Interpretation Bias & Basics
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
What are the steps for the overview of interpretation principles?
Select appropriate image type
Make sure image is diagnostic
Identify presence of any abnormalities in the image
Determine what the abnormality is (differential diagnosis)
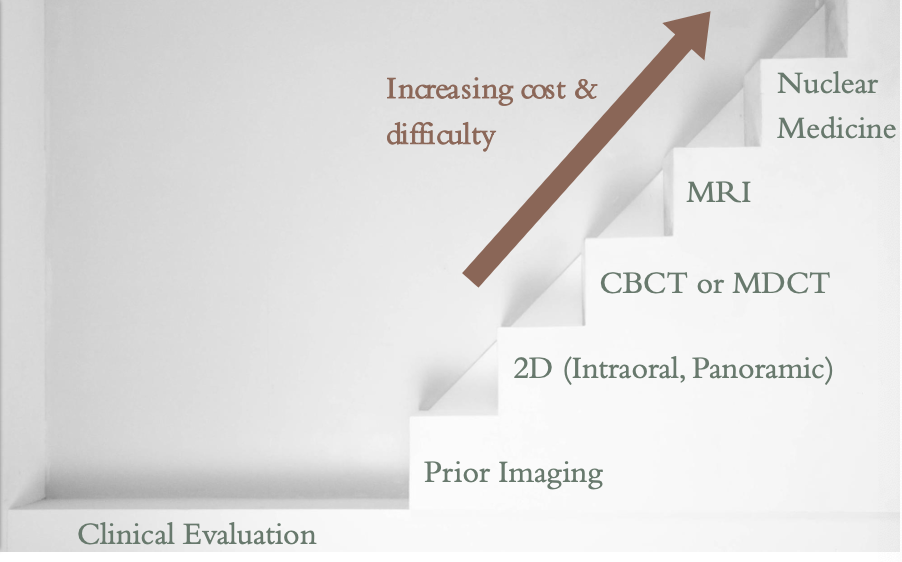
What is image selection?
Effectiveness of imaging refers to likelihood that it will meet diagnostic objectives
Imaging should be guided by
The perceived nature or severity of abnormality (size and accessibility)
Efficacy of technique to accurately reveal characteristic radiologic features of abnormality
Amount of image detail required (density, contrast and spatial resolution)
Radiation dose, accessibility and cost to patient
What are intraoral images good for?
Highest spatial resolution relative to other modalities in dentistry
Best for evaluating diseases involving teeth and supporting structures
What are panoramic images good for?
Allows examination of more extensive disease involving a larger area (includes TMJs, more of maxillary sinuses)
Lower image resolution and more artifact than intraoral
What are CBCT and MDCT images good for?
Indicated when there is a need to evaluate anatomy in multiple dimensions without anatomical superimpositions
What are MRI images good for?
Soft tissue evaluation (more info than MDCT but at a lower resolution and hard tissues less well visualized)
What are imaging steps?
What are intraoral images?
Full-mouth radiographic series (FMX) or intraoral complete series- survey of whole mouth intended to display crowns and roots of all teeth, periapical areas, interproximal areas and alveolar bone including edentulous areas
Periapical images
Bitewing images
What are periapical images good for?
Optimal to demonstrate roots, supporting structures (periodontal ligament and lamina dura), and peri-radicular alveolar process
Limitation is geometric distortion
What are bitewing images good for?
Optimal for revealing interproximal caries
Project the crests of the alveolar processes relative to adjacent teeth with minimal distortion
What is a panoramic image?
Visualization of a larger region of anatomy than intraoral images
What is the main disadvantage to panoramic images?
Lack of fine anatomic detail (lower spatial resolution than intraoral)
What are some other disadvantages to a panoramic image?
Susceptibility to patient positioning and movement
Unequal magnification and geometric distortion across image
Complex pattern of superimposition of anatomic structures challenges interpretation
Occasionally overlapping structures can hide lesions (ex. cervical spine)
Why is a panoramic image not as useful as IOs?
It doesn’t detect small carious lesions, fine structure of periodontium, or early periapical disease
It doesn’t provide much additional useful information beyond an FMX for most patients
Panoramic combined with BWs and selected PAs could provide diagnostic information similar to FMX
What is image quality?
Reliability of an image in its representation of the true state of anatomy examined
What are the parameters of radiographic image quality?
Image sharpness
Spatial resolution
Contrast resolution
Magnification
Distortion
What is the quality criteria for radiographs?
Should record the complete area/s of interest on the image
Have the least possible amount of magnification and distortion
Have optimal contrast and spatial resolution to facilitate interpretation for the diagnostic task
What should quality criteria do for your image?
Assess whether the diagnostic objectives of the imaging examination were adequately met
If not, determine which additional images to take and/or which images need to be retaken to meet the diagnostic objectives
What is a systematic search strategy?
Improves detection of abnormalities
Helps avoid “satisfaction of search”
what is the systematic search strategy for a periapical image?
You would look for:
crown
root structure
pulp chamber and root canal system
periodontal ligament space
lamina dura
what is the systematic search strategy for a panoramic image?
You would look for:
Posterior border of maxilla
maxillary sinus floor
zygomatic process of maxilla
infraorbital rim
condyles
what is the systematic search strategy for a CBCT image?
You could look for review of captured anatomy through entire volume in axial, coronal, and sagittal planes
What is diagnostic reasoning?
Method of identifying features of the abnormality that will assist in arriving at a plausible interpretation or diagnosis
What is important for interpretation accuracy?
Feature memorization is generally less effective than understanding basic disease mechanisms
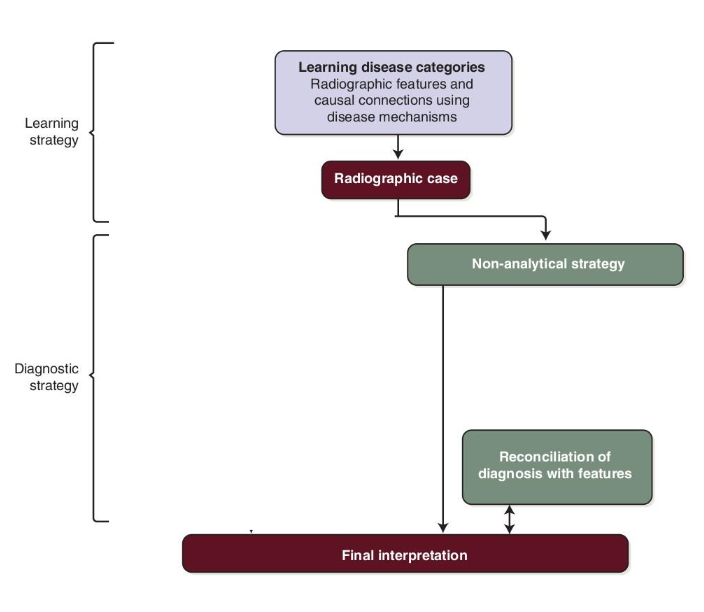
What is a non-analytic strategy for diagnostic reasoning?
Assumes viewing abnormality in its entirety on a global level leads to a more holistic diagnostic hypothesis
Deliberate search for features that support the hypothesis
“pattern recognition”
Success is limited by experience level
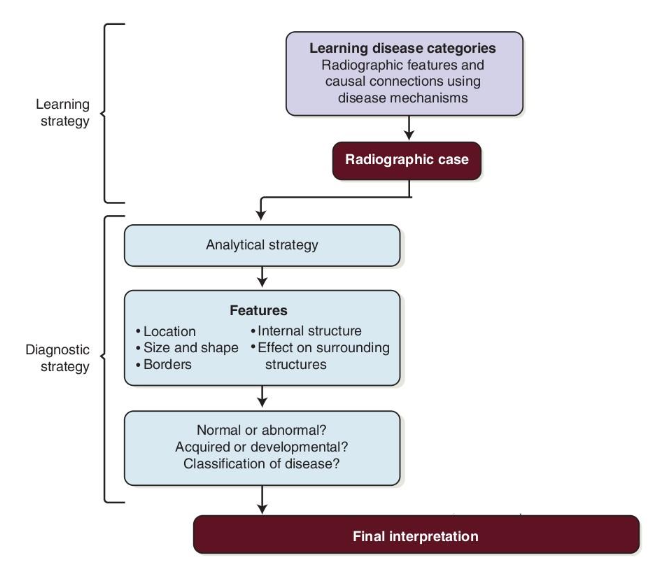
What is an analytical strategy for diagnostic reasoning?
Step-by-step analysis of all features which are used to make interpretation/diagnosis
Reduces bias and premature closure of decision-making process
How can analytical and non-analytical strategies be complementary?
They can be used together but
Avoid use of non-analytical alone
Avoid rote memorization of lesion features
What are the steps for the analytical strategy?
Describe lesion features
Interpret significance of observed features
a. Use features to determine disease category
b. Narrow down to differential diagnosis- short list of most likely entities
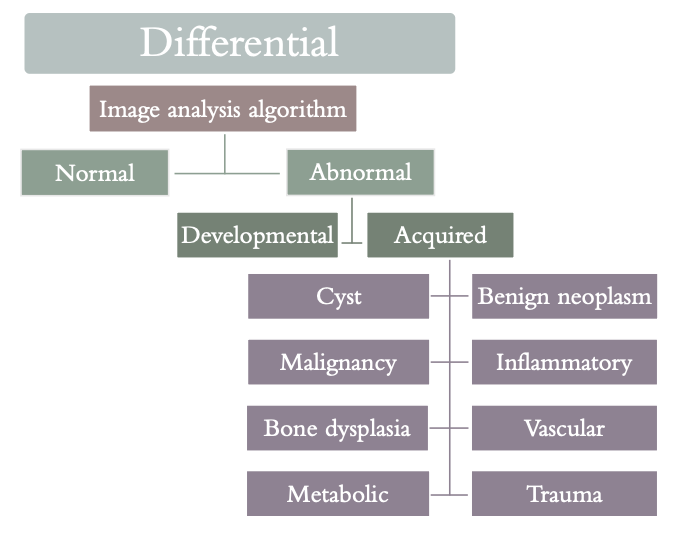
What is the acronym for analytical strategy?
L- location
E- Edge (border)
S- shape/size
I- internal content
O- other structures
N- number
What is the description for lesion?
Localized/generalized
Single/multifocal
Unilateral/bilateral
Epicenter/position in jaw
What is the description for external border/edge (periphery)?
Well or poorly defined
corticated or non-corticated
What is the description for internal content/structure/pattern?
Lucent/opaque/mixed
Septations
Calcifications
What is the description for other effects on structures/anatomy?
Teeth, inferior alveolar canal,, maxillary sinuses, cortices, trabecular pattern
What is the description for number?
Solitary or multiple
What is the first step in the analysis of intraosseous lesions?
Localize the abnormality
Anatomic position (epicenter)
Localized or generalized
Unilateral or bilateral
Single or multifocal
What is the second step in the analysis of intraosseous lesions?
Assess periphery and shape of abnormality
Well defined (corticated, punched out, sclerotic, soft tissue capsule)
Poorly defined (blending, invasive)
Shape (circular, scalloped or irregular)
What is the third step in the analysis of intraosseous lesions?
Analyze the internal structure
Totally radiolucent or totally radiopaque
Mixed radiolucent and radiopaque (describe the pattern)
What is the fourth step in the analysis of intraosseous lesions?
Assess the effects of the lesion on adjacent structures
Teeth, lamina dura, periodontal ligament space
Inferior alveolar nerve canal and mental foramen
Maxillary sinus
Surrounding bone density and trabecular pattern
Outer cortical bone and periosteal reactions
What is the fifth step in the analysis of intraosseous lesions?
Formulate an interpretation
What is epicenter?
The geometric center of the lesion
Midpoint of the mesial-distal, superior-inferior, and buccal-lingual extensions
May assist in determining cell or tissue type the lesion is derived from
less accurate with very large or poorly defined lesions
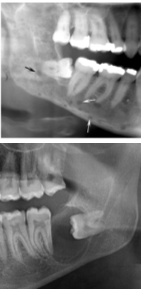
How is the epicenter relative to the inferior alveolar canal?
Within IAC → more likely neural or vascular
Above IAC → more likely odontogenic
Below IAC → more likely nonodontogenic
Epicenter in ramus, coronoid or condyle or within maxillary sinus more likely non-odontogenic
What can narrow interpretation?
The extent of the lesion, whether it is generalized or localized
Metabolic and endocrine processes tend to uniformly impact structures
Few lesions tend to be multi-focal which can narrow diagnosis
In order to know where the lesion is, what do you have to do?
Describe the lesion extent in multiple dimensions (ex. superior-inferior, medial-lateral) relative to other structures (ex. teeth)
Peri-coronal, peri-apical, inter-radicular
Certain lesions tend to be found in certain locations
Location alone should never be used as sole feature when formulating diagnosis
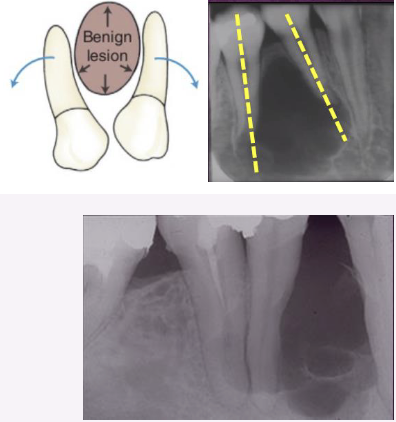
What are the types of periphery/borders? And what do they mean?
Well defined
If you can confidently (*mostly*) trace the border
Tends to be benign
Poorly defined
Difficult to exactly delineate or reproducibly draw
Tends to be malignant
Zone of transition
How quickly normal bone transitions to abnormal
Narrow vs. wide
What do you see in a well defined border?
Punched out – sharp, narrow zone of transition; non-corticated
Term tends to be strongly associated with multiple myeloma
Corticated – thin, radiopaque line of bone at lesion periphery
Associated with benign, slow-growing process
Sclerotic – wider, more diffuse zone of transition
Reflects ability of lesion to stimulate bone production (reactive bone formation)
Radiolucent periphery – rim of radiolucency representing soft tissue
Generally with outer corticated border and inner/internal radiopacity
Associated with benign, slow-growing lesion
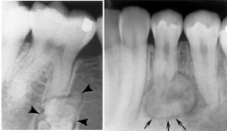
What do you see in a poorly defined border?
Blending – gradual, wide zone of transition
Focus on trabeculae rather than marrow spaces
Invasive – wide zone of transition with few or no trabeculae between lesion periphery and normal bone
Focus on enlarging radiolucency at expense of normal trabeculae
Also called permeative – lesion appears to grow through trabeculae producing finger-like extensions
Associated with rapid growth and aggressive and malignant lesions
Size can be measured depending on what?
imaging modality
Lesion may have a particular shape or be irregular
Circular or “hydraulic” shape (inflated or water-filled balloon) is characteristic of a cyst
Unilocular
Scalloping – series of contiguous arcs or semicircles that may develop around roots of teeth or in adjacent bone or cortices (sometimes see this called lobulated or loculated)
May reflect mechanism of lesion growth
Can be seen in cysts and benign neoplasms
What are three basic categories of internal structures?
Entirely radiolucent – normal bone resorbed
Entirely radiopaque – lesion filled with mineralized matrix
Mixed radiolucent and radiopaque (mixed density)
What do you need to look at for mixed radiolucency and radiopacity?
Examine shape, size, pattern, and density of the opaque/calcified material
Ex. enamel is more opaque than bone
In 2D imaging, can be challenging to determine whether the perceived radiopacity is located within the lesion itself or buccal or lingual to lesion
What are some things to look for in internal structures?
Abnormal trabecular patterns – variations in numbers, lengths, thickness and orientations of trabeculae
Internal septation –
Multilocular – compartments created by septations (striations of bone within lesion)
Can represent normal, trapped, residual bone
Can be manufactured/created by lesion
Appearance of septa (length, thickness, orientation) can indicate nature and pathogenesis of lesion
Dystrophic calcification – mineralization in damaged soft tissue (ex. chronically inflamed cysts)
Amorphous bone –dense often cortical-like bone but poorly organized
Tooth structure – enamel, dentin, pulp
What are effects on adjacent structures?
Used to infer biologic behavior of lesion
May aid in diagnosis
Understanding disease mechanisms that gives rise to changes is required
Teeth, lamina dura, and PDL space
Displacement of teeth –more commonly with benign, slower-
growing, space-occupying lesionsDirection of displacement can help identify lesion epicenter
Ex. Lesions with epicenter above crown will displace tooth apically
Tipping suggests slower growth
Bodily tooth displacement is more associated with a tumor over a cyst
Resorption of teeth usually occurs with slow-growing, benign processes
May result from chronic inflammation
Some malignant tumors can occasionally resorb teeth
What are some examples of biological behavior of lesions on adjacent structure?
Ex. periapical inflammatory disease can stimulate bone resorption (rarefaction) or formation (sclerosis)
Ex. space-occupying lesion (cyst, benign neoplasm or tumor) slowly creates its own space by displacing teeth and other adjacent structures
Ex. malignancy tends to be fast growing and destructive to bone, but usually leaves the teeth