8 - Transport in Mammals 🫀
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
28 Terms
Explain the ways in which the structure of an artery is adapted to its function
1) thick tunica media to withstand high blood pressure
2) endothelium/tunica intima are smooth so there's little friction to blood flow
3) elastic fibres stretch to allow surges in blood flow and recoil to maintain blood pressure
4) smooth muscle contacts to regulate blood flow
5) collagen fibres avoid rupturing
Explain how tissue fluid is formed in the capillary network
1) higher hydrostatic pressure of blood at the start of the capillary
2) causes leakage of plasma
3) glucose, amino acids and salts are filtered out
4) gaps between endothelial lining allow the plasma to leak
capillaries
1) wall made of endothelium; one cell thick
2) 7 micrometers in diameter
3) gaps present between individual cells that from the endothelium allow plasma to leak through forming tissue fluid
vasovasorum
Network of small blood vessels that provide blood supply and nourishment for tunica externa and media of large blood vessels
structure of arteries
1) tunica intima/endothelium - very smooth, single layer of cells
2) tunica media - thickest in artery; elastic fibres, collagen fibres, smooth muscle
• allows artery wall to stretch and recoil in response to pressure changes
3) tunica externa - collagen fibres, elastic fibres
Structure of veins
1) large lumen
2) tunica externa is thickest in veins (mostly collagen fibres)
3) tunica media is very thin (contains some smooth muscle and fibres)
tissue fluid
1) as blood flows through capillaries within tissues some plasma leaks out due to the pressure and seeps into places between cells of tissues; this is tissue fluid
2) fluid tends to flow out of capillaries at arterial ends and into capillaries near venuous ends
3) if blood pressure is too high, too much fluid is forced out of capillaries causing accumulation of fluid; oedema
6) it's through tissue fluid that exchange between cells and blood occur
role of lymphatic system
1) drainage system
2) digestive (assimilation of fatty acids)
3) immunity (production of lymphocytes)
adaptation of lymphatic system
1) lymphatics are tiny blind ended vessels
2) they contain valves which allow tissue fluid to flow in but not out
3) walls are wide enough to allow larger protein molecules to pass through
4) fluid inside lymphatics is lymph
5) lymph is transported to subclavian vein
6) lymph vessels have smooth muscle in their walls which contact to push lymph along
red blood cells/erythrocytes
1) contains haemoglobin which gives red colour and transports oxygen
2) produced in the bone marrow
3) biconcave disc shape - inc SA in relation to volume
4) spongy/flexible- have a specialised cytoskeleton made of protein filaments that allow them to be squashed
5) no nucleus, ER, mitochondria - more space for Hb maximising amount of oxygen carried
6) broken down in spleen
structure of heart
1) consists of two atria and 2 ventricles
2) right and left side separated by septum
3) made of cardiac muscle
4) atria and ventricles have valuables between them called atrioventricular valves which prevent from ventricles back to atria
• right side - tricuspid
• left side - bicuspid/mitral
Types of valves
1) atrioventricular- tendons
2) semilunar - pockets
atrial systole
1) heart is filled with blood and atria contract
2) pressure in atria > than ventricles so blood forces AV valves open and flows into ventricles
3) semilunar valuables in pulmonary veins and venacava prevent backflow from atria
ventricular systole
1) ventricles contact increasing pressure and pushing blood out of heart
2) pressure in ventricles > than atria forces AV valves shut
3) blood rushes upwards into aorta and pulmonary artery as pressure of blood forces aortic semilunar valves open
ventricular diastole
1) muscle relaxes - pressure in ventricles drops
2) whole of heart muscle relaxes during diastole;
• blood flows into atria
• some blood leaks down into ventricles
3) presence of semilunar valves prevent backflow of blood from aorta and pulmonary artery
4) atrial muscle then contracts forcing blood into ventricles, AV valves close
5) pressure in arteries is higher than ventricles causing the aortic semilunar valves to close
outline the cardiac cycle
1) SAN (pacemaker) sends waves of excitation which stimulates atria to contact
2) non conducting tissue between atria and ventricles prevent them from contracting together
3) AVN delaying impulse allows atria to empty into ventricles/ contract first
4) AVN sends impulses down to bundle of his and along purkine fibres
5) this causes ventricles to contact from the base upwards
- brief break when no impulse is generated allowing blood to enter atria
Bohr shift
1) presence of high partial pressures of carbon dioxide causing Hb to release oxygen is the Bohr effect
2) carbon dioxide dissolved in cytoplasm of RBC forming carbonic acid, reaction is catalysed by carbonic anhydrase
CO2 + H2O <—-> H2CO3
H2CO3 <—-> H+ + HCO3-
3) Hb has higher affinity for H+ ions than O2 therefore O2 is released
Carbon dioxide transport
85% - HCO3- diffuse out of RBC into blood plasma and are carried in solution
5% - CO2 that hasn't dissociated dissolves in blood plasma
10% - CO2 combines directly with anime groups of Hb forming carbaminohaemoglobin
how carbon dioxide (CO2) and For
hydrogen ions (H+) play a role in the unloading of oxygen from haemoglobin [5]
1) diffusion of carbon dioxide
2) into red blood cell from correct source
3) carbonic acid formation followed by H+ production due to action of enzyme
4) carbonic anhydrase
5) haemoglobin has a higher affinity for hydrogen ions than oxygen; haemoglobin releases oxygen more easily in acidic conditions
6) formation of haemoglobinic acid
7) higher partial pressures of CO2 linked to (oxy)haemoglobin releasing oxygen more readily; Bohr shift
8) formation of carbamino-haemoglobin
Explain the need for transport systems in multicellular plants and animals (3)
1) small surface area to volume ratio
2) long(er) distances (to reach cells / tissues)
3) diffusion (alone), too slow / insufficient / unable to satisfy needs
Effect of nicotine on the cardivasculour system
1) raises, heart rate / blood pressure
2) reduces diameter of arterioles
3) decreases blood flow to body extremities
4) increases 'stickiness' of platelets / promotes blood clotting / thrombosis
systolic blood pressure
maximum blood pressure in arteries
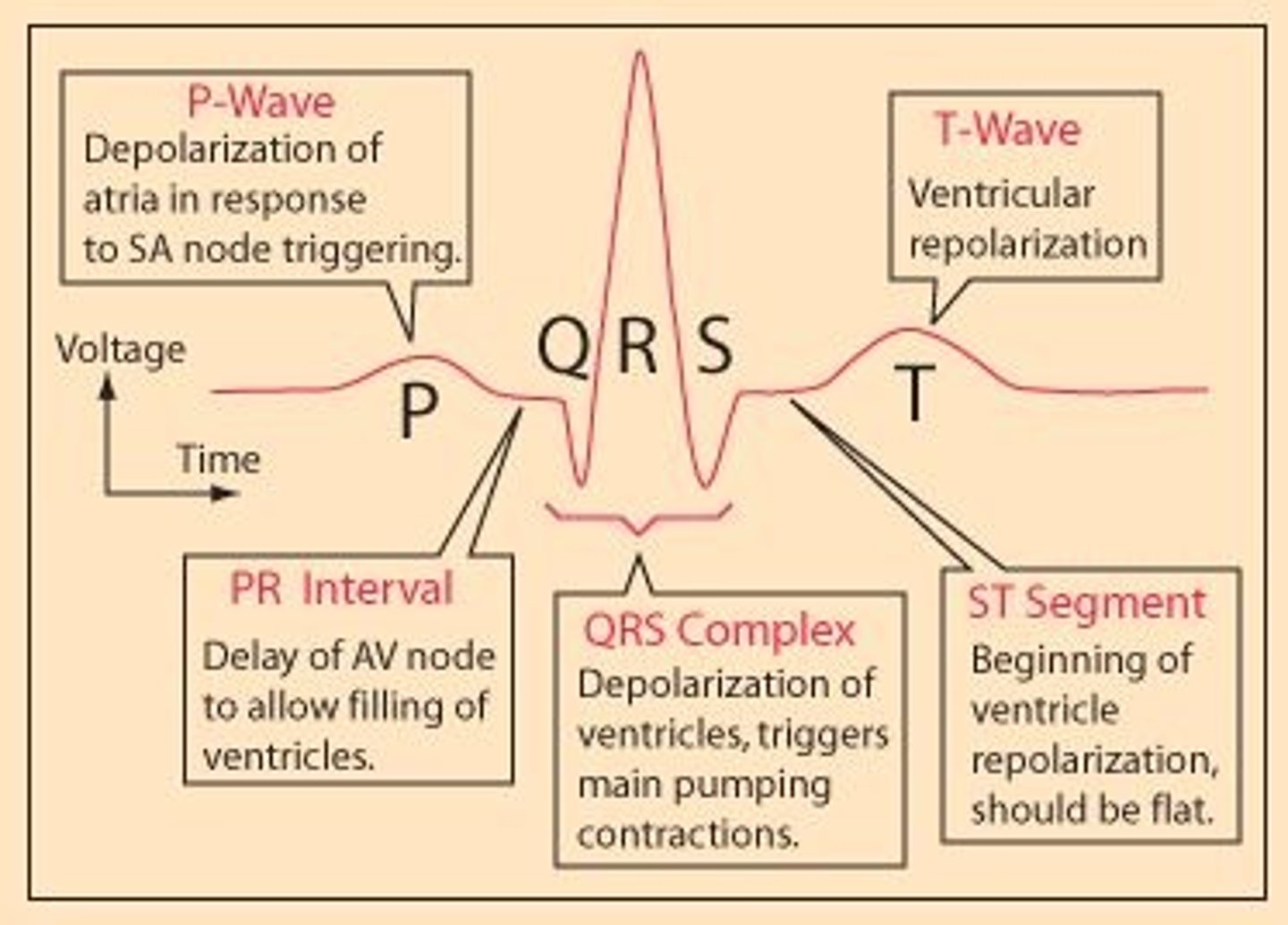
PQRST waves
electrical activity of heart during a single heart beat
1) P wave - SAN and atria contract
2) PQ - impulses reach AVN, 0.1s delay allows atria to empty
3) QRS - ventricular contraction
4) T wave - recovery of ventricles (heart rests)
Describe the role of SAN
1) acts as the pacemaker of the heart
2) emits waves of excitation at regular intervals
3) stimulates atrial contraction
Outline the role of Hb in the transport of CO2
1) Hb combines with carbon dioxide
2) carbon dioxide reacts with amine groups
3) to form carbaminohaemoglobin
4) each polypeptide can carry a molecule of CO2
5) CO2 remains bound to Hb until in a region of high pO2
6) carbonic acid dissociates to form H+ ions which bind to Hb forming haemoglobinic acid
7) hydrogencarbonate ions to plasma
Explain why the wall of the left ventricle in the heart is thicker than the wall of the right ventricle.
1. to generate a higher blood pressure (during systole)
2. to overcome higher resistance
3. to transport blood a greater distance
4. right ventricle generating low pressure to avoid damaging capillaries in the lungs
State precisely where the sinoatrial node is located.
wall of right atrium
Explain the role of the atrioventricular node in the coordination of heart action.
passes the impulse wave of excitation to the Purkyne fibres, allows a short delay so so atria and ventricles don't contract at the same time