Week 1: Appraising Evidence about Diagnostic Tests & Clinical Measures
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
126 Terms
Diagnosis
A process of integrating and evaluating the data that are obtained during the examination to describe the individual condition in terms that will guide the physical therapist in determining the prognosis and developing a plan of care.
Differential Diagnosis
A systematic process for distinguishing among two or more possible causes of a clinical disorder or condition.
Index test or measure
The diagnostic test or clinical measure of interest, the utility of which is being evaluated through comparison to a gold (or reference) standard test or measure.
Sensitivity (Sn)
The proportion of individuals with the condition of interest that have a positive test result.
Specificity (Sp)
The proportion of individuals without the condition of interest who have a negative test result.
Ability of the test to correctly identify (- test result) in someone without the disorder
Positive predictive value (PPV)
The proportion of patients or clients with a positive test result who have the condition of interest.
Ability of the test to correctly determine the % of people with the disorder from all of the people with positive test results
Prevalence
The proportion of individuals with a condition of interest at a given point in time.
Positive likelihood ratio (LR+)
The likelihood that a positive test result will be obtained in an individual with the condition of interest as compared to an individual without the condition of interest.
Negative predictive value (NPV)
The proportion of patients or clients with a negative test result who do not have the condition of interest.
Ability of the test to correctly determine the % of people without the disorder from all of the people with a negative test result
Negative likelihood ratio (LR-)
The likelihood that a negative test result will be obtained in a patient or client with the condition of interest as compared to a patient or client without the condition of interest.
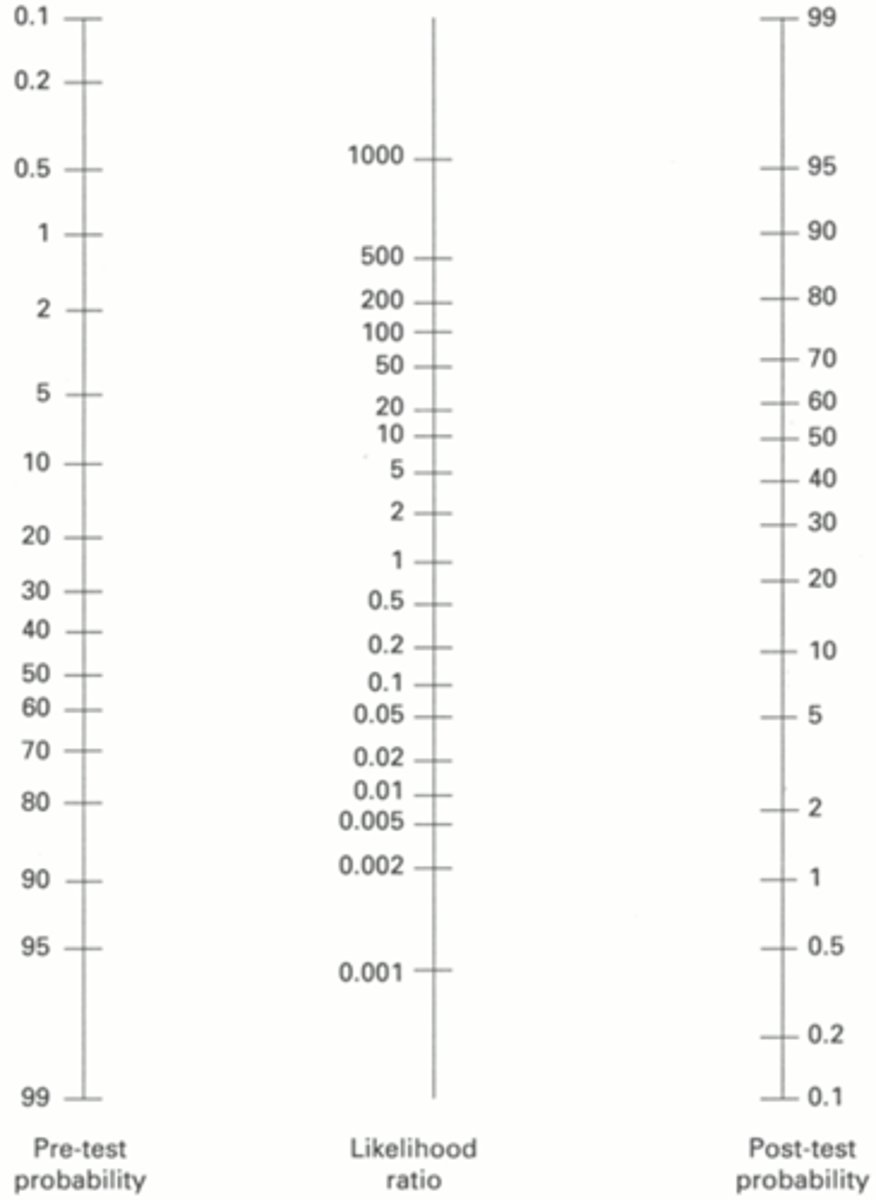
Posttest probability
The odds (probability) that an individual has a condition based on the result of a diagnostic test.
Pretest probability
The odds (probability) that an individual has a condition based on clinical presentation before a diagnostic test is conducted.
Concurrent Validity
A method of criterion validation that reflects the relationship between a test or measure of interest and a measure with established validity, both of which have been applied within the same time frame.
Instrumentation
A threat to research validity characterized by problems with the tools used to collect data that may influence the study's outcomes.
Diagnosis does what
Labels patients
Classifies a problem
Determines prognosis
Determines and guides intervention
Purpose of diagnostic tests
Focus the examination on a particular body region or symptom
Identify potential problems requiring referral to a physician or other specialist
Assist in the classification process
Key thresholds for diagnostic tests
Test threshold and treatment threshold.
Normal
The range of results beyond which the target disorder becomes highly probable.
Test threshold
"The probability below which a diagnostic test will not be ordered or performed because the possibility of the diagnosis is so remote”
Treatment threshold
The probability above which a diagnostic test will not be ordered or performed because the possibility of the diagnosis is so great that immediate treatment is indicated"
Diagnostic tests in PT
Clinical examination techniques and tests performed and/or interpreted by others (e.g., radiographs, lab tests).
Measures in Physical Therapy
Techniques we perform to quantify a patient's impairment, functional limitation, or disability.
Assessment of study credibility
-Does the study of the given test compare to a reference test? (gold standard)
-Were practioners blinded to subject grouping?
-Are important details adequately described?
-Are measures of reliability discussed?
-Are measures of Validity discussed?
Did the investigators include subjects with all levels or stages of the condition being evaluated by the index test (measure)?
Determines the usefulness of the test (measure) with respect to distinguishing between important gradations in the diagnosis or impairment
-Does the study of the given test compare to a reference test? (gold standard)
Determines the usefulness of the test (measure) with respect to distinguishing between important gradations in the diagnosis or impairment
Did the investigators evaluate (or provide a citation for) the reliability of the index diagnostic test (measure)?
A necessary precondition for validity; may be tested in a separate investigation
Was there a comparison to a "gold" (reference) standard test (measure)?
Verifies the test (measure) does what it's supposed to do
Did all subjects undergo the test (measure) of interest and the gold standard test (measure)?
Addresses the issue of bias due to manipulation of the sample
Were the individuals interpreting each test's (measure's) results unaware
Addresses the issue of measurement bias
Was the time between application of the index test (measure) and the "gold standard" comparison diagnostic test (measure) short enough to minimize the opportunity for change in the subjects' condition?
Addresses the potential for misclassification (inaccurate quantification) due to natural changes in the subjects' status (e.g., healing)
Was the study repeated on a second set of subjects?
Addresses the reproducibility of the results
Additional Considerations for diagnostic studies
Is there a detailed description of the:
Clinical Setting
Inclusion criteria
Exclusion criteria
Protocol for test(s)
Reliability
The degree to which a test produces stable and consistent results.
Sources of variability for reliability
Observer
Subject
Instrument
Environment
Types of reliability measures
Standard Error of Measurement (SEM)
Correlation coefficient (e.g., Pearson r, ICC, Kappa, etc.)
ICC AND Pearson's r are for
interval and ratio data
Spearman's rho is used for
ordinal data
Validity
Measure represents what it's supposed to represent.
Types of measurement validity
All instruments
Face validity
Criterion validity
Concurrent validity
Discriminant validity
Predictive validity
Types of measurement validity
Survey instruments: everything plus...
Content validity
Construct validity
SpPin
High specificity indicates that a positive test result can rule in a disorder.
High specificity + Positive test result = Rule in disorder
Sensitivity (SnNout)
High sensitivity indicates that a negative test result can rule out a disorder.
Predictive values depend on
prevalence
LRs are independent of
Prevalence
LRS can be applied to
individuals
Formula for sensitivity
Patients with the disease who test positive/all patients with the disease
a/a+c
Formula for specificity
Patients without the disease who test negative/ all patients without the disease
d/b+d
Formula of PPV
Patients with the disorder who test positive/ all patients who test positive
PPV = a/(a+b), where a is true positives and b is false positives.
Formula for NPV
Patients without the disorder who test negative/ all patients who test negative
NPV = d/(d+c), where d is true negatives and c is false negatives.
Formula for PLR
sensitivity/(1-specificity)
(a/a+c)/(1-(d/b+d))
Formula for NLR
(1- sensitivity)/specificity
(1-(a/a+c))/(d/b+d)
Receiver operating characteristic curve
A graphic way to evaluate different test scores with respect to the number of true-positive and false-positive results obtained at each threshold or cut point
Y-axis of ROC curve
Sensitivity
X-axis of ROC curve
1 − Specificity
Area under the curve (AUC)
Reflects diagnostic usefulness
Pre-test probability
What you think the odds are that the patient has the disorder before you conduct the diagnostic test
Post-test Odds
What you think the odds are that the patient has the disorder after you conduct the diagnostic test
Post-test Probability
Probability of the disorder once the test results are obtained
LR+ > 10 or LR - < 0.10 indicates
large and conclusive change
LR+ = 5-10 or LR- = 0.10-0.20
moderate change
LR+ = 2-5 or LR- = 0.20-0.50
Small but sometimes important change
LR+ = 1-2 or LR- = 0.50-1.0
Negligible change in pre-test probability
Nomograms
Visual tool to convert: Pretest probability → Posttest probability
P-value
The probability that the result occurred due to chance
95% Confidence Interval (C.I.)
The range of values within which the true value is estimated to lie within a 95% probability
If an LR = 1.0 it represents a
50:50 chance of increasing or decreasing the probability of a diagnosis
Should you use this evidence?
Is the study high quality (e.g., does the design minimize bias)?
Are the results important enough to use?
Is the test or measure of interest available, practical, and safe for application in the clinical setting?
Was your patient or client represented in the study sample?
Can you estimate the pre-test probability of the disorder?
Patient's or client's values and preferences re:
Diagnostic tests purpose in PT
Help focus the examination process to a particular body region or system
Fatal flaw in research quality
If not all subjects receive the reference standard, accuracy is inflated
Limitations of Traditional Test Interpretation
Sensitivity and specificity are population-based, not patient-specific
They do not tell you how much probability changes for an individual patient
Preferred diagnostic test measurement
Likelihood ratios
Decision thresholds
Below test threshold → don't test; Above treatment threshold → treat
Tests with LRs close to 1.0
Are essentially useless
Core purpose of diagnostic tests
Should not be used in isolation; they refine clinical judgement but don't replace it
Strategies for control of unwanted factors (minimizing bias)
Clear inclusion/exclusion criteria
Subjects suspected to have condition of interest
Clear performance protocols
Include criteria for positive/negative test
Verify examiner's competence
Verify presence/absence of condition of interest via comparison test
Masking of examiners
Observed score (X)
X = true score (T) and an error component (E).
Sources of measurement error
Rater, instrument used, patient/subject being measured, challenge when response is inherently unstable.
Intra-rater
Measurement error within individuals.
Inter-rater
Measurement error between individuals.
Pearson's product moment correlation (r)
Statistical method used for interval/ratio data to evaluate reliability of interval or ratio data
ICC
Intraclass correlation coefficient, used to assess reliability of interval or ratio data
Spearman's rho (p)
Statistical method used for ordinal data to evaluate reliability
Kappa (k)
Statistical method used to assess agreement between raters of nominal data
kappa 0-0.25
little to no change
kappa 0.26-0.5
fait degree of relationships
kappa 0.51-0.75
moderate to good degree of relationship
kappa 0.76-1.00
good to excellent degree of relationship
2x2 tables
chi square statistic indicated an association between two variables; simpler analysis than linear regression --> easier to explain to policymakers but loose a lot of information through simplification
High sensitivity means
high rate of false positives
High specificity means
higher false negatives
Receiver Operating Characteristic (ROC) curves
Used to determine cut points for sensitivity and specificity.
Sensitivity and specificity have some limitations
Indicate a test's performance in individuals whose status is known
Reduce information to two options based on cut point for positive/negative
ROC Y-axis
true positive/ sensitivity
ROC X-axis
1-specificity
true negatives
Likelihood ratios
Mathematical calculations that reflect a diagnostic test's ability to provide persuasive information.
P value
Probability that result occurred due to chance.
Advantages of LRs
Ratios can be calculated for all levels of test results
Not dependent on prevalence of the condition
Can be applied to individuals
LR of 1.0
Value of 1.0 = no added info, no better than chance; coin flip
Confidence interval
Range of scores within which the true score is estimated to lie within a specified probability.
Clinical measures
Used to quantify and describe a patient's impairments in body functions and structures.