SAS Exam 4
1/54
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
55 Terms
Pathogenesis of Osteoarthritis
AKA: DJD degenerative joint disease
Arthritis: Inflammation disease within a joint!
Et: Aberrant repair and degradation of articular cartilage
Altered subchondral bone metabolism
Periarticular osteophyte formation
Synovial inflammation
Loss of stiffness and tensile strength of articular cartilage
Mobility impairment = pain
Common sites: Hip, Elbow, Stifle, Shoulder!!
Risk factors for Osteoarthritis (OA)
Primary: Idiopathic & age! → cats
Secondary: developmental
Age: alters joint structure and function
Species: cats > dogs
Body weight: increases joint stress
Adipokines:
Leptin: inhibits chondrocyte growth
Adiponectin: induces cartilage degradation
Gender/Hormonal factors: Estrogen protective effect from inflammation
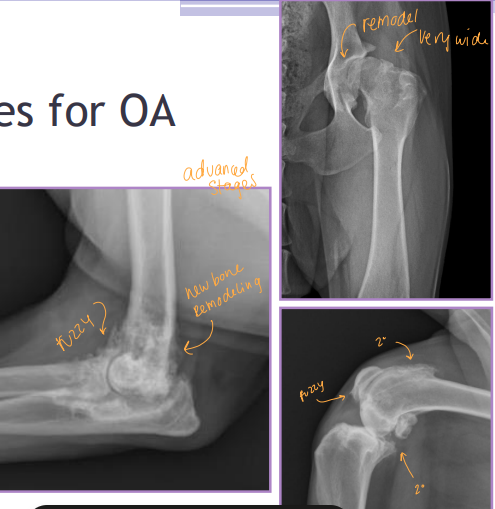
Progression of Osteoarthritis
Stage I: Proteolytic cartilage matrix breakdown
Stage II: Fibrillation and surface erosion of cartilage
Release of breakdown products into synovial fluid
Stage III: Synovial inflammation, phagocytosis stimulates
Cytokine and protease production
Diagnosis of Osteoarthritis
Cs: Slow to rise, Morning stiffness, Improved after activity, Lameness after exercise(pm), Pain
Radiography (#1): Evaluates subchondral bone, cartilage lesions, synovium
Cons: Not sensitive in early stages, Limited soft tissue evaluation, Poor correlation with clinical signs: do not tx the xray
Arthroscopy: Direct visualization of joint, diagnostic, therapeutic, assesses cartilage damage
Synovial fluid analysis Evaluate cell count + types, color, turbidity, viscosity, detect infectious agents
Cons: Risk of introducing infection → sterile prep
Preform AFTER xrays/CT/MRI
Diagnosis of Osteoarthritis: MRI vs. CT
MRI: Soft tissue, cartilage defects, thickness, effusion, synovitis, edema, menisci, ligaments, osteophytes
Cons: $$, limited availability, requires anesthesia
Pros: Shoulders!
CT: Bone, osteophyte, complex joints evaluation & combo w/ arthrography
Cons: Poor for soft tissue
Pros: elbows and tarsals
Lifestyle Osteoarthritis Management
Considerations: No cure or approved disease-modifying drugs, Multifactorial disease
Multimodal approach: GOAL- improve quality of life and CS!
Lifestyle: Weight Control BCS 4/9 and Low-impact exercise
Passive range of motion, Water treadmill, Strengthening exercises, Heat/cold therapy, Acupuncture
Diet: Low fat / weight loss diets! & family support
Glucosamine + Chondroitin sulfate: PSGAGs
Stimulate chondrocytes
Anti-inflammatory
Takes 4–6 weeks for effect
Omega-3 fatty acids: EPA/DHA, Fish oil
Anti-inflammatory
Medical Osteoarthritis Management
Pain Management: NSAIDs, Gabapentin, Amantadine
Anti-NGF ab: IM injections - Librela (dogs), Solensia (cats)
Stem Cell Therapy: Intra-articular injection of adult multipotent stem cells
Anti-inflammatory, regenerative effects
Platelet-Rich Plasma: Stimulates natural healing response
Adequan: Semi-synthetic glycosaminoglycan, PSGAGs
Disease-Modifying Agent: Inhibits MMPs, prostaglandins, cytokines and promotes HA, collagen, proteoglycan synthesis
SPRYNG: Intra-articular injection, repeat q 1.5y
Disease-Modifying Agent: Creates microcushion matrix and absorbs/release synovial fluid with impact

Surgical Osteoarthritis Management
examples: CCL, patella, articular damage
Corrective: Slows down progression of OA
Goals: Address underlying condition
Types: CCL stabilization, Patellar luxation repair, Articular fracture repair, Remove fragmented coronoid process, OCD lesion debridement
Salvage: Joint replacement(total hip), (FHNO) Femoral head & neck ostectomy, Arthrodesis(fusion)
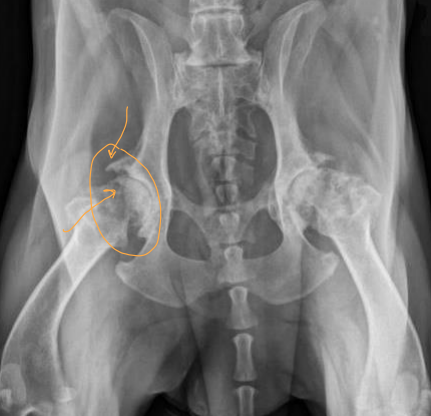
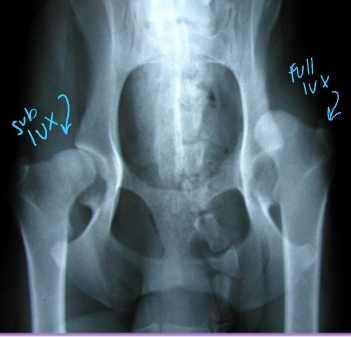
Pathogenesis of Hip Dysplasia
Dev: Abnormal development of the coxofemoral joint
Subluxation + Osteoarthritis (DJD)
#1 dz of the coxofemoral joint
Primary: genetic, Environmental: contributing
Et: Round lig and joint capsule are stretched → subluxation of femoral head
Phase 1: excessive joint lax → phase 2: osteoarthritis
Cartilage damage, Trabecular bone microfracture, Synovitis
Risk: Genetics, rapid weight gain or growth, high Ca + protein diet, activity, flooring, decreased pelvic muscle mass, large breeds

Clinical Presentation of Hip Dysplasia
Bilateral > unilateral
<6-8 months: Abnormal gait, Bunny hopping, Asymmetric sitting, Waddling, Reluctant to jump, Mildly painful
6-12 months: unilateral/bilateral Hind limb lameness, Difficulty rising, Exercise intolerance, Stiff gait, Thigh muscle atrophy, Pain, Decreased muscle mass
10-12 months: Fxn improvement, Joint capsule fibrosis and tightening, Residual lameness
Long-Term: Lameness, Thigh muscle atrophy, Crepitus, Pain, Chronic low-grade OA, circumduction, hopping
lameness worse in AM & after exercise
32% of dogs will also have CrCL rupture
Differentiate from Hip Dysplasia and Lumbosacral Disease
Direct palpation in lateral/non-weight bearing
Weakness due to neurologic disease = Conscious proprioception deficits (LS)
Rectal palpation can identify LS disease(direct pressure)
hip extension → flexes LS joint, stretch iliopsoas muscle

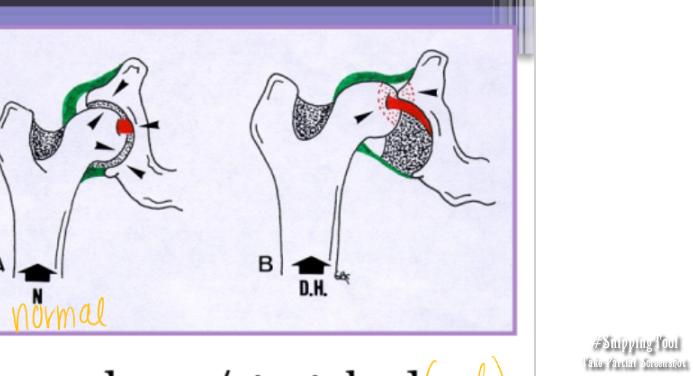
Laxity Tests for Hip Dysplasia
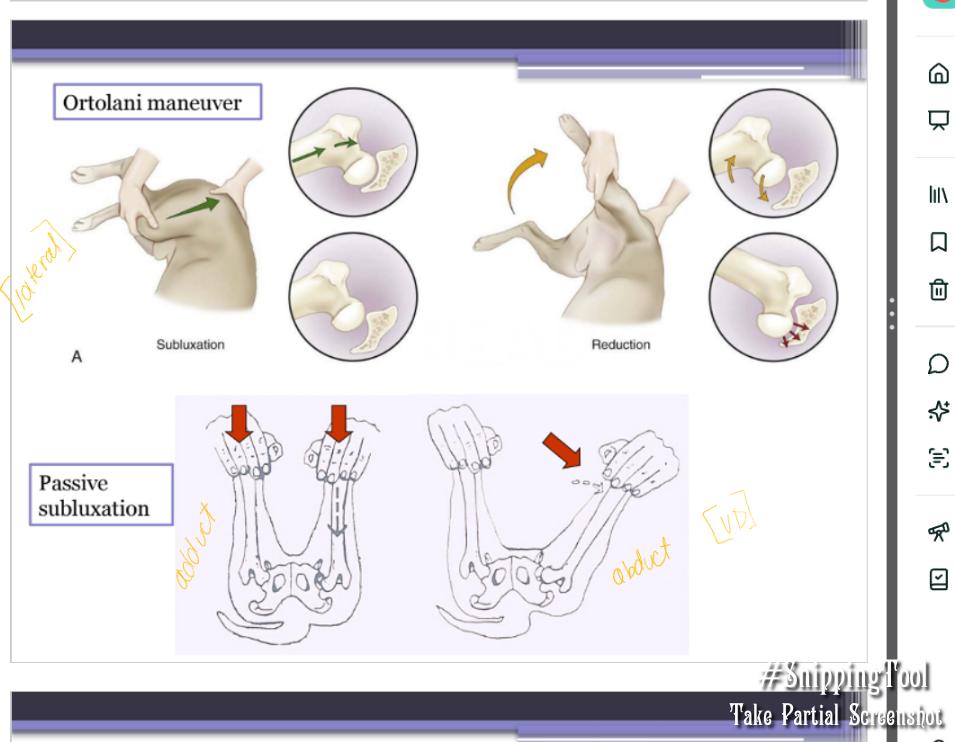
Ortolani maneuver: angle of reduction → evaluates for laxity
How: Force femur to subluxate then reduce, done under sedation
Results:
‘Clunk’ = laxity present
‘Clunk’ = reduction of hip
No laxity, shallow acetabulum, severe OA
Barlow test: angle of subluxation
How: Force femur to subluxate
1st ½ of ortolani maneuver → “how far can we get them to luxate”
Barden test
How: Laterally displace femur
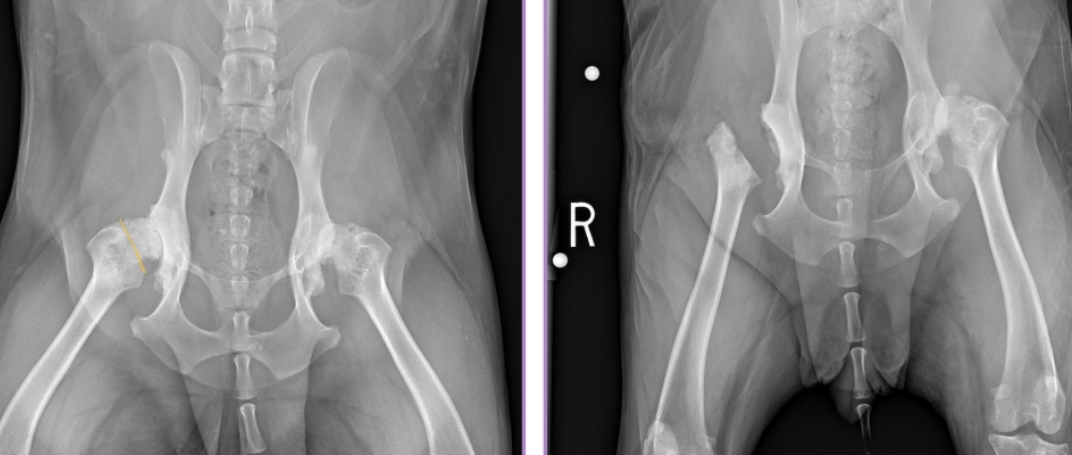
Screening for Hip Displasia
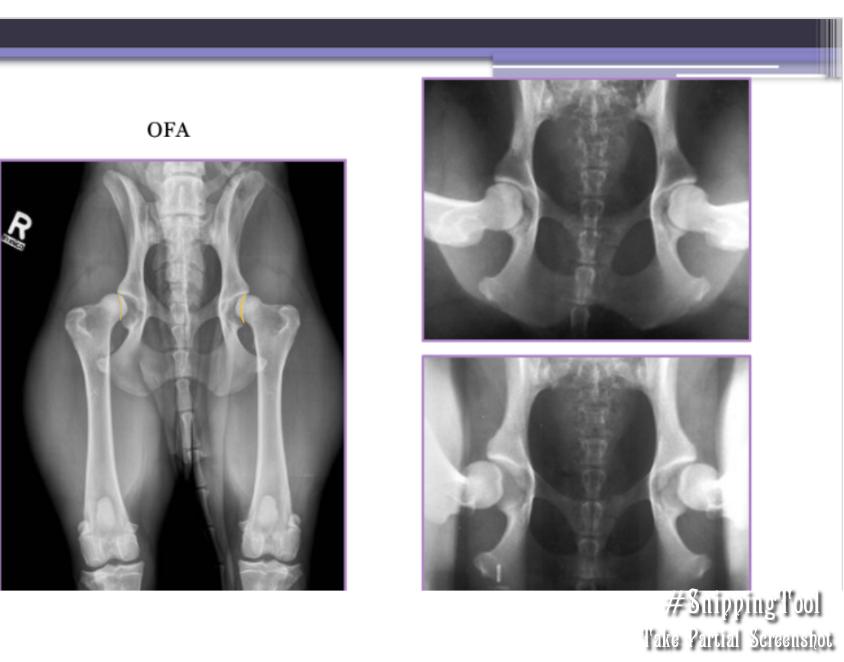
OFA: Evaluates passive laxity
When: Certified >2 years
Grades:
Normal: excellent, good, fair, borderline
Dysplastic: mild, moderate, severe
PennHip: Evaluates passive distractive laxity
When: Certified >16 weeks
Grades: Scale 0–1
0.58 = 58% femoral head displacement
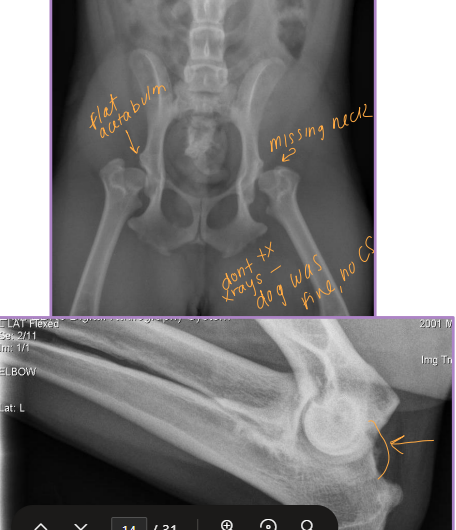
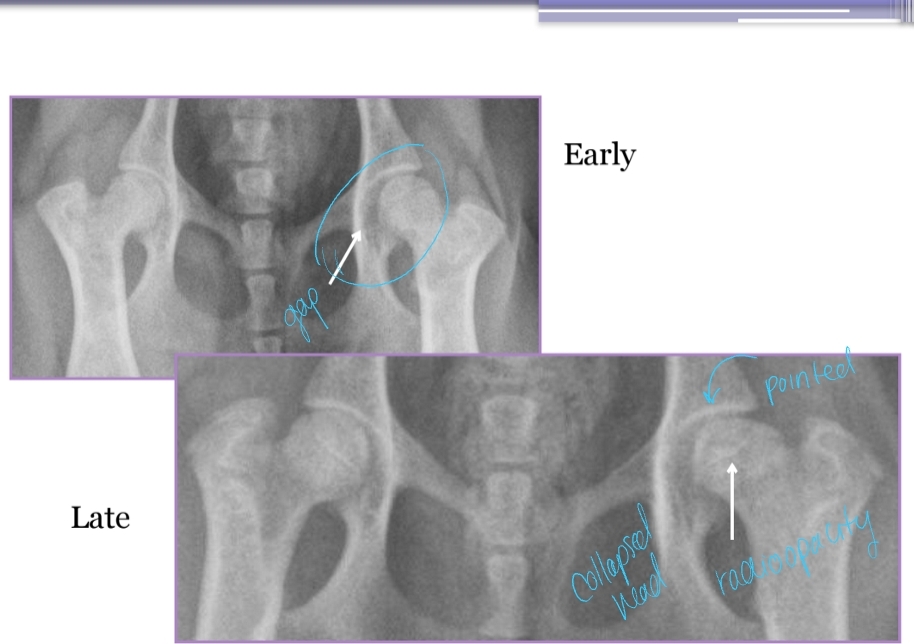
Diagnostic Imaging for Hip Dysplasia
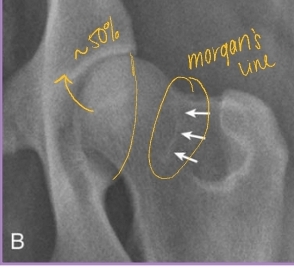
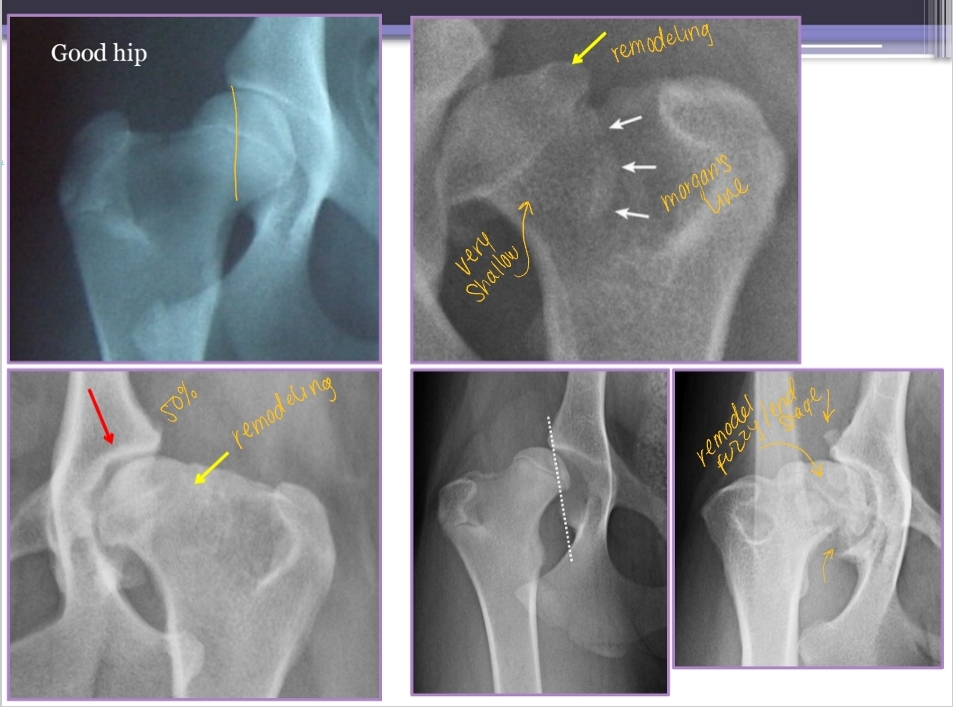
VD most useful
Want >50% acetabular coverage!
Rads: Bone shape, remodeling, osteophytosis(neck), enthesiophytosis (Morgan’s line), laxity
Do not treat the radiograph!
CT + MRI: not useful and expensive
Arthrocentesis: Rule out infection or neoplasia
Arthroscopy: Articular lesion evaluation, prior to TPO
Rarely needed
Juvenile Pubic Symphysiodesis (JPS)
Young, showing CS
Sig: 12-24 weeks
Use: Prophylactic and preventative, increase femoral head coverage, fuse pubic symphysis growth plate, decrease OA progression, Improved congruency
Burns the pubis symphysis
Triple Pelvic Osteotomy
Physically rotating acetabulum
Sig: Age <12m, laxity but no OA, Lg breeds, angle of reduction ≤30°
Use: Preventative and palliative, rotate acetabulum to increase coverage, cut ilial body, pubis, ischium
Cut in 3 places, place plates to stabilize
Pro: 90% success rate
Con: OA may still progress but slower

Total Hip Arthroplasty
Use: Salvage, replace end-stage joint with prosthesis
Pro: Near-normal fxn, Quick
Cons: expensive
Femoral Head and Neck Ostectomy (FHNO)
Adequate muscle mass is present!
Use: remove pain by excising joint, salvage
Pro: Cheaper, easier, faster
Con: worse fxn
Begin Aggressive rehabilitation ASAP
Treatment of Hip Dysplasia
Medical: use for as long as possible, treat OA, use until refractory response or muscle loss
Juvenile Pubic Symphysiodesis
Triple Pelvic Osteotomy
Total Hip Arthroplasty
Femoral Head and Neck Ostectomy
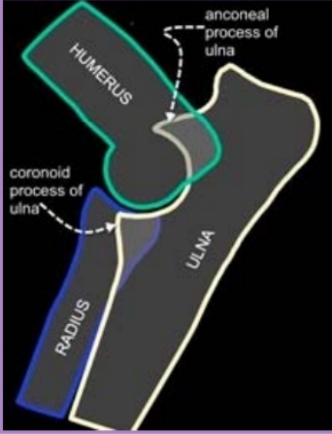
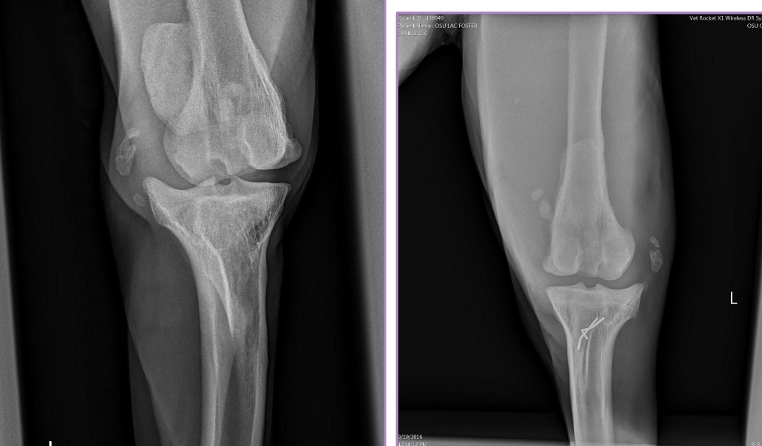
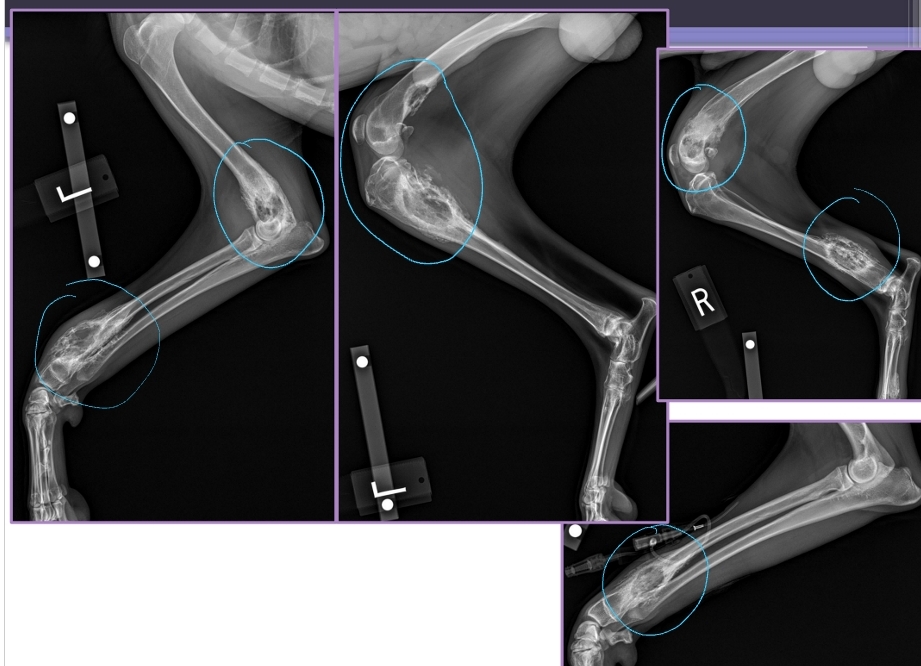
Elbow Dysplasia Clinical Presentation
Et: Genetics + environ factors
Ununited anconeal process, medial compartment disease, medial coronoid disease, OC, OCD, Elbow incongruity
Sig: Young >>> older, large breeds, rapidly growing dogs
Cs: lameness
#1 cause of forelimb lameness
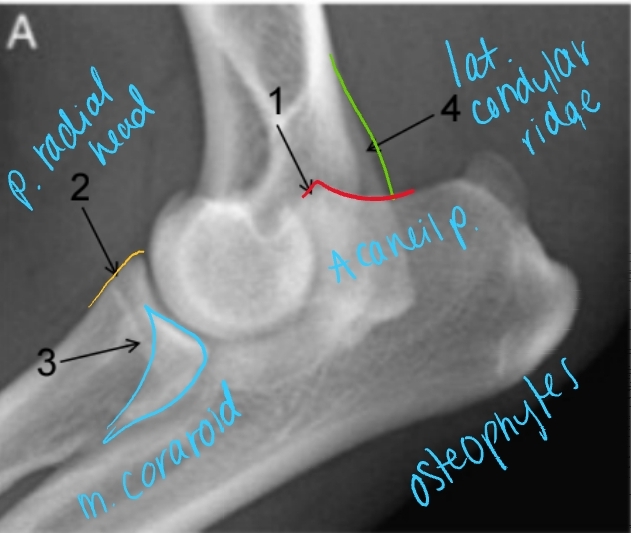
Medial Compartment and Coronoid Disease
Growing/developmental disease, Bilateral
Et: Growth incongruency radius/ulna, abnormal joint stress, pressure on medial coronoid of ulna
Sig: Large breed dogs, Labs, Bernese Mountain Dog, Male > Female, 6-18 months
Cs: OA, Lameness with ambulation, Decreased ROM of elbow joint, Pain(PE/palpation), Minimal joint effusion, Muscle atrophy
Dt: Lateral, AP, flexed, Crlat-oblique
Rads: Osteophytes(back of elbow), Effusion, Subtrochlear sclerosis, Joint incongruity
CT: Most sensitive
Tx: Rx: Management of OA
Sx: gold standard
Medial arthrotomy:
Cons: Limited view, high postoperative morbidity
Arthroscopy (#1): gold standard
Pro: Min invasive, good view
Cons: higher cost, learning curve
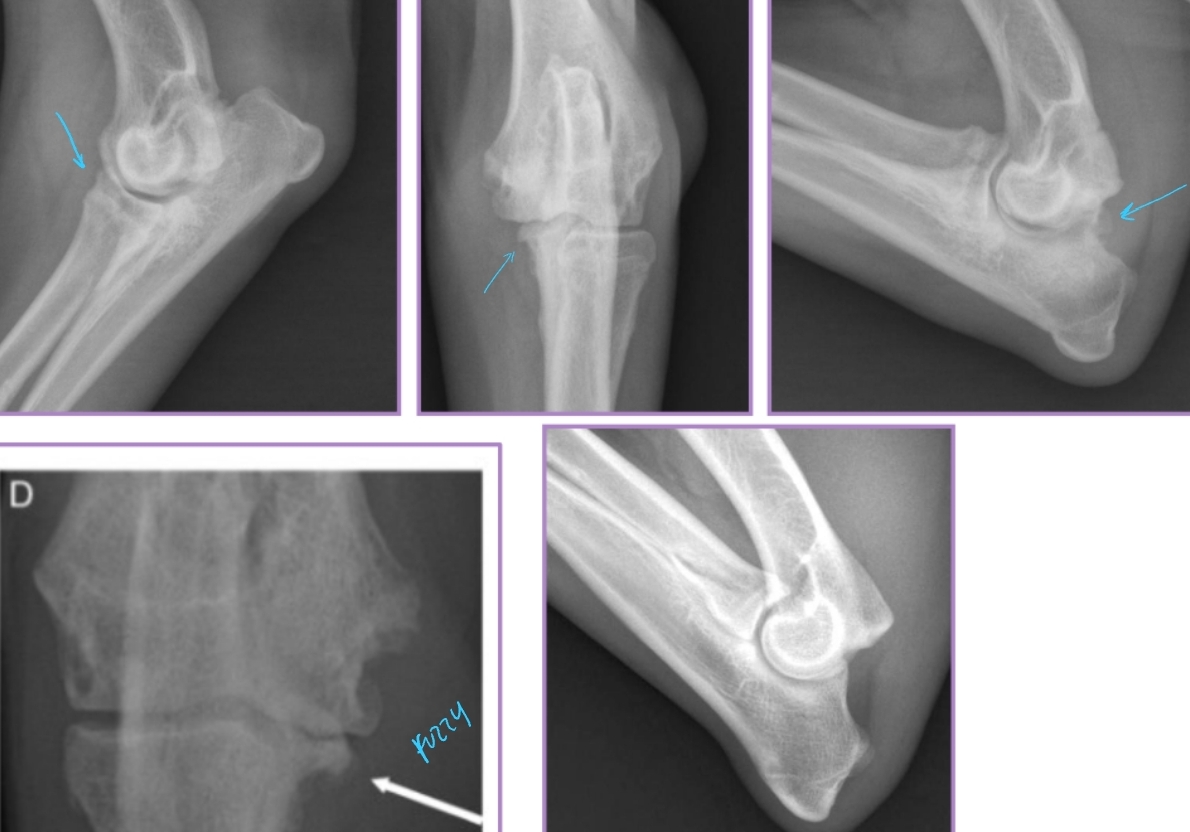

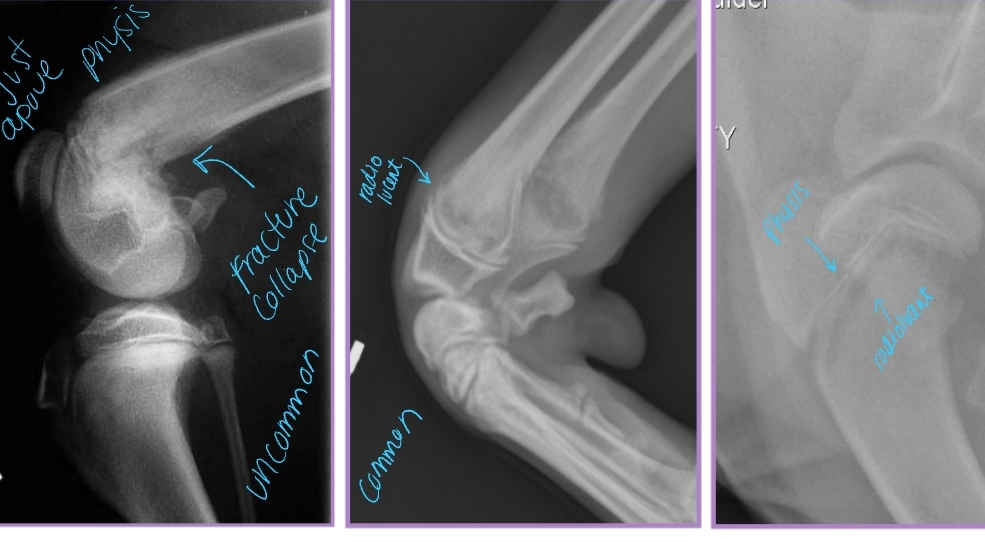
Osteochondrosis and Osteochondritis Dissecans
Et: Defect of normal endochondral ossification
Shoulder
Sig: large breed dogs, rapid growth, 5-10 months
Cs: lameness, pain, decreased ROM, muscle atrophy, effusion
Dt:
Rads: Divot of subchondral bone, OA, free cartilage flap
CT: Detects subtle subchondral bone lesions
Tx: Arthrotomy or arthroscopy
Remove cartilage flap, debride subchondral bone, promote fibrocartilage repair


Ununited Anconeal Process
Et: Anconeal process of ulna fails to unite with proximal ulnar metaphysis
Failure of endochondral ossification, Joint incongruity
Hereditary, environmental, hormonal factors
Sig: Large breeds, GSD, Male > female, 5-12 months
Dt: Radiographs FLEXED lateral!
Osteophytes, Effusion, Anconeal process fragment, Joint incongruity
Tx:
Rx: OA management
End stage or financial issues
Sx: #1 , <1yr - early sx **
Early: primary repair, viable cartilage
Ulnar osteotomy → remove stress, allow fusion
Lag screw fixation of anconeal process
Chronic: excision of anconeal process
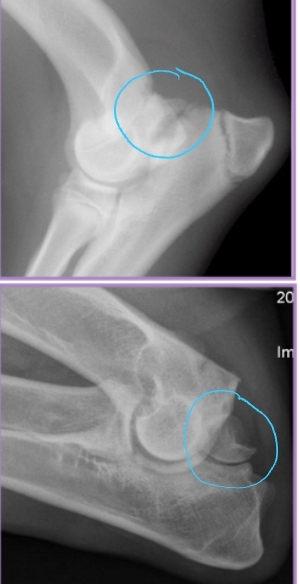
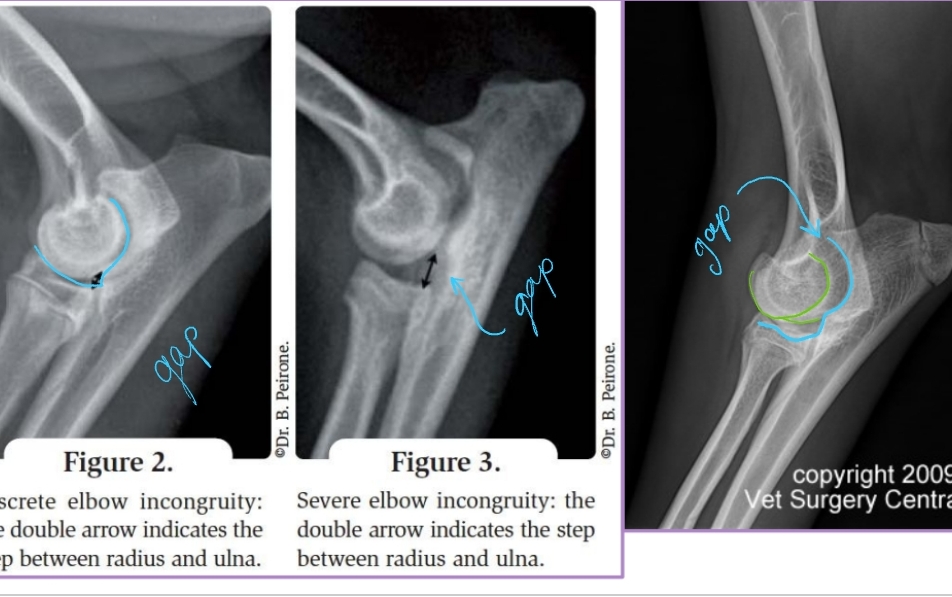
Elbow Incongruity
Et: Asynchronous growth of radius and ulna
Dt: radiographs
Tx: Corrective ulnar ostectomy (short radius syndrome)
Redistribute stress in joint
Allow bone alignment at joint level
Decrease joint stress
Secondary stabilizers of stifle
Secondary stabilizers:
Menisci
Medial: larger, more ovoid
Stuck to meniscus/tibia
ruptures w/ CrCL tears
Lateral: smaller, more circular
Meniscofemoral ligament! protects from CrCL tear
Fxn: Protects from injury with a CrCL tear, shock absorption, lubrication, stability
Tendons: LDE, patellar, popliteal
Fibrous joint capsule
Cranial Cruciate Ligament Disease Pathogenesis
Et: Chronic inflammatory stimulus, Trama, Genetics
Cranial tibial thrust, Repetitive microtrauma to CrCL, Release of degradative products, Synovitis, Articular cartilage damage, Loss of proteoglycans, Increase in cartilage water content, Metalloproteinase production and release, Cytokine production and release
Sig: 2-10 years, Neutered, Large breeds
Breeds: Labrador, Boxer, Newfoundland, Rottweiler
Conformation: Straight stifle joint, Narrow intercondylar notch, Excessive tibial plateau slope
Cranial Drawer
Cranial translocation of the tibia
How: lateral recumbency, stabilize femur, move tibia cranially
One hand: thumb on fabellae, index on patella
Other hand: thumb on fibular head, index on tibial crest
Results:
Present in flexion only = partial tear
Present in flexion and extension = complete tear
Tibial Thrust
Tibia translates cranially relative to femur
How: Stabilize stifle, flex hock, feel tibia move cranially
One hand: cup distal femur/stifle, index on tibial crest
Other hand: grasp paw distal to hock
Results:
Absent = normal or partial tear
Present = torn CrCL
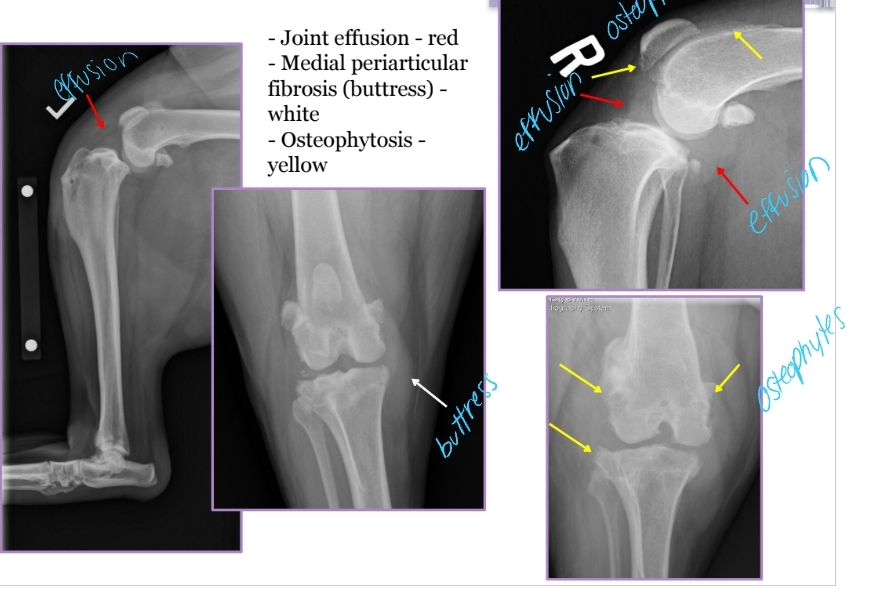
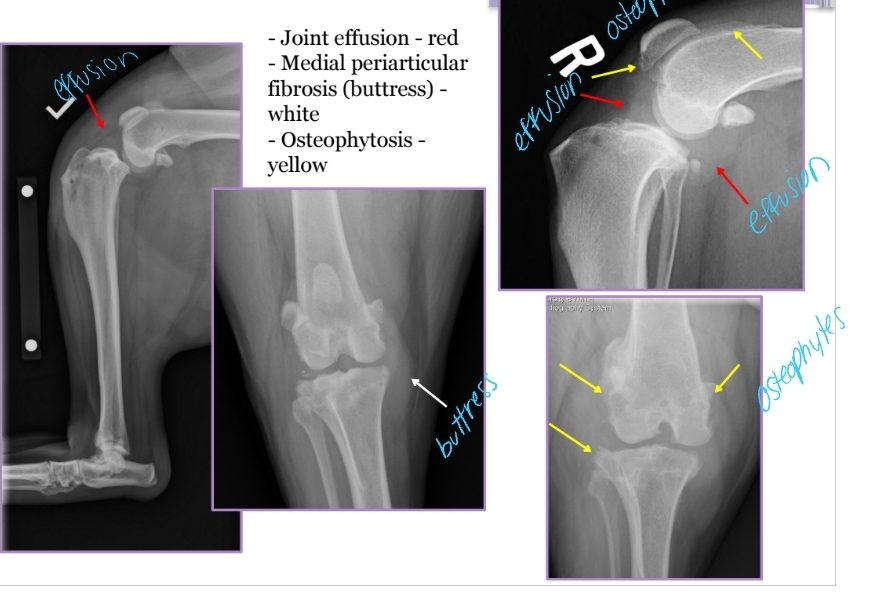
Cranial Cruciate Ligament Disease Diagnosis
PE: Crouched hindlimbs, external rotation of affected limb, Failed “sit test”
Acute clinical presentation
Meniscal Click: Torn meniscus pops due to shear with range of motion
Radiographs: Joint effusion, Medial periarticular fibrosis(medial buttress), Osteophytosis, Cranial drawer placement, OA
Cranial Cruciate surgical repairs
Arthrotomy: Debride CrCL + torn meniscus
Extracapsular Stabilization: Lateral suture stabilization eliminates cranial drawer and tibial thrust
Limb fixed at standing angle
Suture placed in path of CrCL
Long-term stabilization via periarticular fibrosis
TPLO: Mechanically alters angle of proximal tibia and eliminates tibial thrust
Faster return to fxn, lower failure risk, working or active dogs
CBLO: cora-based leveling osteotomy (reverse TPLO)
TTA: tibial tuberosity advancement
Primary repair of meniscus: not feasible
Cranial Cruciate Ligament Disease Treatment
Rx: Crate rest × 6 weeks, limited activity, OA management, pain control
Poor anesthetic candidate, Financial constraints, Patient <15 kg
Continue lifelong OA management even with Sx
Sx: Debilitation, CrCL tear, lameness without obvious instability
Px: High risk of tearing contralateral CrCL within 2 years, meniscus tear risk, OA progression

Patellar Luxation Pathophysiology
Et: Traumatic, Congenital
Shallow trochlear groove, malalignment of extensor mechanism, abnormal hip joint conformation, femoral malformation, tibial malformation, quadriceps tightness
Sig: Medial most common, 98%
Medial: Small breeds, young age
Lateral: large breeds
Grading Medial Patellar Luxation
Grade 1:
Patella can be luxated but returns to normal position spontaneously
Functionally normal
Grade 2:
Patella luxates out of groove occasionally
Can be replaced manually or reduces spontaneously
Grade 3:
Patella luxates most of the time
Can be replaced manually
Grade 4:
Patella luxates all of the time
Cannot be replaced back into the groove
Requires corrective osteotomy!!!
Patellar Luxation Diagnosis
Cs: Skipping, kicks leg straight backwards, non-weight-bearing lameness
Attempt to elicit luxation: Fully extend stifle joint, Internally rotate tibia, Apply medially directed pressure to patella while flexing stifle
Evaluate for CrCL tear: 15–20% of chronic MPL patients have CrCL tear
Radiographs: Stifle, pelvis, angular limb deformity, OA
Patellar Luxation Treatment
Rx: OA management, rest 8 weeks, Modified Robert Jones bandage 2 weeks
Sx: Only when CS and patient is effected!
Soft tissue: Medial retinacular release, Lateral retinacular imbrication
Bone: Tibial crest transposition(laterally), recession trochleoplasty(deepens groove), femoral/tibial osteotomies, anti-rotational suture, lateral stabilization, patellofabellar suture
Px: OA progress slowly, Half reluxate postop
Good: Grades 1-3
Poor/guarded: Grade 4

Shoulder Luxation
Et: congenital or trama
Ligamentous laxity, Glenoid dysplasia
Sig: Young small breeds (congenital)
Cs: lameness
Tx:
Congenital: MCL repair, arthroplasty
Acquired: Medial, Closed reduction, Bandage 2 weeks, rest 2 weeks, sling, MCL repair
Velpeau sling: for medial luxation
Neutral sling: for lateral luxation
Salvage: Arthrodesis, Glenoid excision

Elbow Luxation
Et: Traumatic most common
Traumatic: Radius and ulna luxate laterally
large medial condyle of humerus prevents medial luxation
Congenital: abnormally shaped radius/ulna/ humerus
Cs: Unable to bear weight, Forelimb abducted and externally rotated (elbow out, paw rotated in)
Dt: limb resists extension, prominent radial head, PAINFUL, Radiographs AP views!
Tx:
Acquired: Closed reduction under GA + brachial plexus block
Flex elbow to 100° and internally rotate
Extend elbow slightly, adduct and inwardly rotate antebrachium while applying medial pressure on radial head
Immobilize 2 weeks w/ spica split
Congenital
If reducible → place transarticular pin while still growing!! remove later on
If non-reducible → arthrodesis when older in standing position

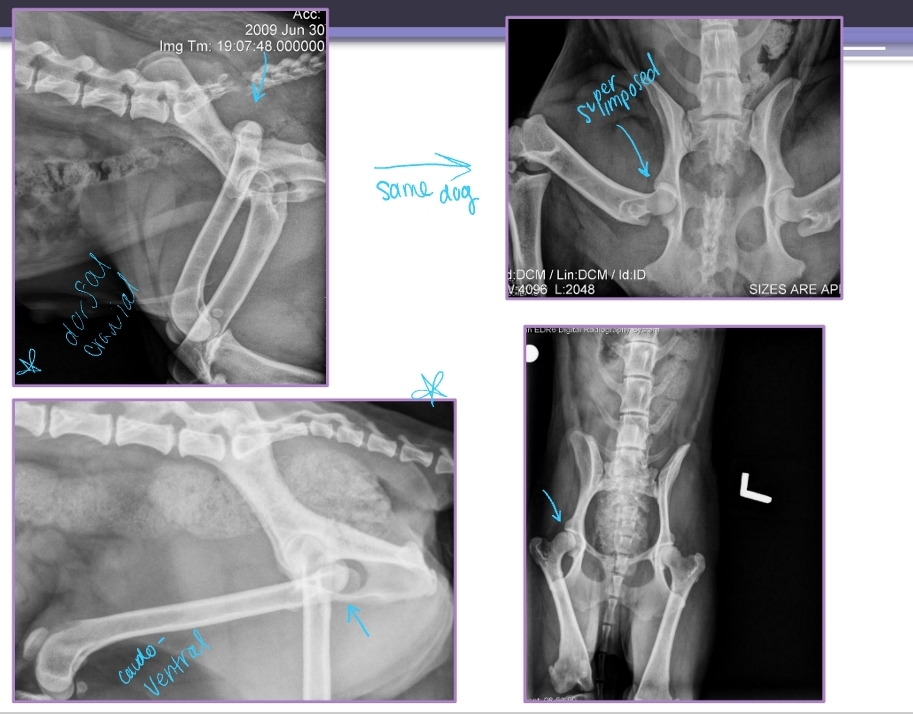
Carpal Hyperextension or Luxation
Et: Palmar fibrocartilage and ligaments torn of loss of support
fall or hyperextension injury
Cs: Non-weightbearing lameness, Stand with carpus hyperextended, Palmigrade stance
Dt: Radiographs
Tx: arthrodesis
Splinting does not work

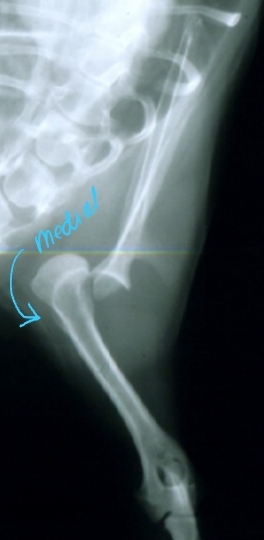
Hip Luxation Pathophysiology
Et: Results from failure or tear of Joint capsule or Round ligament
Most common joint luxation in dogs
Types:
Craniodorsal (#1): hit-by-car or blunt trauma
Caudoventral: fall with abduction
Hip Luxation Diagnosis
Cs: Crepitus, pain, shortened limb length(craniodorsal), pelvic asymmetry
Palpate: Iliac crest(wing), Greater trochanter of femur, and Ischiatic tuberosity form a straight line
Normal = shallow triangle
Thumb test: Place thumb in ischiatic notch and externally rotate limb
Normal = Thumb should be pushed out of notch
Radiographs: lateral & VD
Hip Luxation Treatment
Closed Reduction:
Craniodorsal luxation:
External rotation → Pull limb caudally and distally → Internal rotation
Ehmer sling 2w → Maintain abduction + internal rotation
Caudoventral luxation:
Abduct limb → Provide distraction → Apply lateral and proximal pressure
Hobbles 2w → Maintain adduction
Open Reduction and Fixation:
Why: Closed reduction unsuccessful
How: Toggle pin technique
Creates synthetic round ligament
Hip must have no evidence of OA
Salvage:
Why: Chronic luxation’s, Damaged articular cartilage, OA
How: Total hip replacement or Femoral head and neck ostectomy(FHNO) more common(cheaper)

Collateral Ligament Injury
Et: Can occur in any joint
Cs: Varus or valgus, lameness
Dt: radiographs
I: Stretching of fibers
II: Incomplete tear
III: Complete tear
Tx:
Rx: Grade I → external coaptation x 6–8 weeks
Sx: Grade II-III → surgical stabilization + external coaptation
Tarsal Injuries
Et: Usually shearing injuries
Collateral instability, Open fractures, Sheared bone, Soft tissue injury
often medial collateral damaged → excessive valgus
Tx: Reconstruction, Arthrodesis
Arthrodesis
Use: Salvage procedure, for carpals/tarsals
Tarsal injuries, Carpal Hyperextension, Carpal Luxation, Shoulder Luxation
How: Permanent fusion of joints with plates, screws, pins or ESF
Remove cartilage and maintain limb at normal standing angle
Px: Eliminates flexion/extension of joint and results in mechanical lameness
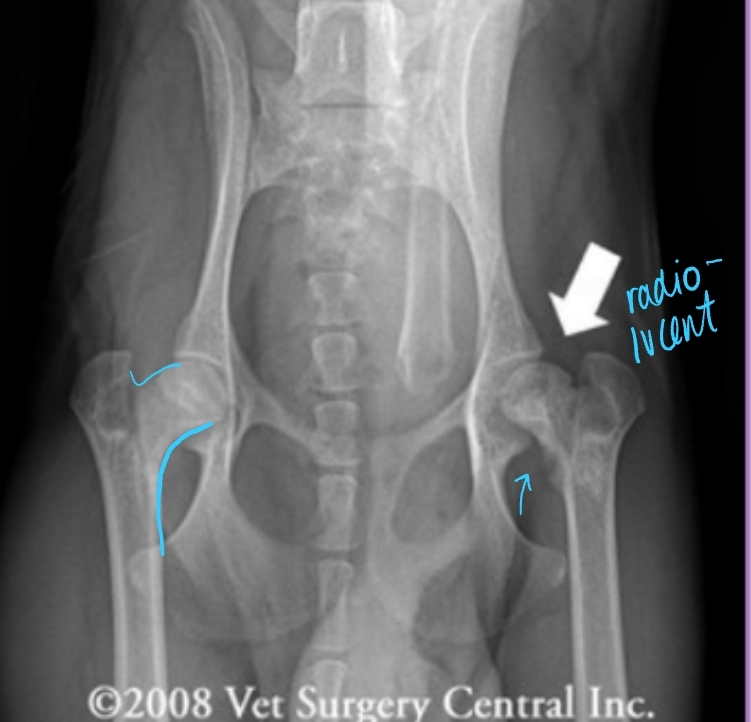
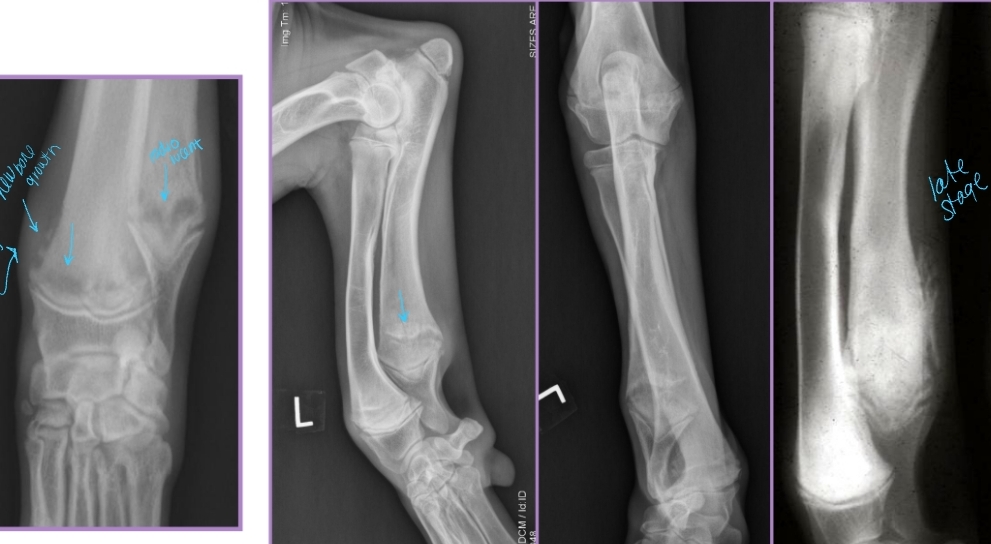
Legg-Calve-Perthes
Et: Avascular necrosis of the femoral head
Vascular damage, necrosis, collapse of femoral head → pain and arthritis
Sig: Young (4-11m), small breed dogs - inherited
Miniature Poodle, Cairn Terrier, Manchester Terrier,cats
Cs: Acute onset hindlimb lameness, P Pain on PE, OA, weight-bearing issues
Unilateral or bilateral
Dt: signalment & Radiographs
Early: Increased opacity of lateral epiphysis (femoral head) and joint space due to effusion
Late: Collapse/flattening/thickening of femoral head + neck, ± Femoral neck fracture
Tx: (Early stages)Robinson sling, Pain control, (late stages)Total hip arthroplasty, Femoral head and neck ostectomy(FHNO)
Splint needs to be non-WB and goes past leg
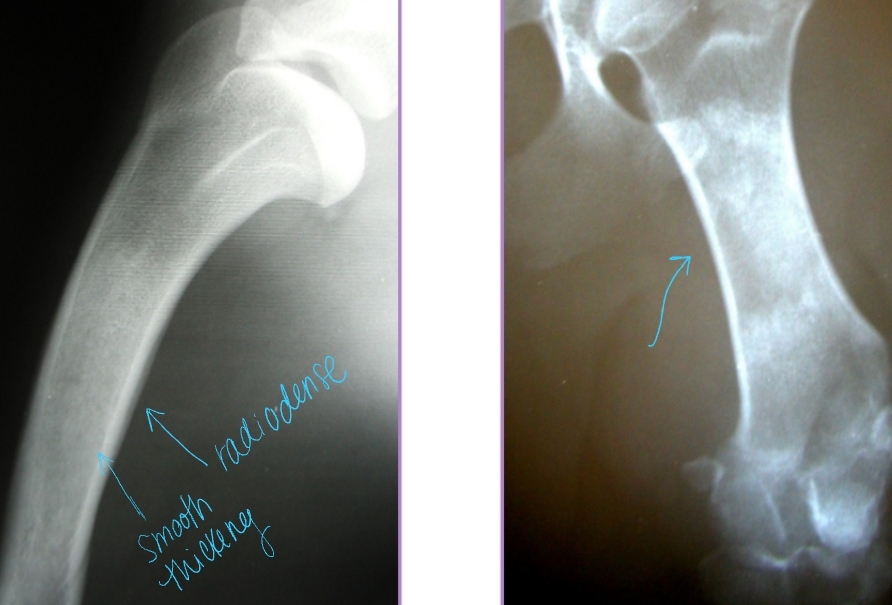
Panosteitis
Et: Disease of endosteum and bone marrow in the long bones
Increased IO pressure due to protein accumulation near nutrient foramen (near major BV), medullary vessels leakage
ulna, humerus, radius, femur, tibia
Forelimb > hindlimb
Sig: 5-18 months, male > female, large breed
Cs: Shifting leg lameness, Lethargic, Pain (cyclic), Anorexia, Fever
Dt:
PE: pain on palpation of diaphysis of long bone
pain receptors in periosteum
Radiographs: Radiodense, patchy infiltrates, Widening of nutrient foramen
Late periosteal response – smooth, thick cortex appearance
Tx: Analgesics, Rest, Self-limiting (1-2w)
relapse can present in other bones
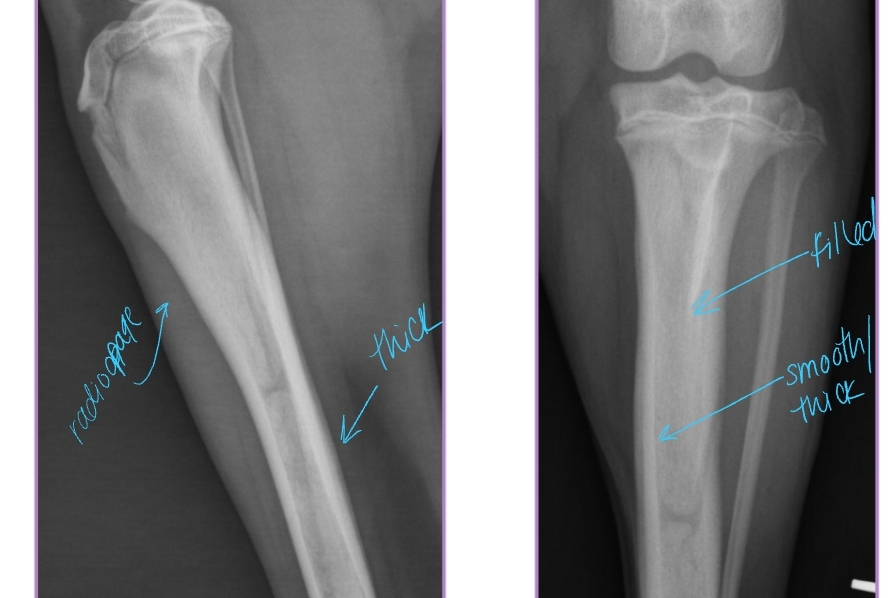
Hypertrophic Osteodystrophy (HOD)
AKA: Scurvy, Moeller-Barlow disease, Metaphyseal osteopathy, Osteodystrophy type I & II, Hypovitaminosis C
Et: Disease of long bones, especially distal metaphyses
Capillary loops become necrotic, vascular congestion, edema, metaplastic cartilage/bone
Forelimbs > hindlimbs
Sig: Juvenile large breed dogs, Rapid growth, <12 months
Cs: Acute onset of lameness, Fever, Lethargy, Anorexia, Diarrhea, Pain at metaphyses, Heat at metaphysis on all 4 limbs!!
Dt: Radiographs
Irregular, radiolucent line in metaphysis adjacent/parallel to physis (“double physeal line”)
Metaphyseal flaring + sclerosis
Subperiosteal and extraperiosteal new bone formation
Tx: Analgesics, antibiotics,self-limiting

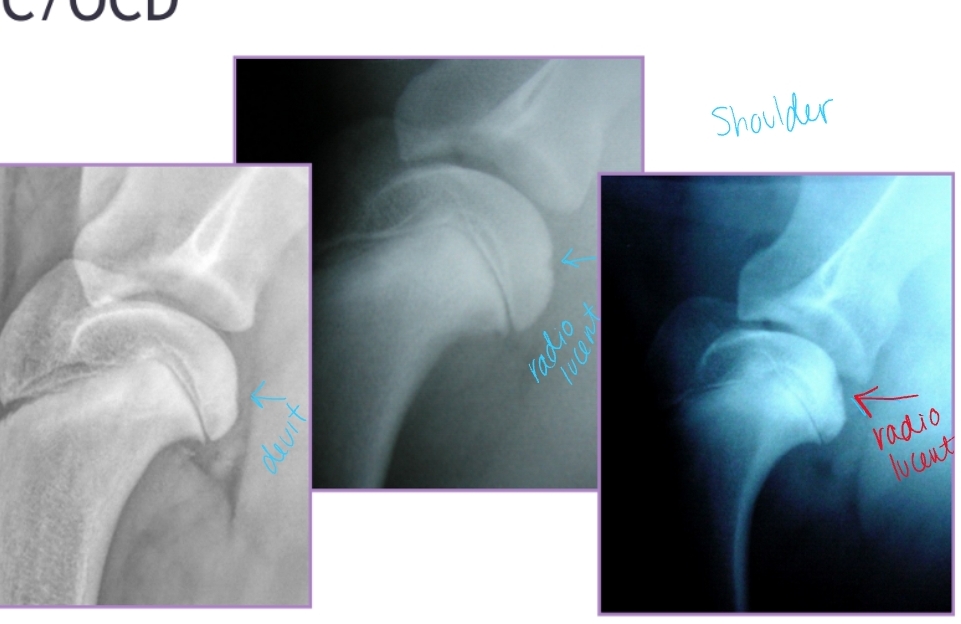
Osteochondrosis + Osteochondritis Dissecans
Et: Defect in normal endochondral ossification
Shoulder(most common), Elbow, Stifle, Hock
Path: Failure of cartilage to ossify → thickened cartilage (OC) → poor nutrition → mechanical trauma → cartilage fissuring/flap(OCD) → synovial inflammation → pain
Sig: Juvenile large breed dogs
Cs: Lameness, Pain, Decreased ROM, Muscle atrophy, Joint effusion palpable
Dt: Radiographs, CT
Caudal humeral head – lateral view
Medial humeral condyle – oblique view(elbow)
Medial aspect of lateral femoral condyle – AP view
Medial/lateral trochlear ridges of hock – AP/oblique views
Tx: Arthrotomy, arthroscopy, remove cartilage flap, debridement of subchondral bleeding bone
Px:
Shoulder: excellent
Elbow/Stifle: good
Hock: guarded

Hypertrophic Osteopathy (HO)
Et: Diffuse periosteal reaction, new bone formation around metacarpal/metatarsal/long bones (running up/down bone)
Paraneoplastic syndrome(lung tumor)
Path: Altered pulmonary function → increased blood flow → connective tissue congestion → periosteal bone formation
Sig: old dogs (rare in cats)
Cs: Reluctance to move, Swelling of distal extremities, Lethargy
Dt: Radiographs: affected limb/chest/abdomen
Uniform periosteal proliferation progressing proximally
Normal articular surfaces
Tx: Treat underlying disease
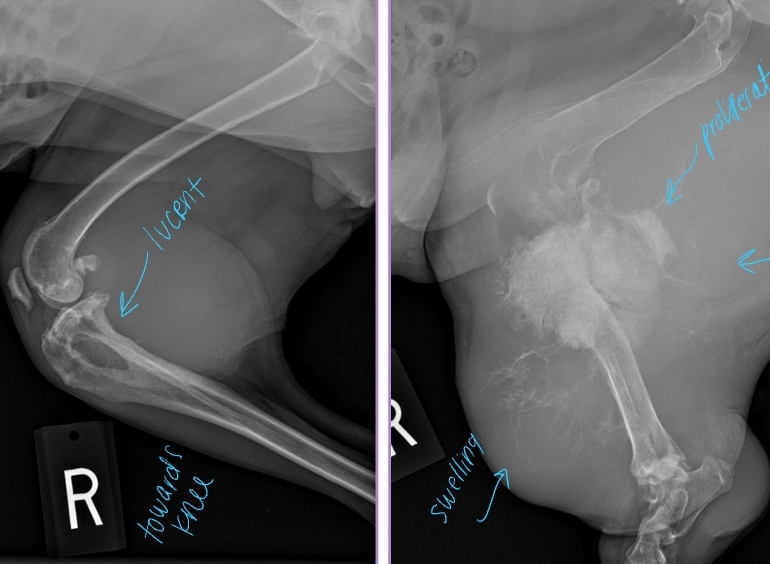
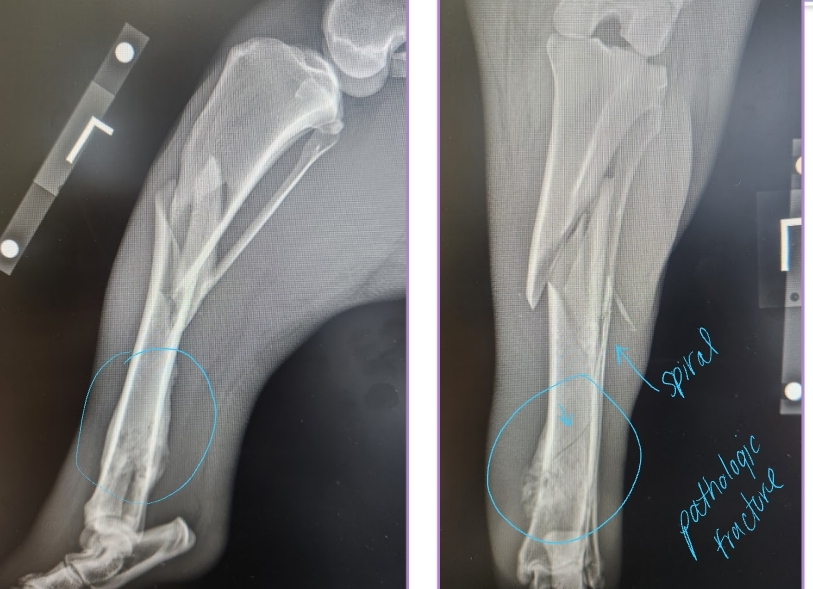
Primary Bone Neoplasia
Et: Osteosarcoma, Chondrosarcoma
Cs: Lameness, Muscle atrophy, Bone swelling
Dt: Radiographs #1, CT, Bone biopsy
Osteolysis, Osteoproliferation, Soft tissue swelling
“Away from the elbow, toward the knee”
proximal humerus, distal radius/ulna & distal femur, proximal tibia
Tx:
Amputation: Eliminates pain, MST 6 months
Amputation + Chemo: Eliminates pain, MST 12 months
Primary Stabilization + Chemo: Allows mobility, MST 12 months
Chemo adds extra time of survival!!
Systemic Infection in Bone
Et: Fungal or bacterial infection
Cs: Lameness, Muscle atrophy, Soft tissue swelling
Dt: Radiographs, Urine!! histoplasmosis antigen (Mira Vista), CT scan,
Bone biopsy and culture
Fungal: fresh
Bacterial: fresh/frozen

Shoulder Injury
Et:
Supraspinatus / Biceps / Subscapularis tendinopathy: Chronic, repetitive microtrauma
Infraspinatus contracture: Acute muscle fiber injury and Fibrous tissue formation
Sig: young, large breed, active dogs, Brittany Spaniel(infraspinatus contracture)
Cs: Shoulder pain
infraspinatus contracture: External rotation of shoulder → elbow abduction + outward rotation of paw(away from body)
Dt: US, Radiographs, MRI, Arthroscopy
Tx: steroid injections→ everyone bedside infraspinatus
platelet-rich Plasma
SX → transect biceps(best), supraspinatus, infraspinatus

Common Calcaneal Tendon Injury
Et: Mid-tendon laceration, Avulsion of tendon from calcaneus, Fracture of calcaneus
Cushing’s, Hypokalemia (cats), Diabetic neuropathy (cats)
Sig: Middle-aged to older, large breed dogs
Cs: Flexed tarsus with extended stifle (“dropped hock”) & flexion of toes w/ WB (gripping floor, SDF intacted)
Usually unilateral
Mild = flexion of hock
Severe = full collapse
Dt: Chronic = thick tendon/minerals
Radiographs: Increased soft tissue opacity, Mineralization, Bone avulsion, Gas in soft tissue
US: Focal hypoechoic area in tendon
Tx: Surgical repair + EC (#1), (sx not option) EC w/ Hock in moderate extension 8w post-op
Repair tendon or avulsed calcaneus, tension band fixation
External coaptation alone is not effective
Px: Long, frustrating recovery process

Iliopsoas Tendinopathy
Uncommon
Et: Due to chronic overuse or traumatic abduction(hind legs splay)
Often coexists with other hip conditions
Cs: Lameness, Hip pain during internal rotation or extension or medial palpation (inguinal area)
Dt: PE, US, MRI
Tx: NSAIDs, strict rest
reinjury very common
Pes Anserinus Contracture
Unilateral or bilateral
Et: Unknown
Muscles Involved: Sartorius, Gracilis, Semitendinosus
Sig: GSD
Cs: Ambulates like a horse with string-halt gait, Palpable thick, ropy band at muscle location, flicks/swings hind legs
Tx: NSAIDs, rest, irreversible!
Surgical resection not beneficial
Px: poor