antibacterials - lecture 31
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
Over-arching theme with all anti-infectives
therapeutics aim to exploit biochemical differences between the pathogen and host
Selectively inhibit pathogen while minimizing toxicity to similar host pathways
Antibiotics
can be bactericidal or bacteriostatic:
bactericidal
kills bacteria
Work best on organisms with rapid growth (as opposed to those trapped within biofilm)
Of note, these are in vitro distinctions and the efficacy of drugs in vivo in clinical situations is more complex than these definitions imply
bacteriostatic
suppress bacterial growth
In theory require robust immune response to clear
infection
Of note, these are in vitro distinctions and the efficacy of drugs in vivo in clinical situations is more complex than these definitions imply
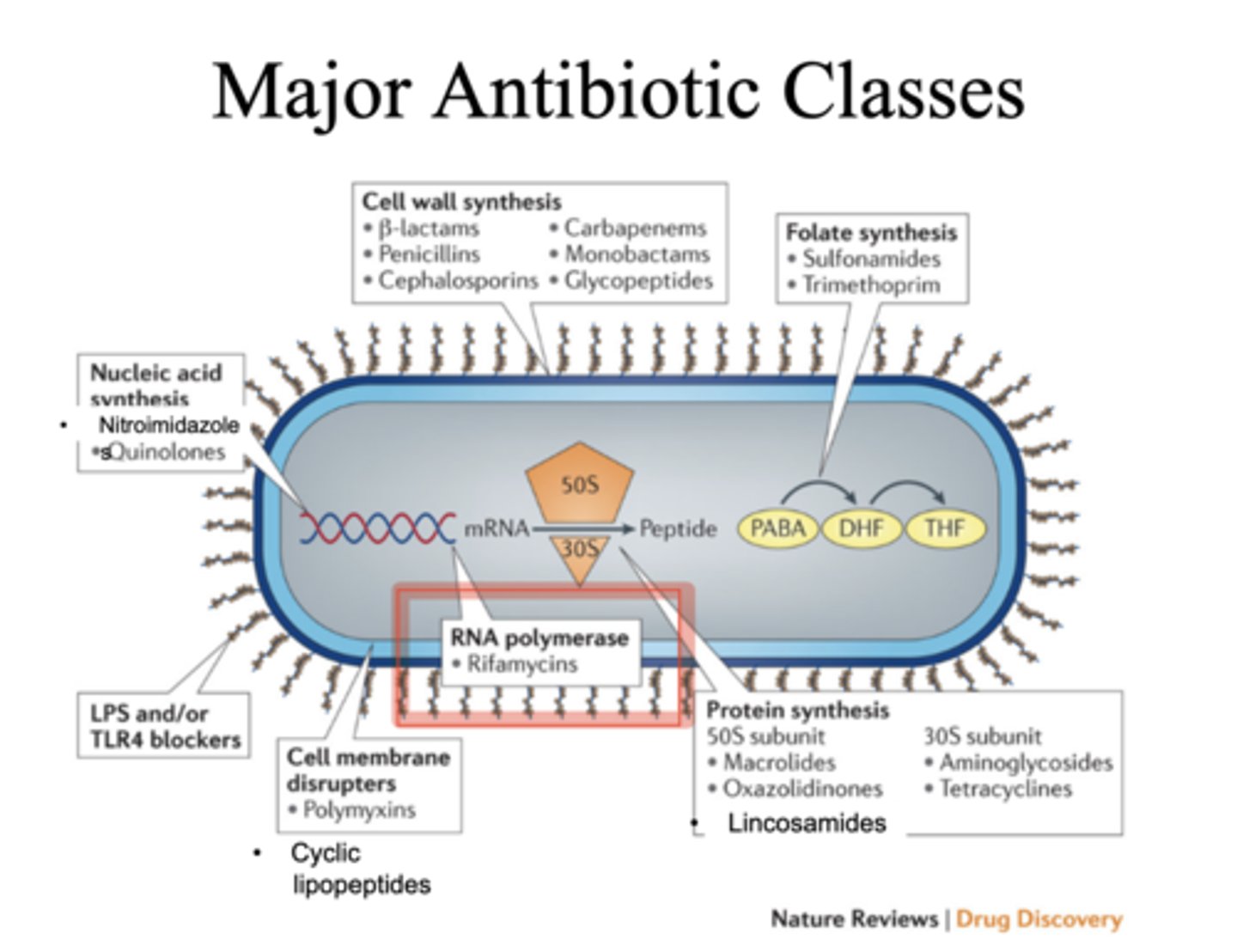
cell wall inhibitors
b-lactams:
Penicillins Cephalosporins Carbapenems Monobactams
glycopeptides
bacterial cell wall synthesis
Our cells do not have cell walls i.e. bacterial cell walls are an excellent therapeutic target
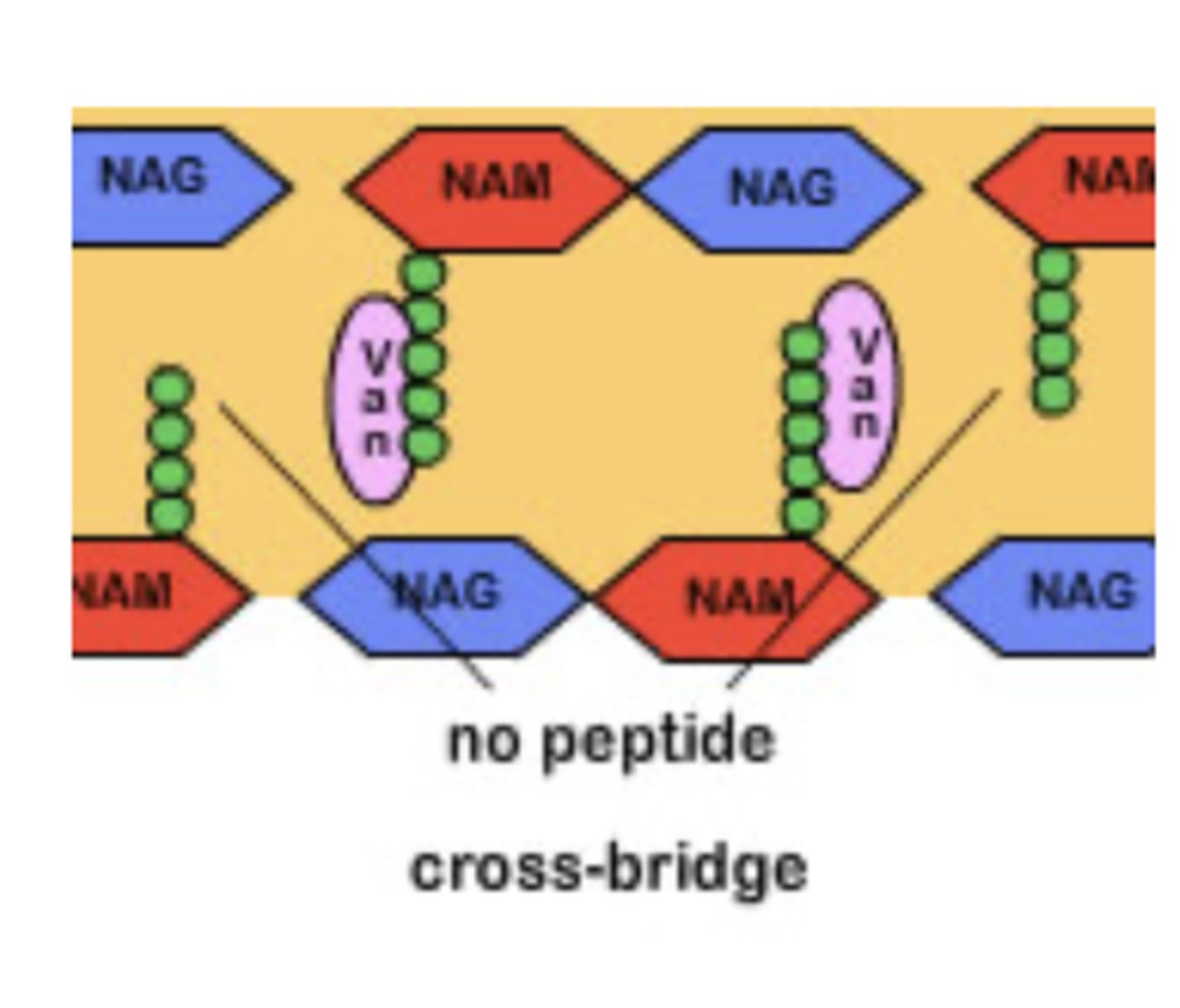
NAM-NAG are cross- linked by
pentapeptides
Cross-linking is catalyzed by
transpeptidases
In Gram (+) bacteria, the cell wall structure is thick
In Gram (-) bacteria, the cell wall structure is thin
2 classes of cell wall inhibitors
Beta lactams — includes 4 subclasses:
Penicillins
Cephalosporins Carbapenems Monobactams
glycopeptides
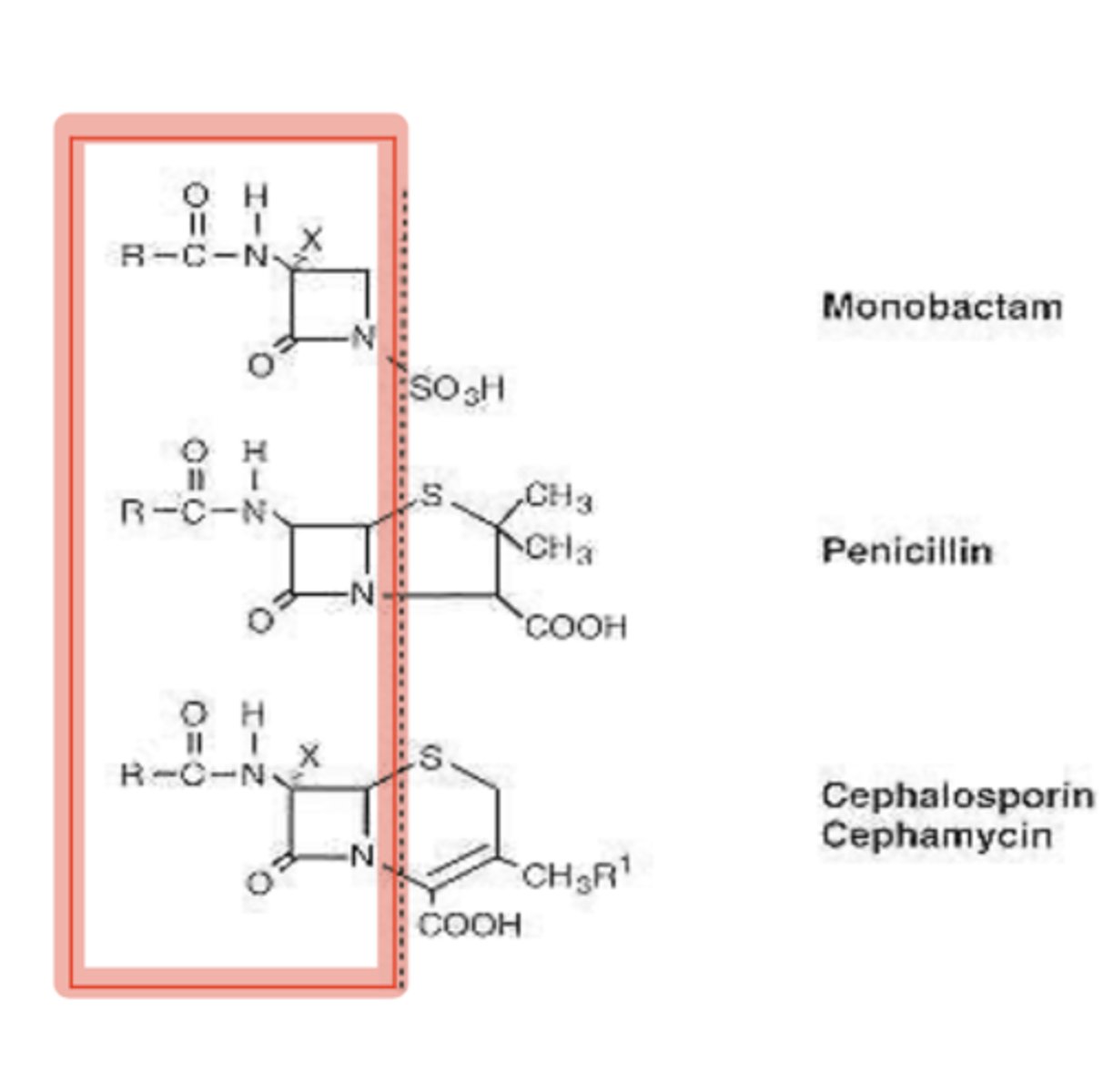
beta lactams
Very important drug class — broad spectrum of activity and favorable side effect profile
Mechanism of action (MOA): inhibit the transpeptidase that catalyzes cell wall cross- linking:
Penicillin binding protein (PBP) = transpeptidase
After cross-linking is halted, the bacterial cell wall cannot be completed and the bacterial cell lyses under suitable osmotic conditions (i.e. bacteriocidal)
beta lactams
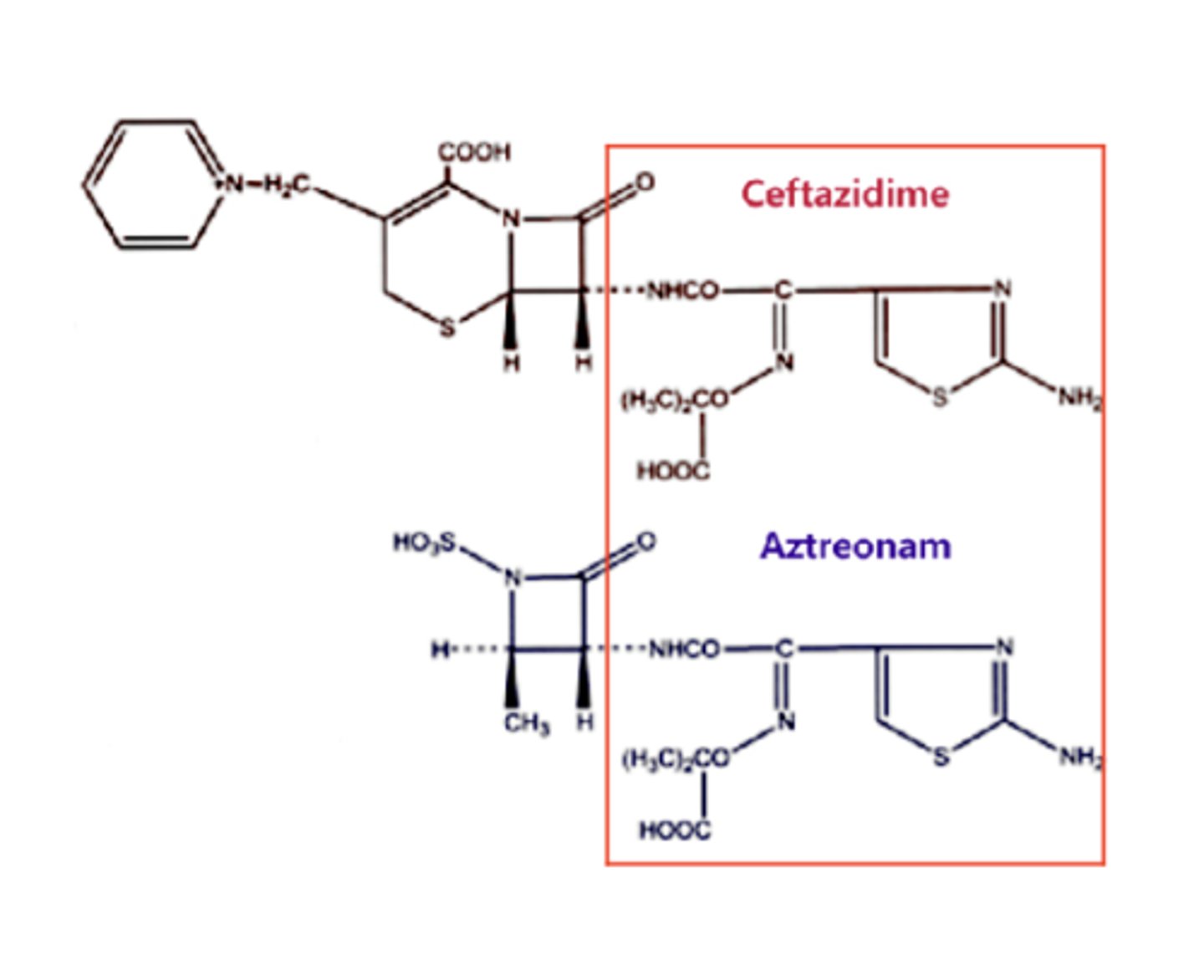
Beta lactam ring and acyl side group are conserved across all subclasses (red box):
Spectrum of activity is determined by variable side groups that determine specificity for particular organisms
Penicillins developed first; new Beta lactams were developed to combat emerging antibiotic resistance particularly in S. aureus, Pseudomonas, and enteric Gram-negative rods (GNRs) e.g. E.coli, Salmonella, Klebsiella
Beta Lactams: Penicillins
Penicillins — the original beta lactam drugs:
Natural penicillins — penicillin G (parenteral: IV or IM), penicillin VK (oral)
Aminopenicillins — ampicillin (IV), amoxicillin (oral)
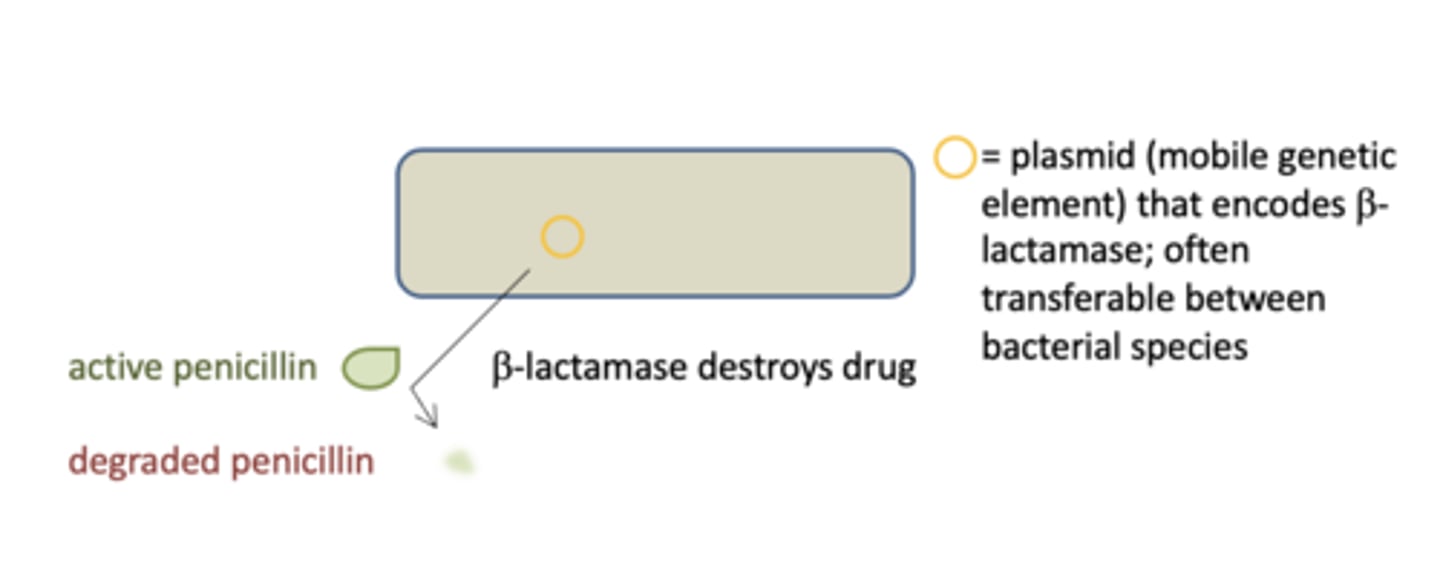
Resistance to Penicillins
Beta lactamases are bacterial enzymes that degrade the beta lactam ring. Bacteria that express beta lactamase can therefore destroy natural penicillins and aminopenicillins i.e. such bacteria have resistance to these drugs.
outcome of resistance to b lactams
bacteria continue to grow in the presence of the penicillin, i.e. they are resistant to the drug
outcome of resistance to b lactams: tools to fight resistance
bacteria do not grow in the presence of the drug(s) i.e. there is effective therapy
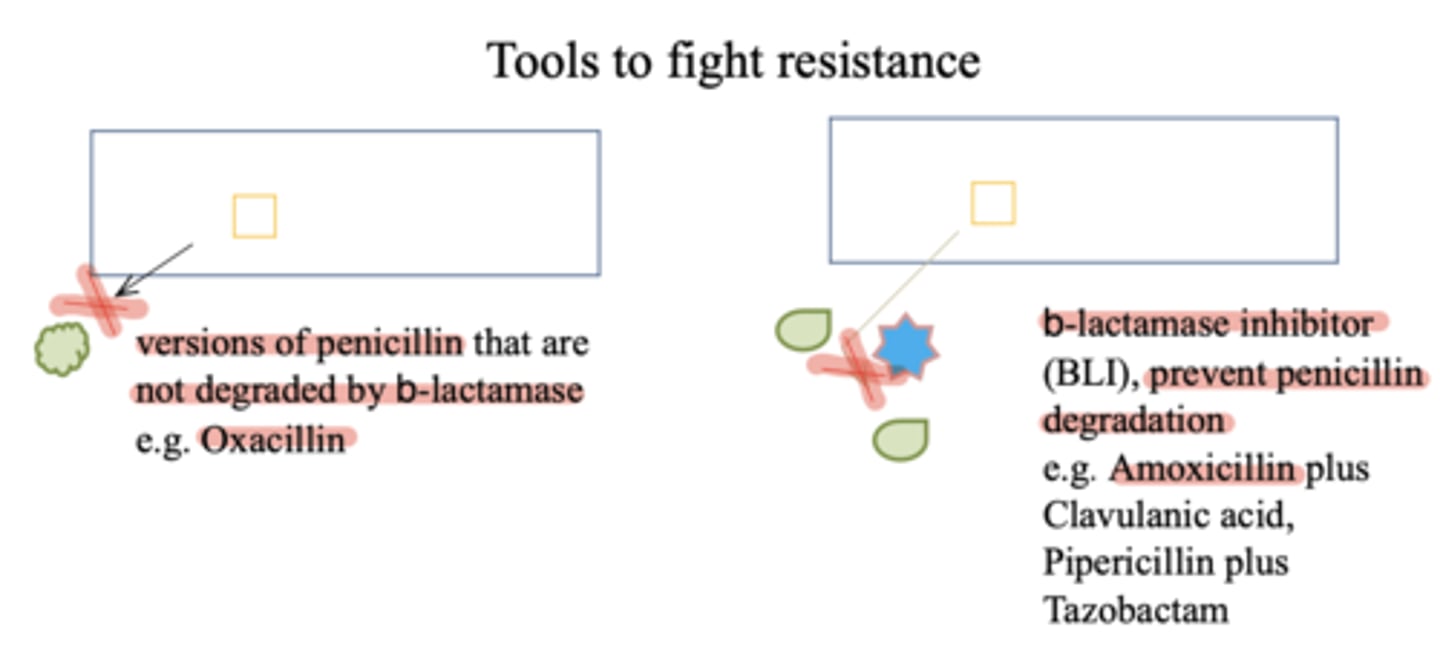
beta lactams
tools to combat drug resistance
Beta lactamase-insensitive penicillins and combination drugs were developed to combat drug resistance in S. aureus and Gram – rods /anaerobes respectively
Beta-lactamase-insensitive penicillins — oxacillin, nafcillin
Penicillin + beta lactamase inhibitors (BLIs) — combination drug of a broad-spectrum penicillin plus a beta-lactamase inhibitor e.g. amoxicillin-clavulanic acid, pipericillin-tazobactam
Cephalosporins - beta lactams
second subclass developed:
1st generation — cefazolin
2nd generation — cefoxitin
3rd generation — ceftriaxone, ceftazidime
4th generation — cefepime
5th generation — ceftaroline
As generation number increases, the drugs become increasingly useful for treating GNR but less useful for anaerobic organisms
(Remember drug class, not individual drugs)
Carbapenems - beta lactams
third subclass developed, “big gun” subclass for severe or high-risk
infections (e.g. multi-drug resistant bacteria):
Meropenem
Imipenem
Created to treat advanced resistance caused by ESBL (extended spectrum beta lactamases) in GNR and anaerobic organisms
Beta Lactams: Monobactams
“designer drug” class:
Aztreonam
Created to treat Pseudomonas infections in patients with penicillin allergies:
Only active against Gram - aerobes
Shares side group with ceftazidime – consequently patients allergic to ceftazidime maybe allergic to aztreonam
b-lactams
pharmacokinetics:
Absorption: rapid from GI tract (some PCN and cephalosporins only) Distribution: widely distributed but concentrations vary from tissue to tissue (e.g., only some drugs penetrate CSF) Elimination: kidney
adverse effects:
Allergic reactions (most common — rash, rarely anaphylaxis)
Nephrotoxicity
Neurotoxicity (high doses induce seizures) Hepatotoxicity (PCN/BLI, ceftriaxone)
drug interactions:
few
glycopeptides
Cell-wall inhibitors that treat resistant Gram (+) organisms
MOA:
Block cross-linking of pentapeptides and prevent cell wall synthesis
Bactericidal
Drug: vancomycin
glycopeptides
pharmacokinetics:
Absorption: none, given IV only (important
exception: C. difficile infections of the gut)
Distribution: widely distributed (including CSF when meninges are inflamed e.g. meningitis)
Elimination: kidneys
adverse effects:
Vancomycin-flushing (previously Red-man) syndrome - extreme flushing due to direct release of histamine from mast cells. Remedy: decrease infusion rate, administer diphenhydramine as necessary
Nephrotoxicity
drug interactions:
none indicated
protein synthesis inhibitors
Aminoglycosides (Gentamicin)
Tetracyclines (Doxicycline)
Macrolides (Azithromycin)
Lincosamides (Clindamycin)
Oxazolidinones (Linezolid)
protein synthesis inhibitors
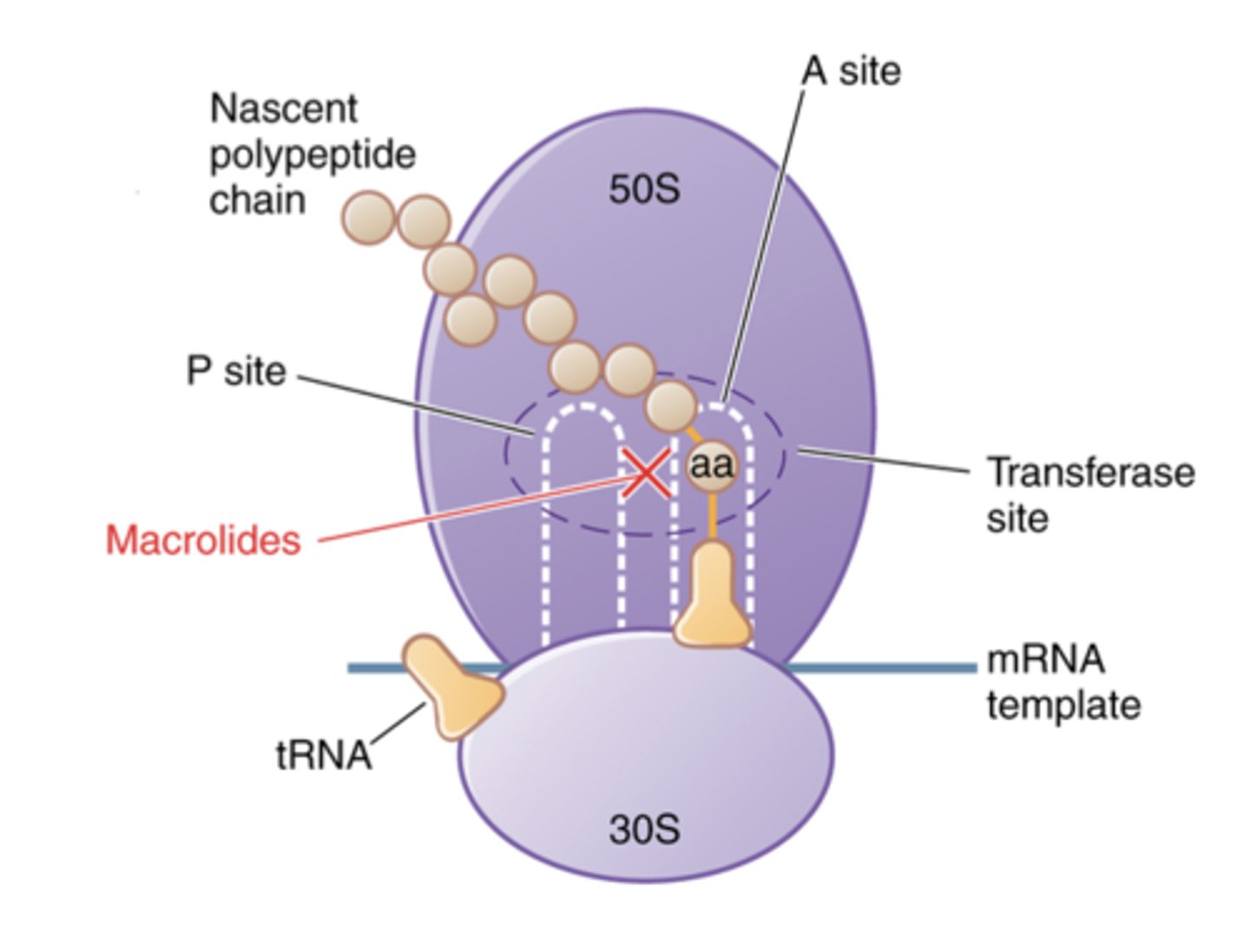
MOA: inhibit bacterial ribosome
Bacterial and mammalian ribosomes are similar but different enough that drugs are selective for the pathogen:
protein synthesis inhibitors
Includes drugs that act on the 2 subunits of the 70S bacterial ribosome:
30S inhibitors:
Aminoglycosides
Tetracyclines
50S inhibitors:
Macrolides Lincosamides Oxazolidanones
Adverse Reactions/Drug Interactions of 30S inhibitors
Aminoglycosides (eg gentamicin)
Not useful against anaerobes
Very effective antibiotics but the toxicity of
aminoglycosides limits their clinical use
Ototoxicity
Nephrotoxicity
Tetracyclines (eg doxicycline)
Particularly useful against intracellular organisms
Tetracycline is incorporated into calcifying structures
(not used in children <8 yrs)
Allergy, superinfection
Hepatotoxic and nephrotoxic
Photosensitivity
Metal cations, like Zn2+, Ca2+, Mg2+ (found in
antacids, dairy products, dietary supplements) impair absorption in GI tract
Adverse Reactions/Drug Interactions of 50S inhibitors
Macrolides (eg azithromycin)
Cholestatic Jaundice
Antagonize other antibiotics targeting 50S
(commonly stated to decrease the effectiveness of oral
contraceptives: false)
CYP 3A4 inhibitor (i.e. many drug-drug interactions)
Cardiac arrhythmias
Lincosamides (eg clindamycin)
Can precipitate antibiotic-associated diarrhea
(C. difficile pseudomembranous colitis)
Oxazolidinones (eg linezolid)
Very useful in ICU settings for resistant Gram + infections eg MRSA, VRE
Myelosuppression, CNS effects
Folic acid synthesis inhibitors
Sulfonamides
Trimethoprim
folic acid
Bacteria must synthesize folic acid for growth
Sulfomamides and trimethoprim are competitive inhibitors of distinct steps in the bacterial synthesis of folic acid
Combined together (e.g. trimethoprim- sulfamethoxazole, Bactrim) because resistance to individual drugs is widespread
Folate Synthesis Inhibitors
Pharmacokinetics
Absorption: rapid absorption from the GI tract
Distribution: widely distributed including CSF
Elimination: renal
Adverse Effects
Rashes
Bone marrow suppression (mostly seen in folate deficient patients)
Nephrotoxicity
Drug interactions
CYP 3A4, CYP 2C8 and CYP 2C9 inhibitors (consequently many drug-drug interactions)
Bacterial replication inhibitors
Quinolones, Fluoroquinolones (Ciprofloxacin)
Nitroimidazoles (Metronidazole)
Fluoroquinolones e.g. Ciprofloxacin
Mechanism of Action:
Inhibit DNA topoisomerase and/or gyrase activity (unique
to bacteria) and hence DNA synthesis
Fluoroquinolones
Pharmacokinetics
Absorption: rapid absorption from the GI tract
Distribution: widely distributed (including CSF)
Elimination: kidney
Adverse Effects
Achilles tendon rupture Cardiac arrhythmias
Drug interactions
Absorption markedly reduced when given with antacids
Nitroimidazoles e.g. Metronidazole
Mechanism of action— complex, unique
Metabolites of nitroimidazoles affect DNA/RNA synthesis and protein synthesis in bacteria
-- bacteriocidal
Spectrum of activity
-- Anaerobes (Gram – and Gram +), some protozoa
Adverse effects
-- Disulfiram (Antabuse)-like reaction with alcohol use
-- Neuropathy
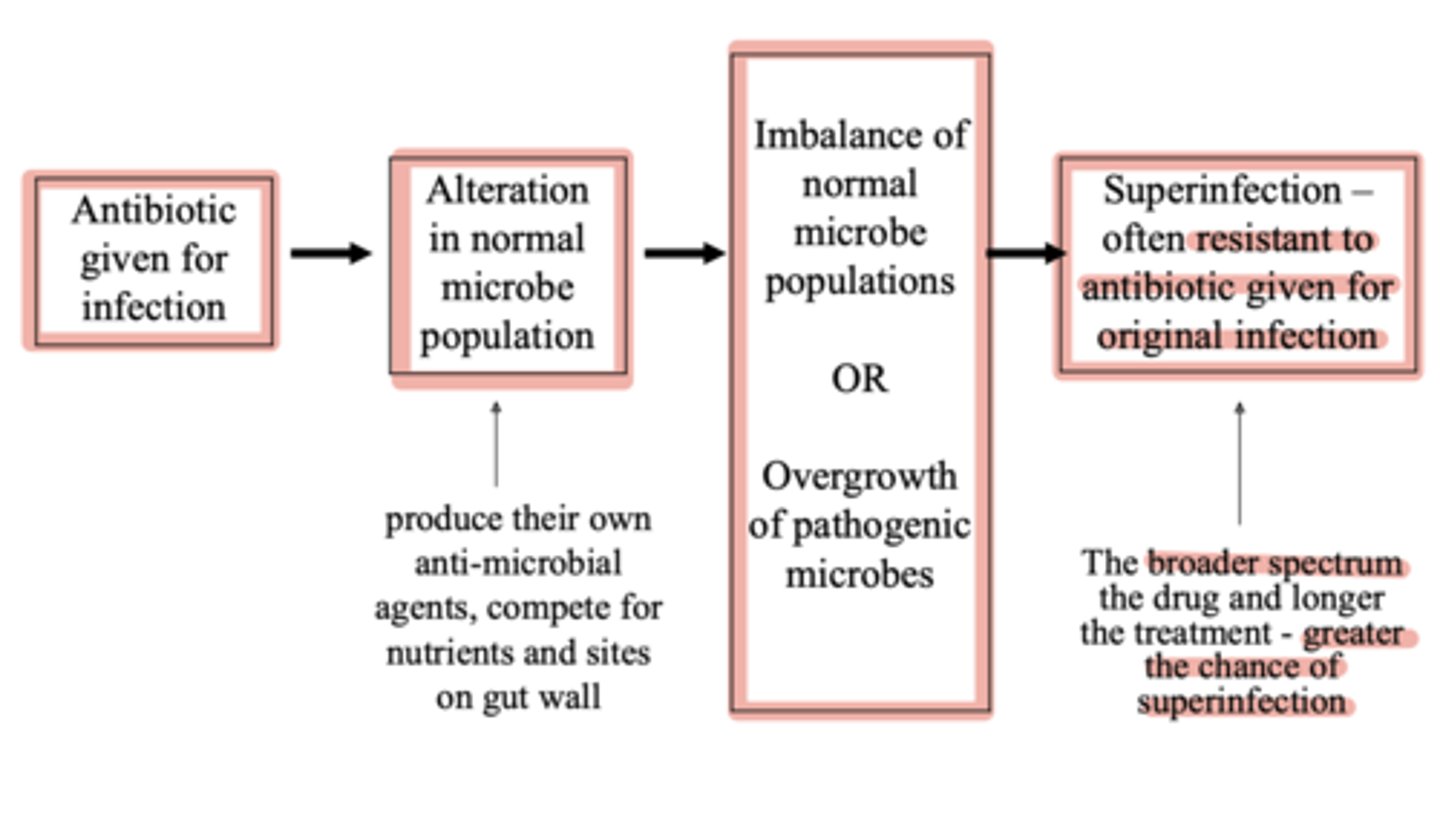
Superinfection
appearance of a secondary infection as a result of treating a primary infection, e.g. C. difficile after Clindamycin treatment
"wont test us on anything after this"
"wont test us on anything after this"