Ischaemic heart disease - clinical
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
What does the term myocardial blood supply/demand imbalance refer to?
It refers to a mismatch between the heart muscle’s need for oxygen and nutrients and the amount actually supplied by the coronary circulation.
What are the main causes of a myocardial blood supply/demand imbalance?
Reduced fuel supply, increased demand, or poor-quality fuel.
What is meant by reduced fuel supply in the context of myocardial blood supply/demand imbalance?
It means there is insufficient blood flow or oxygen delivery to the heart muscle, often due to coronary artery disease or obstruction.
How can increased demand lead to a myocardial blood supply/demand imbalance?
Conditions such as exercise, fever, or tachycardia increase the heart’s workload and oxygen demand beyond what the blood supply can meet.
What is meant by poor-quality fuel in relation to the myocardium?
It refers to a reduced ability of the blood to carry or deliver oxygen effectively, as seen in anaemia or hypoxaemia.
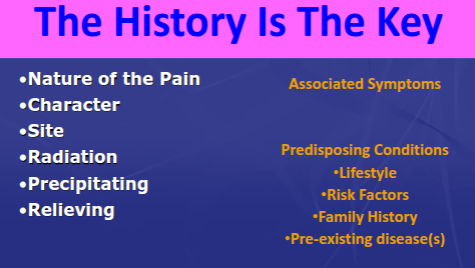
What type of pain is characteristic of ischaemic chest pain (angina)?
The pain is typically described as crushing or vice-like in nature, and may be indicated by Levine’s sign (clenched fist over the chest).
Where is the pain of angina usually felt?
Classically retrosternal, but it may also radiate to the arms (usually the left more than the right), neck, or jaw, or any combination of these areas.
What factors commonly precipitate angina?
Exertion, emotional stress, or exposure to cold winds.
How quickly does angina pain typically develop?
It has a gradual onset over about 10 to 30 seconds.
How long does an episode of angina usually last, and how is it relieved?
It typically lasts 2 to 15 minutes and is relieved by rest or glyceryl trinitrate (GTN) within 2 to 3 minutes.
What symptoms often accompany angina pain?
Shortness of breath and sweating are commonly associated.
Differential Diagnosis of Chest Pain
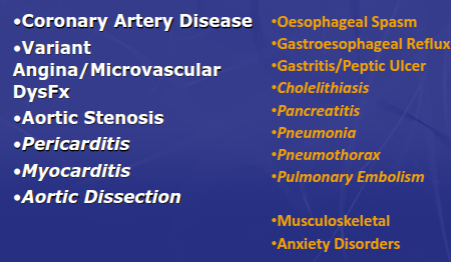
Differential Diagnosis of Chest Pain
What are the atypical clinical symptoms of ischaemia, and in which patients are they most common?
Elderly, diabetic, and female patients with ischaemic heart disease (IHD) may present atypically with breathlessness, tachycardia, nausea or vomiting, and sweating or clamminess, rather than classic chest pain.
On what basis should stable angina be suspected according to NICE?
Stable angina should be suspected based on clinical assessment and the typicality of chest pain.
How are angina symptoms classified according to NICE?
Symptoms are classified according to their typicality—as either typical angina, atypical angina, or non-anginal chest pain.
What are the three features of typical angina?
Precipitated by physical exertion.
Constricting discomfort in the front of the chest, neck, shoulders, jaw, or arms.
Relieved by rest or glyceryl trinitrate (GTN) within about 5 minutes.
How is atypical angina defined?
Atypical angina is present when two of the three features of typical angina are met
Atypical angina is chest pain that doesn't fit the classic description of typical angina (pressure/heaviness, exertion-related, relieved by rest/nitroglycerin) but is still suspected to be cardiac-related, often presenting as sharp/stabbing pain, positional pain, or associated with nausea, sweating, or fatigue, common in women, and requiring investigation to rule out heart issues
What are some additional symptoms that may occur with atypical angina?
Gastrointestinal discomfort, breathlessness, and/or nausea.
According to NICE, which factors make a diagnosis of stable angina more likely?
Increasing age
Male sex
Presence of cardiovascular risk factors
History of established coronary artery disease, such as previous myocardial infarction or coronary revascularisation
According to NICE, which factors make a diagnosis of stable angina less likely?
Pain that is continuous or prolonged
Pain unrelated to activity
Pain brought on by breathing
Pain associated with dizziness, palpitations, tingling, or difficulty swallowing
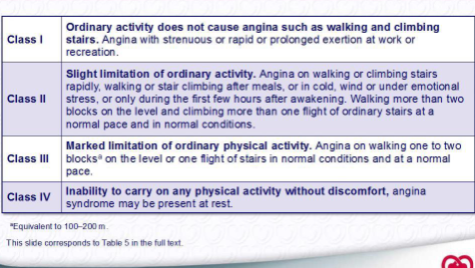
Classification of angina severity according to the Canadian Cardiovascular Society
According to NICE, when is coronary CT angiography recommended as the first-line investigation for chest pain of recent onset?
Coronary CT angiography is the first-line test for patients with typical angina, atypical angina, or non-anginal chest pain accompanied by ST-T changes or Q waves on a 12-lead resting ECG.
According to NICE, how is significant coronary artery disease (CAD) defined on CT coronary angiography?
Significant CAD is defined as ≥70% diameter stenosis of one or more major epicardial arteries, or ≥50% diameter stenosis in the left main coronary artery.
What factors can intensify ischaemia, allowing less severe lesions (50–70%) to produce angina?
Reduced oxygen delivery (e.g. anaemia, coronary spasm)
Increased oxygen demand (e.g. tachycardia, left ventricular hypertrophy)
Large mass of ischaemic myocardium (e.g. proximally located lesions)
Longer lesion length
According to NICE, when should non-invasive functional imaging for myocardial ischaemia be performed in the investigation of angina?
It should be performed when CT coronary angiography shows coronary artery disease of uncertain functional significance or yields non-diagnostic findings.
How should angina be investigated in patients with confirmed coronary artery disease, according to NICE?
Offer non-invasive functional testing if there is uncertainty about whether chest pain is due to myocardial ischaemia.
An exercise ECG may be used as an alternative to functional imaging.
Consider repeat angiography if there are concerning clinical features or abnormal test results.
What high-risk features on an exercise ECG suggest severe coronary artery disease?
Diminished exercise capacity
Significant ST-segment depression at low workload or heart rate <130 bpm
Fall in systolic blood pressure during exercise
Complex ventricular ectopy or ventricular tachycardia at low levels of exercise
What stress echocardiography findings indicate high risk?
Baseline left ventricular dysfunction
Increasing number of resting wall motion abnormalities
Increasing number of inducible wall motion abnormalities
What myocardial perfusion imaging (MPI) findings are associated with high risk?
Dynamic left ventricular cavity dilatation with stress
Increased lung uptake
Ischaemia in multiple territories (total perfusion defect, TPD >10%)
How should non-invasive test results be interpreted in suspected ischaemic heart disease?
They should always be interpreted in the context of the patient’s age and co-morbidities.
What are the key areas to manage in risk factor modification for ischaemic heart disease?
Lipids, hypertension, and diabetes should be optimally managed to reduce cardiovascular risk.
What lifestyle modifications are recommended to reduce cardiovascular risk?
Weight management
Healthy diet
Regular physical exercise
Smoking cessation
What are the main pharmacological treatments used for risk factor modification in ischaemic heart disease?
Aspirin (or clopidogrel as an alternative)
Statin for lipid control
ACE inhibitor if there is a coexisting indication or vascular risk
Diabetes management medications, such as metformin or SGLT2 inhibitors
Why is smoking cessation important in patients with ischaemic heart disease?
It significantly reduces the risk of further atherosclerotic progression, myocardial infarction, and mortality.
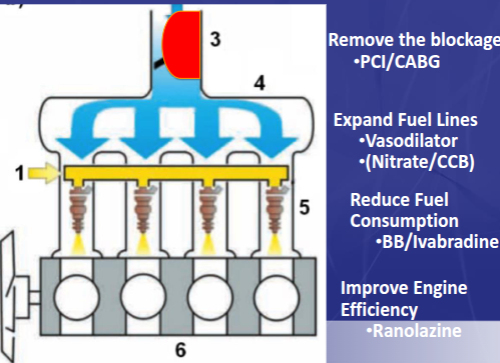
According to NICE, what is the initial approach to treating stable angina?
Patients should be offered optimal medical therapy (OMT) rather than revascularisation procedures initially.
What is the first-line pharmacological treatment for stable angina?
A beta-blocker and/or a calcium channel blocker.
Which drugs can be used as add-on treatments if first-line therapy does not adequately control symptoms?
Long-acting nitrate
Ivabradine
Nicorandil
Ranolazine
When should a third anti-anginal agent be considered?
Only if symptoms are not controlled on two agents and the patient is awaiting revascularisation or is not suitable for such a procedure.
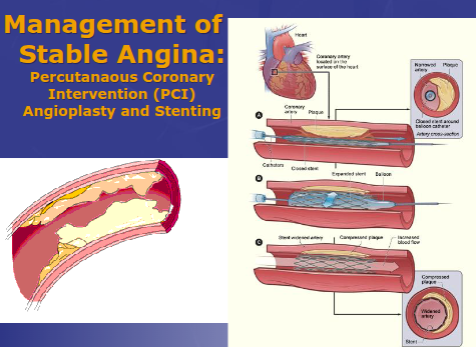
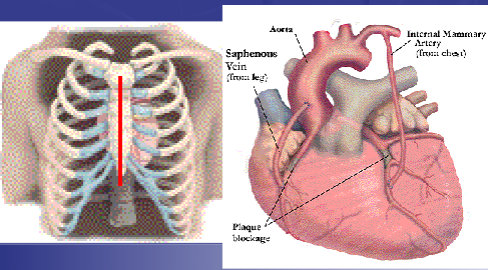
Management of Stable Angina: Percutanaous Coronary Intervention (PCI) Angioplasty and Stenting
Management of Stable Angina: Coronary Artery Bypass Surgery (CABG)
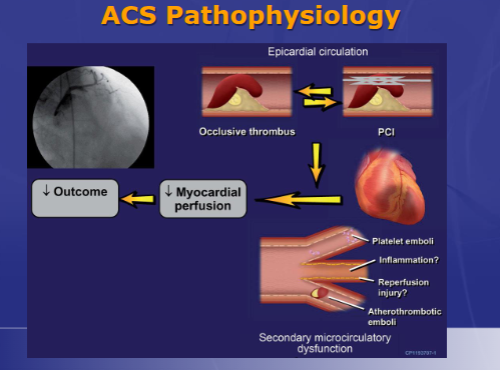
Acute Coronary Syndromes
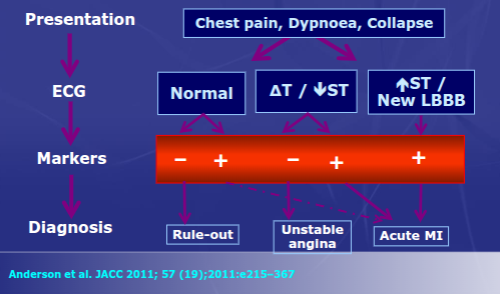
What are the key diagnostic features of an acute myocardial infarction (AMI)?
Symptoms characteristic of myocardial pain
Characteristic ECG changes due to ischaemia
Evidence of cardiac myocyte necrosis — which is required to confirm acute myocardial infarction in clinical practice.
What is meant by a ‘silent’ myocardial infarction, and in whom does it most often occur?
A silent myocardial infarction occurs when the event is undiagnosed or unrecognised, due to absent or atypical symptoms. It is more common in elderly and diabetic patients.
Time dependent: Emergency evaluation of ACS
What are the key components of optimising secondary prevention after myocardial infarction or established coronary artery disease?
Beta-blockers
RAAS inhibition (e.g. ACE inhibitors or ARBs)
Lipid lowering therapy (e.g. statins)
Antiplatelet therapy
What are the key benefits of beta-blockers after myocardial infarction (post-MI)?
They reduce heart rate and blood pressure, decrease cardiac workload, have anti-arrhythmic effects, and improve clinical outcomes
What are the benefits of Renin–Angiotensin–Aldosterone System (RAAS) inhibitors after myocardial infarction (post-MI)?
ACE inhibitors, ARBs, or MRAs reduce sodium and water retention, lower blood pressure and afterload, decrease cardiac workload, prevent cardiac remodelling, and improve outcomes.
What are the benefits of lipid-lowering therapy after myocardial infarction (post-MI)?
Statins (and ezetimibe or PCSK9 inhibitors if needed) reduce atherogenic lipoproteins (LDL-C), lower inflammation, stabilise atherosclerotic plaques, and improve clinical outcomes.
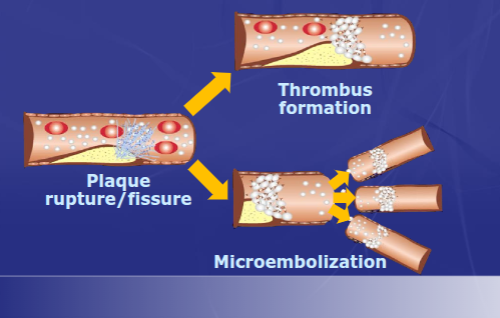
Stabilising the Atherosclerotic Plaque
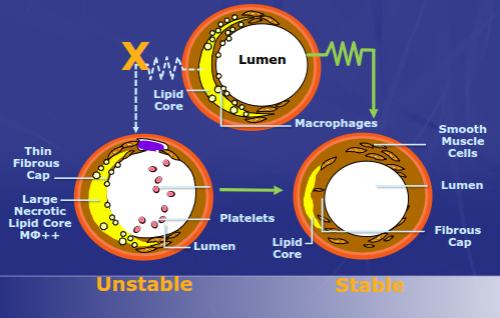
ACS Cascade
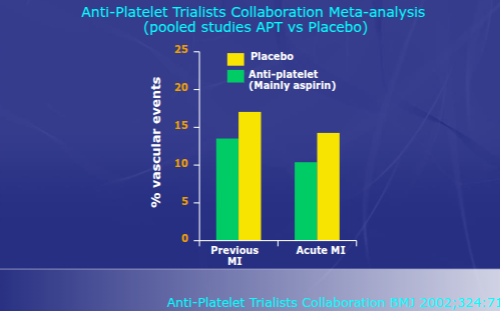
Anti-Platelet Therapy reduces Recurrent Vascular Events
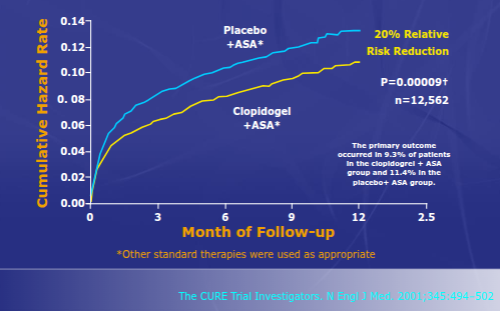
Dual Antiplatelet Rx beats monoRx:
The CURE study Clopidogrel + Aspirin
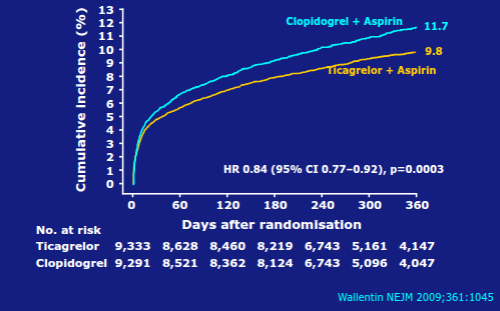
LATO Study: Ticagrelor beats Clopidogrel
(CV death, MI or stroke)
What is the routine post-myocardial infarction (post-MI) prescription?
Aspirin plus a P2Y12 antagonist (ticagrelor, prasugrel, or clopidogrel)
Atorvastatin 80 mg
Bisoprolol (target dose 10 mg)
Ramipril (target dose 10 mg once daily or 5 mg twice daily)
What are the key steps in the management of ischaemic heart disease (IHD) or acute coronary syndrome (ACS)?
Confirm diagnosis and assess risk
Use ECG and troponin in suspected ACS
Evaluate coronary anatomy or perform stress testing
Relieve ischaemia through revascularisation (in ACS, high-risk, or symptomatic stable disease)
Provide symptom relief with beta-blockers, calcium channel blockers, nitrates, or other agents
Optimise secondary prevention — control diet, exercise, smoking, blood pressure, and lipids
Prescribe statin, antiplatelet, beta-blocker, and ACE inhibitor
What is the utility of the ECG during acute coronary events?
ECG helps to:
Detect complicating arrhythmias (ventricular fibrillation/tachycardia, atrial fibrillation, heart block)
Show evidence of previous myocardial infarction
Identify dynamic ST-segment changes
Determine the need for reperfusion therapy
Monitor response to therapy
Detect recurrent ischaemia
How is patient “vulnerability” addressed in cardiovascular disease management?
By targeting:
Vulnerable structures:
Myocardium
Atherosclerotic plaque
Blood (thrombogenicity)
Risk assessment:
Invasive vs conservative management
Medical therapy vs revascularisation
Optimising secondary prevention