Mullerian Development and Abnormal Puberty
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
How does embryologic development occur?
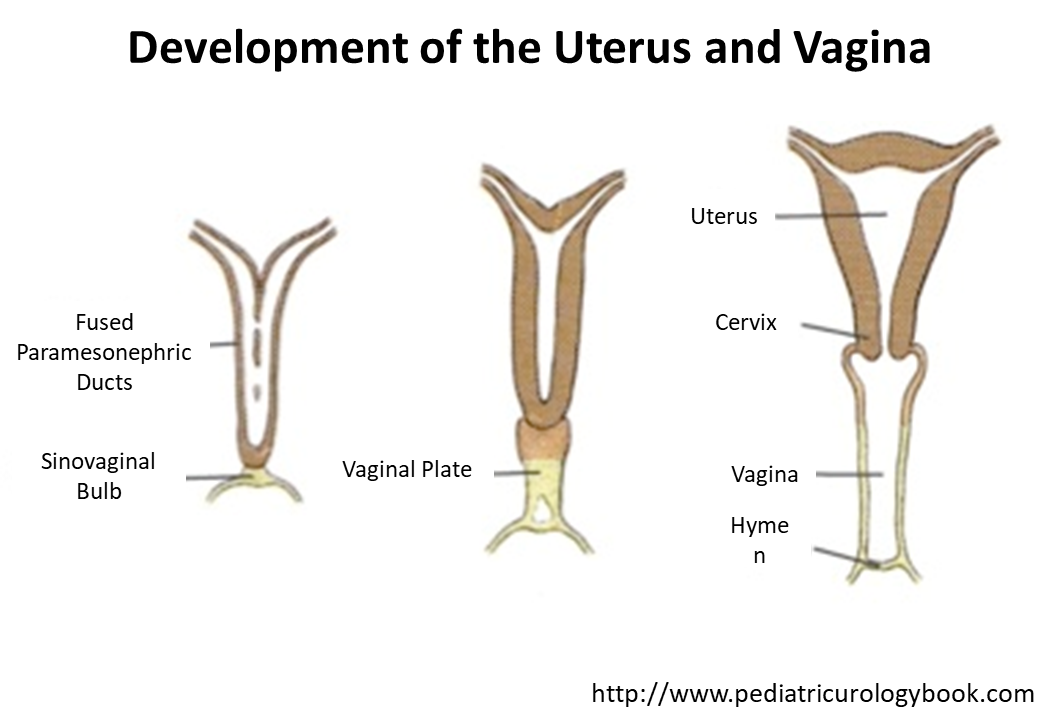
In the absence of an Y chromosome and Mullerian Inhibiting Hormone, the undifferentiated gonads will develop into the female reproductive system through influence of things like the WNT gene
1) Mullerian Ducts/paramesonephric ducts will meet midline fusing together and then grow caudally to fuse with the urogenital sinus
→ Mullerian gives rise to the fallopian tube, uterus, upper vagina and cervix
→ Urogenital Sinus gives rise to the vagina and hymen with its development being dependent on estrogen
What are the physiologic changes that occur in female puberty?
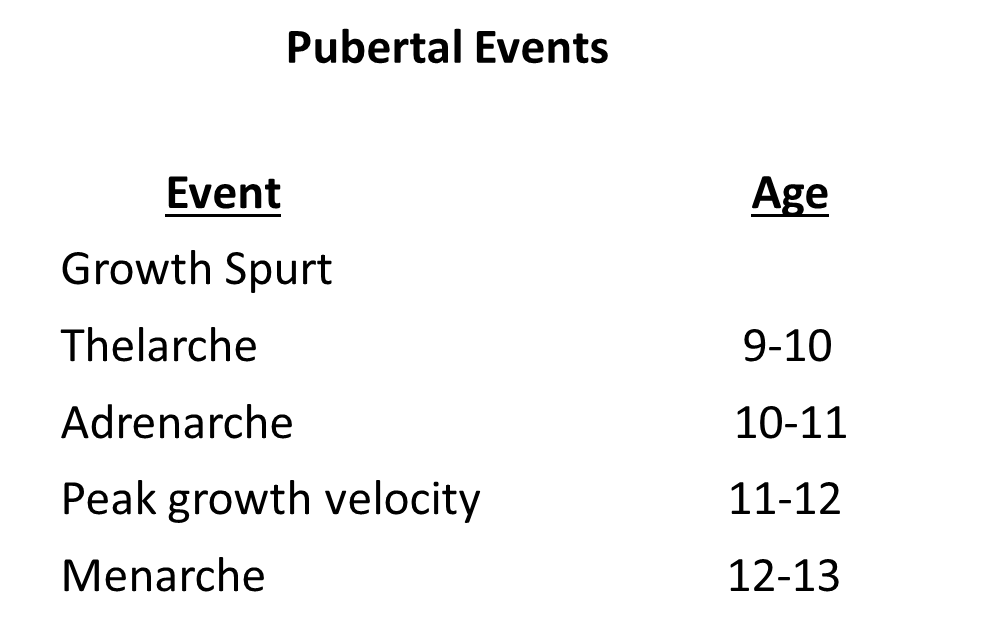
Puberty onset occurs in 9-13 years old in females and follows an ordered sequence over around 4-5 years
1) Increase in growth velocity (first clinical sign)
2) Breast budding (thelarche)
→ thelarche and adrenarche can be switched depending on your genetics/ethnicity
3) Pubic hair (adrenarche)
→ while most of these are made by increasing estrogen, this one is caused by increase in androgen levels
4) Peak growth velocity
5) Menarche (first period)
What is the difference between gonadarche and adrenarche?
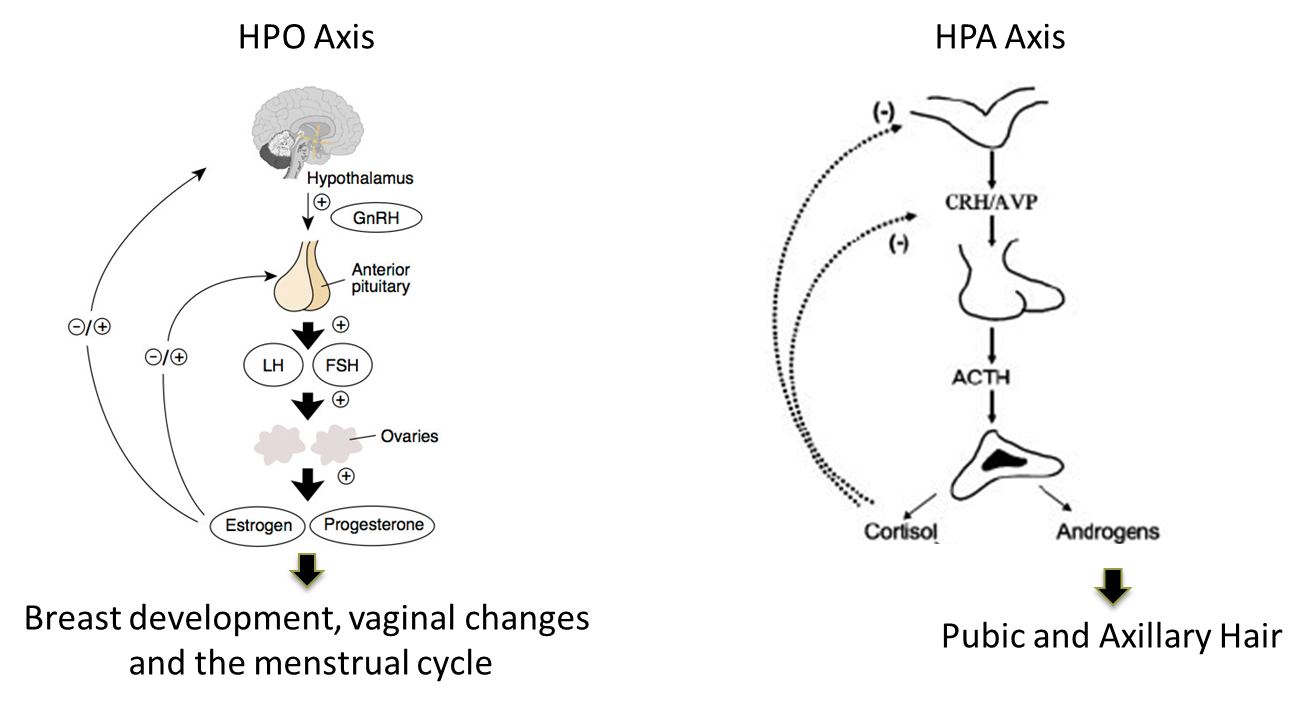
1) Gonadarche is the activation of the HPO axis leading to increased release of GnRH
→ leads to an increase in LH and FSH leading to increased androgen to estrogen production
→ causes thelarche (breast development) and menarche as well as the majority of the secondary sexual female characteristics
2) Adrenarche is the activation of the HPA axis going to the zona reticularis to upregulate androgen secretion
→ makes our pubic hair, acne and body odor
What is precocious puberty?
Precocious puberty is defined as secondary sex characteristics prior to age 7 or a menarche before age 9
→ can be central (CNS) or peripheral (gonads, endocrinopathy, exogenous)
What is Central Precocious Puberty?
Central Precocious Puberty is the early onset of puberty that follows the same pace and order as normal puberty and is Gonadotropin releasing hormone dependent
1) While the majority of the time it is idiopathic some causes are congenital defects or tumors
2) Treated with observation or suppression of the HPO axis
→ leuprolide-acetate/histrelin are GnRH agonists that suppress the HPO axis
What is Peripheral Precocious Puberty
Peripheral Precocious Puberty is GnRH independent with hormonal stimulation coming from a different source
1) Patients will also have progression that does not match regular puberty
→ often will be incomplete, being either thelarche alone or adrenarche alone
2) Typically caused by a estrogen expression without HPO activation
→ exogenous exposure
→ Primary hypothyroidism (treated with levothyroxine)
→ McCune Albright syndrome
What is McCune Albright Syndrome

McCune Albright Syndrome is caused by defect in GNAS gene leading to constitutively active adenylate cyclase
1) It is spontaneous mutation that exhibits mosaicism of expression
→ treated with selective estrogen receptor modulators and aromatase inhibitors
2) Patients will have precocious puberty and cafe-au-lait spots
→ patients also have polyostotic fibrous dysplasia (bone is replaced with fibrous scar tissue)
→ cafe-au lait spots will not cross midline and have a bumpy “coast of Maine border”
How to evaluate and treatprecocious puberty?
1) Perform a wrist X-ray in order to perform a bone-age
→ if their bone age is advanced compared to their age, they probably have precocious puberty
2) Make sure to check estrogen levels as well as thyroid levels
→ hypothyroidism can cause precocious puberty
3) Imaging for potential CNS lesions
4) Make sure to make sure the kids are able to match their peers and not feel ostracized for going through puberty early
→ also try to maximize their height
What is Primary Amenorrhea?
Primary Amenorrhea is the absence of menarche by age 15 and can be structural or hormonal
→ if a patient lacks secondary sexual characteristics it is more than likely to be hormonal in origin
1) Structural - lack of a reproductive tract structure that prevents you from having a period
→ abnormal Mullerian structures
→ defective vaginal development
2) Hormonal issues
→ HPO dysfunction
→ Ovarian or Pituitary dysfunction
What is Congenital Absence of the Uterus?
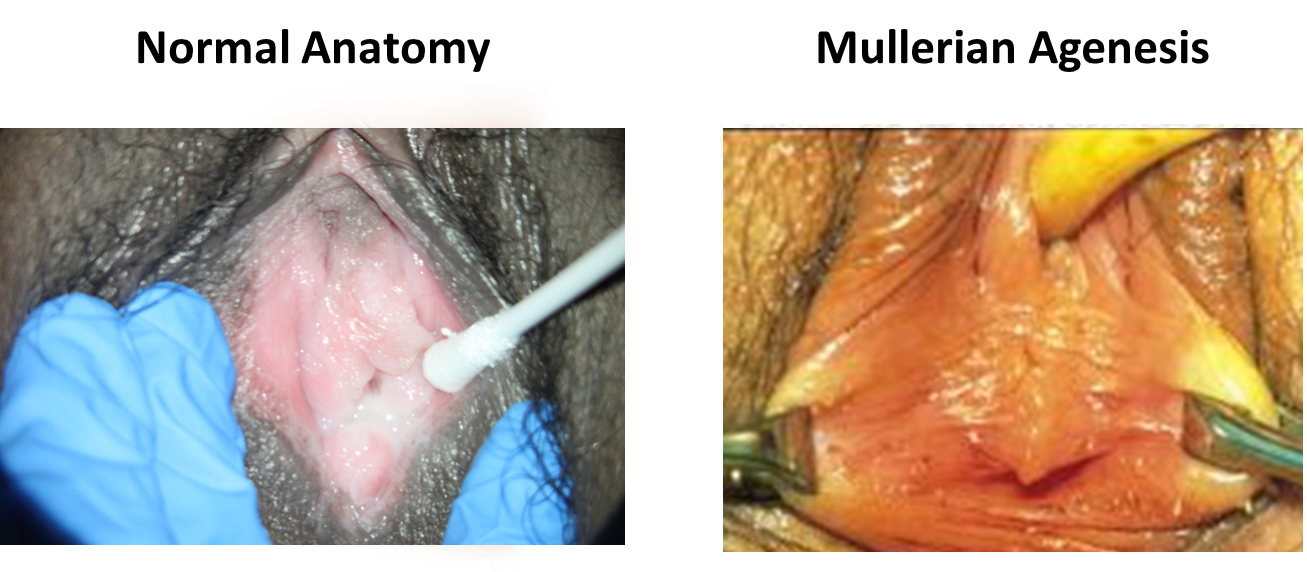
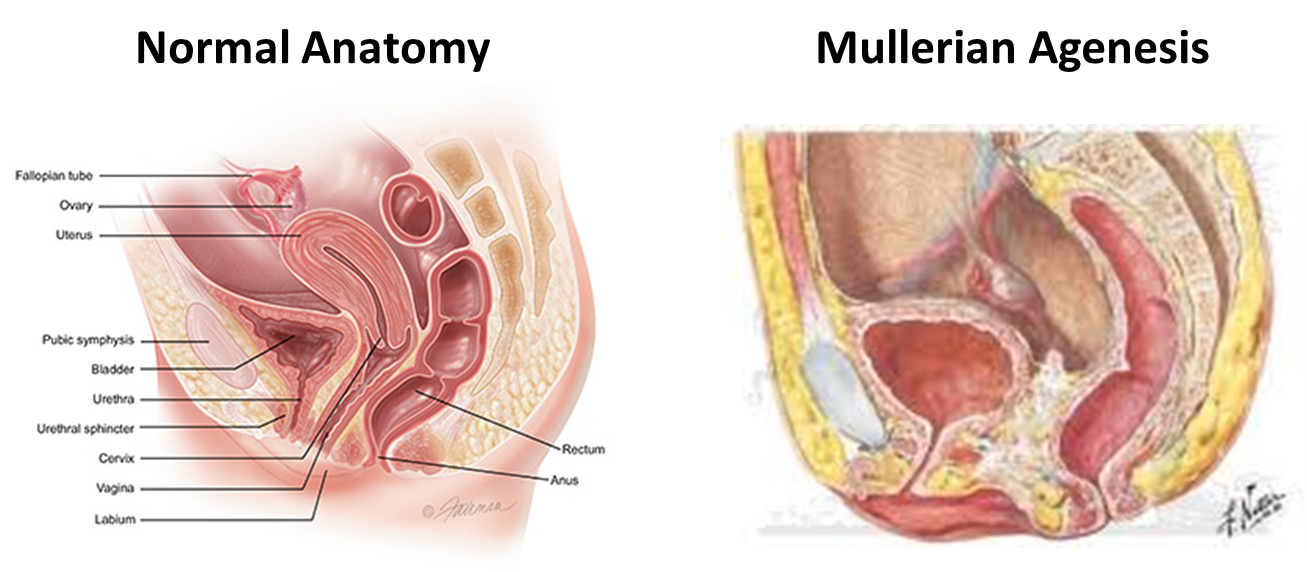
Congenital Absence of the Uterus is a common cause of structural form of primary amenorrhea
1) Mullerian Agenesis
→ patients are XX females with normal ovaries but patients will lack a uterus and vagina
→ patients will have their vagina replaced by connective tissue
→ their hymen tissue will end in a blind pouch rather than having a normal opening
2) Androgen Insensitivity
→ XY female with male gonads due to patients lacking receptors to testosterone
→ because they cannot sense testosterone, it is all converted to estrogen leading to secondary sexual characteristics
What are the findings and treatments associated with congenital absence of the uterus?
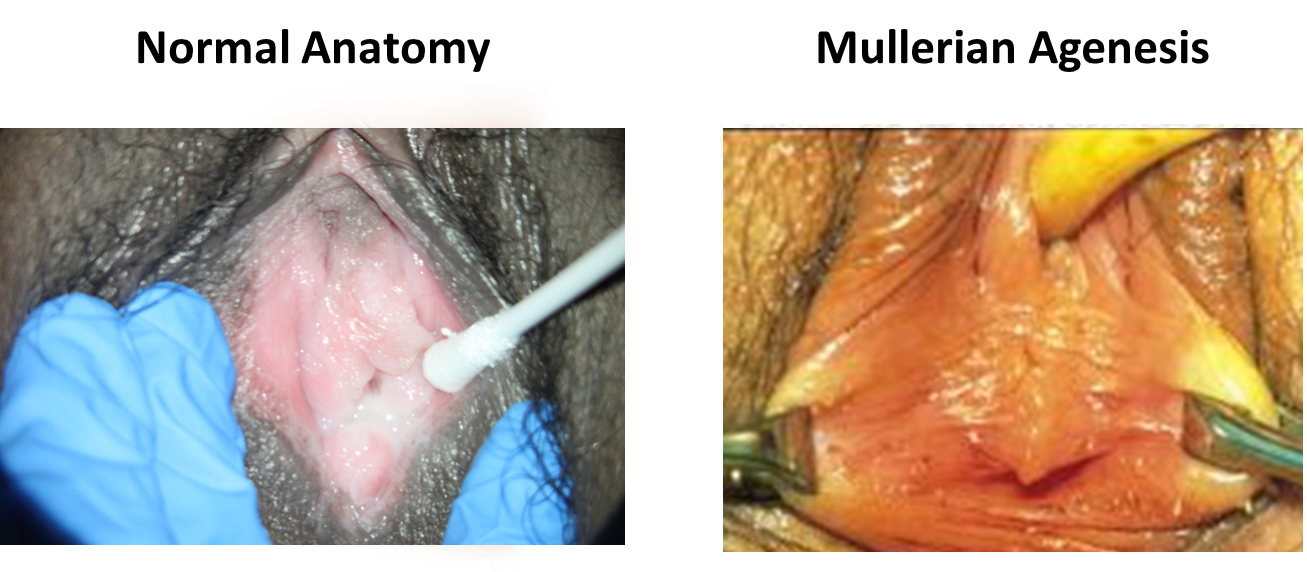
Perform a GU exam to evaluate for normal female external structures with a lack of vagina
1) If a patient has testosterone that is high and in male range it is more likely to be androgen insensitivity syndrome
→ Mullerian Agenesis will have female level testosterone
→ can also karyotype
2) Treated with neovagina or creating a vagina
→ Mullerian agenesis patients can get pregnant
→ Androgen insensitivity patients will have testis so cannot get pregnant
What is Obstruction of Menstrual Outflow?

Obstruction of Menstrual Outflow is a structural issue that causes primary amenorrhea.
→ patients with these outflow obstructions will still have periods but will be unable to bleed due to their vagina being blocked
1) Imperforate Hymen
→ hymen is not-canalized with incomplete invagination or apoptosis of the urogenital sinus
→ causes the hymen to bulge with increased intrabdominal pressure
→ is blue due to deoxygenated blood
2) Transverse Vaginal Septum
→ connective tissue band forms in the vagina preventing flow of blood
→ can perform a rectal exam to feel their vagina bulging from all the blood
3) Vaginal Agenesis
→ the urogenital sinus does not canalize
What is Hypogonadotropic Primary Amenorrhea?
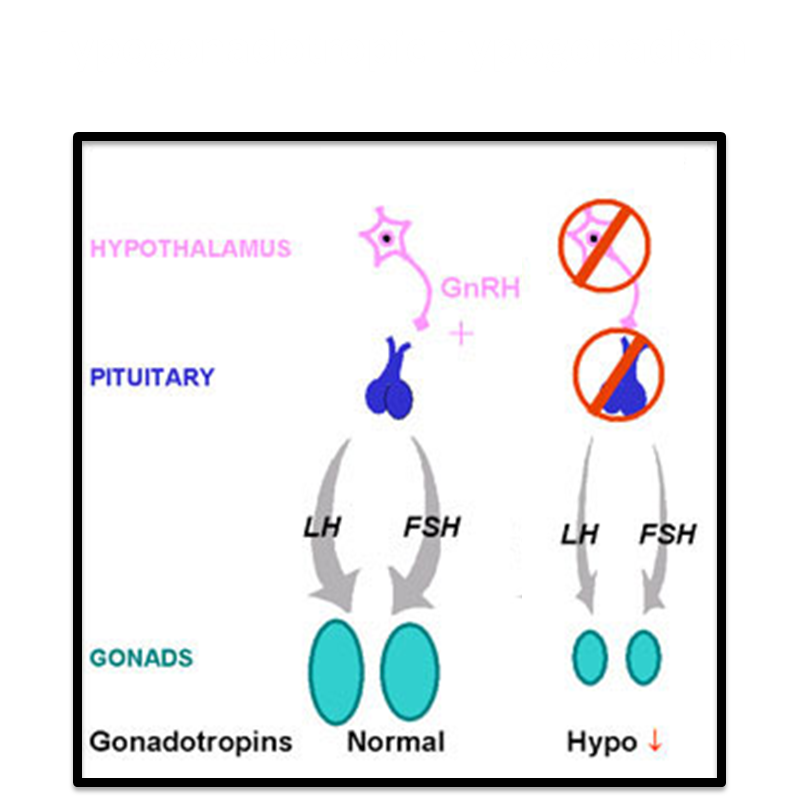
Both are considered hypogonadotropic hypogonadism
Congenital GnRH deficiency
→ congenital GnRH deficiency resulting in low FSH and LH and absent estradiol
Functional Amenorrhea
→ FSH and LH are low to normal
→ Estradiol is absent to low
→ seen in patients who are functionally nutrient deficient or malabsorptive - seen in very thin patients
What can prolactinomas do?
Prolactinoma are pituitary gland tumors that lead to amenorrhea
→ patients will also present with galactorrhea
What ovarian dysfunction causes primary amenorrhea?
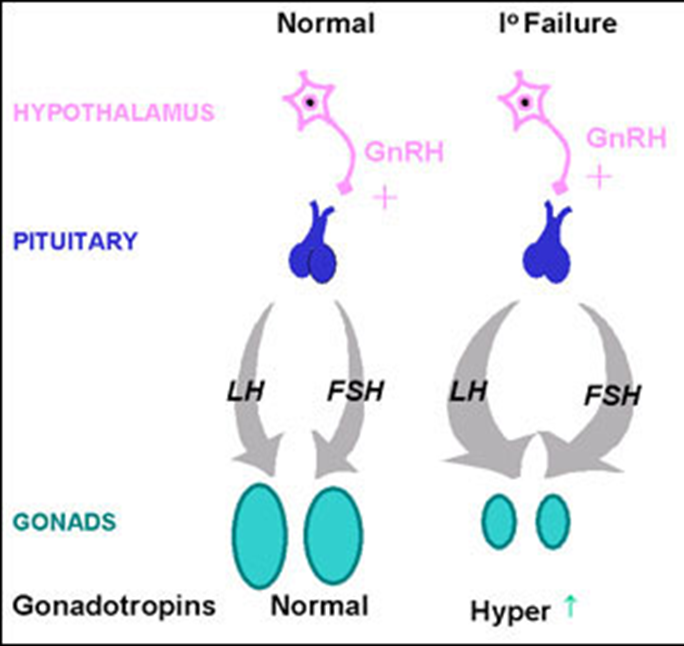
Ovarian Dysfunction causes hypergonadotropic hypogonadism
→ patients have constitutively high levels of LH and FSH but the ovaries are not responding resulting in low estrogen levels
1) Primary Ovarian Insufficiency
→ patients are XX and have had failure of their gonads resulting in elevated FSH and absent E2
→ treated with hormone replacement therapy
2) Turner Syndrome
→ elevated FSH and absent estradiol due to a XO karyotype
→ very short, streak gonads, webbed neck and shield chest
→ hormonal replacement therapy
What does hyperthyroidism and androgen excess cause in terms of puberty?
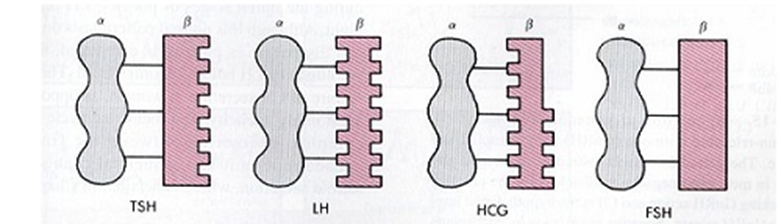
The alpha subunit of TSH, HCG, LH, and FSH are all very similar so they can have cross-reactivity
→ thyroid excess can lead to primary amenorrhea
Androgen excess can cause primary amenorrhea
→ 21-hydroxylase deficiency where patients can’t make cortisol and aldosterone, so it all gets funneled into making androgens