Cardiology Examination - 2nd Year
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
36 Terms
How should you begin the examination?
WINDEC
Briefly describe the examination
The cardiology exam will involve inspecting your hands, face and chest, as well as listening to and feeling your chest for your heart beat.
After WINDEC, what is the first step of the cardiology exam?
Inspect the patient’s general condition and their surroundings.
During the general inspection of the patient and their surroundings, what should you look for?
Cyanosis
SOB
Pallor
Malar flush
Oedema
Medical equipment
Mobility aids
Pillows
Vital signs
Fluid balance
Prescriptions
After the first general inspection of the patient and their surroundings, what comes next?
Inspect the hands
When inspecting the hands, what should you look for?
Cyanosis
Pallor
Tar staining
Splinter haemorrhages
Osler nodes
Janeway lesions
ulceration?
Arachnodactyly
Finger clubbing (Schamroth’s window)
Janeway lesions
Small painless haemorrhages on the hands and feet that indicate endocarditis.

Splinter haemorrhages
A haemorrhage under the nail that resembles a splinter. They are usually caused by trauma, but they can indicate bacterial endocarditis.

Osler nodes
Painful red, raised lesions on the hands and feet that indicate bacterial endocarditis.

Xanthomata
A skin lesion caused by the accumulation of fat in macrophages of the skin.

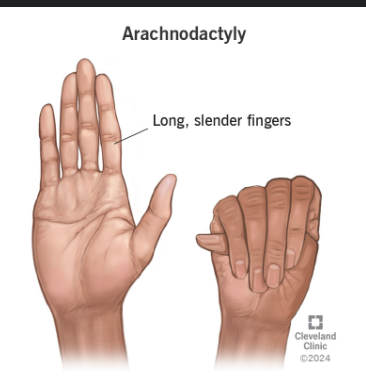
Arachnodactyly
Long slender fingers. This indicates the patient may have Marfan’s syndrome.
After inspecting the hands, what is the next step?
Check pulse and respiratory rate.
After taking the pulse, what is the next step?
Ask the patient to move their head 45 degrees to the left so you can measure the JVP.
How do you measure the JVP?
Position the patient in a semi-recumbent position at 45 degrees
As the patient to turn their head slightly to the left
Inspect for evidence of the IJV running in between the medial end of the clavicle and ear lobe - under the medial aspect of the sternocleidomastoid - it has a double waveform pulsation
Measure the JVP by assessing the vertical distance between the sternal angle and the top of the pulsation point of the IJV (just look at this stage)
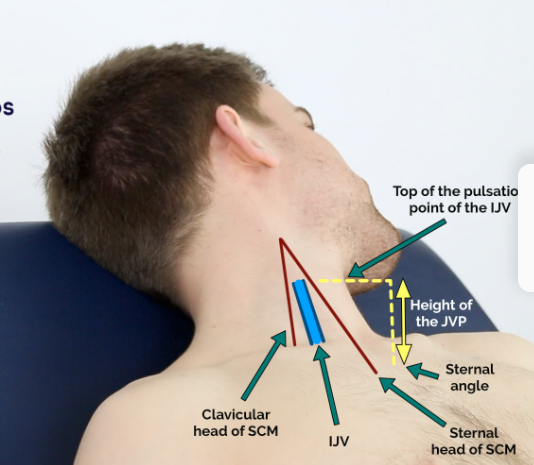
What is a healthy JVP?
No greater than 3 cm
What causes a raised JVP?
It indicates venous hypertension. Cardiac causes of this include:
Right sided HF (caused by left sided HF, or pulmonary hypertension due to COPD or interstitial lung disease)
Tricuspid regurgitation (caused by infective endocarditis and rheumatic heart disease)
Constrictive pericarditis (idiopathic, or caused by RA or TB)
After checking the JVP, what is the next step?
Inspect the eyes and the face.
When inspecting the eyes, what are you looking for?
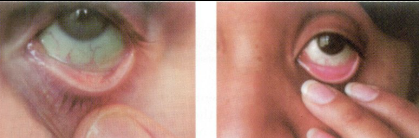
Conjunctival pallor
Corneal arceus
Xanthelasma
Kayser-Fleischer rings
Conjunctival pallor
Paleness of the mucous membrane that lines the eyelid (conjunctiva) that indicates anaemia.
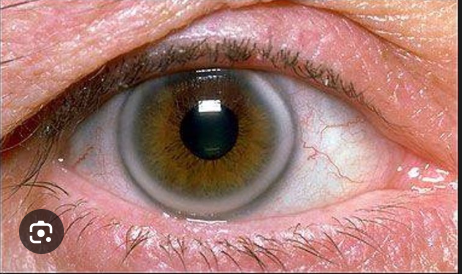
Corneal arcus
A white/gray arc/ring that lines the iris. It is caused by the deposition of lipids in the cornea. In patients under 40, it is associated with hypercholesterolaemia and an increased risk of coronary artery disease.
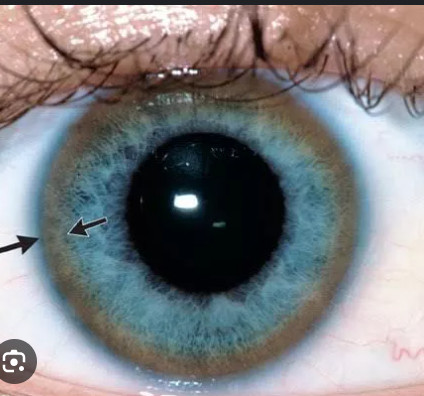
Kayser-Fleischer rings
Dark rings that encircle the iris associated with Wilson’s disease - disease that causes abnormal copper processing by the liver, resulting in deposition of copper in various places (including the heart which can cause cardiomyopathy).
When inspecting the mouth, what should you look for?
Central cyanosis
Dental hygiene (risk factor for infective endocarditis)
Angular stomatitis (inflammation in corners of mouth)
High arched palate (indicator of Marfan’s syndrome)
After checking the eyes and face, what is the next part of the exam?
Closely inspect the anterior chest - remember to ask the patient to lift up their arms.
When closely inspecting the anterior chest, what are you looking for?
Scars suggestive of a previous thoracic surgery
Pectus excavatum
Pectus carinatum
Visible pulsations
Before touching the patient, what should you do?
Ask them if they have any pain and signpost you are about to touch them.
What is the next step after close inspection of the anterior chest?
Palpation
What are you palpating the chest for?
Apex beat
Heaves
Thrills
(in this order)
How do you palpate the apex beat?
Place fingers firmly horizontally on the chest on the fifth intercostal space in the midclavicular line.

How to count intercostal spaces
Find the sternal angle on the patient - this is adjacent to the second intercostal space.
How do you palpate heaves?
Place the heel of your hand firmly parallel to the left sternal edge (fingers vertical)
A heave will lift the heel of the hand with each systole
How do you feel for thrills?
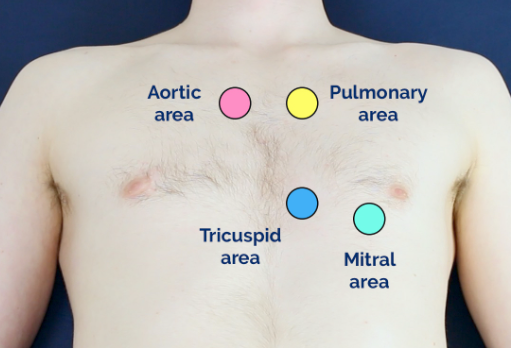
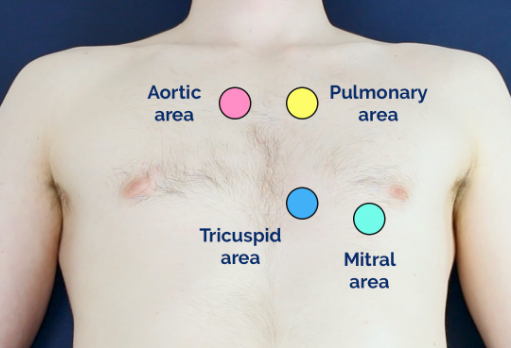
Place your hand horizontally across the chest wall with the flats of your fingers and palm over the valve. There are four valves to assess:
Mitral valve: 5th intercostal space in the midclavicular line
Tricuspid valve: 4th/5th intercostal space at the lower left sternal edge
Pulmonary valve: 2nd intercostal space at the lower left sternal edge
Aortic valve: 2nd intercostal space at the right sternal edge
After palpation, what is next?
Auscultation
How is auscultation performed during the cardiology exam?
Place the diaphragm of the stethoscope on the 4 valves you just palpated for thrills, using the carotid pulse to help with timing.
Place the diaphragm at the base of the neck on the carotid artery (each side) to check for bruits
Get the patient to sit up so you can listen to the base of each lung
After auscultation, what is the next step?
Check for oedema at the ankles - insect them, then press on their ankle with your finger.
After checking the patient’s ankles for oedema, what is the next step?
Finish up the examination - thank the patient for their time and wash your hands.
Things I always seem to forget
Carotid pulse timing
Listening to lung base
Check for ankle oedema