neutralizing the acid from urine and prostate gland in the urethra. It also secretes mucus that lubricates the penis and the lining of the urethra.
Testes - 5%
Seminal Vesicle - 60% to 70%
Prostate Gland - 20% to 30%
Bulbourethral Gland - 5%
Four Fractions of Seminal Fluid
Sperm Cells and Prostatic Fluid.
Components of the First Portion of the Ejaculate.
Mostly Seminal Vesicle Fluid
Components of the Second/Last Portion of the Ejaculate.
Sperm Count - Decreased
pH - Falsely Increased (Alkaline)
Specimen - Will not liquefy
Effects of Missed First Portion of the Ejaculate.
Semen Volume - Decreased
Sperm Count - Falsely Increased
pH - Falsely Decreased (Acidic)
Specimen - Will Not Clot
Effects of Missed Last Portion of the Ejaculate.
Seminal Vesicle - Alkaline
Prostate Gland - Acidic
Bulbourethral Gland - Alkaline
pH of Seminal Vesicle, Prostate Gland, and Bulbourethral Gland
Varicocele
This is the most common cause of infertility for male. It is formed when valves inside the veins along the spermatic cord prevent blood from flowing properly, causing the swelling and widening of the veins (hardening of veins that drain the testes). And one of the signs in semen analysis for this is the tapering of the head of the sperm cells.
Mumps or Beke
This one cause infertility around 40% of the time/cases.
Varicocele
Mumps
Klinefelter’s Syndrome (XXY)
Malignancy
4 Causes of Infertility
Spermatogenesis
This term means the formation and development of sperm in the seminiferous tubules of the testes.
Spermiogenesis
This term refers to the maturation of spermatids into sperm cells.
90 Days
How long does spermatogenesis take?
Start of Spermatogenesis
Spermatogonium → Mitosis = 1 Spermatogonium , 1 Primary Spermatocyte or Sperm Cells
Primary Spermatocyte → Meiosis I = Secondary Spermatocyte
Secondary Spermatocyte → Meiosis II = Spermatid
Spermatid → Spermiogenesis = Sperm Cell
End of Spermatogenesis
Flow of Sperm Cell Maturation
Sertoli Cells
Cells responsible for providing support and nutrients for the germ cells (spermatogonium, spermatocytes) as they undergo mitosis and meiosis.
Ejaculatory Ducts
This receives both the sperm from the ductus deferens and fluid from the seminal vesicles.
Fructose, Prostaglandin, Clotting Proteins, and Flavin
Fast Forward Po, Clotting Proteins
Components of Seminal Vesicle
Fructose
Semen component that provides nutrients to the sperm cells.
Prostaglandin
Component of semen responsible for sperm motility and viability.
Clotting Proteins
Component of semen responsible for coagulation of semen after about 5 seconds of ejaculation.
Flavin
Component of semen that makes its appearance Gray or Opalescent, as well as the Blue to Yellow Fluorescence when semen is visualized under ultraviolet light (Wood’s Lamp) or Geen-White Fluorescence under UV Light.
Proteolytic Enzymes
Prostatic Specific Antigen
Citric Acid
Acid Phosphatase
Choline and Spermine
Zinc
PePsa, CaAp, Choline and Spermine, Zinc
Components of the Prostatic Fluid
Citric Acid
Component of semen used by sperm for ATP production.
Proteolytic Enzymes
Component of semen that breaks down clotting proteins and liquefy semen.
Usually, 30 to 60 minutes after collection.
Liquefaction Time
Choline and Spermine
Component of semen that inhibit bacterial growth.
Masturbation
After Interrupted Sexual Intercourse [Coitus Interrupts or Withdrawal Method]
Condom
Aspiration from Vaginal Canal after Intercourse
Collection Methods
St. Lukes Medical Center
For IVF testing, other than doing it in U.S., Japan, or Singapore, what hospital here in the Philippines offer IVF testing already?
After Interrupted Sexual Intercourse [Coitus Interrupts or Withdrawal Method]
Collection method that should be used when a patient is not allowed to masturbate because it is against their beliefs.
Sperm Clumping
Sign of Anti-sperm Antibodies
Empty Bladder
Sexual Abstinence
Fertility Testing
Warm Sterile Glass
Requirements prior to collection of semen.
Ideally kept at room temperature or body temperature [37C]
Delivered to the laboratory within 1 Hour of Collection
Requirements for transport of semen.
Color: Grayish White or Pearly White
Translucent
Not Clear, Not Turbid
Clear: No Sperm Cells
White Turbid: Many WBCs and Infection
Odor: Musty or Bleach-Like
Normal Appearance/Color or Odor of Semen.
Clear: Low Sperm Count
Yellow: Urine Contamination, Prolonged Abstinence, Medications
Gray: Flavin
Red: RBCs (Abnormal)
Colors of Semen (Clear, Yellow, Gray, and Red) and Its Meaning.
Deficiency in Prostatic Enzymes or Proteolytic Enzymes.
It should be reported.
Indication if the liquefaction time took more than 60 minutes.
After 2 Hours
After how many hours, before you initiate putting proteolytic enzymes in a specimen that took too long to liquefy?
Dulbecco's phosphate-buffered saline (DPBS), or
alpha-chymotrypsin bromelain
If after 2 hours the specimen has not liquefied, add _____ or proteolytic enzymes such as _____.
2 to 5 ml per ejaculate
Normal Volume of Semen
Pours like Droplets
Normal Viscosity of Semen
7.2 to 8
Normal pH of Semen
Infection
Indication of High Seminal pH
Increased Prostatic Fluid
Obstruction of the Ejaculatory Duct
Problem in the Seminal Vesicle
Indication of Low Seminal pH
Sperm Concentration
Motility
Morphology Percentage
3 Microscopic Examination for Semen Analysis
20 to 250 Million Sperm PER ML
Sperm Concentration Reference Value
10 to 20 Million Sperm PER ML
Sperm Concentration Borderline Reference Value
AT LEAST 40 Million PER EJACULATE
Sperm Count Reference Value
Sodium bicarbonate
Diluting fluid that dissolves mucus.
Formalin
Diluting fluid that immobilizes sperm
Chilled Water [Not Tap]
Diluting fluid that we always use in the laboratory. The cheapest and always available
Saline and Distilled Water
Diluting fluid other than the sodium bicarbonate, formalin, or chilled water.
Sperm Conc. / mL = [# of Cells Counted x DF (20) x 1,000] / [# of Squares (2) x Vol. of 1 Square (0.1)]
or
Sperm Conc. / mL = # of sperm cells counted x 100,000
if the dilution factor is 1:20 and the WBX squares are 2.
or
Sperm Conc. / mL = [# of Cells Counted x DF (20) x 1,000] / [# of Squares (5) x Vol. of 1 Square (0.004)]
or
Sperm Conc. / mL = # of sperm cells counted x 1,000,000
if the dilution factor is 1:20 and you’re counting in 5 RBC Squares.
Sperm Conc. Formula
Sperm Count/Ejaculate = Sperm Conc. x Semen Volume
Sperm Count / Ejaculate Formula
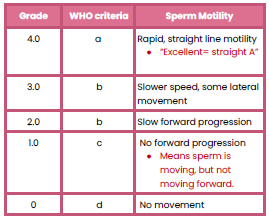
Sperm Motility Grading [Grade - WHO Criteria - Sperm Motility]
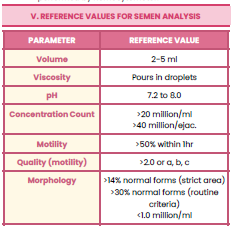
Reference Values for Semen Analysis: Volume, Viscosity, pH, Concentration, Count, Motility, Quality of Motility, Morphology