Sleep Apnea & Obesity Hypoventilation Syndrome
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
what are the types of sleep apnea?
- obstructive (OSA)
- central (CSA)
what is obstructive sleep apnea (OSA) characterized by?
obstructive apnea, hypoapnea &/or respiratory effort-related arousals
- caused by repetitive collapse of the upper airway during sleep
what is apnea?
cessation or near cessation of airflow for at least 10 seconds
what is hypoapnea?
reduction of airflow that is insufficient to meet criteria for apnea
- airflow decreases at least 30% & lasts at least 10 seconds
what are respiratory effort-related arousals?
arousals that do not meet the criteria for apnea or hypoapnea
in healthy individuals, reduced upper airway (UA) muscle activity during sleep is of little consequence; however, how may this impact susceptible individuals?
the UA narrowing may lead to obstruction
what are central apneas?
periods of absent airflow due to lack of respiratory effort
what is the difference between obstructive sleep apnea (OSA) & central sleep apnea (CSA)?
OSA:
respiratory efforts are present during cessations of airflow
CSA:
respiratory efforts are NOT present during cessations of airflow
what is the underlying issue in CSA?
the brain is not sending signals to the muscles that control breathing
- which leads to the patient becoming apneic
central apnea is usually due to:
a. hypoventilation
b. hyperventilation
b. hyperventilation
how does hyperventilation lead to central apnea?
causes hypocapnia
- if CO2 decreases below certain threshold, respiratory drive is decreased resulting in apnea
- once CO2 reaccumulates to normal levels or becomes slightly elevated, the body responds w/ hyperventilation
hyperventilation --> ↓ CO2 --> ↓ RR --> apneic event -->
↑/normal CO2 --> hyperventilation (& cycle repeats)
what is the most common sleep-related breathing disorder?
OSA
- CSA is less prevalent
1 multiple choice option
it is estimated that ___ of the cases of moderate-severe OSA are undiagnosed
80%
in a population based study (w/ individuals >/= 40 y/o), approx. half of the CSA cases were associated w/ ________________ breathing
cheyne-stokes
3 multiple choice options
median age of patients w/ CSA was ________.
69 y/o
CSA is more common among patients w/ _______________.
heart failure
3 multiple choice options
risk factors for OSA:
- older age
- male gender
- obesity
- craniofacial & UA abnormalities (particularly in Asian pts)
- smoking
- fam hx of snoring or OSA
- nasal congestion
- variety of medical conditions
risk factors for CSA:
- age (> 65 y/o)
- male gender
- afib
- chronic opioid use (including, methadone)
s/s of sleep apnea:
- daytime sleepiness
- inattention/poor concentration/moodiness
- snoring, gasping, choking, or any interruptions during sleep (including apneic events)
- paroxysmal nocturnal dyspnea
- nocturia
- nocturnal angina & palpitations
- morning HAs
- sleep maintenance insomnia
- decreased libido & impotence
what is the most common clinical/PE finding in patients w/ OSA?
obesity (BMI >/= 30 kg/m3)
- although, some may be overweight or normal weight
what possible things may you find on PE that could cause a crowded upper airway?
- craniofacial conditions (receding jaw & wide craniofacial base)
- tonsillar hypertrophy
- elongated or enlarged uvula
- high arched or narrow palate
what is the name of the classification system used to quantify airway narrowing?
mallampati classification
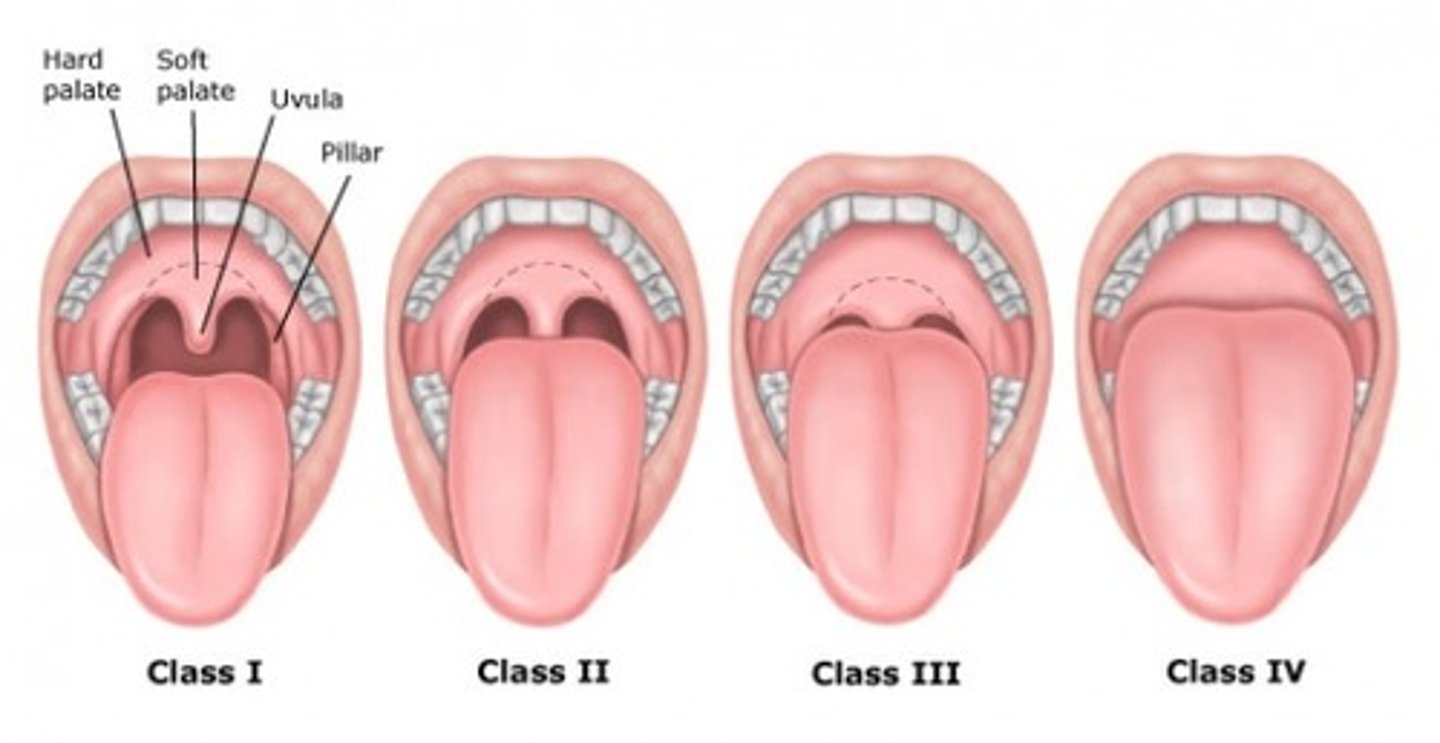
classes _____ of the mallampati classification are considered positive for narrow airway
3 & 4
signs of sleep apnea on PE:
- obesity
- crowded upper airway
- nasal septum deviation & nasal polyps
- increased neck size or waist circumference (OSA)
- floppy eyelid syndrome
are there any PE findings that are specific for CSA?
no, other than findings that may correlate w/ an associated disease (such as, CHF)
- for example: peripheral edema, S3 gallop, JVD, etc..
what are the recommendations regarding screening for OSA?
for those who are asymptomatic & w/o risk factors, use clinical judgement to determine if use of questionnaires is needed
for those who are symptomatic or at high risk, screening should be considered
examples of OSA screening questionnaires:
- STOP Bang
- epworth sleepiness scale (ESS)
is overnight pulse oximetry recommended for diagnostic eval of OSA?
no
is overnight pulse oximetry recommended for screening for sleep apnea?
use w/ caution
is pulse oximetry highly sensitive or specific for OSA?
specific
- but low sensitivity
reasons why overnight pulse oximetry should be used w/ caution to screen for sleep apnea:
- some pts (younger) have ability to maintain adequate O2 throughout apneic event
- machine cannot differentiate if pt is awake or asleep (particularly important in hospitalized patients)
- if normal, cannot r/o sleep apnea, so will still have to do a sleep study
- if abnormal, sleep study still needed to confirm dx
when is a home sleep study (HSAT) a reasonable alternative to an in-lab polysomnography (PSG)?
for patients w/ highly suspected uncomplicated OSA
when is the only time that home sleep studies (HSAT) should be considered?
in those w/ a high clinical suspicion of sleep apnea w/o multiple co-morbidities & who are not a mission critical worker
who does the AASM state have a high pretest probability of moderate-severe OSA?
pts w/ daytime hypersomnolence & at least 2 of the following 3 criteria:
- habitual loud snoring
- witnessed apnea
- gasping/choking
or diagnosed HTN w/o additional comorbidities
what is the preferred test for a patient who does not meet the criteria for high-pretest probability of mod-severe OSA?
in-lab sleep study
2 multiple choice options
can sleep apnea be ruled out w/ a HSAT?
no
1 multiple choice option
what is the gold standard test for sleep apnea?
in-lab sleep study (polysomnography [PSG])
patients who meet the criteria for a diagnosis of OSA are traditionally classified as having mild, moderate or severe disease, based on their..
apnea-hypoapnea index (AHI)
what is apnea-hypoapnea index (AHI)?
(apneas + hypoapneas)/total sleep time in hrs
AHI between 5-14 =
mild sleep apnea
AHI between 15-30 =
moderate sleep apnea
AHI > 30 =
severe sleep apnea
for patients who are diagnosed w/ OSA, & who choose positive airway pressure (PAP) therapy, a ___________ study is recommended
titration
what is a titration study?
when PAP therapy is applied to the patient & the sleep technician calibrates the appropriate pressure that controls a patient's sleep apnea
what should all patients diagnosed w/ OSA be offered as initial therapy?
positive airway pressure (PAP)
- options: CPAP or BiPAP
benefits of CPAP:
can be set to:
- a pressure based on what was successful in treating the patient's sleep apnea during a titration study
- autotitrate (if device detects more resistance it will increase in pressure & vice versa)
when would BiPAP be used?
reserved for patients who fail or do not tolerate CPAP
why may patients feel "smothered" by the CPAP?
it may be difficult to exhale against the positive pressure
- it's a continuous pressure throughout inhalation/exhalation
why may BiPAP provide relief for these patients that feel "smothered" by the CPAP?
bc the IPAP is stronger than the EPAP & mimics a more natural breathing pattern
what are some alternative options for treatment of OSA?
- oral appliances
- upper airway surgery
for pts w/ mild-moderate OSA who decline or fail to adhere to PAP therapy an ______________ can be considered
oral appliance
what are the major types of oral appliances used to treat OSA?
- mandibular advancement splints
- tongue retaining devices
disadvantages of using an oral appliance for treatment:
- requires a qualified dentist
- less effective than PAP at improving AHI & oxyhemoglobin saturation
when is upper airway surgery an option for OSA treatment?
when PAP &/or an oral appliance are ineffective or declined (after at least a 3 month trial of therapy)
upper airway surgery is most effective for tx of OSA if there is an obstructing lesion that is correctible, such as:
- tonsillar hypertrophy
- adenoid hypertrophy
- cranial abnormalities
are there any pharmacologic agents proven to be effective in tx of OSA?
no
1 multiple choice option
lifestyle modifications for those w/ OSA:
- weight loss (healthy diet & exercise)
- change sleep position
- avoid alcohol (it may worsen OSA)
_________ should be avoided in untreated OSA patients
benzos
other meds that may exacerbate OSA include:
- antiepileptic drugs
- sedating antidepressants
- antihistamines
- opiates
which is 1st line for OSA or CSA?
a. CPAP
b. BiPAP
a. CPAP
what can be tried for CSA patients w/ an EF >45% who failed CPAP therapy or who do not tolerate CPAP?
an adaptive sero-ventilation (ASV)
what is an ASV?
an autotitrating BiPAP that provides a back-up respiratory rate
the AASM recommends against the use of ASV in CSA patients w/ an EF _____%
what trial proved that we should use caution when considering an ASV in pts w/ heart failure?
SERVE-HF trial
- due to increased mortality (may be due to ↓ CO & SV or cheyne-stokes respirations)
how is nonadherence to PAP therapy defined?
using PAP therapy for < 4 hrs/night or < 70% of nights in total
to be considered compliant, how often must a patient wear their PAP therapy device?
- at least 4 hrs/night
- 5 to 7 nights/wk (or > 70% of nights)
potential barriers to proper PAP therapy compliance:
- mask related issues
- intolerance of pressure
- nasal or upper airway dryness or congestion
- air leaks
potential complications of untreated sleep apnea:
- cardiac disease or arrhythmias
- cancers
- CKD
- cognitive & behavioral disorders
- CVA (stroke)
- asthma
- eye disorders
- metabolic disorders
- weight gain
what is obesity hypoventilation syndrome (OHS)?
presence of awake alveolar hypoventilation (arterial PaCO2 > 45 mmHg) in an obese individual (BMI >/= 30)
- which cannot be attributed to other conditions assoc. w/ alveolar hypoventilation (ex: neuromuscular disorders)
a complex interaction of the following factors is likely involved in the pathogenesis of OHS:
- sleep disordered breathing (SDB)
- altered pulmonary mechanics
- impaired ventilatory control
- CO2 over production
the prevalence of OHS increases as BMI ______________.
increases
s/s of OHS
- hypersomnolence
- loud snoring
- choking
- fatigue
- impaired concentration & memory
- small oropharynx
- thick neck
- obesity
possible diagnostic features of OHS:
elevated HCO3 & CO2 (hypercapnia)
- PaO2 < 70 (hypoxemia) or polycythemia may also be present
polycythemia may be seen in OHS or sleep apnea due to _____ventilation
hypoventilation
1 multiple choice option
OHS is often a diagnosis of exclusion which can be made when the following criteria are met:
- obesity (BMI > 30)
- awake alveolar hypoventilation (pCO2 > 45 on ABG)
- alternative causes have been excluded
why is a sleep study also recommended for diagnosis of OHS?
bc most people w/ OHS also have sleep apnea
treatment of OHS:
- CPAP if pt also has OSA (2nd line: BiPAP, 3rd line: average volume pressure support (AVAPS))
- repeat ABGs in 1-3 months
- behavioral management/lifestyle modifications