GENETICS EXAM #2: Immunogenetics, GENETIC EXAM #2: Wiskott Aldrich Syndrome, GENETICS EXAM #2: Inborn Errors of Metabolism, GENETICS EXAM #2: Developmental Genetics
1/149
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
150 Terms
What are the main contributors to cellular immunity?
T regulatory cells, cytotoxic T cells, and memory T cells
What are the main contributors to humoral immunity?
Memory B cells and plasma cells
Which type of immunity is absolutely essential in fighting off bacteria?
Humoral
In addition to the MHC molecule and foreign peptide, humoral immunity requires _______________________ molecules.
Costimulatory
Which part of the antibody binds to the antigen?
Variable region
The constant region of the antibody is constant among...
Classes
Ex: all IgG have the same constant region
What holds antibodies together?
Disulfide bonds
What is the variable region of the antibody made up of?
Heavy and light chains
What are the four parts of the T cell receptor?
Variable region
Constant region
Joining region
Diversity region
The constant region of the T cell receptor is plugged into the _______________.
Bilayer
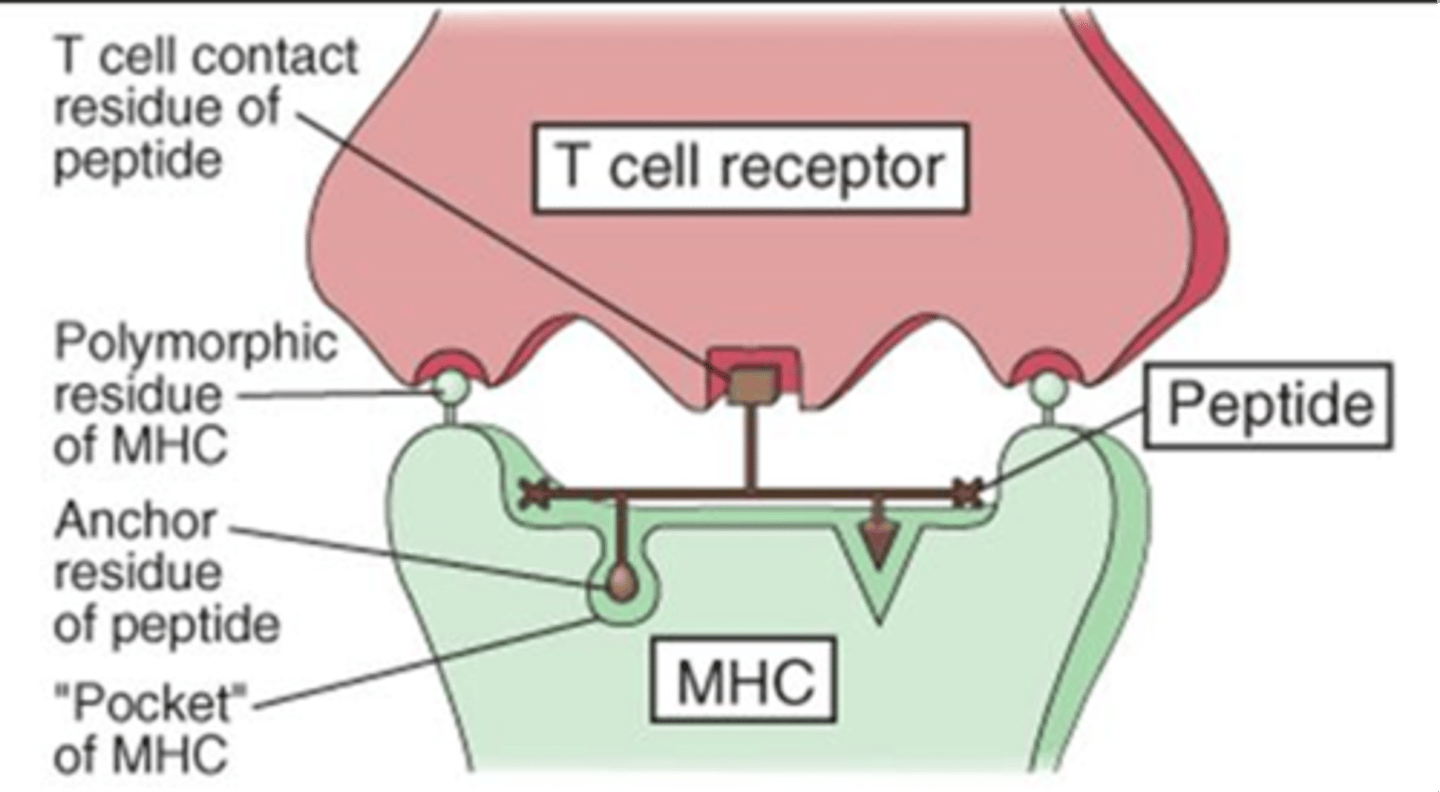
True or False: The way in which an antigen peptide is presented can vary from person to person depending on the way MHC binds the antigen
True
Ex: In the picture, MHC binds triangle and circle and presents square. But in another person, it might bind triangle and square and present circle.
Why don't T cells respond to self MHC + self Ag?
No costimulatory molecules
Which MHC alerts CD8+ T cells in the case of a viral infection?
MHC I
What is the key factor in determining tissue matching for transplant donors and recipients?
MHC
MHC molecules have a ______________ (broad, narrow) specificity for peptides, meaning many different antigens can bind within the ______________ (same, different) binding cleft.
Broad; same
Peptides associated with MHC have a ______________ (slow, fast) on and off rate
Slow
True or False: MHC molecules discriminate from self and foreign peptides
False; they do NOT discriminate, they only recognize amino acid sequences
The MHC _____________________ of an individual determines which peptides bind and how peptides bind.
Haplotype
MHC was originally only linked to ________________________ but was later found to be critically important to all _________________________________________________.
Graft rejection; immune responses involving protein antigens
MHC is also known as...
HLA (human leukocyte antigen)
MHC genes are highly...
Polymorphic
They are actually the most polymorphic genes in the human genome
MHC alleles are _______________________ expressed.
Codominantly
Both maternal and paternal MHC genes are expresed in offspring (haplotype)
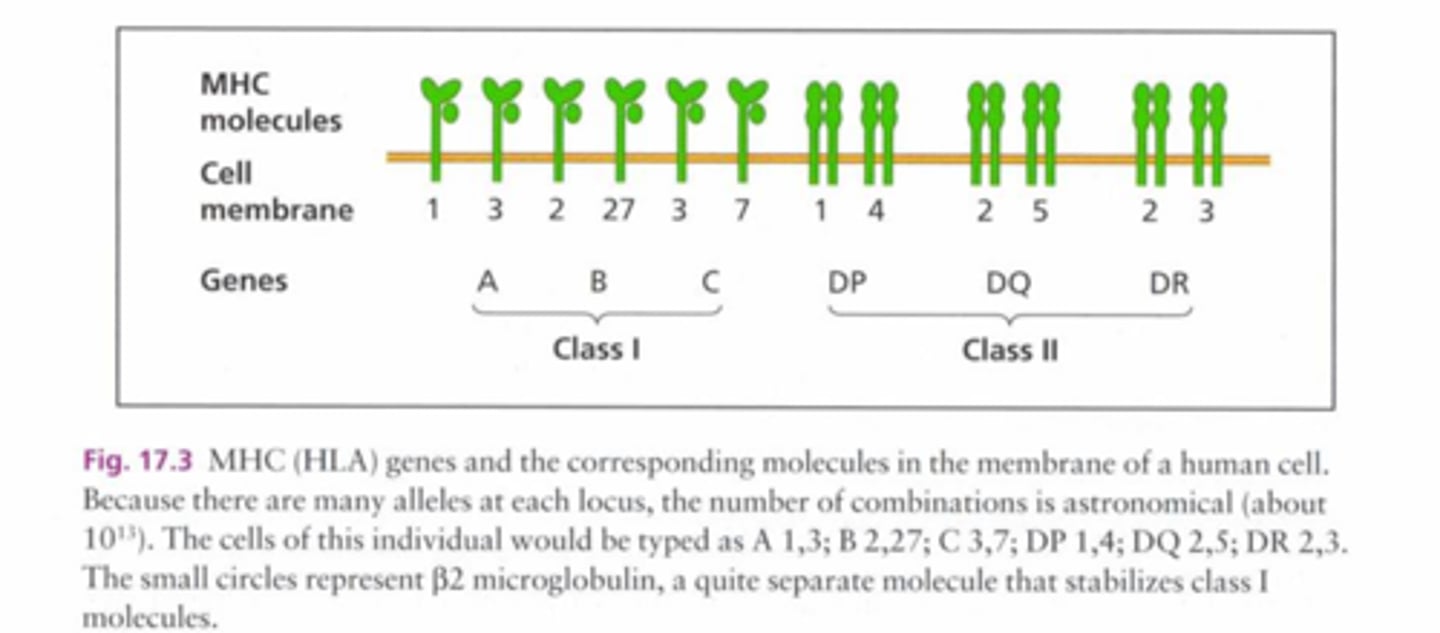
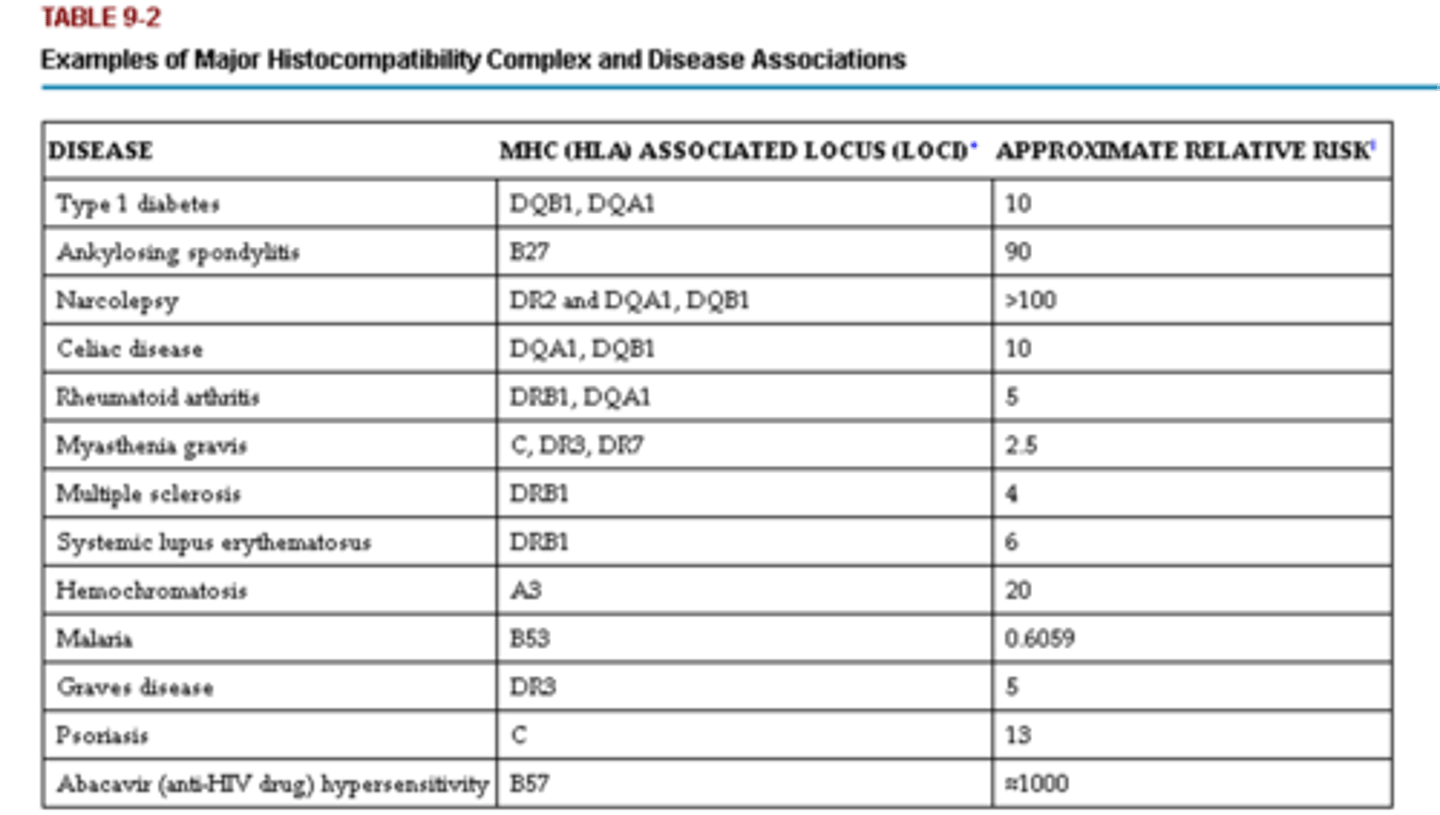
What can MHC haplotype influence?
- How an individual responds to certain pathogens
- Susceptibility to certain diseases
- Transplant success
______________________ diseases are often associated with HLA.
Autoimmune
True or False: It is possible to see a complete deficiency in macrophages
False; you will NEVER see a complete deficiency in macrophages (it is incompatible with life), but you can see it with lymphocytes
Describe primary or congenital immunodeficiencies
- Genetic defects that result in increased susceptibility to infection
- Frequently manifested in infancy and childhood
- Affect about 1 in 500 people in the US
Describe secondary or acquired immunodeficiencies
Develop as a consequence of:
- Malnutrition (alcoholics)
- Disseminated cancer
- Treatment with immunosuppressive drugs (steroids)
- Infection of cells of the immune system (HIV)
Any loss-of-function mutation affecting a ____________________________ has negative consequences for survival.
Toll-like receptor (TLR)
How might immunodeficiencies result?
- Defects in ___________
- Defects in ____________
- Defects in leukocyte maturation or activation
- Defects in effector mechanisms of innate or adaptive immunity
What can help predict the type of immunodeficiency?
The type of recurring infection a patient experiences
Deficient ______________________________ usually results in increased susceptibility to infection by pyogenic bacteria.
Humoral immunity
What was the first primary immunodeficiency disease to be described?
Bruton (X-linked) agammaglobulinemia (XLA)
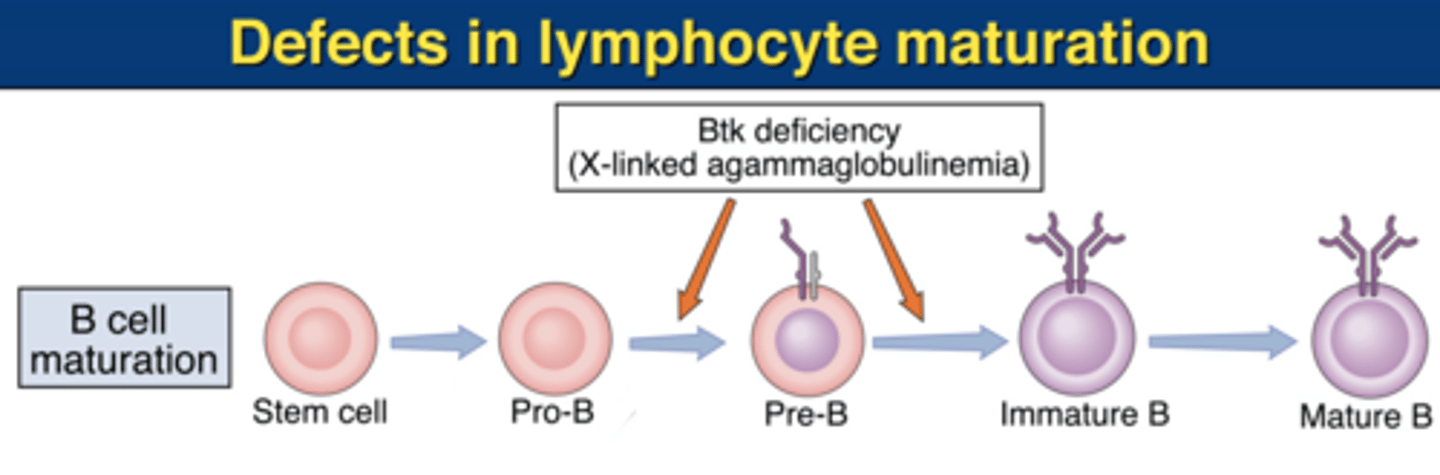
Describe XLA
- All antibody isotypes are very low
- Circulating B cells are usually absent
- Pre-B cells are present in reduced numbers in the bone marrow
- Tonsils are usually very small and lymph nodes are rarely palpable due to absence of germinal centers
True or False: In XLA, the thymus and other T cell dependent areas of spleen and lymph nodes are normal
True
Why do most boys with XLA not show symptoms for the first 6-9 months of life?
The presence of maternally transmitted IgG antibodies
Loss of function of Bruton Tyrosine Kinase
Important in pre-B cell expansion and maturation into Ig-expressing B cells
what defect does this describe?
XLA
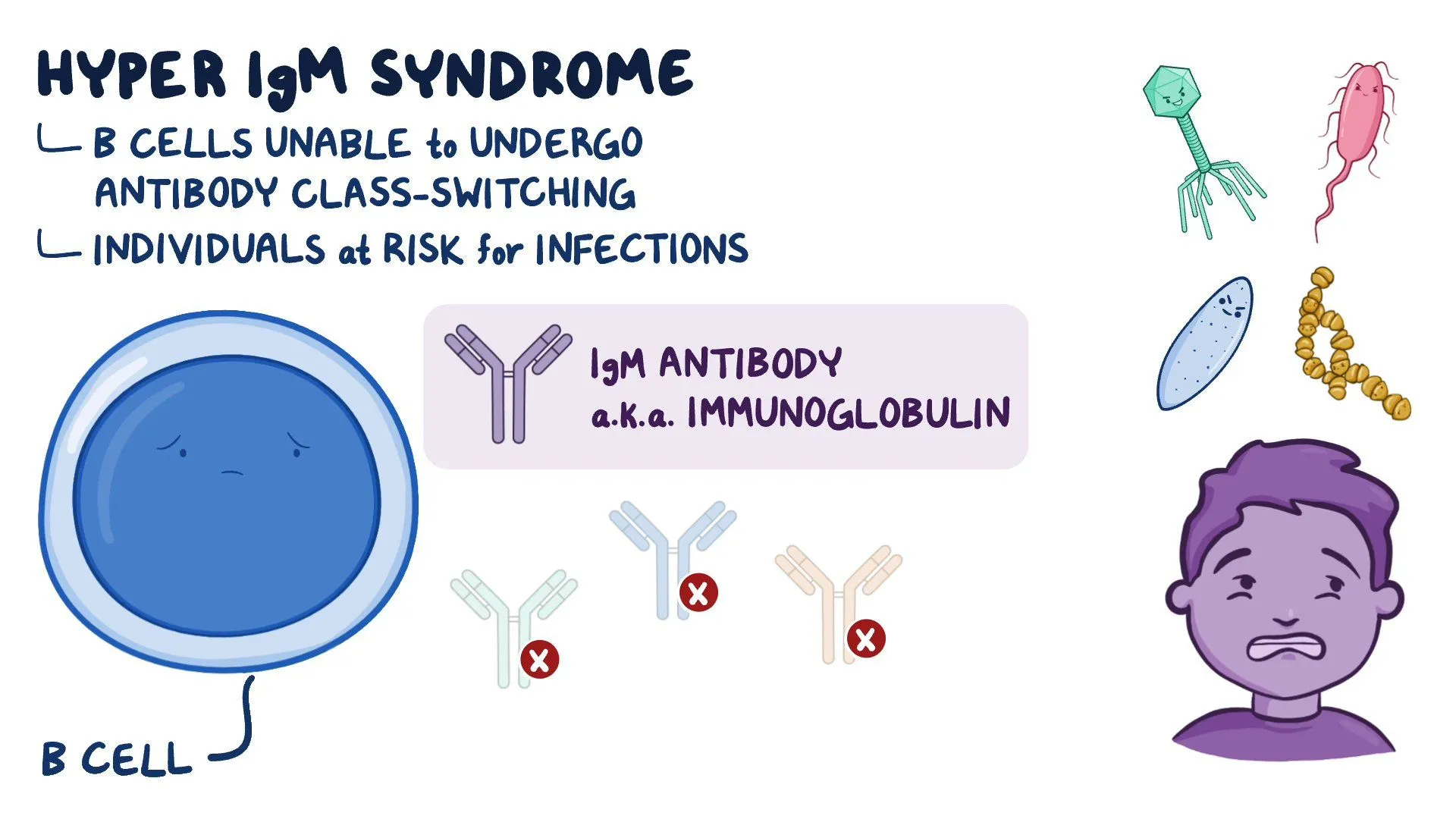
Very low serum IgG, IgA, and IgE
Elevated concentration of polyclonal IgM
Recurrent pyogenic infections within the first ot second year of life (otitis media, sinusitis, pneumonia, tonsillitis)
this describes which immunodeficiency?
X-linked immunodeficiency with hyper-IgM
In contrast to patients with XLA, hyper-IgM patients have _________________________________.
Lymphoid hyperplasia
What is the defect in X-linked immunodeficiency with hyper-IgM?
Loss of function of CD40 ligand (CD154) that is expressed on helper T cells
Prevents the T cell from co-stimulating antigen-specific B cells
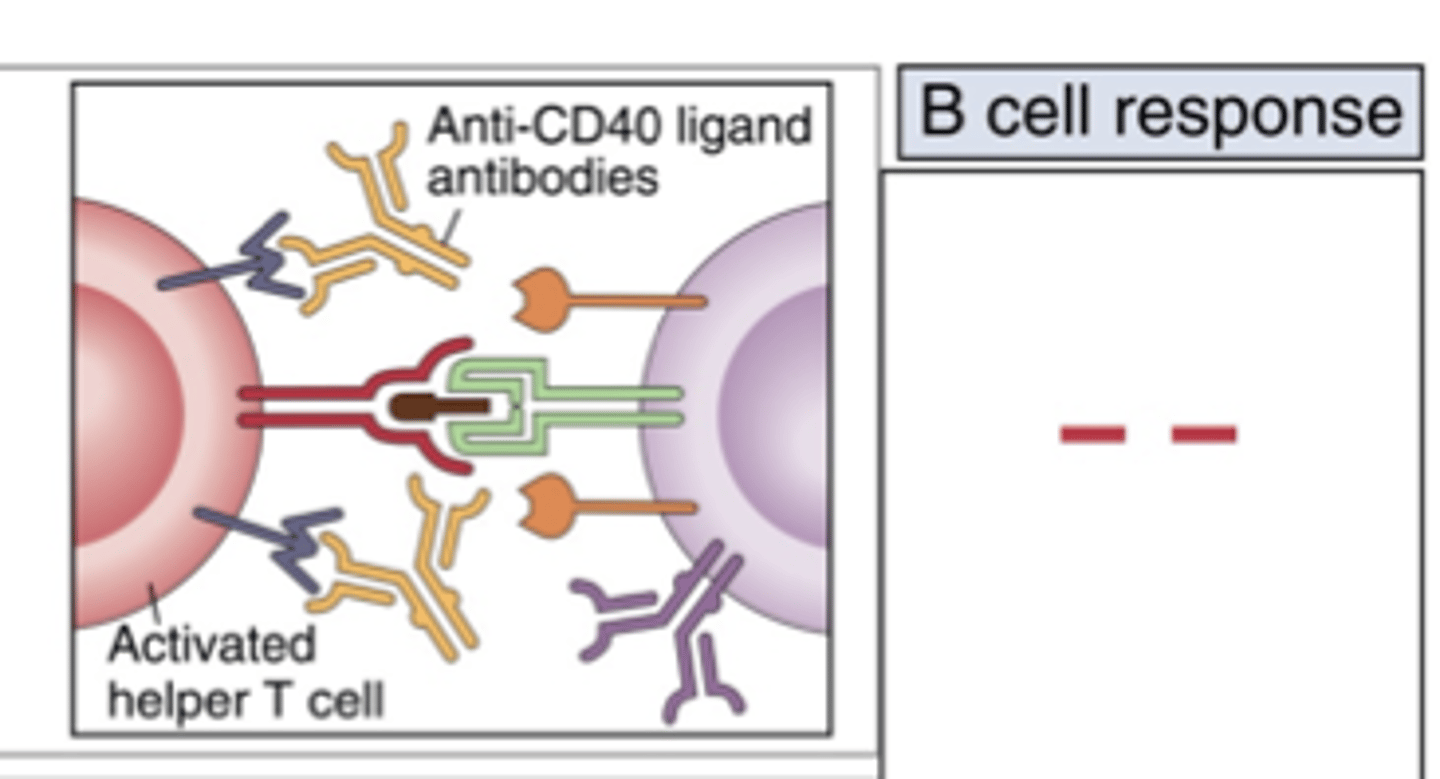
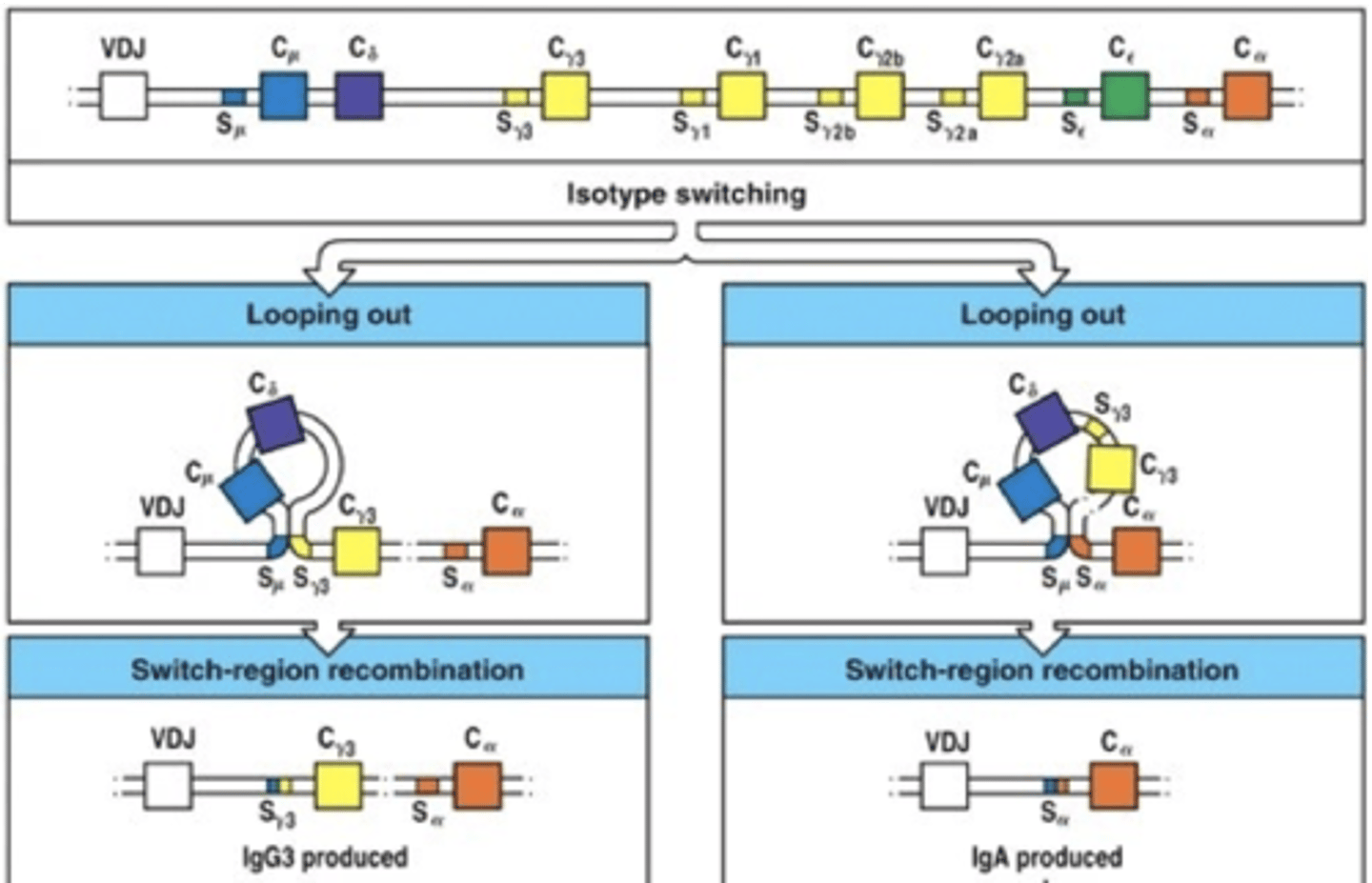
In hyper-IgM, B cells are not signaled to go through ________________________ and therefore only produce IgM.
Isotope switching
What is the treatment for XLA or hyper-IgM?
Prophylactic antibiotics and/or gamma-globulin therapy
Deficient ______________________________ usually results in increased susceptibility to viruses and other intracellular pathogens.
Cell-mediated immunity
True or False: There are many treatments for deficient T cell responses
What is the survival rate for T-cell defects?
False; it is rare that patients with absolute defects in T-cell function survive beyond infancy or childhood
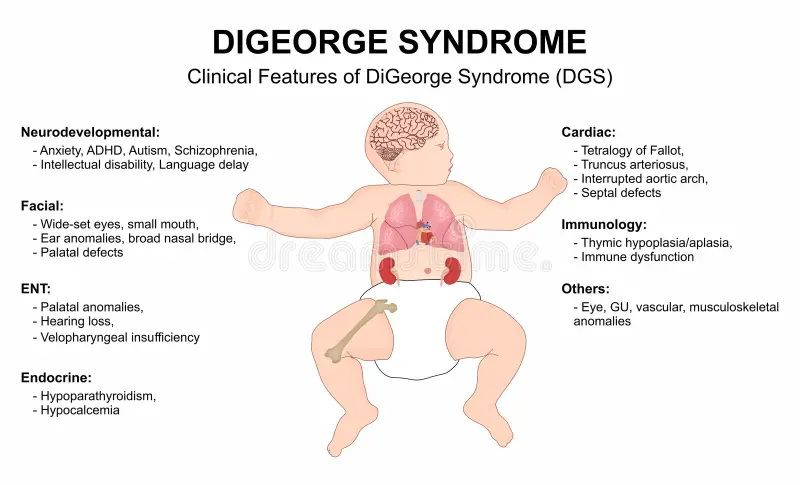
What is DiGeorge's syndrome?
Developmentally-related disease associated with tissue morphogenesis
Thymus never develops (along with many other important structures and vasculature)
In DiGeorge's syndrome, the percentage of T cells is variable ____________________ (increased, decreased), resulting in a relative _____________________ (increase, decrease) in percentage of B cells.
Decreased; increase
There are clinical similarities between DiGeorge's syndrome and __________________________________.
Fetal alcohol syndrome
What is X-linked Recessive Severe Combined Immunodeficiency Disease (XSCID)?
What is the fundamental problem with the T cells making them self-delete?
Rare, fatal syndrome characterized by profound deficiencies of T- and B-cell function
T cells can be made but receptors are nonfunctional, so they get deleted, and B cells cannot be helped
Patients with XSCID have persistent infections with ________________________ organisms.
Opportunistic (candida albicans, pneumocystis carinii, varicella, measles, parainfluenzae, cytomegalovirus, and EBV)
Patients with XSCID are at risk for ______________ as a result of maternal T cells that cross into fetal circulation.
GVHD; they lack the ability to reject foreign material
XSCID patients have few or no __________________ cells and elevated ____ cells.
T and NK; B
Why don't the B cells in XSCID patients produce immunoglobulin normally?
No T cell help; function is not helped even after T-cell reconstitution of bone marrow
_____________________________ is currently the treatment of choice for various immunodeficiency diseases.
Bone marrow transplantation
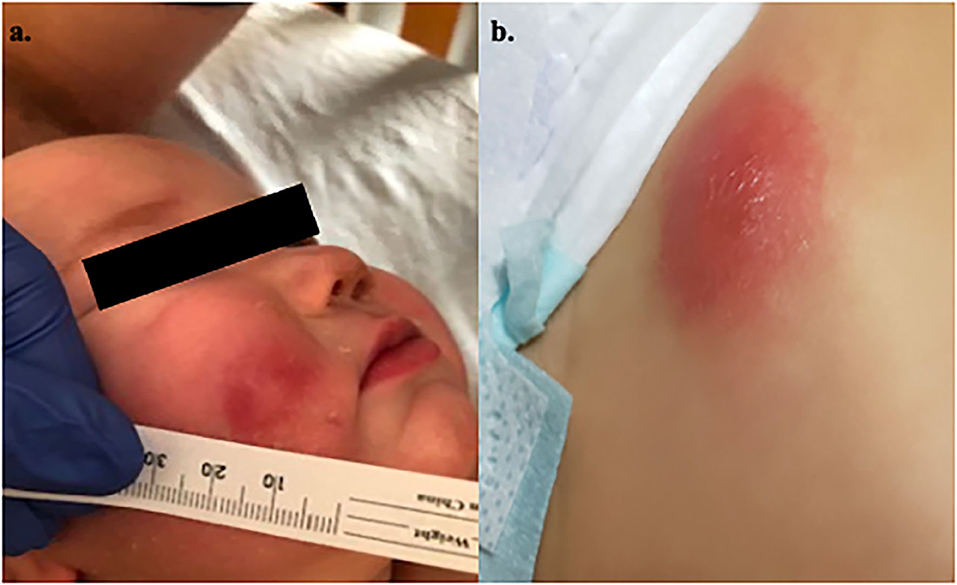
What type of immunodeficiency disorder is Wiskott Aldrich Syndrome Classified?
X-linked primary immunodeficiency disease

What symptoms are typically present in patients with Wiskott Aldrich Syndrome at diagnosis?
Recurrent infections, eczema, microthrombocytopenia
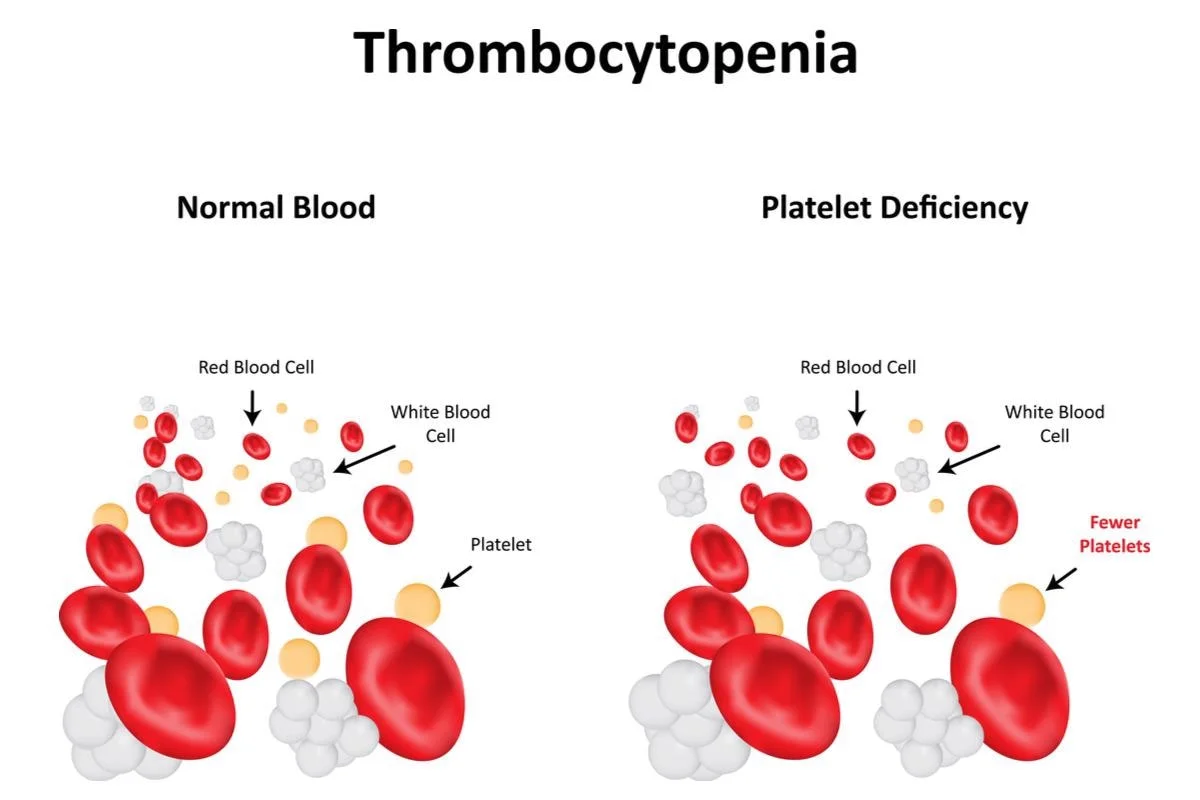
What finding is pathognomonic for WAS?
small platelets in the context of thrombocytopenia
What is the gold standard in the diagnosis of WAS?
Genetic analysis
What treatments are indicated for patients with confirmed WAS?
hematopoietic stem cell transplantation (HSCT) or stem cell gene therapy (GT)
Phenylketonuria (PKU) is a disorder of _________________________ metabolism that results in a build up of _________________________ and deficiency of __________________________.
Amino acid; phenylalanine; tyrosine
True or False: Children with PKU present with symptoms acutely
False; it is an insidious disease
What is the first disorder screened for at birth?
PKU
- Musty odor
- Light features (complexion, hair, eyes)
- Eczema
- Early on: ID
- Later on: psychiatric/behavioral issues
Clinical features of PKU
Lack of proper dietary therapy during pregnancy resulting in infant's microcephaly, mental retardation, growth retardation and congenital heart defects
maternal PKU
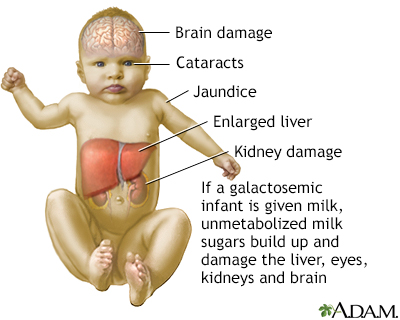
Galactosemia is a disorder of ____ metabolism.
Carbohydrate
What is gastrulation?
Rearrangement of the single layer into trilaminar structure
- Ectoderm
- Mesoderm
- Endoderm
What is the key feature of gastrulation? When does it form?
Primitive streak; 14-28 days
What is neurulation?
- Folding process that turns the neural plate into the neural tube
- Separation of the ectoderm into neural tube, epidermis, and neural crest cells
Closure of the neural tube occurs at _____ different sites.
5; it doesn't just zip up, which helps to explain spina bifida
What are the components of the mesoderm?
Notochord, dorsal mesoderm, intermediate mesoderm, lateral mesoderm, and head mesenchyme
What does the notochord form?
Neural tube and body axis
What does the dorsal mesoderm form?
Axial skeleton, skeletal muscle, and connective tissue
What does the intermediate mesoderm form?
Kidneys and GU
What does the lateral mesoderm form?
Heart, viscera, and body wall
What does the head mesenchyme form?
Eyes and head muscles
Because there are many genes active during this time, errors in _______________________ are likely culprits of birth defects.
Gastrulation
What does the endoderm form?
Lining of digestive tract, lining of respiratory tree, and lining of middle ear, thymus, parathyroids, and thyroid
The primitive streak creates the ___________________________________ axis.
Anterior/posterior
___________________ expression initiates and maintains the primitive streak.
Nodal
________ genes are key for positioning of cells and tissues.
Hox
Mutations in Hox genes can cause abnormalities of ___________ function.
Limb
What are the other axes?
Ventral/dorsal, medial/lateral, left/right
Proper internal organ development relies on the ______________ axis.
Left/right
What is situs solitus?
Normal position of thoracic and abdominal organs
What is situs inversus?
Left-right reversal of organ placement
What is situs ambiguous? Which organs does it affect the most?
Describes anatomy that falls in between situs solitus and situs inversus (kind of like a mirror image)
Affects the heart and spleen the most
True or False: There is significant overlap between brain and skull structure development
True
Which gene directs craniofacial development?
HOX genes
- Directs function and movement of the cells
- Precursors to muscles and bones of the head and neck
Prevalence of limb defects are second to only what?
Heart defects
Limb development is _____________ and involves multiple _____________.
Complex; axes
The limb is derived primarily from the ___________________ and consists of ___________________ and _________________ plates.
Mesoderm; somitic and lateral
What is the first step of limb development?
Induction of fore- and hind-limbs
What influences progression of the limb?
Apical ectodermal ridge
- Stimulates proliferation of mesodermal cells
What specifies anterior/posterior information in limb development? What is this key for?
Zone of polarizing activity
- Key for thumb-finger differentiation
Holt-Oram Syndrome
Hereditary syndrome of malformations of the heart and upper extremities
- Often more severe in left than right
- Sloping shoulders and restricted movement at the joint
- Congenital heart disease and cardiac conduction disease (heart block w/ or w/o afib)
Cells with a common function become...
Tissues
Organogenesis can only happen once...
Axes are established
When do organs form?
When common cells and tissues collaborate for a unified function; signal exchange between tissues promote growth and differentiation
Skeletal formation is dependent upon _______________________.
Osteoblasts
Cleidocranial dysostosis
Defects of the skull and clavicle due to imperfect ossification
- Open fontanelle
- Hypertelorism (wide set eyes)
- Absent clavicles
What is ectopic expression?
Expression of a gene in a place or at a time where/when the gene is not normally expressed
What is a malformation?
Defects due to intrinsically abnormal development
- 3-5% of newborns
- 1% of newborns have multiple malformations (usually indicates a syndrome or cause)