Sleep health + Obstructive sleep apnea
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
What is a circadian rhythm?
is a biological clock which regulated bodies sleep / wake cycle
what are the factors involved in circadian rhythm
- input
-master clock (Core oscillator)
- output
where is the master clock for circadian rhythm found
can be found in the hypothalamus
what is the main hormone that regulates circadian rhythm and whats its role
as we reach the night cycle melatonin production increases, this is responsible for activating night cycle behaviours
what is the process of circadian rhythm activating wake cycle
- input --> sunlight will be recived by cells in the eye which transmit the message to the master clock
- master clock --> input received by hypothalamus which results in release of neurotransmitters which activate wake cycles
- output --> change of major organ behaviours for wake cycle
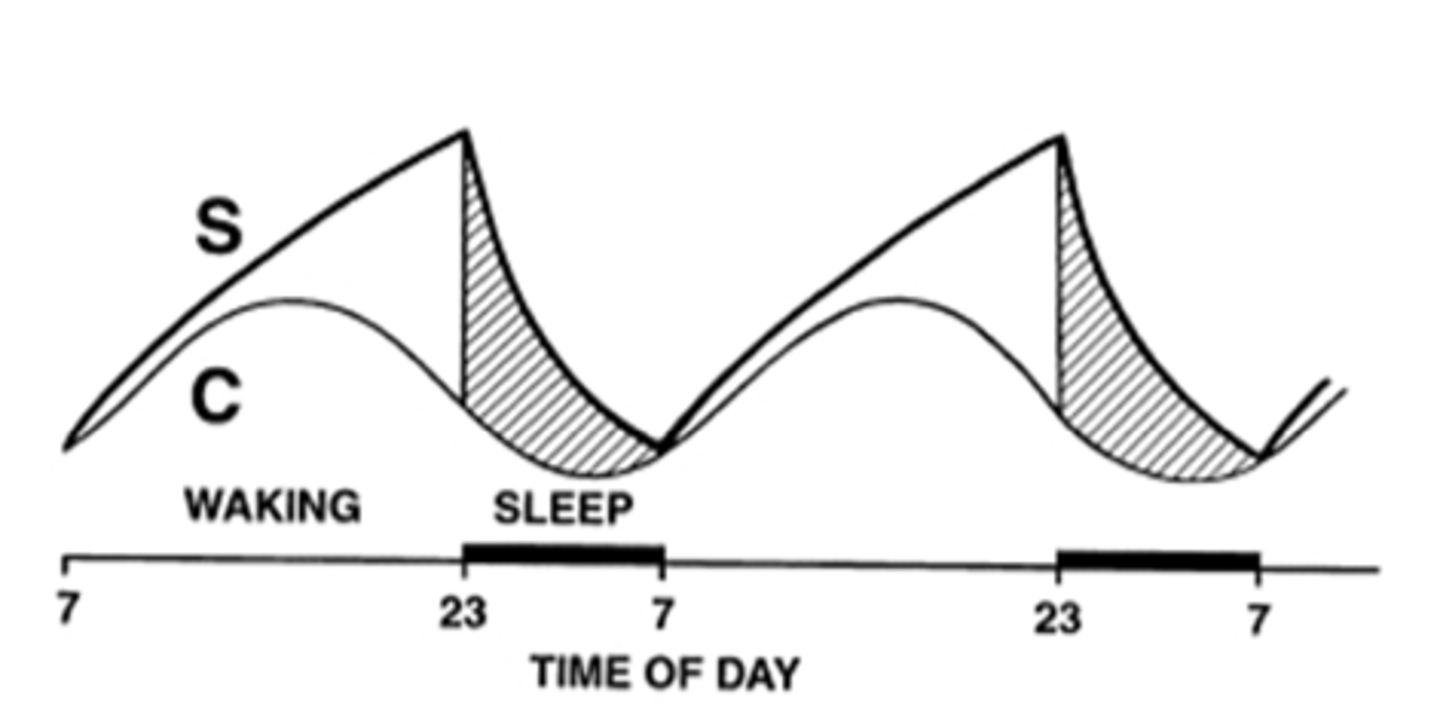
What is the homeostatic cycle
energy use will increase the energy debt as our day goes by, this energy debt will reach a max point where our sleep drive is at its highest
whats the link between circadian rhythm and homeostatic cycle
during moring --> energy debt and melatonin should be at its lowest
throughout day --> energy debt and melatonin will increase alongside each other
sleep time --> energy debt and melatonin should be at its highest
what is happening in our brain during awake phase
circadian system and activated clock genes will activate neurons in the brain which fire messages all throughout the brain which help you stay awake and do day activities
this is where sleep urge is at its lowest
whats happening in our brain during sleep phase
GABA neurons will inhibit wakefulness neurons increasing the sleep need and urge
why are orexin neurons important in our sleep cycle
orexin neurons are responsible for seperating our awake and sleep phases, preventing any sudden changes between phases
what can loss of function in orexin neurons cause
loss of function in orexin neurons can cause narcolepsy which is a condition that results in sudden changes in sleep phase, where someone who is awake can suddenly fall asleep
how can age affect sleep cycle
- sleep cycle can be fragmented resulting in frequent wake ups at night
- REM sleep is reduced
what is insomnia
Difficulty in falling asleep or staying asleep
what can cause insomnia
- Circadian process misalignment
- Delayed of advanced melatonin secretion
- Homeostatic process irregularities
- Maladaptive sleep health behaviours
- Over activity in neuronal circuits
what can cause circadian misalignment
when the circadin clock is alterd by factors such as
- light / dark cycles --> working night shifts can result in brain getting confused
- activation of metabolic pathways through late night snacking
your brain wants to activate sleep cycle but factors such as environment or lifestyle are interrupting it
what happens during homeostatic misalignment and how is it caused
homeostatic misalignment is when energy debt and sleep drive is at its max at unusual times
this can be caused as a result of
- poor sleep routine (sleeping to late at night and waking up late)
- poor sleep hygiene (eating late at night, exercising late at night, taking naps and drinking caffeine after mid day)
what are likely causes of delayed sleep phase syndrome
- delayed melatonin production which results in the person sleeping later at night
this is more prevalent in teenagers due to hormonal changes
what are the likley causes of Advanced sleep phase syndrome
- when the melatonin drive occurs to early causing people to sleep earlier
How should insomnia be diagnosed and seen asmaybe examinable
insomnia should always seen as a primary disorder that should always be treated, it should be considered a symptoms of other causes rather should be its own disorder
how can we diagnose someone with chronic insomnia
when a person is experiencing insomnia for more then 3 days a week for 3 months
what are long term issues with acute insomnia
acute insomnia can eventually lead to chronic insomnia, this can be due to the worry and anxiety generated by the person when trying to sleep, resulting in the person not being able to sleep due to overthinking it. This can alter sleep behaviour and result in mental disorders which leads to chronic insomnia.
what is the first line of treatment for insomnia
providing cognitive and behavioural treatments through referral and providing them with sleep hygiene tips
what are some behavioural tips for treating insomnia
Sleep hygiene:
- Go sleep and wake up same time
- No caffeine or alcohol after midday
- Not exercising in the evening
- Avoid napping
Stimulus control:
- If unable to sleep while in bed for 20 mins, get up and do a boring task away from the bed
Cognitive therapy:
- Addressing anxiety
how can benzodiazepines help with insomnia
benzodiazepines help activate GABA receptors in the brain which are responsible for inhibiting wakefulness cycle
what are some practice points for benzodiazepines
- should only be used for short term (2-4 weeks) due to tolerance
- can cause side effects such as blurred vision, dizziness, hangover sedation
how can orexin receptor antagonists drugs help with insomnia
are orexin receptor anatgonists help people stay awake by regulating change between sleep / awake cycles
therefore by disabling it people go into sleep cycle and fall asleep
how can antihistamines (H1 receptor antagonists) be used to help with insomnia
Blocking the H1 histamine receptors (responsible for mediating wakefulness) which as a result makes the person want to sleep
practice points of antihistamines
- should only be used for short term (around 3 days) due to tolerance
- avoid in elderly due to them being more prone to anticholinergic effects and chances of falls
- avoid in children <2 years
how can melatonin be used to help with insomnia
helps increase melatonin drive which will help the person go into sleep phase
what population should melatonin be used in
- elderly due to decreased melatonin drive
- Used in children with neurodevelopmental disorders which have abnormal melatonin's secretion (extended release formulation)
- for people who experience jet lag, night shift work and lifestyle habits that shift circadian rhythm
practice points of melatonin
- Melatonin should be taken around 2 hours before bedtime for optimal effect
- avoid in hepatic impairment
s
f
what is sleep apnoea
temporary cessation of breathing during sleep
what are the two types of sleep apnea
obstructive sleep apnea and central sleep apnea
what is the pathophysiology of sleep apnea
when we go into our sleep phase, the tone in our muscles will relax. Muscles in the upper airway such as tounge and uvula when relaxed are pushed by gravity and form a obstruction in the airways
when the person is not able to breathe the high CO2 levels in the body are detected by receptors which send signals tor the brain that they are not breathing
the body will experience a micro arousal (short period of wakefulness) where the body starts breathing again
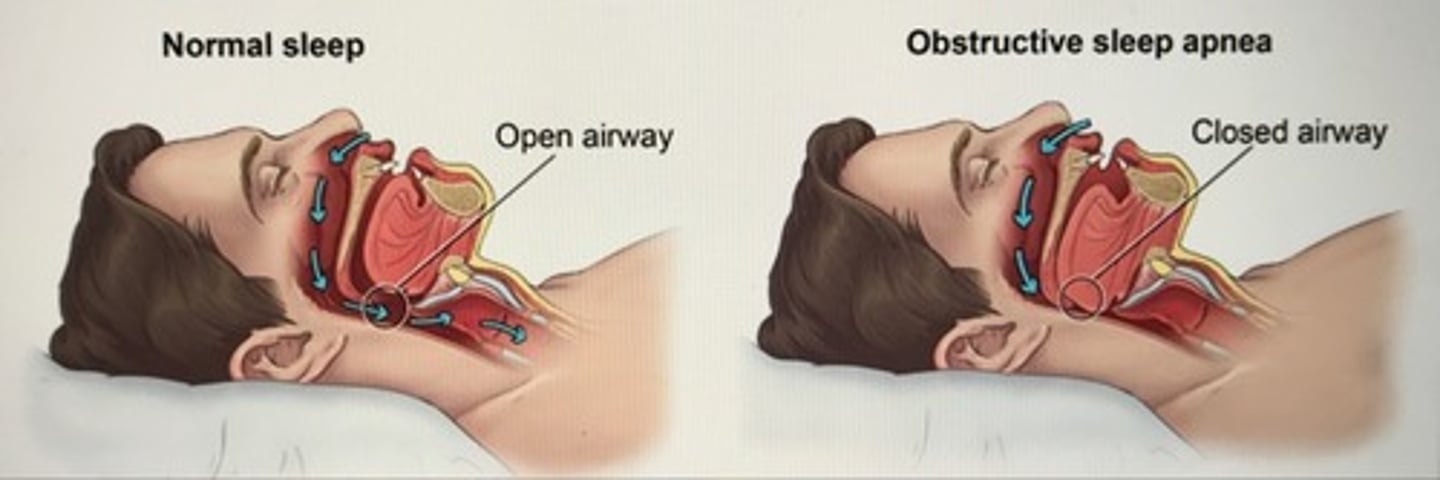
what is the difference between central and obstructive sleep apnoea
central --> the problem is associated with function of the body
obstructive --> the issue is the lack of space in upper airways
what are some reasons for obstructive sleep apnoea
Obesity (presence of fat)
Presence of tumour
Infection in airways causing inflammation
what are some reasons for central sleep apnoea
Upper airway muscle control
Miscommunication between lung and brain resulting in poor respiration control
how can we diagnose sleep apnoea
through polysomnography (PSG) test
what does the polysomnography (PSG) test consist of
the PSG test consists of a variety of channels which measure different outcomes such as:
- electroencephalography (EEG),
- electro-oculography (EOG),
- electromyography (EMG),
- pulse oximetry (SpO2),
- electrocardiography (ECG) and
- measurement of respiration and respiratory movements
what are the different type of sleep studies and what do they measure
Type 1 → in lab PSG test which is the diagnostic gold standard which includes 12 channels being measured
Type 2 → a portable home based diagnostic which is acceptable as a diagnostic test (measures at least 7 channels)
Type 3 → measures around4 channels
Type 4 → single channel measurements
what is hypopnoea
when there is a reduction in ventilation by at least 50% which also causes O2 saturation levels to decrease by 4% or more
at which stage of sleep does apnoea usually occur
during REM sleep since the tone of muscles decreases during this time
what do we use to categorise obstructive sleep apnoea
apnoea- hypopnea index
what is the apnoea- hypopnea index equastion
AHI = no. of apneas + hypopneas / total sleep time in hours
what categories of apnoea- hypopnea index are there for obstructive sleep apnoea
AHI values <5 --> normal
AHI values 5-14 --> mild
AHI values 15-29 --> moderate
AHI values 30> --> severe
when a person experiences sleep apnoea what happens in the body
Increased heart rate → due to low O2 levels the heart pumps harder so more oxygen reaches each organ
Hyperventilation
Increased glucose levels → release of glucose so the body has energy to increase heart rate
what are some health consequences associated with frequent sleep apnea
- insulin resistance (due to constant release of glucose during sleep to provide energy for heart rate)
- hypertension --> increased heart rate
- cardiomyopathy
- heart failure
- stroke
- pulmonary hypertension
- depression
- glucose intolerance
what are symptoms of obstructive sleep apnoea
- Loud snoring
- Daytime sleepiness'
- Poor sleep quality
- Morning headache
- ↓libido
- Nocturia
-↓memory concentration
what are some risk factors of obstructive sleep apnoea
- males
- obesity
- smoking
- age
- alcohol
to what patients is the CPAP machine gold standard treatment for
CPAP machine is gold standard treatment for patients with moderate to severe obstructive sleep apnoea
for a patient with mild to moderate obstructive sleep apnoea what is the typical treatments
Mandibular advancement splints (MAS) and nasal EPAP (not much evidence)
what types of surgeries are availbe for people with obstructive sleep apnoea
bariatric surgery --> for really obese patients, heling them lose weight
upper airway surgery --> suitable for most OSA patients
tonsillectomy --> useful for children, helping with large tonsils
what are some lifestyle managements of OSA
losing weight, stopping smoking and alcohol
what is CPAP
continuous positive airway pressure -- a means of continuously blowing positive air into the airway to prevent airway collapse or to help alleviate difficulty breathing
gold standard for OSA in moderate to severe cases
what equipment is found in a CPAP
the CPAP consists of a machine which sucks in room air and pressurises it for inhalation
humidifiers are also present to prevent cold dry air from reaching the lungs
the pressurised air can then travel through tubing and into a mask worn by the patient
what are some types of CPAP machines
- auto set algorithm --> smart machine that detects when apnea occurs and measures how many times it occurs
- manual titration --> manually choosing the pressure at which the machine will produce to keep airways open
what are some problems with CPAP machines
Adherence
Side effects- nasal dryness, dry mouth, pressure sores, infections
Social/lifestyle, attitude
Expense
Psychological- claustrophobia
how can patients care for CPAP
Tubing inspection
Mask care, new masks
Filters
Machines
what is the PALM model
a model which consists of 4 variables which are measured in an individual.
these variable can differ between patients which expresses different types of phenotypes
what is the P in the PALM model
Pcrit → is the critical pharyngeal pressure, which determines at what pressure causes the airways to close (the pressure at which closes the airways will differ between patients)
what is the best treatment for patients with a high pcrit value (phenotype)
since the pharyngeal collapse is the main problem the CPAP machine is most effective
what is the M in PALM model
muscle responsiveness --> the muscles which hold the airways open are not functioning well
what is the best treatment for patients with low muscle responsiveness (phenotype)
a way to stimulate the muscles
what is the L in PALM model
Loop Gain --> the bodies reaction to a change in the respiratory system (e.g., amount of oxygen in the body)
having a high loop gain means that the body overexaggerates to the smallest changes in the respiratory system
causing them to wake up to easily
the ventilatory response (waking up and increasing breathing) is to much for the ventilatory changes (decreased ventilation, obstruction) that have occurred in the body
what is the A in PALM model
Arousal --> where very small changes in a persons body causes them to wake up
easily woken up
what are some pharmalogical treatments for patients with low arousal threshold (phenotypes)
sedatives
what are some pharma logical treatments for patients with unstable loop gain (phenotype)
Carbonic Anhydrase Inhibitors e.g.
acetazolamide
what are some pharma logical treatments for patients with upper airway collapsibility (phenotype)
Desimipramine (TCA)
Fluticasone, Leukotriene Receptor Antagonists
REM Sleep (antidepressants, clonidine)
Muscarinic tone to reduce REM based UA muscle inactivation e.g. donepzil
Cannabinoids CB1 and CB2 receptor agonists