chapter 26: Respiratory function and disorders of system of children
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
106 Terms
how do changes take place in the lungs with age?
changes take place in the air passages that increase the respiratory surface
major changes are in the number and size of alveoli and in the increased branching of terminal bronchioles
when is respiratory fuction first evident during gestation?
approximately 20 weeks of gestation
describe the respiratory rate and volume during growth
RR: steadily decreases until it levels off at maturity
volume: air inhaled increases with the growth of the lungs and is closely related to body size
amount of oxygen: in the expired air gradually decreases and the amount of carbon dioxide increases
mechanical respiratory devices (artificial)
increase the pressure entering the air passages (positive pressure breathing devices) or lowers the pressure around the body (negative pressure ventilator)
vetilation
exchange of gases in the lung
results from changes in pressure gradients created by changes in the size of the thoracic cavity
contractions of the diaphram and external intercostal muscles
increases the size of the thorax and decreases the intrathoracic pressure
As a result, air moves from the atmosphere, which has a higher pressure, into the lungs, which have a lower pressure
surfactant
a lipoprotein at the air-fluid interface that allows alveolar expansion and prevents alveolar collapse, and elastic recoil, the tendency of the lungs to return to the resting state after inspiration (a passive process that requires no muscular effort)
compliance
normally high in the newborn and infant because of a more pliant (flexible) rib cage
primary forces that affect the mechanics of breathing
measure of chest wall and lung distensibility
It represents the relative ease with which the chest and lungs expand with increasing volume and then collapse away from the pleural wall with decreasing volume (elastic recoil)
The two major factors determining: alveolar surface tension, which is lowered by surfactant and elastic recoil, the tendency of the lungs to return to the resting state after inspiration
what is and what are causes of tachypnea?
rapid respirations
anxiety, excitement, elevated temperature, severe anemia, metabolic acidosis, respiratory alkalosis
what is and what are causes of hyperpnea
too deep respirations
fever, severe anemia, respiratory alkalosis associated with psychosis, central nervous system (CNS) disturbances, and respiratory acidosis that accompanies disorders such as diabetic ketoacidosis or diarrhea
what is and what are causes of hypopnea
too shallow respirations
metabolic alkalosis.
in preterm infants may occur as a result of pulmonary immaturity, absence of adequate substrate to support respiratory muscle activity, neurologic insult, and neurologic immaturity
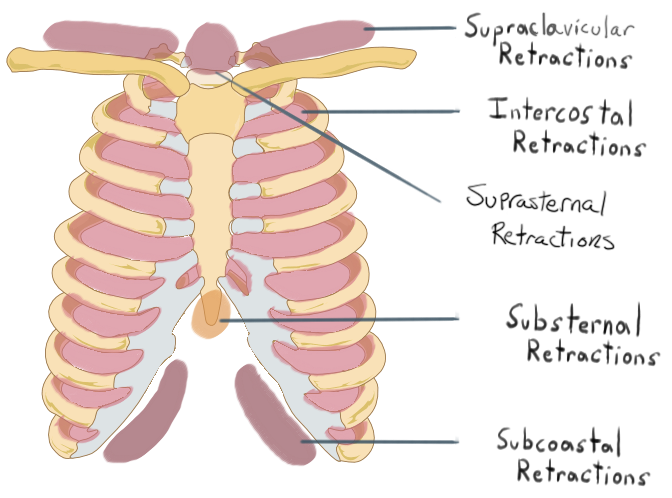
retractions
sinking in of soft tissues relative to the cartilaginous and bony thorax
types:
supraclavicular retractions
suprasternal notch retractions
intercostal retractions
substernal retractions
Subcostal retraction
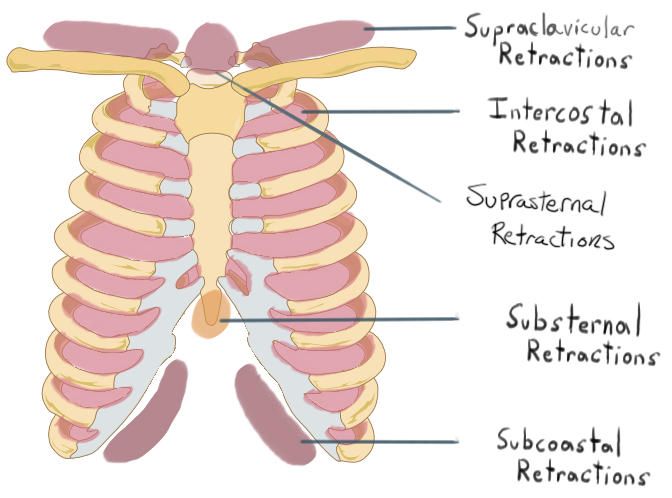
observed anteriorly at the lower costal margins, indicates a flattened diaphragm because it not only lowers the floor of the thorax but also pulls on the rib cage in response to a greater than normal decrease in intrathoracic pressure
Subcostal retraction
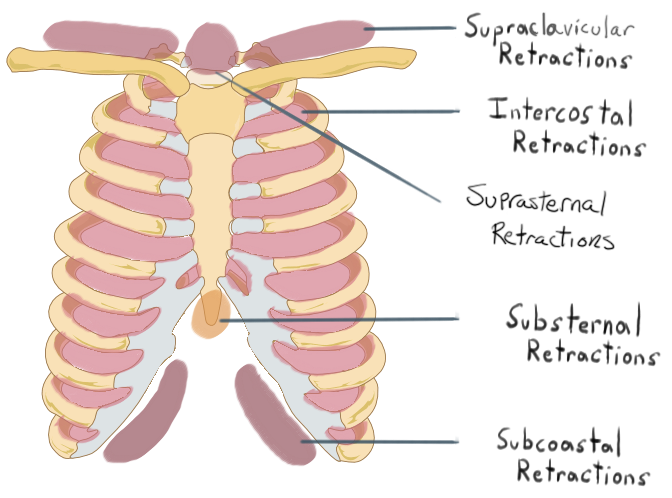
severe airway obstruction, retractions extend to the
supraclavicular areas and the suprasternal notch
nasal flaring
sign of respiratory distress
significant finding of respiratory compromise
enlargement of the nostrils helps reduce nasal resistance and maintains airway patency
may be intermittent or continuous and should be described as minimum or marked.
head bobbing
This is caused by neck flexion resulting from contraction of the scalene and sternocleidomastoid muscles.
seen in a sleeping or exhausted infant is a sign of dyspnea
The head, supported on the caregiver’s arm only at the suboccipital area, bobs forward with each inspiration
noisy breathing
“snoring” is frequently associated with hypertrophied adenoidal tissue, choanal obstruction, polyps, or a foreign body (FB) in the nasal passages.
stridor
high-pitched, noisy respiration, is an indication of narrowing of the upper airway
result of edema and inflammation
in association with an upper airway obstruction from mucus secretions or a foreign object.
may be inspiratory or expiratory
what are common cause of stridor in children?
croup, epiglottitis, FB, or tracheitis
grunting
sign of pain in older children and acute pneumonia or pleural involvement
observed in pulmonary edema (PE) and is a characteristic of respiratory distress in newborns and infants
It is the body’s attempt at more efficient respiration
serves to increase end-respiratory pressure and thus prolong the period of oxygen and carbon dioxide exchange across the alveolocapillary membrane
wheezing
continuous musical sound originating from vibrations in narrowed airways
heard on expiration
Infants may have it as a result of increased airway resistance and a compliant chest wall.
Older children often have it with a lower respiratory tract infection as a result of inflammation, bronchospasm, and accumulated secretions
Color changes of the skin
mottling, pallor, and cyanosis
mottling and cyanosis are significant and usually indicate cardiopulmonary disease
Except for the peripheral bluish discoloration (acrocyanosis) resulting from circulatory stasis in the newborn
mottling resulting from a cool environment
chest pain
complaint of older children
caused by both pulmonary and nonpulmonary
It may be caused by disease of any of the chest structures.
Most pleural pain is related to respiration. Rapid and shallow respiratory movements may be accompanied by grunting, especially in the younger patient
clubbing
proliferation of tissue about the terminal phalanges, accompanies a variety of conditions, frequently those associated with chronic hypoxia, primarily cardiac defects, and chronic pulmonary disease (cystic fibrosis [CF])
does not accurately reflect disease progression
degree depends on the extent to which the nail base is lifted on the dorsal surface of the phalanx by the tissue proliferation
greater the angle formed above the finger or toe at the skin-nail junction, the more pronounced the it is, especially when there is a decided curvature to the nail
cough
protective mechanism and an indicator of irritation
severe cough is associated with measles and CF
paroxysmal cough accompanied by an inspiratory “whoop” is typical of pertussis in infants and small children.
A brassy, nonproductive cough is part of the symptomatology of croup and FB aspiration.
Because there are no cough receptors in the alveoli, a cough may be absent in a child with pneumonia in the early stages of the disease but is a common feature during active pneumonia and recovery.
how is respiratory funtion diagnosed and assessed?
repsiratory funtion test
radiography
blood gas measure
pulse ox
pulmonary fuction Tests
pneumotachography or spirometry
noninvasive
radiography
frquesntly used
lead shields to protect correctly placed and consistently applied to areas not needed for diagnostic purposes, are essential.
Play and modification of methodology effectively reduce the trauma sometimes associated with the procedure and gain the child’s cooperation
blood gas
information regarding lung function, lung adequacy, and tissue perfusion and are essential for monitoring conditions involving hypoxemia, carbon dioxide retention, and pH
guides decisions regarding therapeutic interventions, such as adjusting mechanical ventilator settings, modifying chest physical therapy (CPT), administering oxygen/continuous positive airway pressure (CPAP)/bilevel positive airway pressure (BiPAP), or positioning the child for maximum ventilation
newborns can have slightly lower values and still be considered normal. For example, normal pH values for a newborn range from 7.26 to 7.29, the average PaO2 is 70 mm Hg, the average PaCO2 is 33 mm Hg, and the average bicarbonate is 20 mEq/L. ABG values also depend on the concentration of oxygen the child is breathing
what protects the respiratory tract from infections?
lymphoid tissues, mucous balnket, ciliary action, epiglottis, cough, position change, lymphatics, humoral defenses
what consists of the upper respiratory tract?
upper airway, consists of the oronasopharynx, pharynx, larynx, and upper part of the trachea
what consists of the lower respiratory tract
consists of the lower trachea, bronchi, bronchioles, and alveoli
what are the most common respiratory tract infectious agents?
viruses, particularly respiratory syncytial virus (RSV), rhinovirus, nonpolio enteroviruses (coxsackievirus A and B), parainfluenza virus, influenza virus, adenoviruses, and human metapneumovirus
Other agents involved in primary or secondary invasion include group A beta-hemolytic streptococci (GABHS), Bordetella pertussis, staphylococci, Haemophilus influenzae, Chlamydia trachomatis, Mycoplasma organisms, and pneumococc
when are infants at risk for infection? WHY?
infection rate increases from 3 to 6 months old
which is the period between the disappearance of maternal antibodies and the infant’s own antibody production
The viral infection rate continues to remain high during the toddler and preschool years
lowers around 5 years but the incidence of Mycoplasma pneumoniae and GABHS infections increases.
conditions that decrease resistance
malnutrition, anemia, and fatigue
Conditions that weaken defenses of the respiratory tract and predispose a child to infection
allergies (allergic rhinitis), BPD, asthma, history of RSV infection, cardiac anomalies that cause pulmonary congestion, and CF
Meningismus
Meningeal signs without infection of the meninges
Occurs with abrupt onset of fever
Accompanied by
Headache
Pain and stiffness in the back and neck
Presence of Kernig and Brudzinski signsSubsides as the temperature drops
Fever
May be absent in neonates (<28 days)Greatest at ages 6 months to 3 years
Temperature may reach 103° to 105 °F (39.5° to 40.5°C) even with mild infections
Often appears as first sign of infection
May leave child listless and irritable or somewhat euphoric and more active than normal, temporarily;
leads some children to talk with unaccustomed rapidity
Tendency to develop high temperatures with infection in certain families
May precipitate febrile seizures
Abdominal Pain
Common complaint
Sometimes indistinguishable from pain of appendicitis in older child
May be caused by mesenteric lymphadenitis
May represent referred pain (e.g., chest pain associated with pneumonia)
May be related to muscle spasms from vomiting, especially in nervous, tense children
Respiratory Sounds
Cough
Hoarseness
Grunting
Stridor
Wheezing
Findings on auscultation:
Wheezing
Crackles
Absence of air movement
Sore Throat
Frequent complaints of older children
Young children (unable to describe symptoms) may not complain even when highly inflamed
Increased drooling noted by parents
Refusal by child to take oral fluids or solids
what is in the assessment of a child with a RTI?
Respiratory effort (respiratory rate, rhythm and depth; accessory muscle use; retractions; nasal flaring)
Oxygenation (pulse oximetry, skin color)
Body temperature
Child’s activity level
Child’s level of comfort
how to treat or ease RTIs in children?
Warm or cool mist is a common therapeutic measure for symptomatic relief of respiratory discomfort
mist tents
steam vaporizers are discouraged
time-honored method: producing steam in the shower for 10-15 mins
promoting comfort:
Topical vapor rubs could be considered for children older than age 2 years
correct administration of nose drops or throat gargles
infant nasal aspirator or a rubber ear syringe is helpful in removing nasal secretions before feeding (Saline nose drops can be prepared at home by dissolving {1/2} to 1 tsp of salt in 1 cup of warm water)
satisfactory method of assessing output in nonhospitalized infants and toddlers who are not acutely ill
Counting the number of wet diapers in a 24-hour period
urinary output
should be approximately 0.5 to 1 mL/kg/hr in a child who weighs less than 30 kg (66 lb) and 30 mL/hr for children 30 kg and larger
what are Signs of clinical deterioration?
increasing respiratory distress, increasing respiratory rate, increasing heart rate, worsening hypoxia, poor perfusion, reduced level of consciousness, behavioral changes, and lethargy. Any deterioration is notified to the primary service.
what are causes of acute viral nasopharyngitis?
rhinoviruses
RSV
adenovirus
influenza virus
parainfluenza virus
what are manifestations of acute viral nasopharyngitis?
self-limiting
lasting 10-14 days (peak on day 2-3 days
Fever
decreased appetite
decreased fluid intake
decreased activity
nasal inflammation/open mouth breathing
vomiting
diarrhea
older children
dryness and irritation of nasal passages and the pharynx
chilling sensations,
muscular aches, an
irritating nasal discharge
occasional coughing or sneezing
what is the therapeutic management of acute viral nasopharyngitis?
managed at home
antipyretics (tylenol)
fluid and rest
Products containing dextromethorphan or codeine may be prescribed for a dry, hacking cough, especially at night
true or false
A cold is often the parents’ first introduction to an illness in their infants
true
what is the Nursing management of acute viral nasopharyngitis?
elevating the head of the bed or crib to assist with secretions
suctioning
vaporizing
saline nose drops
gentle suction with bulb syringe (before feeding)
maintain fluid intake (popcicles, gelatin, broths, soups)
avoid contact with affected persons
handwashing and cough into elbow
hand sanitizer use
what is the family support for acute viral nasopharyngitis?
reassure because URIs are so frequent in children younger than 3 years of age
families may feel they are on an endless roller coaster of illness
Reassure them that frequent colds are a normal part of childhood, there are hundreds of viruses that cause them, and that by 5 years of age most children will have developed immunity to many viruses
what is Early Evidence of Respiratory Complications that Parents are instructed to notify the health professional if they note any?
Evidence of earache
Respirations faster than 50 to 60 beats/min
Fever over 101 °F (38.3°C)
Listlessness
Increasing irritability with or without fever
Persistent cough for 2 days or more
Wheezing
Crying
Refusal to eat
Restlessness and poor sleep patterns
what is Acute Streptococcal Pharyngitis and what can it cause?
GABHS infection of the upper airway (strep throat) is not in itself a serious disease,
affected children are at risk for serious sequelae: acute rheumatic fever, which is an inflammatory disease of the heart, joints, and CNS, and acute glomerulonephritis
skin manifestations, including impetigo and pyoderma
scarlet fever
may also occur because of a strain of group A streptococcus.
The clinical manifestations of scarlet fever include pharyngitis and a characteristic erythematous sandpaper-like rash
otherwise scarlet fever shares the same clinical manifestations as those mentioned for GABHS, and treatment and sequelae are the same.
Severe case is rarely seen in the United State
what are clinical manifestations of Acute Streptococcal Pharyngitis?
no symptoms
abrupt
characterized by pharyngotonsillitis
headache
fever
abdominal pain
The tonsils and pharynx may be inflamed and covered with exudate
petechiae on palete
strawberry tongue
Anterior cervical lymphadenopathy
Anterior cervical lymphadenopathy
resolves for 3-5 days
mild-severe pain
tender nodes
difficulty swallowing
what is the therapeutic management of Acute Streptococcal Pharyngitis?
oral penicillin or other related medications such as ampicillin or amoxicillin is prescribed for 10 days
Intramuscular (IM) penicillin G benzathine
oral macrolide (erythromycin, azithromycin, clarithromycin) or a cephalosporin (cephalexin) is indicated for children who are allergic to penicillin
nursing care of Acute Streptococcal Pharyngitis?
obtain throat swab
instructs the parents about administering the antibiotic and analgesics as prescribed
Cold or warm compresses to the neck
old enough to cooperate, warm saline gargles offer some relief of throat discomfort.
Pain may interfere with oral intake, and the child should not be forced to eat
encourage cool liquids or ice chips, which are usually more acceptable than solids
Never administer penicillin G procaine or penicillin G benzathine suspensions intravenously; they may cause embolism or toxic reaction with ensuing death in minutes. Instead, administer these medications deep into the muscle tissue to decrease localized reactions and pain
how to prevent the spread of Acute Streptococcal Pharyngitis?
Children with streptococcal infection are noninfectious to others 24 hours after initiation of antibiotic therapy.
It is generally recommended that children not return to school or daycare until they have been taking antibiotics for a full 24-hour period.
replace toothbrush
what is tonsillitis?
inflammation of the tonsils
Because of the abundant lymphoid tissue and the frequency of URIs
sore throat
temperature greater than 100.9 °F (38.3°C)
cervical adenopathy (>2 cm or tender nodes)
exudate on the tonsils
positive culture for GABHS
what are clincal manifestations of tonsilitis?
caused by inflammation
self-limiting
palatine tonsils enlarge from edema, they may meet in the midline (kissing tonsils), obstructing the passage of air or food
difficulty swallowing or breathing
mouth breathing is continuous, the mucous membranes of the oropharynx become dry and irritated
odor/bad breath
impaired smell/taste
voice has a nasal and muffled quality
persistent cough
otitis media or difficulty hearing
what is the therapeutic management of tonsilitis?
treatment of viral is symptomatic
throat culture positive for GABHS infection requires antibiotic treatment
tonsillectomy (removal of palatine tonsils) for massive hypertrophy
adenoidectomy(removal of adenoids)
what is indicated for a tonsillectomy?
more than one peritonsillar abscess
PFAPA (periodic fever, aphthous stomatitis, pharyngitis, and adenitis syndrome)
airway obstruction
chronic tonsillitis unresponsive to antimicrobials
multiple antibiotic allergies
tonsils requiring tissue pathologic study
consideration:
at least seven episodes of tonsillitis in the previous year, or at least five tonsillitis episodes in each of the previous 2 years, or at least three episodes of tonsillitis in each of the previous 3 years
why would a adenoidectomy be recommended?
treatment of chronic nasal or sinus infections, recurrent OM, nasal obstruction, and sleep disturbance or suspected sleep-disordered breathing.
what is the nursing care of tonsilitis?
comfort and minimizing activities or
interventions that precipitate bleeding postoperatively
soft to liquid diet is generally
Warm saltwater gargles, warm fluids, throat lozenges
analgesic-antipyretic (acetaminophen and nonsteroidal antiinflammatory and ibuprofen) are useful to promote comfort
Ice collar
NPO until they can swallow it
Straws should be avoided because they may damage the surgical site and cause subsequent bleeding.
most obvious early sign of bleeding after a tonsilectomy
child’s continuous swallowing of the trickling blood
While the child is sleeping, note the frequency of swallowing
signs of hemorrhage are tachycardia, pallor, frequent clearing of the throat or swallowing by a younger child and vomiting of bright red blood. Restlessness, an indication of hemorrhage, may be difficult to differentiate from general discomfort after surgery. Decreasing blood pressure is a much later sign of shock
what is Infectious mononucleosis?
self-limiting
infectious disease that is common among young people under 25 years old
Epstein-Barr virus is the principal cause
transmitted through direct contact with oral secretions, blood transfusion, transplantation
diagnosis: nonspecific heterophil antibody tests (Monospot or Paul-Bunnell) and spot test (Monospot)
what are clinical manifestations of Infectious mononucleosis?
appears 10 days - 6 weeks after exposure
malaise
sore throat
fever with generalized lymphadenopathy and splenomegaly
exudative pharyngitis with or without petechiae
an increase in atypical lymphocytosis
what is the therapeutic management for Infectious mononucleosis?
symptom treatment
rest for fatigue
mild analgesic for headache, fever, malaise
corticosteroids decreases airway obstruction
Gargles, warm drinks, analgesic or anesthetic troches, or analgesics, including opioids, can relieve a sore throat
nursing care management of Infectious mononucleosis?
comfort measures
airway management
pain meds
what is influenza?
the flu
A, B, C
droplet spread: talking, sneezing, coughing
1- to 4-day incubation period (average of 2 days), and affected persons are most infectious for 24 hours before and 3 to 7 days after the onset of symptoms
what are clinical manifestations of the flu?
dry cough and a tendency toward hoarseness
A sudden onset of fever and chills is accompanied by flushed face
photophobia
myalgia
sore throat
headaches
malaise
hyperesthesia
sometimes prostration
what is the therapeutic treatment and prevention of the flu?
acetaminophen or ibuprofen for fever and sufficient fluids to maintain hydration.
Children should not receive aspirin because of its possible link with Reye syndrome
for patients at high risk of complication:
Oral oseltamivir (ages 2 weeks and older),
inhaled zanamivir (for ages 7 and older),
IV peramivir (for all ages)
oral baloxavir (for ages 5 and older)
prevent: vaccine at 6 months and older annually
what is the nursing care management for the flu?
same as URI
educate parents on prevention and antiviral meds
what is Otitis Media(OM)? Acute otitis media (AOM)? otitic media with effusion?
(OM): An inflammation of the middle ear without reference to etiology or pathogenesis
(AOM): An inflammation of the middle ear space with a rapid onset of the signs and symptoms of acute infection—namely, fever and otalgia (ear pain) in 24 mo
(OME): Fluid in the middle ear space without symptoms of acute infection
what is the most prevelent illnesses of ealry childhood?
Otitis media
what causes otitis media?
AOM is frequently caused by S. pneumoniae, H. influenzae, and Moraxella catarrhalis. The two viruses most likely to precipitate OM are RSV and influenza, although the adenoviruses, human metapneumoviruses, and picornaviruses (rhinovirus and enterovirus) also cause a significant number of URIs and OM
what children are at risk for Otitis media?
Children living in households with many members are more likely to have OM than those living with fewer persons.
Passive smoking increases the risk of persistent middle ear effusion by enhancing attachment of the pathogens that cause otitis to the respiratory epithelium in the middle ear space, prolonging the inflammatory response and impeding drainage through the eustachian tube
eustachian tubes are short, wide, and straight and lie in a relatively horizontal plane
The cartilage lining is undeveloped, making the tubes more distensible and therefore more likely to open inappropriately
The normally abundant pharyngeal lymphoid tissue readily obstructs the eustachian tube openings in the nasopharynx.
Immature humoral defense mechanisms increase the risk of infection.• The usual lying-down position of infants favors the pooling of fluid, such as formula or exudate, in the pharyngeal cavity
what are complications of ear infections?
hearing loss
tympatic membrane structural retractions
Tympanosclerosis (eardrum scarring)
Adhesive OM (glue ear)
Cholesteatoma
what are clinical manifestations of ear infections?
fluid accumulates
pain from pressure
Infants become irritable and can indicate their discomfort by holding or pulling at their ears and rolling their head from side to side
fever of 104
postauricular and cervical lymph glands may be enlarged
Rhinorrhea
vomiting
diarrhea
signs of concurrent respiratory tract or pharyngeal infection
loss of appetite
children with OME: exudate accumulates and pressure increases, with the potential for tympanic membrane rupture
feeling of “fullness” in the ear, a popping sensation during swallowing, and a feeling of “motion” in the ear if air is present above the level of fluid.
chronic serous OM is the most frequent cause of conductive hearing loss in young children, audiometry may reveal deficient hearing.
what is the therapeutic management of Acute Otitis Media (AOM)
Delayed antibiotic prescriptions are recommended by the American Academy of Pediatrics for patients 6 months and older with mild to moderate unilateral OM. The caregiver is provided a prescription to only fill if symptoms do not improve in 2 to 3 day:
Children younger than 6 months of age
Children 6 months of age and older with ear drainage, fever higher than 39°F, ear pain for at least 48 hours, moderate/severe ear pain
Bilateral AOM in a child between 6 and 23 months of age
When antibiotics are necessary, oral amoxicillin in high doses (80 to 90 mg/kg/day, divided twice daily) is recommended for 5 to 7 days with children 2 years and older, and 10 days with younger children
what is the therapeutic management of: recurrent otitis media?
tympanostomy tube placement
what is the therapeutic management of: otitis media with Effusion?
residual effusion include observation, antibiotics alone, or a combination of antibiotic and corticosteroid therapy.
how to prevent ear infections?
Routine immunization with the pneumococcal vaccine
breastfeeding infants for at least the first 6 months of life
avoiding propping the formula bottle
decreasing or discontinuing pacifier use after 6 months
maintaining up to date vaccination
preventing exposure to tobacco smoke
Acute Otitis Externa (AOE)
Swimmers ear
commonly caused by Pseudomonas aeruginosa, Staphylococcus epidermidis, or Staphylococcus aureus but may include other pathogens such as Aspergillus and Candida spp
Inflammation occurs when this environment is altered by swimming, bathing, or increased environmental humidity; by infection, allergic contact dermatitis, dermatoses, or insufficient cerumen; or by trauma from a FB or device in the ear (e.g., hearing aids, earphones) or a by a finger. The ear canal becomes irritated, and maceration takes place.
It is most common in 5 to 14 year olds
peaks in summer
what is the Nursing care management of ear infections (AOM&OME)?
relieve pain and fever (Ibuprofen, heat, position)
If the ear is draining, the external canal may be cleaned with sterile cotton swabs coupled with topical antibiotic treatment
Antibiotics if indicated
Myringotomy with tubes
Adenoidectomy
Hearing screening
Eliminate tobacco smoke
Feed infants in upright position
In an older child (usually older than 3 years of age), to keep the ear dry, pull the auricle up and out to straighten the canal
croup syndromes (what is it, causes, types)
definition
symptom complex of acute respiratory manifestations: a barking cough, hoarseness, inspiratory stridor, and respiratory distress from edema in the laryngeal area
causes:
H. influenzae type B, most cases of croup in the United States are attributed to viruses: parainfluenza viruses, and to a lesser degree, influenza types A and B, adenovirus, RSV, and measles, and M. pneumoniae
more common in boys than girls
6 months-3 years old and rare after 6 years
types: LTB and Epiglottitis
why are acute infections of the larnyx of greater importance in infants and smaller children than older children?
increased incidence in children in this age-group and the smaller diameter of the airway which renders it subject to significantly greater narrowing with the same degree of inflammation
treatment of croup
Airway protection, possible intubation, tracheotomy
Humidified oxygen
Fluids
Antibiotics
Reassurance
Corticosteroids
Fluids
Nebulized epinephrine (possible short-term improvement)
Heliox: moderate-to-severe croup
Cool mist
key differences between LTB and epiglottitis
absence of cough, the presence of dysphagia, and the high degree of toxicity in children with epiglottitis.
Children with epiglottitis usually look worse than they sound, in contrast to children with LTB, who sound worse than they look
acute epiglottitis
medical emergency
serious obstructive inflammatory process between 2-5 years
cause:
H. influenzae type b.
noninfectious: ingestion of caustic agents, smoke inhalation, smoking drugs (e.g., crack cocaine), or by FBs
LTB and epiglottitis do not occur together.
Males are affected more than females.
A lack of adequate vaccination against H. influenzae type b increases the risk
what are clinical manifestations of acute epiglottitis
onset abrupt,
less old symptoms; more sore throat
rapidly progress to severe respiratory distress
goes to bed asymptomatic to awaken later complaining of sore throat and pain on swallowing
fever
appears sicker than clinical findings
The child insists on sitting upright and leaning forward (tripod position), with the chin thrust out, mouth open, and tongue protruding.
Drooling of saliva is common because of the difficulty or pain on swallowing and excessive secretions
Suprasternal and substernal retractions
throat is red and inflamed, and a distinctive, large, cherry red, edematous epiglottis
absence of spontaneous cough, presence of drooling, and agitation
slides from class: High fever; muffled voice, sore throat, difficulty
swallowing; excessive drooling refusal of food & fluids, sitting-up
with neck extended (sniffing position); breathing thru mouth
how can epiglottistis be prevented?
H. influenzae type B conjugate vaccine beginning at 2 months old
Laryngotracheobronchitis (LTB)
most common croup
6 mo - 3years
causes: parainfluenza virus types 1, followed by parainfluenza virus types 2 and 3, adenoviruses, RSV, and M. pneumoniae. Less common causative organisms include influenza A and B, rhinoviruses, human coronaviruses, measles, metapneumoviruses, enteroviruses, herpes simplex virus, S. aureus, Streptococcus pyogenes, and S. pneumoniae
manifestations: inspiratory stridor; tachypnea; tachycardia; restlessness; cyanosis; substernal or intercostal retractions; barky cough; low-grade fever; previous URI; Respiratory acidosis,
what are Early signs of impending airway obstruction?
include increased pulse and respiratory rate; substernal, suprasternal, and intercostal retractions; nasal flaring; and increased restlessness.
bronchitis
Lower airway infection of first 4 years
inflammation of the trachea and bronchi; usually associated with a URI
causes:
viral: influenza A and B, parainfluenza, coronavirus (types 1 to 3), rhinovirus, RSV, and human metapneumovirus.
The bacteria: pertussis, M. pneumoniae, and Chlamydia pneumoniae
Persistent dry, hacking cough (worse at night), becoming productive in 2-3 days
treat:
analgesics, antipyretics, and humidity
Brinchiolotis
caused by RSV
spring and winter
Respiratory Syncytial Virus (RSV)
spread through direct contact
secretions can survive for several hours on countertops, gloves, paper tissues, and cloth, and for 30 minutes on skin; it remains infectious when transferred from hands or objects
manifestations:
initial: Rhinorrhea, Pharyngitis, Coughing, sneezing, Wheezing, Possible ear or eye infection
Intermittent: fever With Progression of Illness, Increased coughing and wheezing, Fever, Tachypnea and retractions, Refusal to nurse or bottle feed, Copious secretions
Severe Illness: Tachypnea >70 breaths/min, Listlessness, Apneic spells, Poor air exchange; poor breath sounds, Cyanosis
peaks 3 - 5days
management:
Immunize with Palivizumabid (synagis) for high risk infants q 30 days ( November to March)
symptomatically with oxygen, fluids, rest
most frequent cause of hospitalization in children younger than 2 years old
RSV infection