Eating, Sex, Sleep
1/185
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
186 Terms
AN diagnostic criteria
restriction of energy intake relative to requirements, leading to sig low body weight relative to development
intense fear of gaining weight or becoming fat, or persistent behavior interfering with weight gain
disturbance in experience of body shape or weight, undue influence of weight/shape on self-eval, persistent lack of recognition of seriousness of current body weight
AN specifications
type: binge/purge or restrictive
remission: partial (A not met, B/C still present) or full
severity:
BMI for adults
BMI percentage for youth
associated features AN
depressive signs/symptoms when seriously underweight
obsessive-compulsive features
inflexibility/desire for control (restrained emotional expression, limited social spontaneity, no eating in public)
binge/purge: impulsivity, drug abuse
excessive physical activity
misuse of medication
development and course AN
onset common in adolescence or adulthood
younger may manifest atypical features
older have longer duration
period of changed eating behavior prior to full criteria met
most remiss within 5y of presentation
5% mortality per decade
risk factors AN
anxiety disorders or obsessional traits in childhood
within thinness valuing culture
genetics (first-degree relatives)
differentiation of AN
body image disturbance and fear of gaining weight differentiates from medical conditions, MDD, SUD, ARFID, and schizophrenia
social fears, obsessions, compulsions, and distortions centering around food/body shape differentiate from SAD, OCD, and body dysmorphia
disturbed body weight differentiates from BN
BN diagnostic criteria
recurrent episodes of binge eating
eating more food in 2h than normal
sense of lack of control over eating
recurrent episodes of inappropriate compensatory behaviors to prevent weight gain
both occur 1/w for 3mo
unduly influenced self-evaluation
does not only occur in AN episodes
BN or BED severity
mild: 1-3 episodes/w
moderate: 4-7 episodes/w
severe: 8-13 episodes/w
extreme: 14+ episodes/w
development and course BN
onset common in adolescence or young adulthood
onset can be precipitated by SLE
symptoms can appear to diminish with/without treatment
risk factors BN
weight concerns
low self-esteem
depressive symptoms
SAD
overanxious childhood disorder
idealization of thin body ideal
childhood sexual/physical abuse
childhood obesity
early pubertal maturation
genetics
differentiating BN
compensatory behaviors differentiate BED and atypical MDD
can be comorbid with BPD
must occur outside AN episode for at least 3mo
BN comorbidity
commonly comorbid with MDD, BD, SUD, GAD
BED diagnostic criteria
recurrent episodes of binge eating characterized by overeating and lack of control
episodes associated with 3+ of (rapid eating, uncomfortably full, large amounts when not hungry, alone over embarrassment, disgust/depression/guilt)
distress
once a week for 3mo
no inappropriate compensatory behavior
BED associated features
can occur at any weight
greater functional impairment, lower quality of life, more subjective distress, and more psychiatric comorbidity than just obesity
BED development and course
occurs at any age
dieting often follows development
those seeking treatment often older
BED differentiation
BN has compensatory behavior
can be comorbid with BD, BPD, MDD, anxiety disorders, SUD
pica diagnostic criteria
persistent eating of nonnutritive, nonfood substances (1mo)
eating inappropriate to developmental level
eating not part of culturally supported or socially normative practice
rumination disorder diagnostic criteria
repeated regurgitation of food (1mo) may be re-chewed, re-swallowed, or spit out
not attributable to associated medical condition
does not occur exclusively during AN, BN, BED, or ARFID
ARFID diagnostic criteria
eating/feeding disturbance manifested by persistent failure to meet appropriate nutritional and/or energy requirements, 1+:
significant weight loss
significant nutritional deficiency
dependence on enteral feeding or oral nutritional supplements
interference with psychosocial functioning
not attributable to associated medical condition
does not occur exclusively during AN, BN
not explained by lack of food
male ED presentation
less weight and shape concern, drive for thinness, or body dissatisfaction
more worry centered on muscularity and being large
less likely to seek treatment, start it later than women
ED assessment (male EDs)
assessments overly reliant on female ED symptoms
Eating Disorder Examination commonly used, subscales dietary restraint and eating concern less relevant for men
Eating Disorder Assessment for Men assesses male-specific symptoms, needs more research
factors enhancing ED treatment outcomes for men
improving interpersonal interactions
therapist characteristics and therapeutic relationship quality
collaborative treatment approach
male-only treatment groups
pediatric ED presentation
atypical
commonly presented as growth stunting
less likely to have body image concerns
considerations for pediatric EDs
higher screening because of atypical presentation, evaluate high-risk behaviors
lower treatment threshold
treatment for pediatric EDs
family based treatment highly recommended, largest evidence base
takes biological and genetic contributions into account, caregivers viewed as allies
3 phases: physical recovery, behavioral recovery, psychological recovery
no pharmacotherapy researched for children/adolescents
CBT-E
focuses on underlying processes of EDs, can be used for any
stages: intensive initial (formulate underlying factors), taking stock, main body of treatment, focus shift to future/final stage
CBT guided self help effective
very effective in BN and BED, moderately effective in AN
IPT for EDs
focuses on IP functioning in relation to ED
initial phase (diagnosis, sick role, IP inventory, formulation)
intermediate phase (strategies shaped by main problem area)
termination phase
works for BN and BED, not AN
interpersonal problem areas in EDs
IP deficits (social isolation or chronically unfulfilling relationships)
IP role disputes (conflicts with important other)
role transitions
grief
pharmacotherapy for EDs
antidepressants work for BN, better than antiepileptics
antidepressants work for BED behavior, weight management medication works for weight loss, stimulants work for both
no significant effective medication for AN
compulsory treatment for EDs
patient-therapist relationship remains same
initial problems more severe and duration of stay longer, but weight at discharge similar
usually feel bad at start but better by the end
long term effects not extensively studied
AN treatment resistance and motivation
resistant to treatment because of egosyntonic symptomatology
resistance significant hinderance to treatment
recommended use of socratic questioning (questioning to synthesize information and allow patient to come to conclusions alone)
factors to be considered in sexual dysfunctions
partner factors
relationship factors
individual vulnerability factors
cultural/religious factors
medical factors
sexual dysfunction specifications
lifelong or acquired
generalized or situational
mild moderate or severe (distress)
delayed ejaculation diagnostic criteria
delay, infrequency, or absence of ejaculation in 75-100% of partnered sexual activity
6mo duration
significant distress
not better explained by another disorder
delayed ejaculation associated features
prolonged thrusting to point of discomfort/exhaustion
avoiding sexual activity
feeling less sexually attractive
delayed ejaculation prevalence
least common male sexual complaint
more common in asian populations
delayed ejaculation differential diagnosis
medical conditions differentiated by problem explanation
substance use
erectile disorder diagnostic criteria
difficulty obtaining or maintaining erection, or decrease in erectile rigidity in 75-100% of any sexual activity
6mo duration
significant distress
not better explained by another disorder/stressor
erectile disorder associated features
low self-esteem, confidence, sense of masculinity
depressed affect
fear/avoidance of sexual encounters
decreased sexual satisfaction and reduced sexual desire
erectile disorder development and course
if after first sexual attempt , associated with negative/uncomfortable experience (pressured, unknown partner, drugs)
if acquired, associated with biological factors, likely to be persistent
if lifelong, associated with psychological factors
erectile disorder differential diagnosis
can be comorbid with MDD
substance use
can coexist with premature ejaculation or hypoactive sexual desire disorder
male/female hypoactive sexual desire disorder diagnostic criteria
persistently/recurrent deficient/absent sexual thoughts/fantasies/desire
6mo duration
significant distress
not better explained by another disorder/stressor
male hypoactive sexual desire disorder associated features
erectile/ejaculatory concerns
decreased/absent initiation of sexual activity
male hypoactive sexual desire disorder risk factors
past history of psychiatric symptoms
alcohol
being gay
endocrine disorders
male hypoactive sexual desire disorder differential diagnosis
substance use
other medical condition
IP factors
can occur with other sexual dysfunction
premature ejaculation diagnostic criteria
persistent/recurrent pattern of ejaculation approx 1min after penetration, before individual wishes, during 75-100% of partnered sexual activity
6mo duration
significant distress
not better explained by another disorder/stressor
premature ejaculation risk factors
anxiety disorders, especially SAD
moderate genetic contribution
female orgasmic disorder diagnostic criteria
delay, infrequency, absence, or reduced intensity of orgam is 75-100% of any sexual activity
6mo duration
significant distress
not explained by another disorder/stressor
female orgasmic disorder associated features
no association with personality, psychopathology, sexual satisfaction
difficulty communicating about sexual issues
female orgasmic disorder risk factors
wide range of psychological factors
relationship problems, physical health, sociocultural factors
medical conditions and medications
genetic contribution
female orgasmic disorder differential diagnosis
substance use
medical condition
IP factors
may occur in association with other sexual dysfunctions
female sexual interest/arousal disorder diagnostic criteria
lack of/significantly reduced sexual interest/arousal, manifested by 3+, absent or reduced:
interest in sexual activity
sexual/erotic thoughts/fantasies
initiation of sexual activity, unreceptive to initiation
sexual excitement/pleasure
sexual interest/arousal in response to cues
genital/non-genital sensations
6mo duration
significant distress
not better explained by other disorder/stressor
female sexual interest/arousal disorder associated features
problems experiencing orgasm
pain during sexual activity
infrequent sexual activity
relationship difficulties
mood disorders
poor sexual techniques
lack of information about sexuality
female sexual interest/arousal disorder risk factors
negative cognitions/attitudes about sexuality
history of mental disorders
difference in propensity for sexual excitation and inhibition
relationship difficulties
developmental history
genetics
female sexual interest/arousal differential diagnosis
nonsexual mental disorder
substance use
medical condition
IP factors
inadequate/absent sexual stimuli
can coexist with other sexual dysfunctions
genito-pelvic pain/penetration disorder diagnostic criteria
persistent/recurrent difficulties with 1+
vaginal penetration during intercourse
vulvovaginal/pelvic pain during vaginal penetration attempts
fear/anxiety about pain anticipating, during, or because of penetration
tensing/tightening of pelvic floor during attempted vaginal penetration
6mo duration
significant distress
not better explained by another disorder/stressor
genito-pelvic pain/penetration disorder associated features
other sexual dysfunctions
avoidance of sexual situations
avoidance of gynecological exams
relationship problems
genito-pelvic pain/penetration disorder risk factors
sexual/physical abuse
vaginal infection history
pain during tampon insertion
inadequate sexual education
genito-pelvic pain/penetration disorder differential diagnosis
often comorbid with other medical condition
inadequate sexual stimuli
biopsychosocial model of sex
biological, psychological, and social aspects each contribute to sexual health
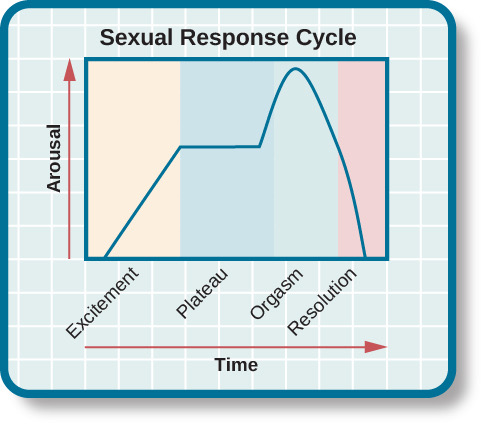
sexual response cycle
sexual response is: excitement, plateau, orgasm, then resolution
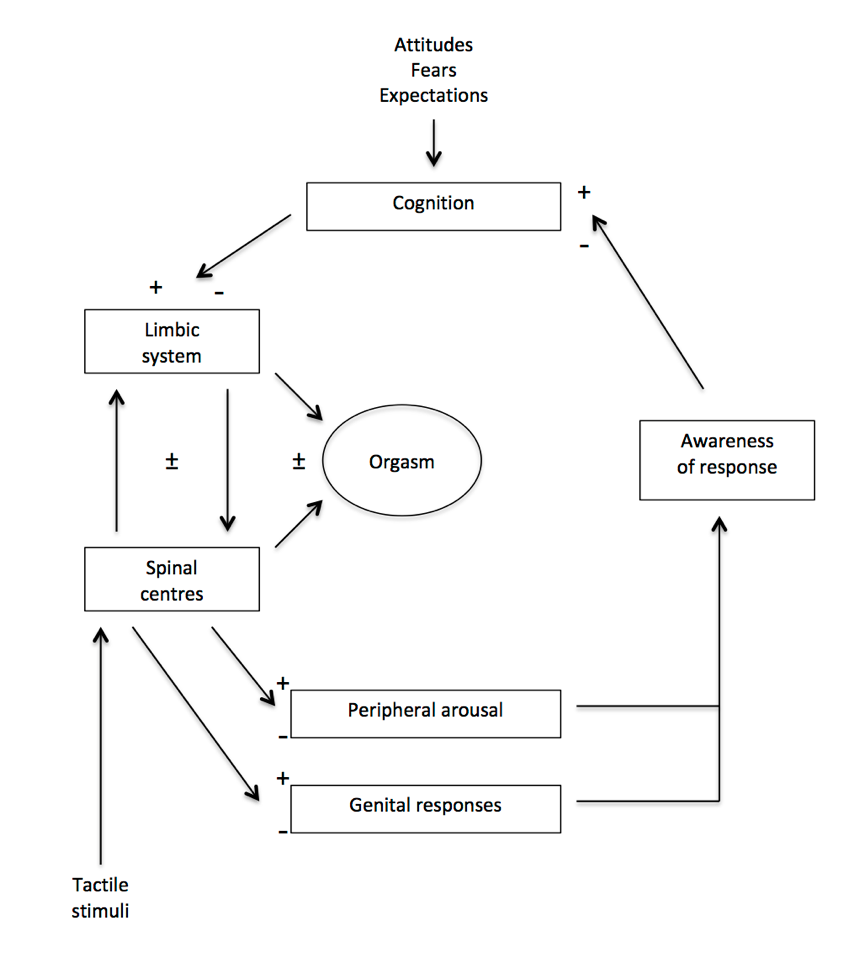
psychosomatic circle of sex
tactile stimuli → spinal cord and limbic system → physical response and arousal → awareness of response → cognition → limbic system and spinal cord → orgasm
cycle can be broken at any point
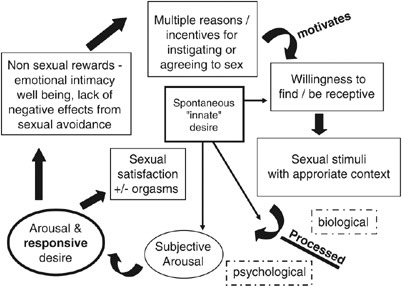
push-pull model of incentive-motivation
desire is result of being confronted with sexual stimuli (pull factor) and thoughts of sexual stimuli (push factor)
incentive motivational model
you feel desire because you’re having sex
circular model for women
desire for women is very complex
includes “spontaneous innate desire” (Freudian)
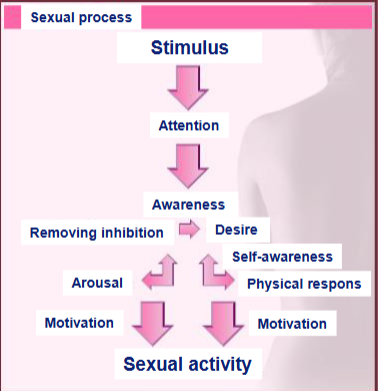
information processing model
explains spontaneous innate desire as being aroused through stimulus without being aware
process works the same for men and women, but men have more stimuli in the world so more easily turned on
diagnosis for sexual dysfunction
history of desire, arousal, orgasm, pain, muscle tension, and satisfaction
qualities of complaint
physical exam
additional assessments if needed
vasocongestion
erectile structures throughout body expand and enlarge in excitement phase
male indicators of excitement
penile erection (might not be full, easily lost)
scrotal skin tightening
testicles rise and englarge
female indicators of excitement
erection and enlargement of clitoris
vaginal lubrication
vagina becomes wider and longer
breasts, nipples, areolas enlarge
plateau phase
arousal levels off, continues with no increase
plateau in women
walls of outer 1/3 of vagina engorge and thicken
walls of inner 2/3 vagina expand
clitoris engorges and retracts closer to body and under clitoral hood
orgasm
climax of sexual arousal
highly variable between and within people
factors influencing intensity and duration of orgasm
length of arousal prior to orgasm
length of time since previous orgasm
alcohol or drug use
feelings of comfort/intimacy with partner
resolution
completion of cycle, body returns to sexually non-aroused state
EPOR model criticisms
number of stages, omitting desire
female sexual response seen as more complex than model suggests
generalizes the differences between men and women
effects of feedback
paying attention to sexual response has slightly beneficial effect on voluntary production of response
visual feedback has enhancing effect for strong erotic stimulus, opposite for weak stimulus
effects of performance demand
normal not adversely affected by demand for response, dysfunctional are
better to focus attention on self if partner not aroused (both normal and dysfunctional)
better to focus attention on partner if partner is aroused (only normal, reverse for dysfunctional)
sexual arousal cognitive model
2 components, automatic and attentional processing
initially automatic sexual appraisal of stimulus, depends on implicit sexual memory
attentional component attributes sexual meaning and processes original stimulus response
sexual content induced delay
completing a task is delayed when erotic element is present for men and women
physiological response to information processing
enhanced tendon reflex reflects early motor preparation for motivated action
effect of distraction by nonsexual stimuli on sexual response
when sexual stimulus is visual, no effect on men but inhibiting effect on women
when sexual stimulus is auditory, inhibiting effect on men and women
misinformation on sexual response
if given placebo pill said to enhance, arousal reported as minimized
if pill said to decrease, arousal is reported as enhanced
dual control model
in some circumstances appraisal of sexual stimulus directly leads to arousal, in others the arousal sequence is inhibited
anxiety and sexual response
inducing anxiety can enhance sexual response
arousal enhances focus on information processing, response depends on what focus is on
sexual satisfaction and quality of life
intrapersonal SS significant predictor of QOL for men and women, stronger for men
interpersonal SS significant predictor of QOL for women
men more likely to associate low SS with low QOL
female orgasm determinants
self-determining attitude toward sexuality
sexual experience with steady partner
happy relationship
oral or manual sex
sexual self-esteem
sexual skills, position, duration
poor female orgasm determinants
social background
physical exercise
psychological symptoms
smoking
moderate alcohol use
factors preventing female orgasm achievement
fatigue/stress
difficulty concentrating
unskillful partner
partner too fast
bad relationship quality
alcohol and sexual response
enhances sexual pleasure or reduces inhibition
associated with increased subjective arousal but decreased vaginal blood flow
alcohol myopia
as result of alcohol, attention focused on positive sexually arousing/rewarding aspects of situation and away from negative consequences and associated inhibition of arousal
alcoholism and sexual response
complex relationship
long-term toxic effects of alcohol on nervous and endocrine systems
drugs and sexual response
opiates consistently associated with reduced sexual interest and response
cocaine has positive effects with early use, negative with chronic use
marijuana sexually enhancing, but not through desire or response, but more relaxation and being in tune with partner
unclear effects of amphetamines
learning disabilities and sexuality
more likely to manifest sexuality inappropriately, because of self-fulfilling prophecy since they are believed to show inappropriate sexual behavior
somewhat less sexually active
more prone to get involved in sexual offences (naivety)
abuse characteristics increasing risk of sexual dysfunction
repeated abuse
abuse including multiple abusers
longer duration
including threat or force
abuser being father
penetrative CSA
CSA and type of sexual dysfunction
can lead to any disorder
majority have more than one dysfunction
more report arousal difficulties
CSA and cognitive associations with sex
lower positive implicit association with sexual stimuli, associated with lower SS
tendency toward threatening interpretation of sex
report more fear, anger, disgust during sexual arousal
CSA and sexual self-schema
less positive emotion words used describing sexual self-schema
positive emotion words associated with better sexual function
CSA and SNS activation
increased SNS activity starts earlier in life for CSA
SNS increases during sexual arousal, but decreases for CSA, impairing sexual function
CSA and body image/esteem
report lower overall body esteem, linked to poorer sexual function
sexual attractiveness explains most variance in excitation in women with CSA