Lecture #1: Shoulder and Axilla
1/123
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
124 Terms
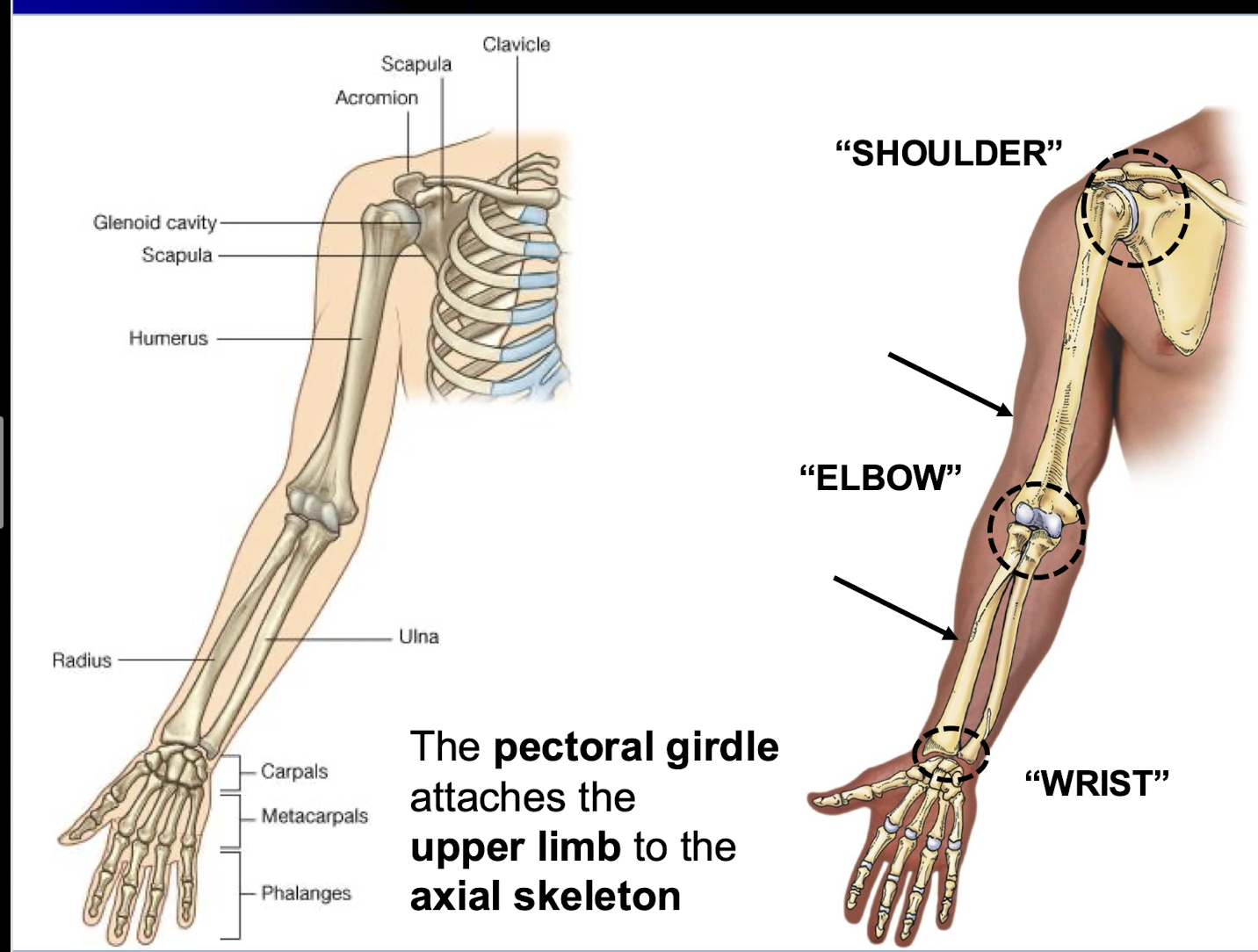
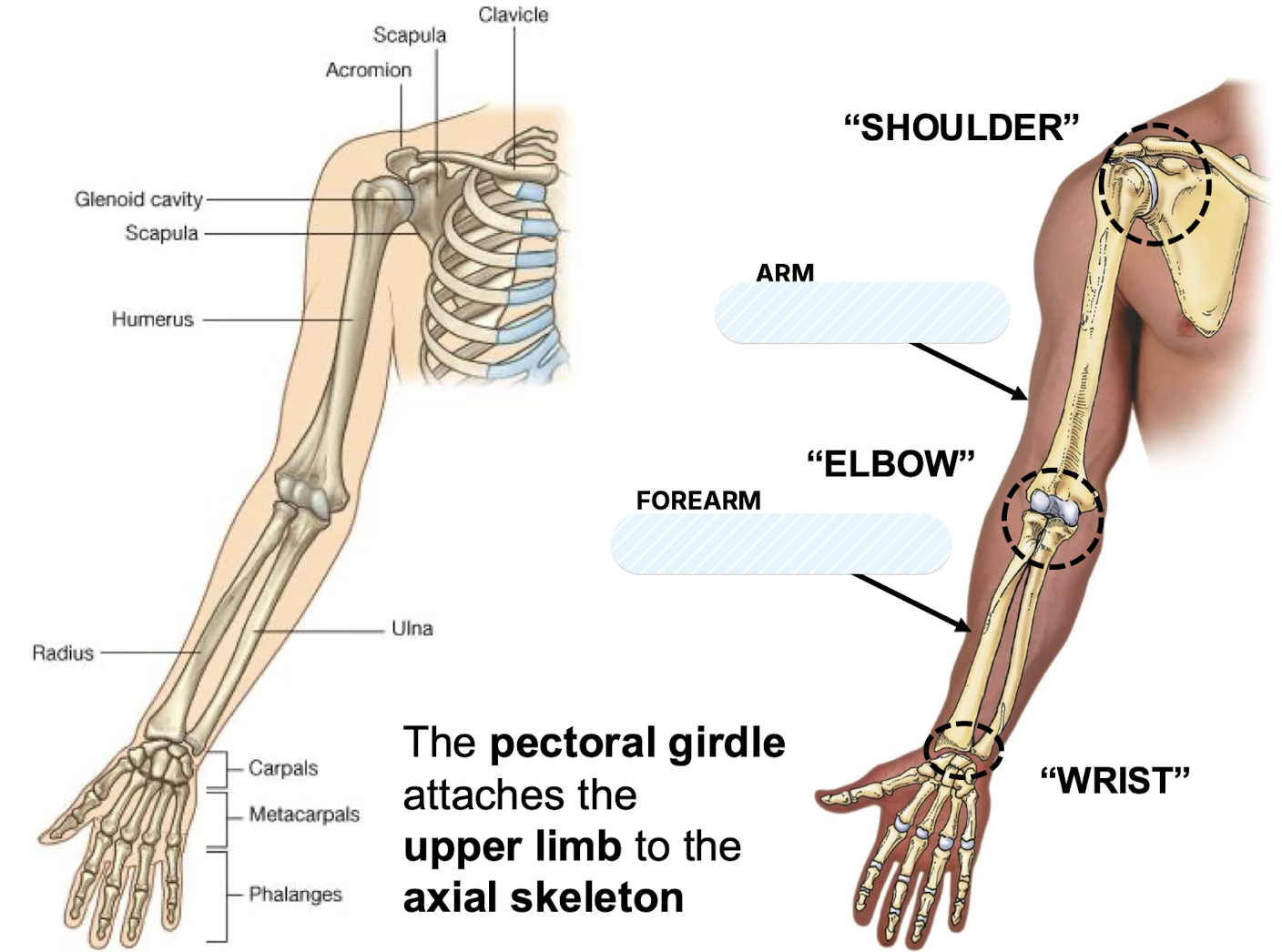
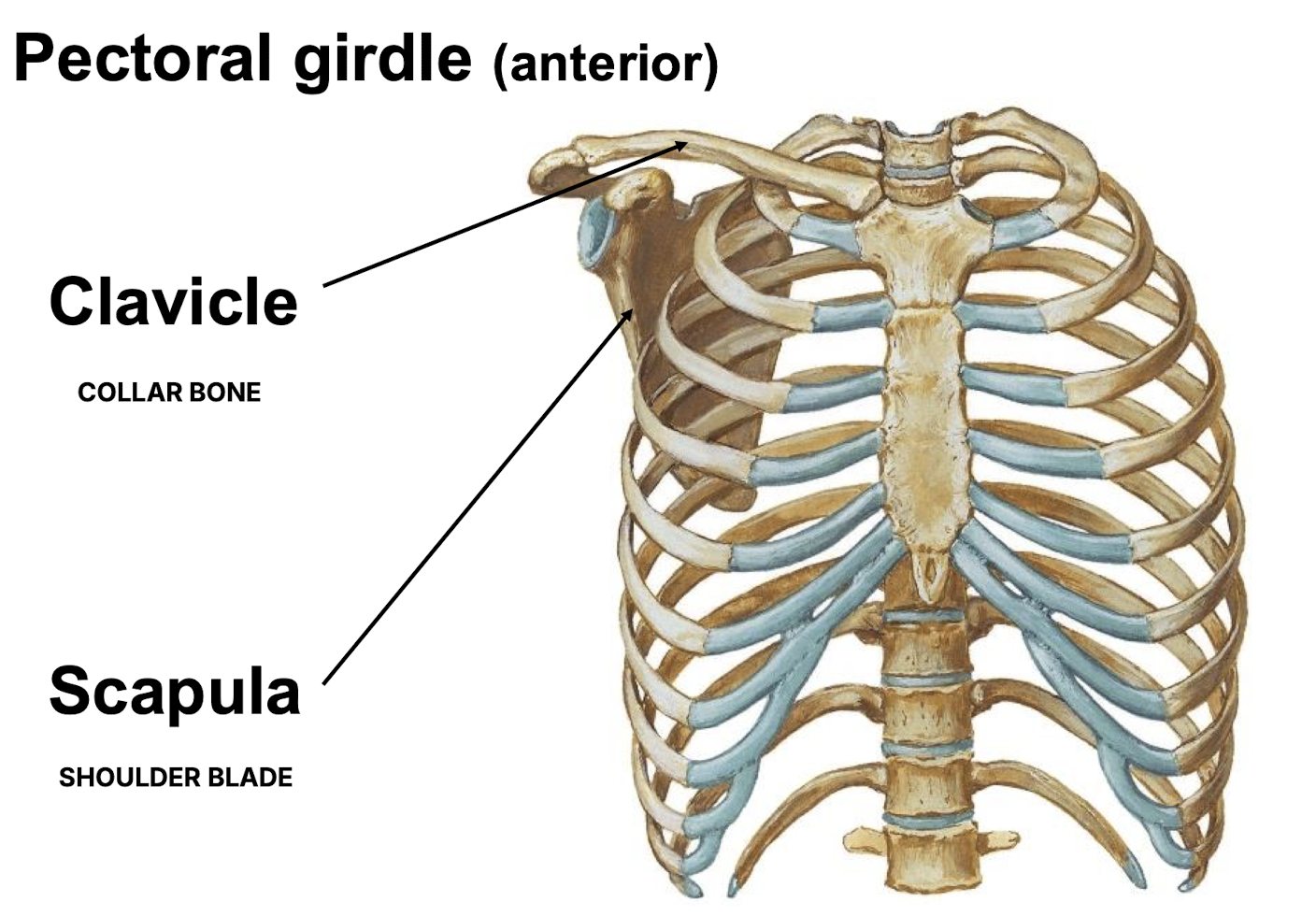
What structure attaches the upper limb to the axial skeleton?
The pectoral girdle.
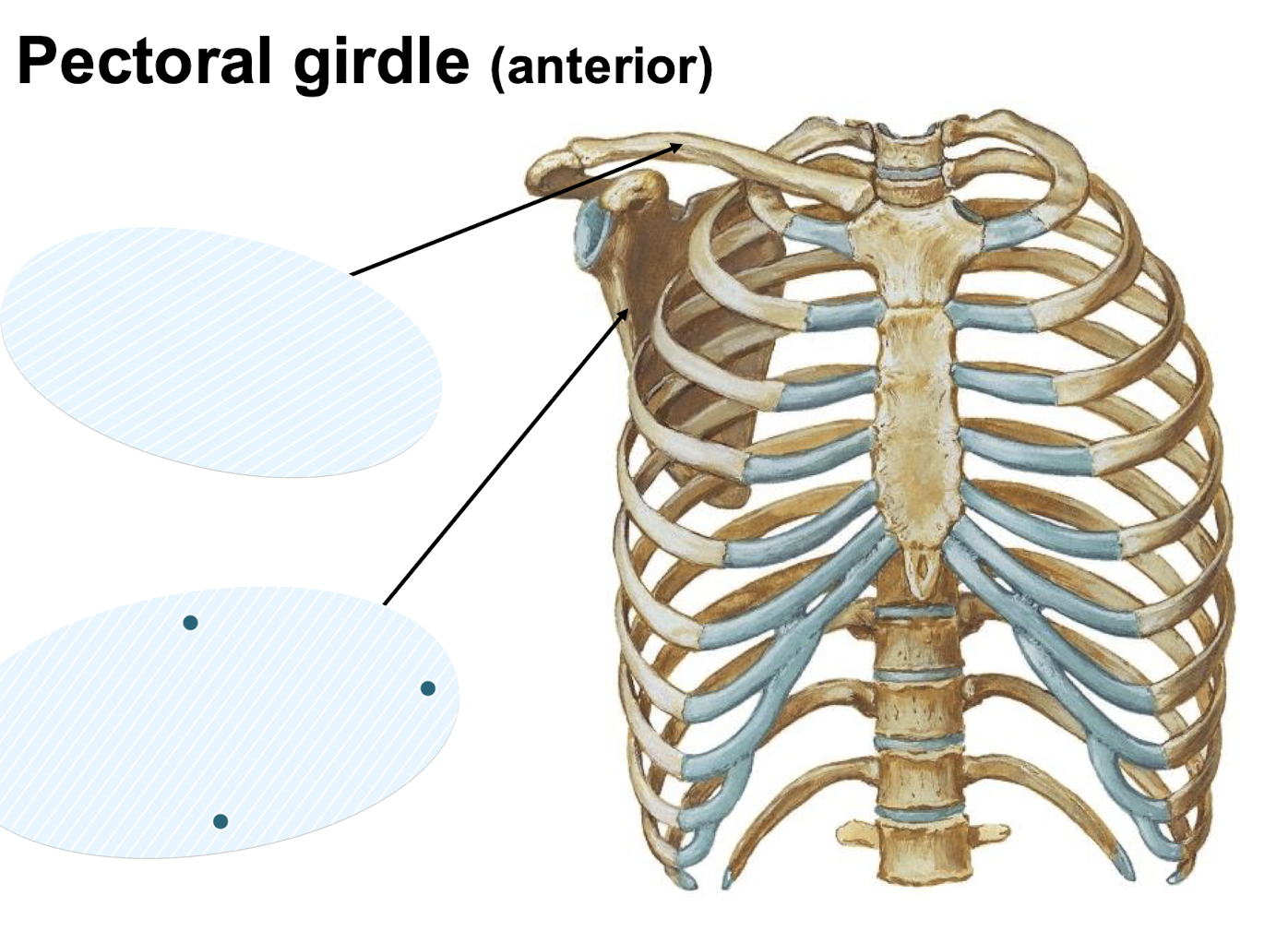
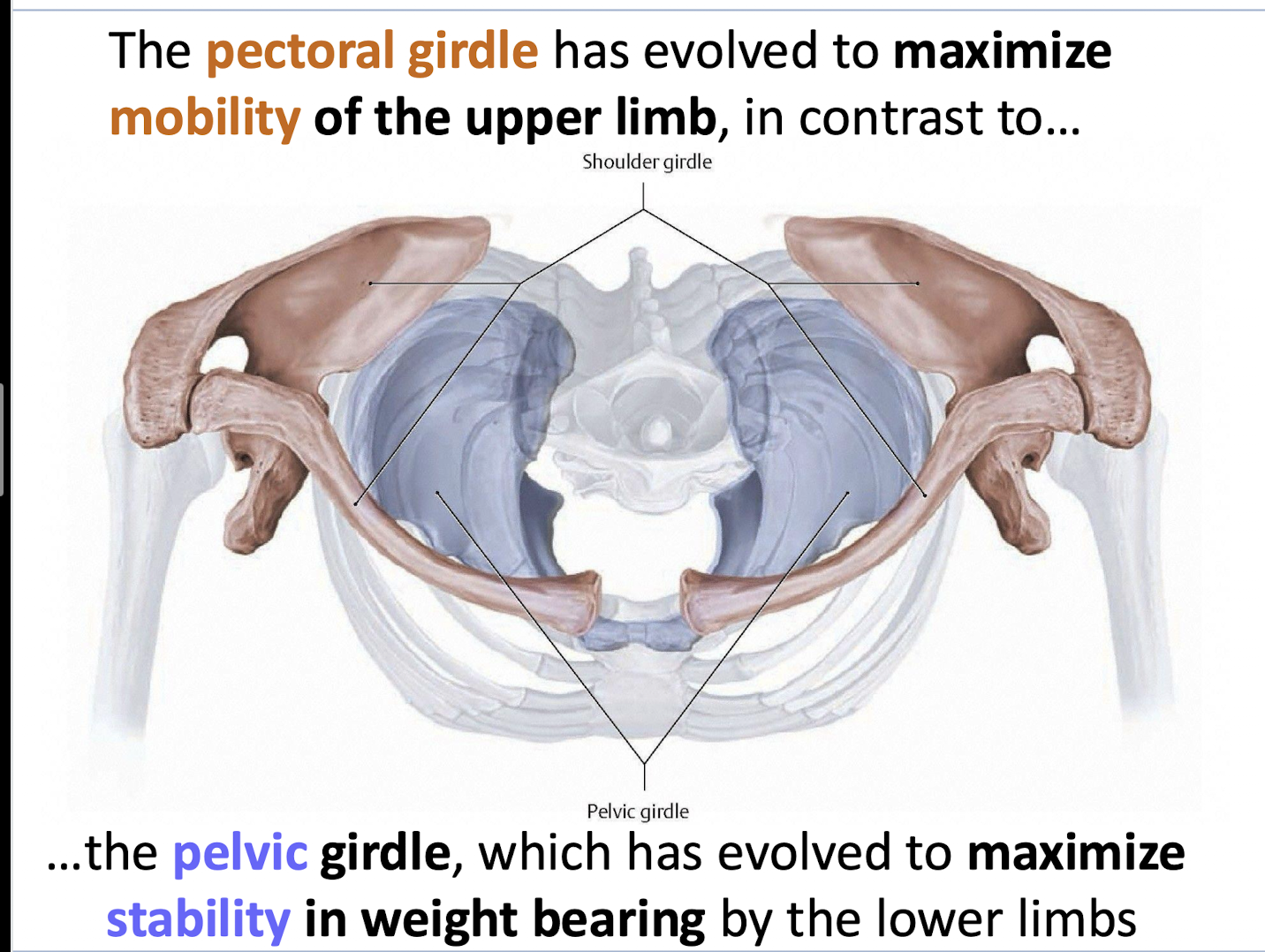
In contrast to the pelvic girdle evolved for stability, for what purpose has the pectoral girdle evolved?
To maximise mobility of the upper limb.
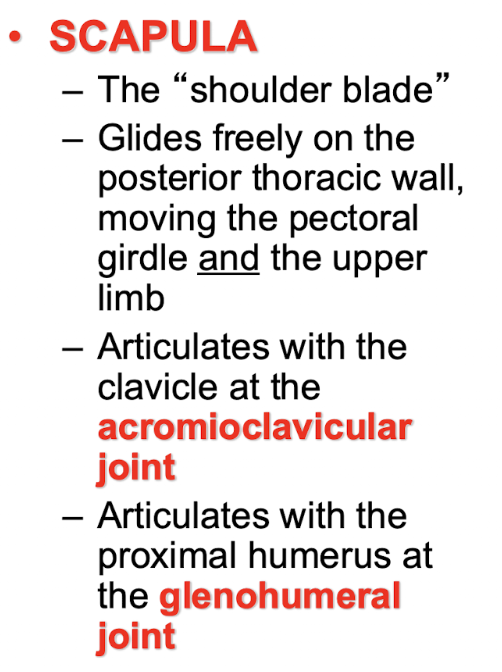
What bone articulates with the clavicle at the acromioclavicular joint?
The scapula
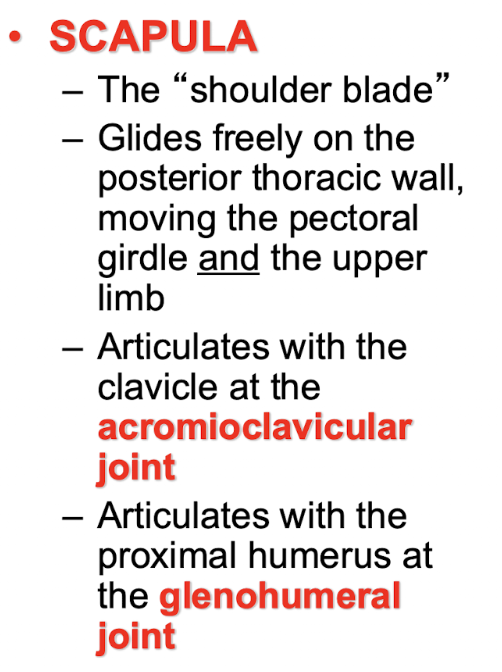
What bone articulates with the proximal humerus at the glenohumeral joint?
The scapula
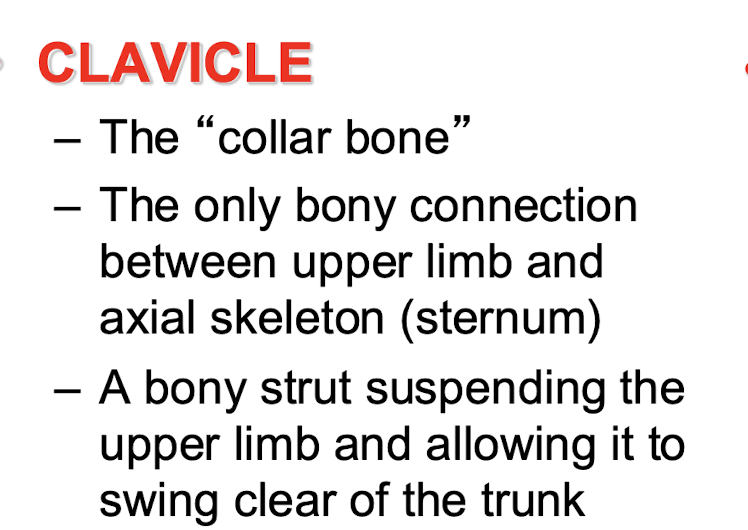
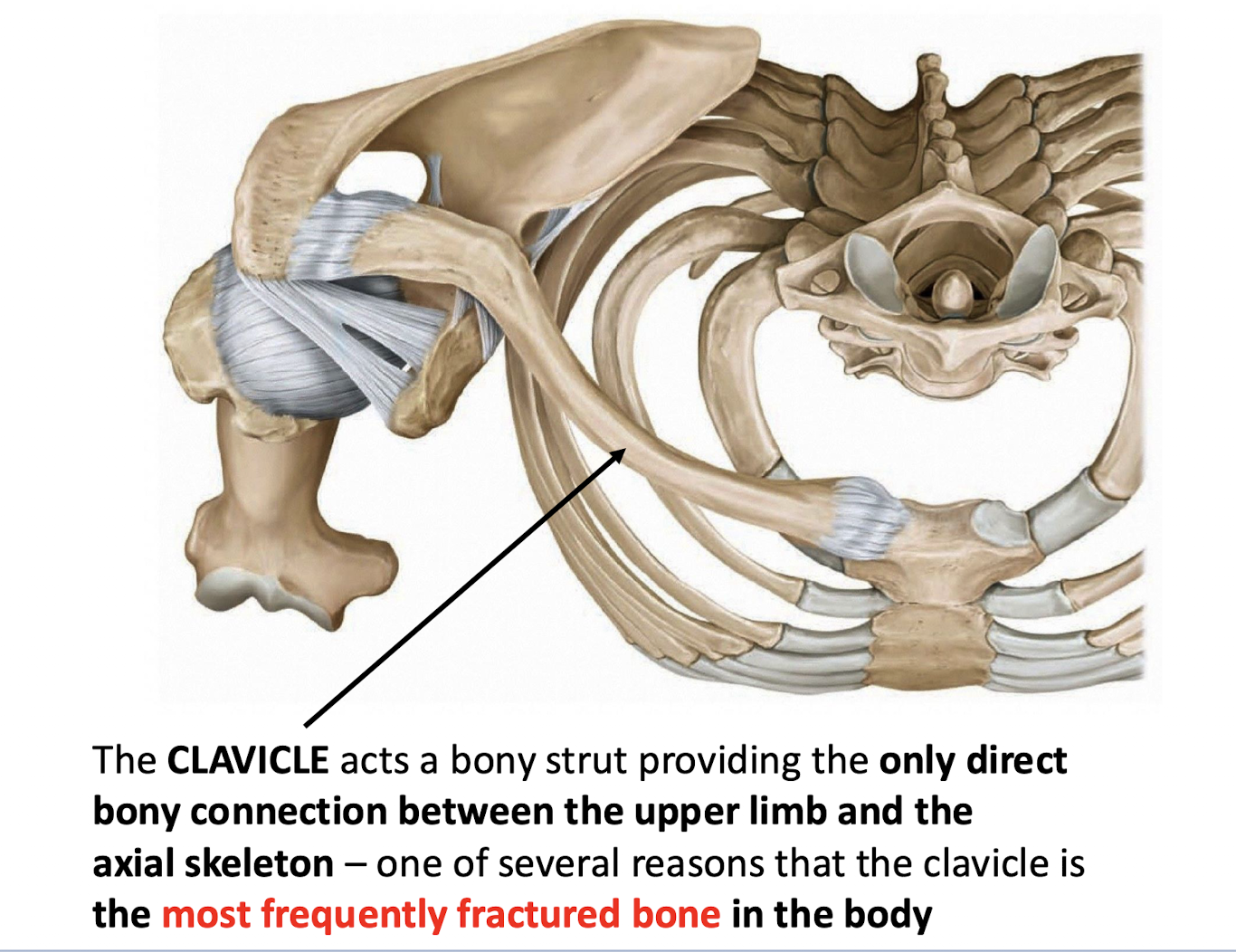
Which bone provides the only direct bony connection between the upper limb and the axial skeleton?
The clavicle, which articulates medially with the sternum (manubrium).
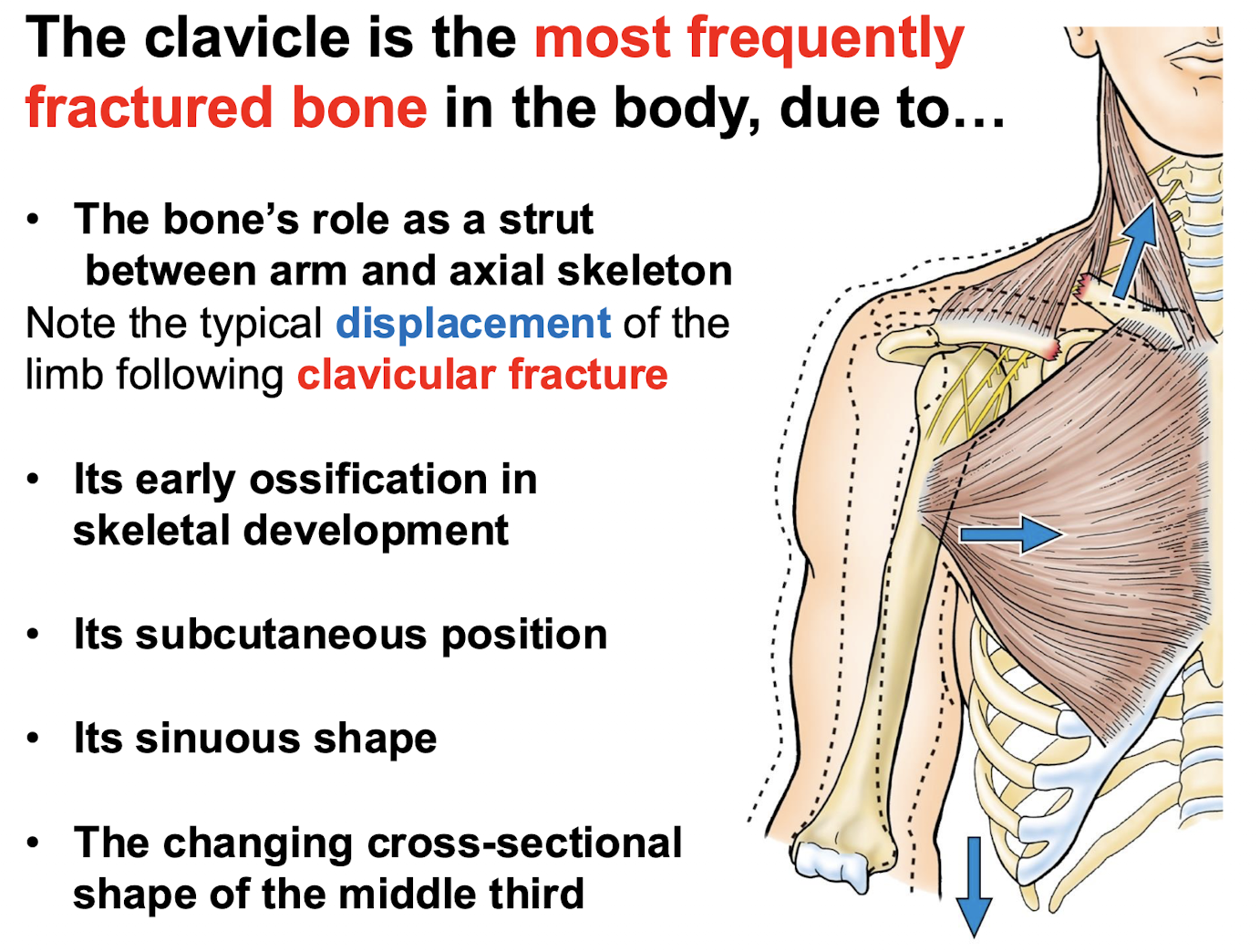
Besides acting as a connection, what is the functional role of the clavicle?
It acts as a bony strut suspending the upper limb to allow it to swing clear of the trunk.
Which bone is the earliest postcranial bone to initiate ossification during skeletal development?
The clavicle.
By what process does the clavicle develop early in skeletal development?
Intramembranous ossification.
What are the anatomical shapes and articulations of the medial and lateral ends of the clavicle?
The medial (sternal) end is rounded and articulates with the manubrium; the lateral (acromial) end is broad and flat and articulates with the scapula
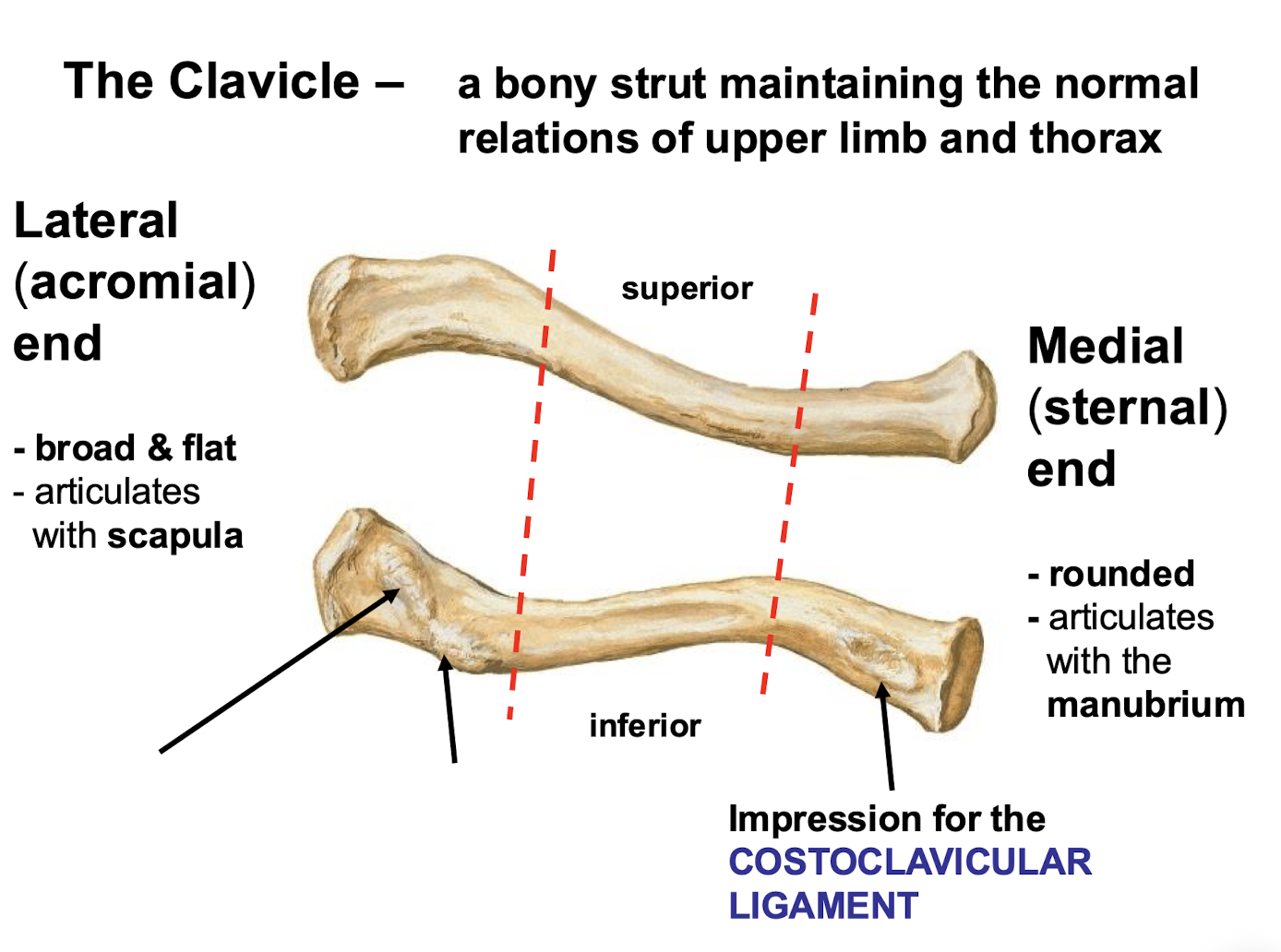
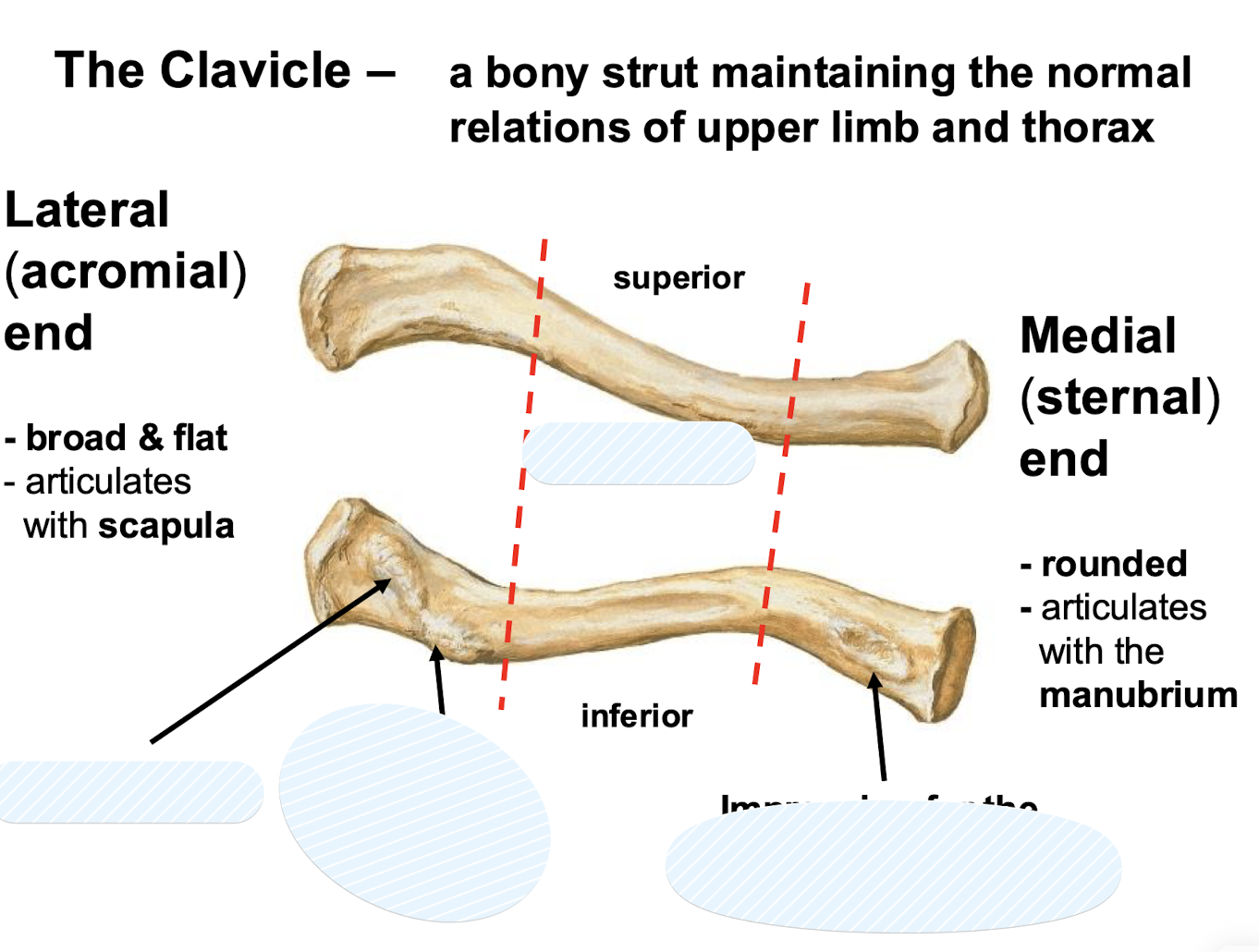
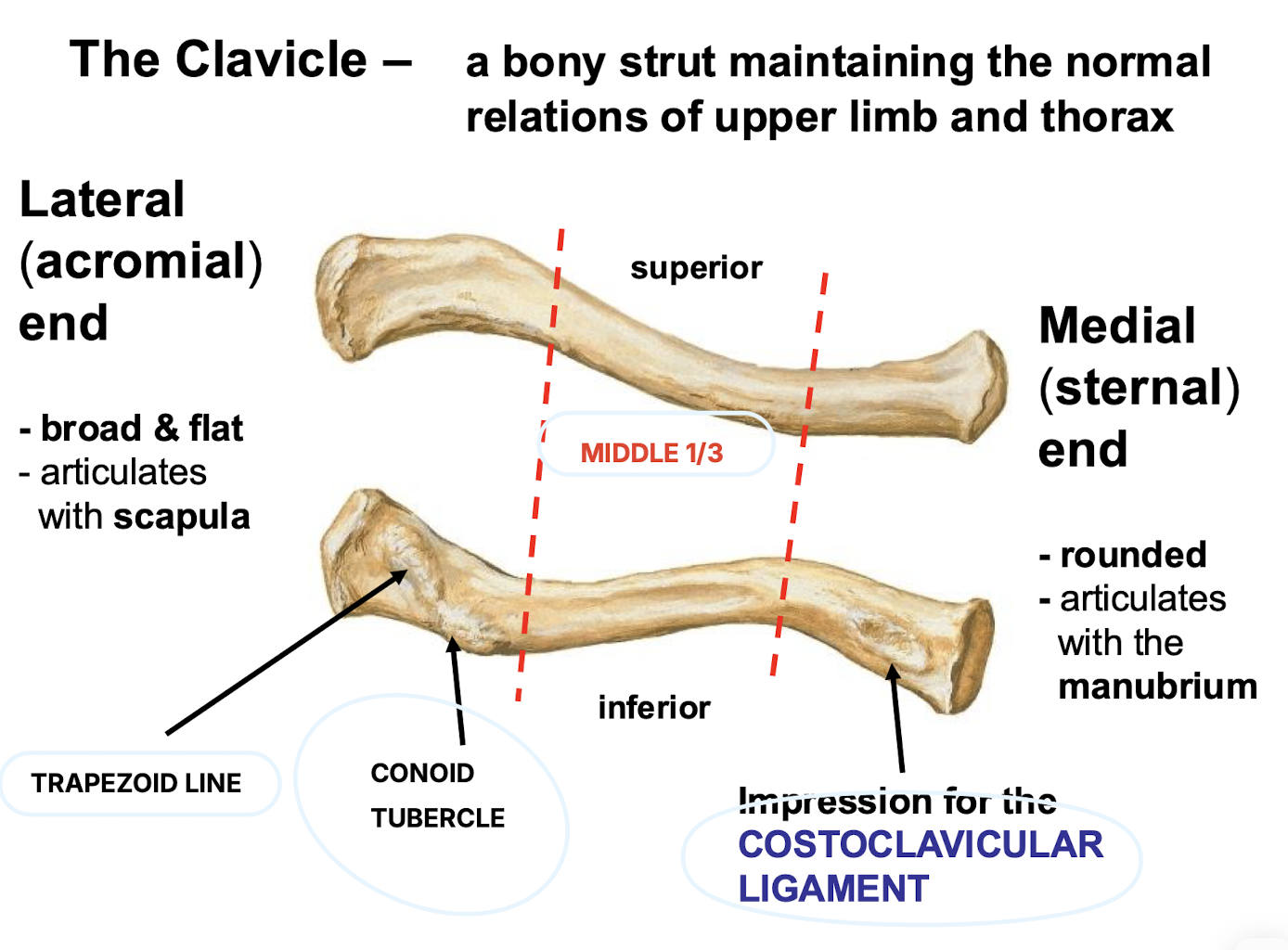
Where is the impression for the costoclavicular ligament located?
On the inferior surface of the clavicle.
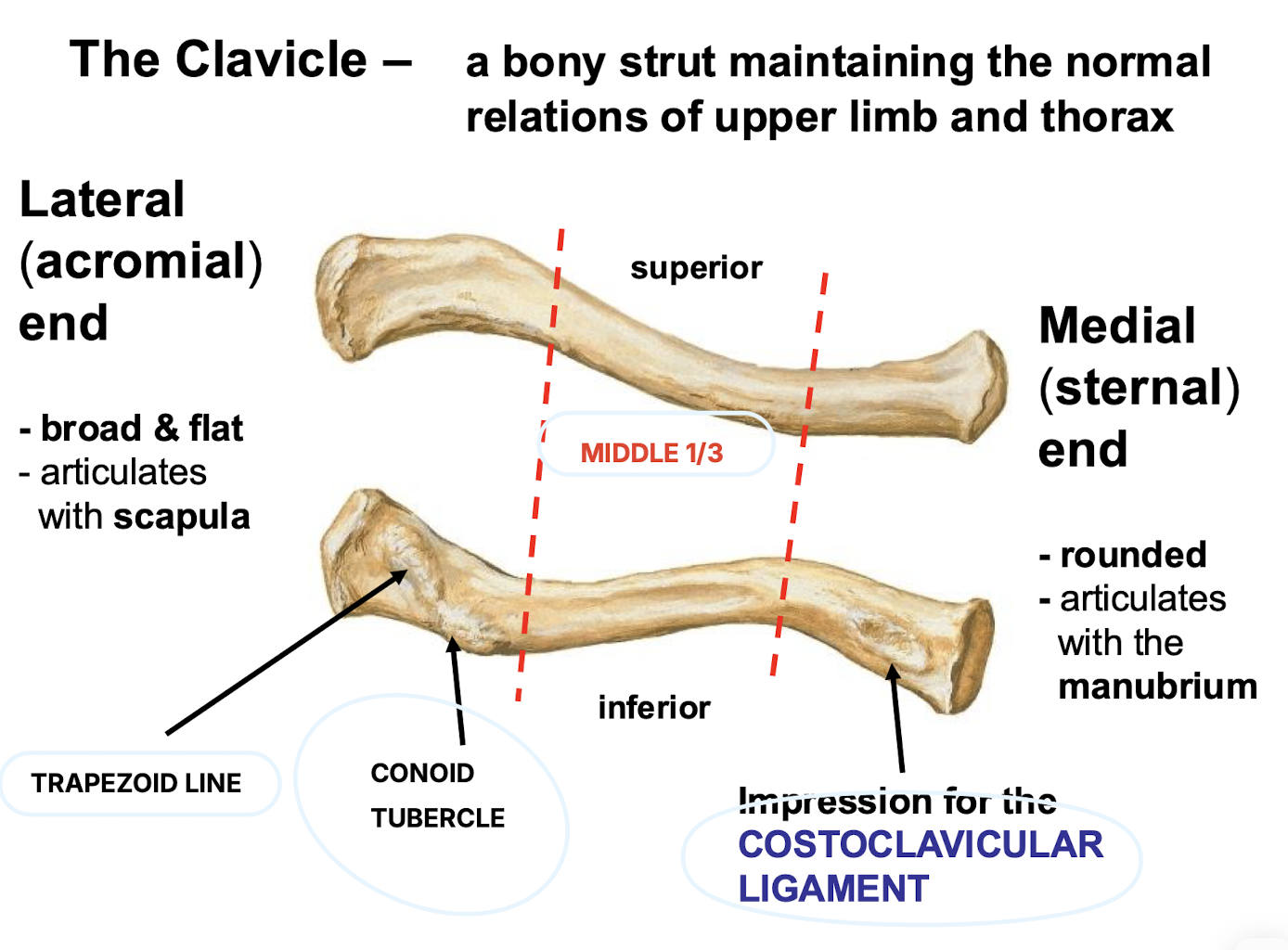
List five reasons why the clavicle is the most frequently fractured bone in the body.
Its role as a strut, early ossification, subcutaneous position, sinuous shape, and the changing cross-sectional shape of its middle third.
What is the typical displacement of the clavicle following a fracture?
The lateral fragment is depressed by the weight of the limb, while the medial fragment is elevated by the sternocleidomastoid muscle.
Identify the three borders and three angles of the scapula.
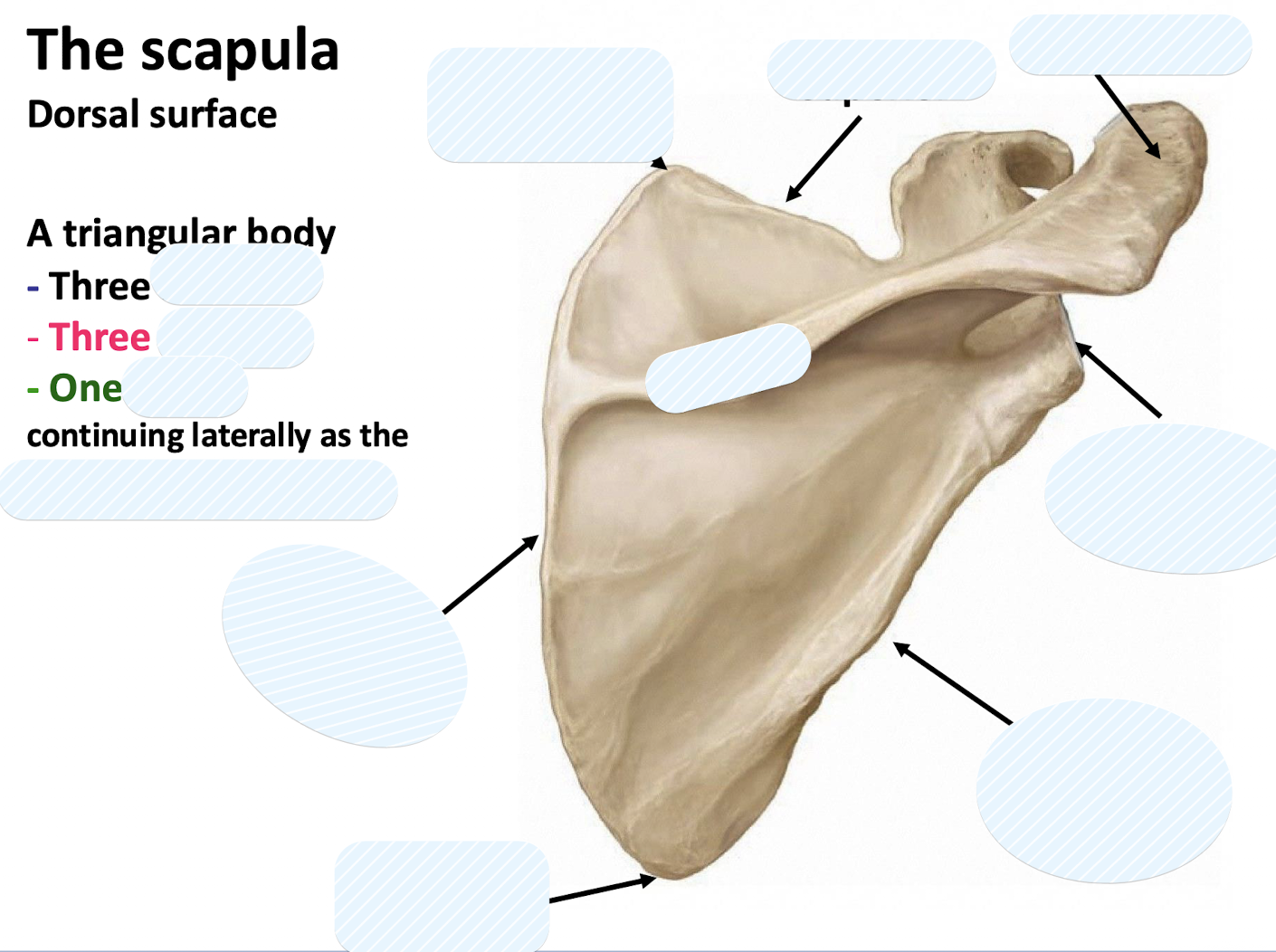
Borders: medial (vertebral), lateral (axillary), and superior; Angles: superior, lateral, and inferior.
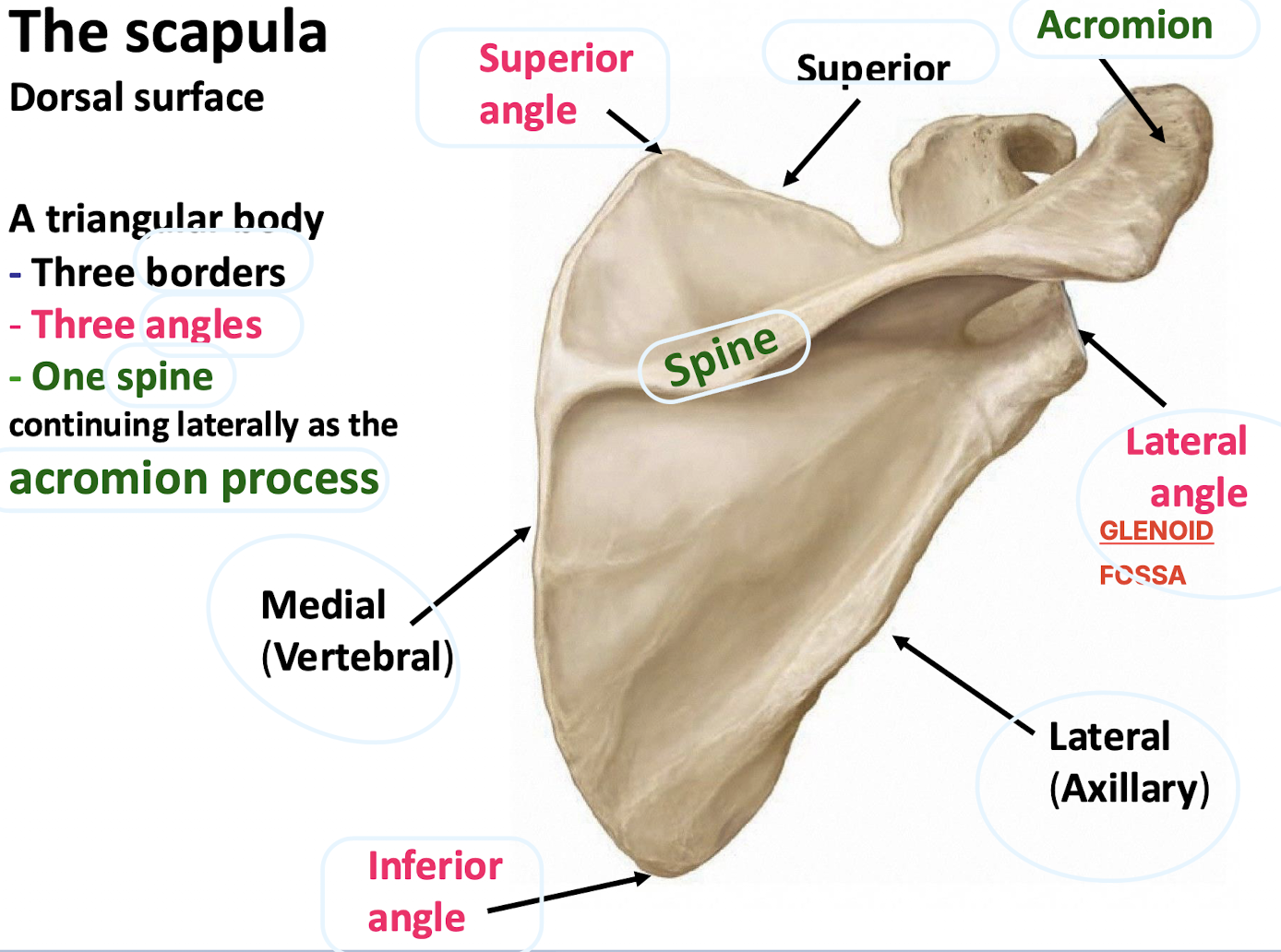
Which dorsal scapular structure continues laterally as the acromion process?
The scapular spine.
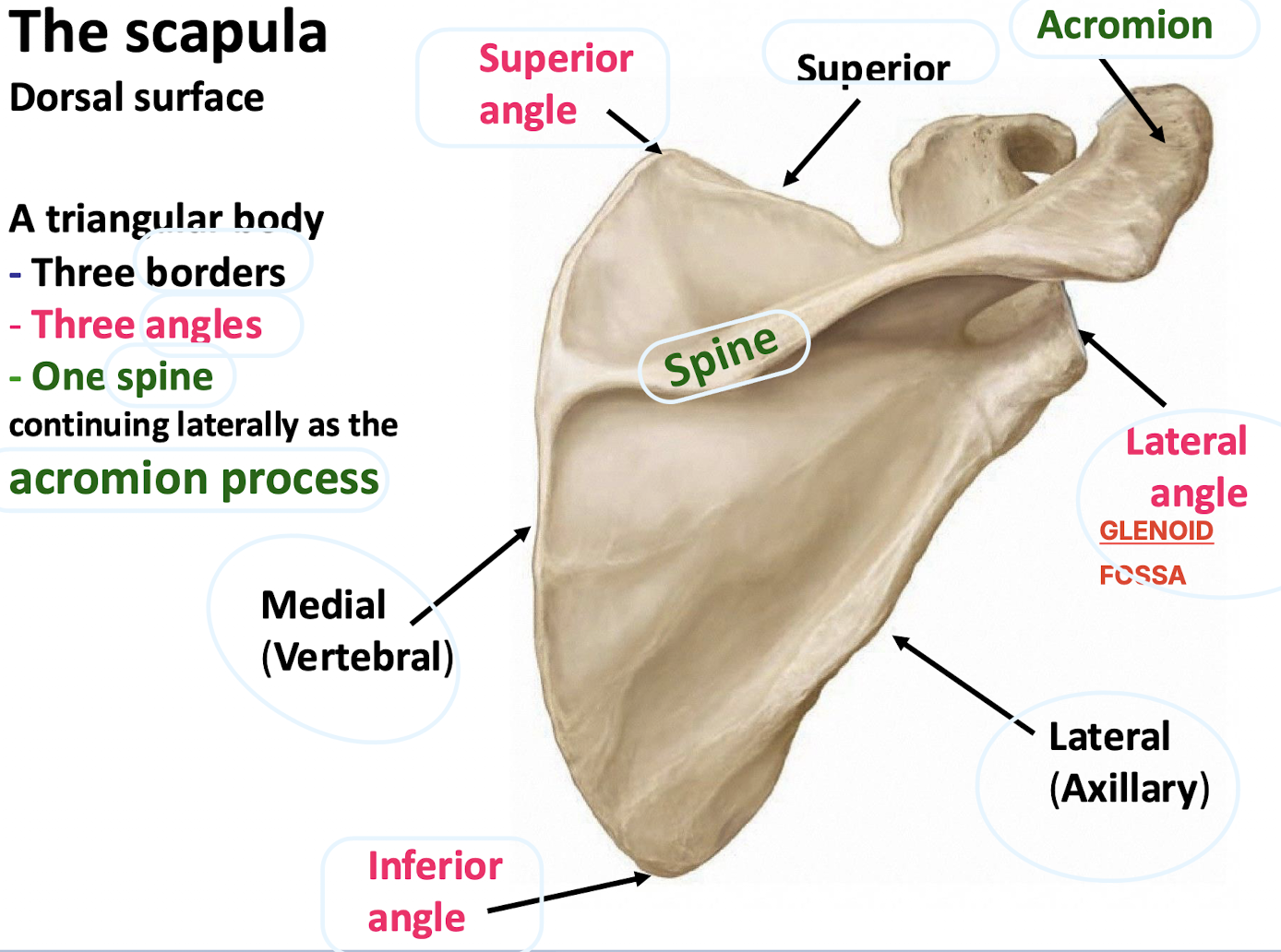
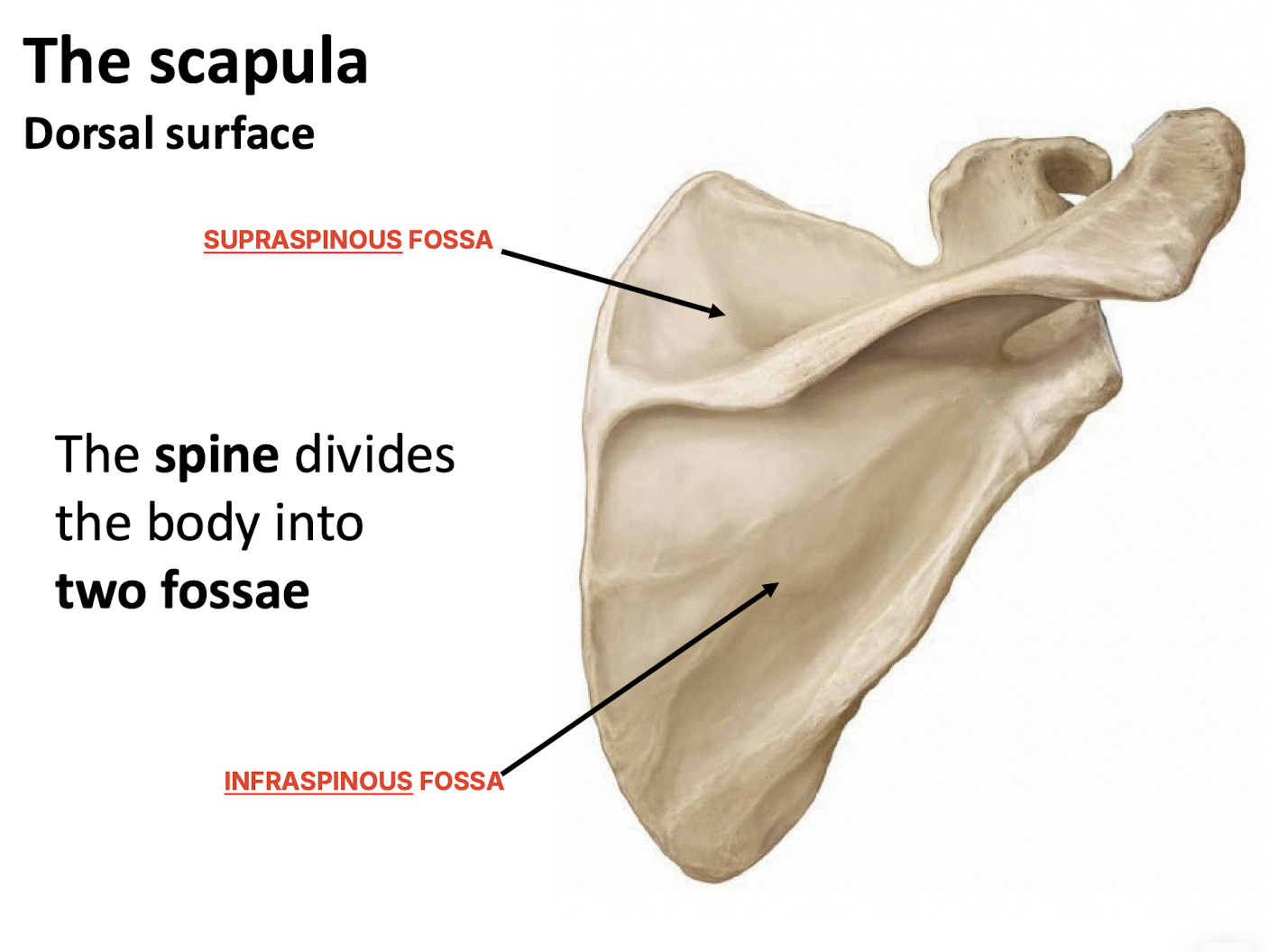
Into which two fossae does the scapular spine divide the dorsal body?
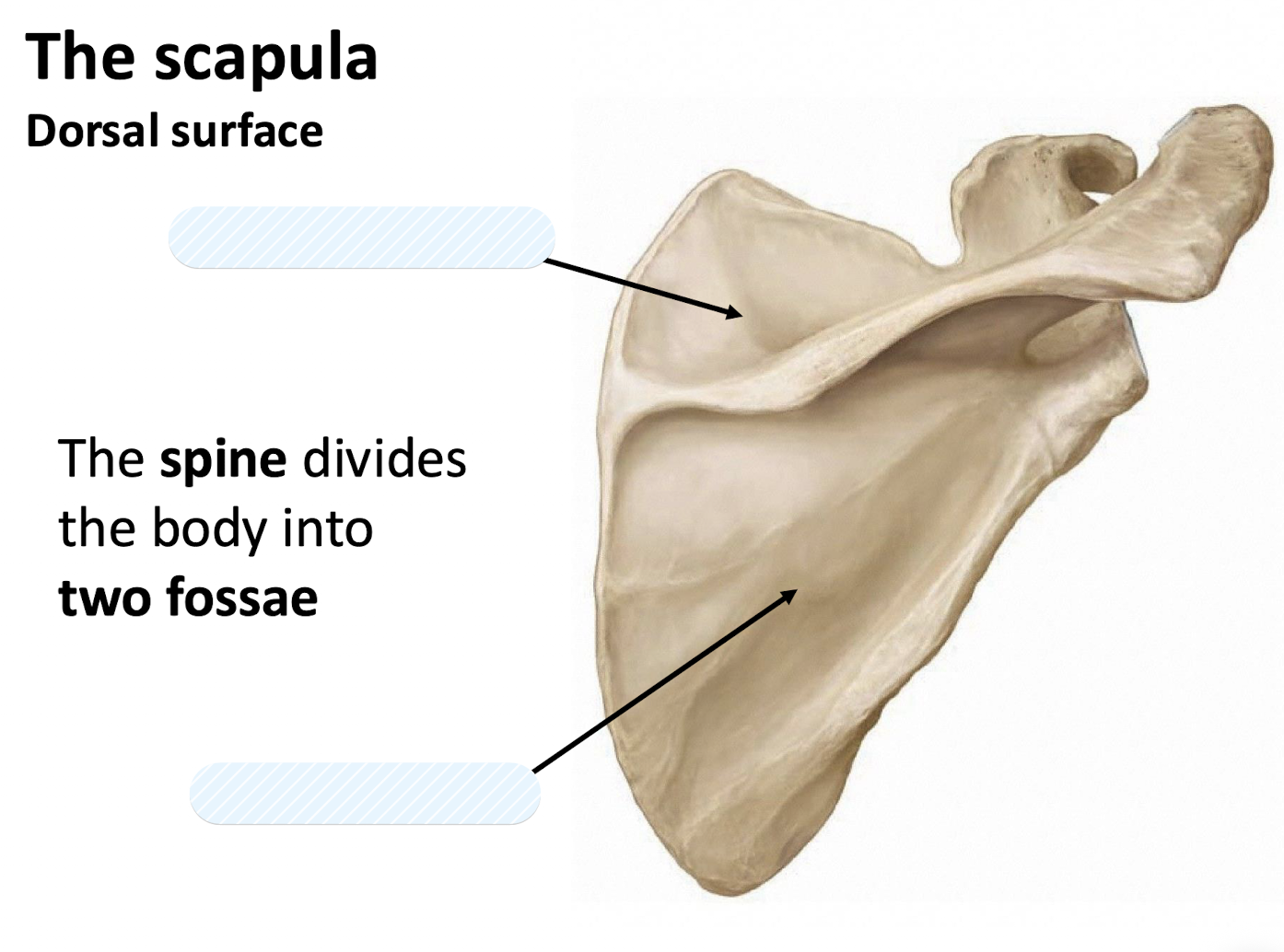
The supraspinous fossa and infraspinous fossa.
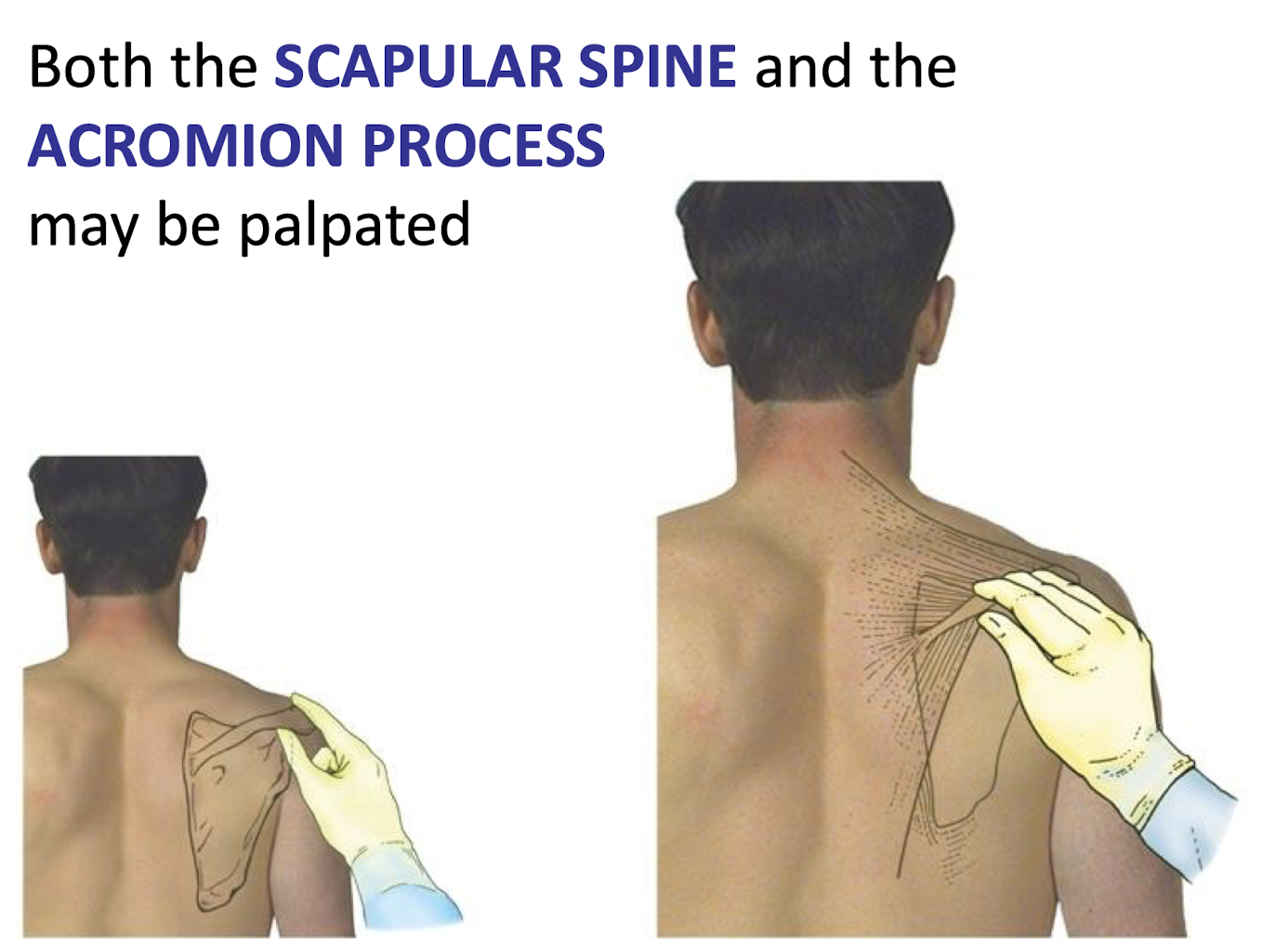
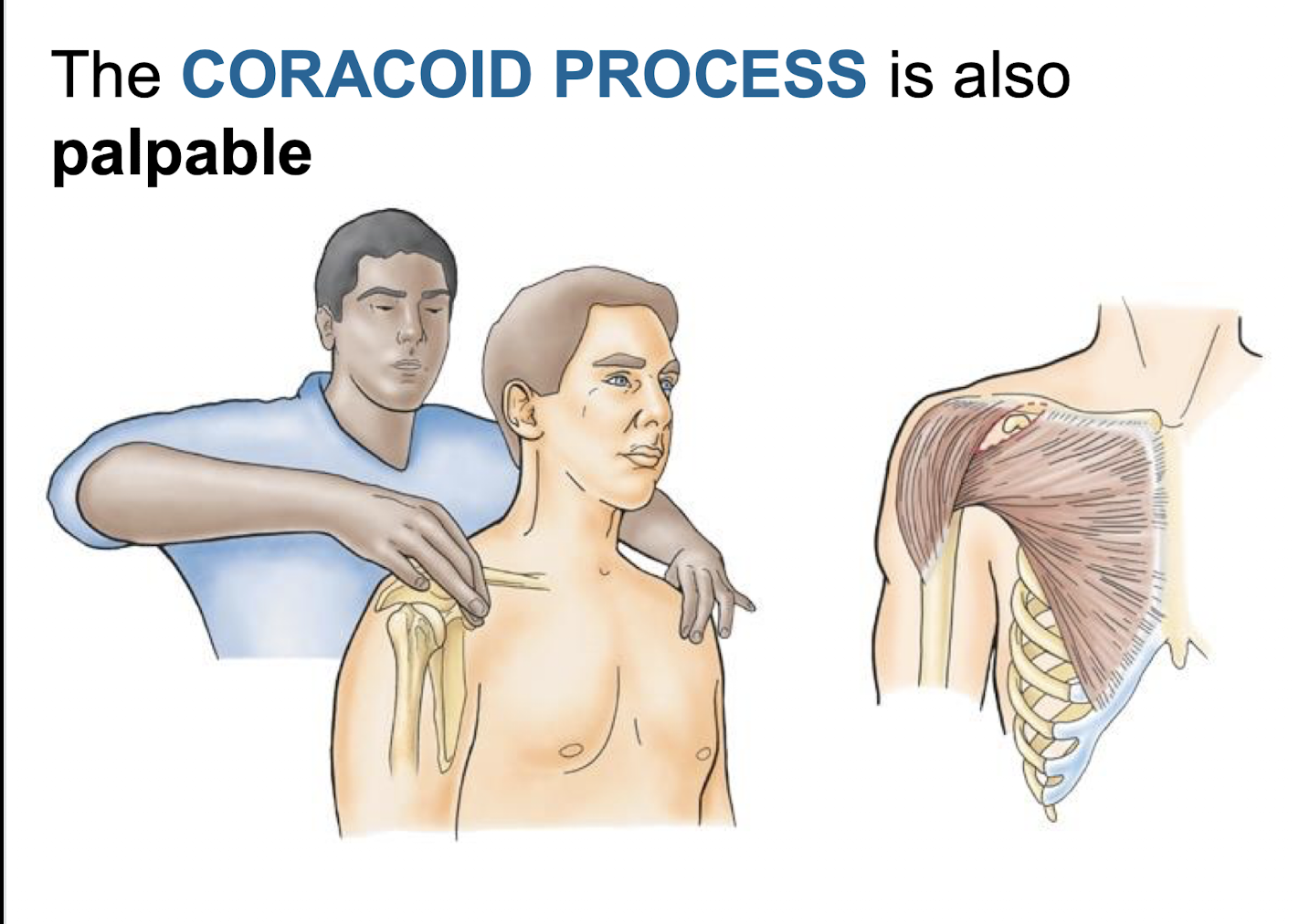
Identify the palpable landmarks of the scapula.
The scapular spine, acromion process, and coracoid process are all palpable.
What is the name of the fossa on the ventral (costal) surface of the scapula?
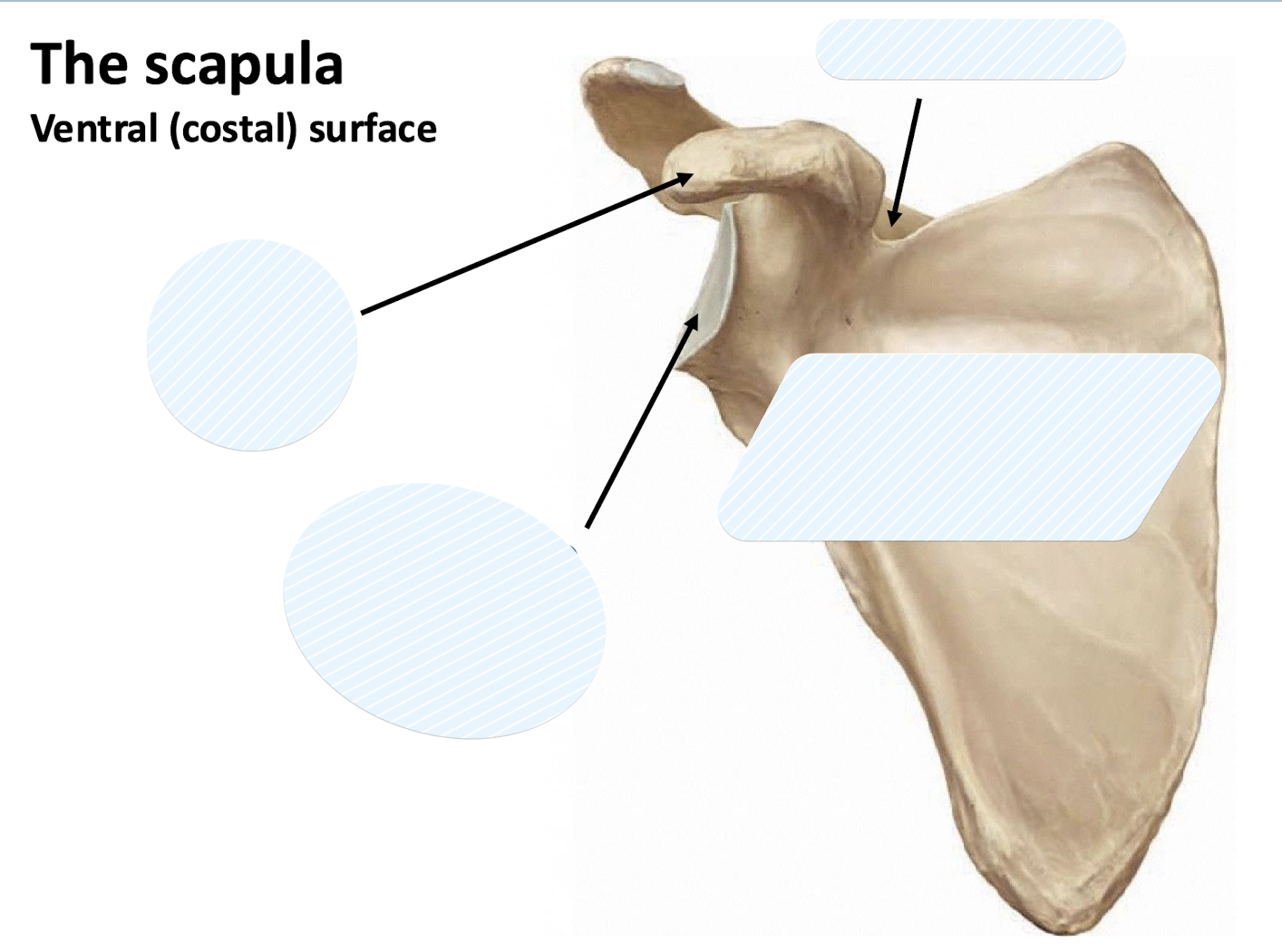
The subscapular fossa.
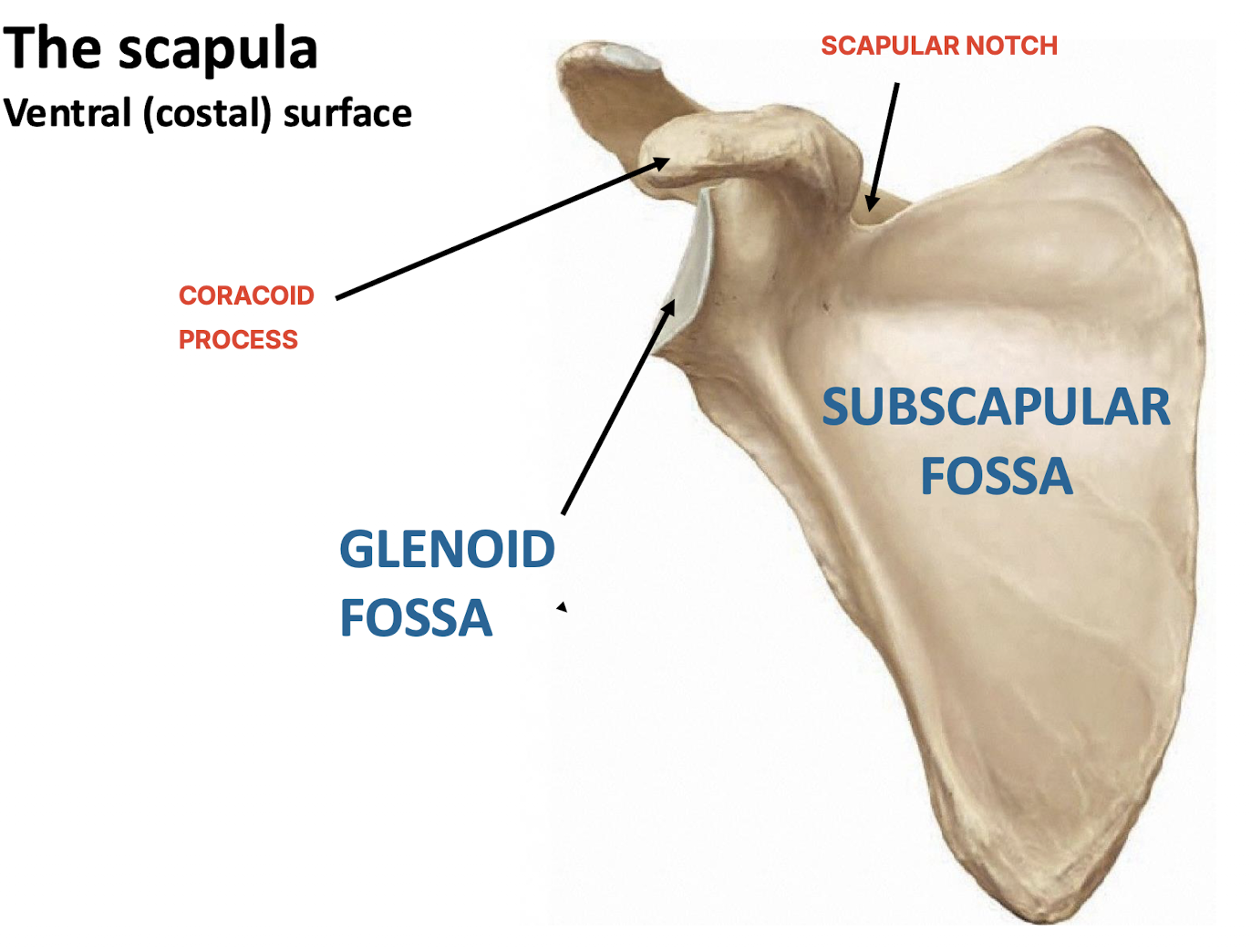
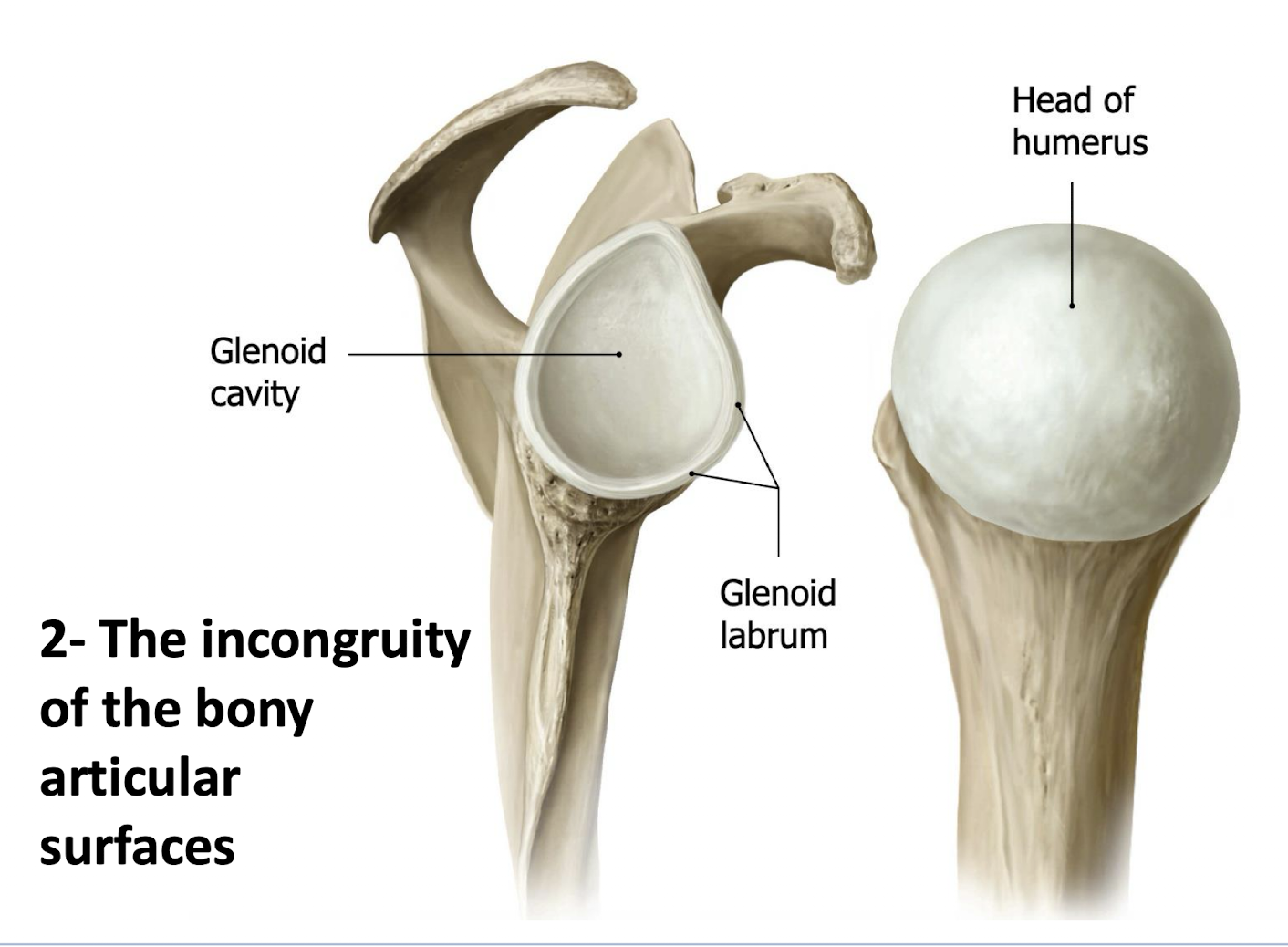
What structure deepens the shallow, oval articular surface of the glenoid fossa?
A cartilaginous labrum.
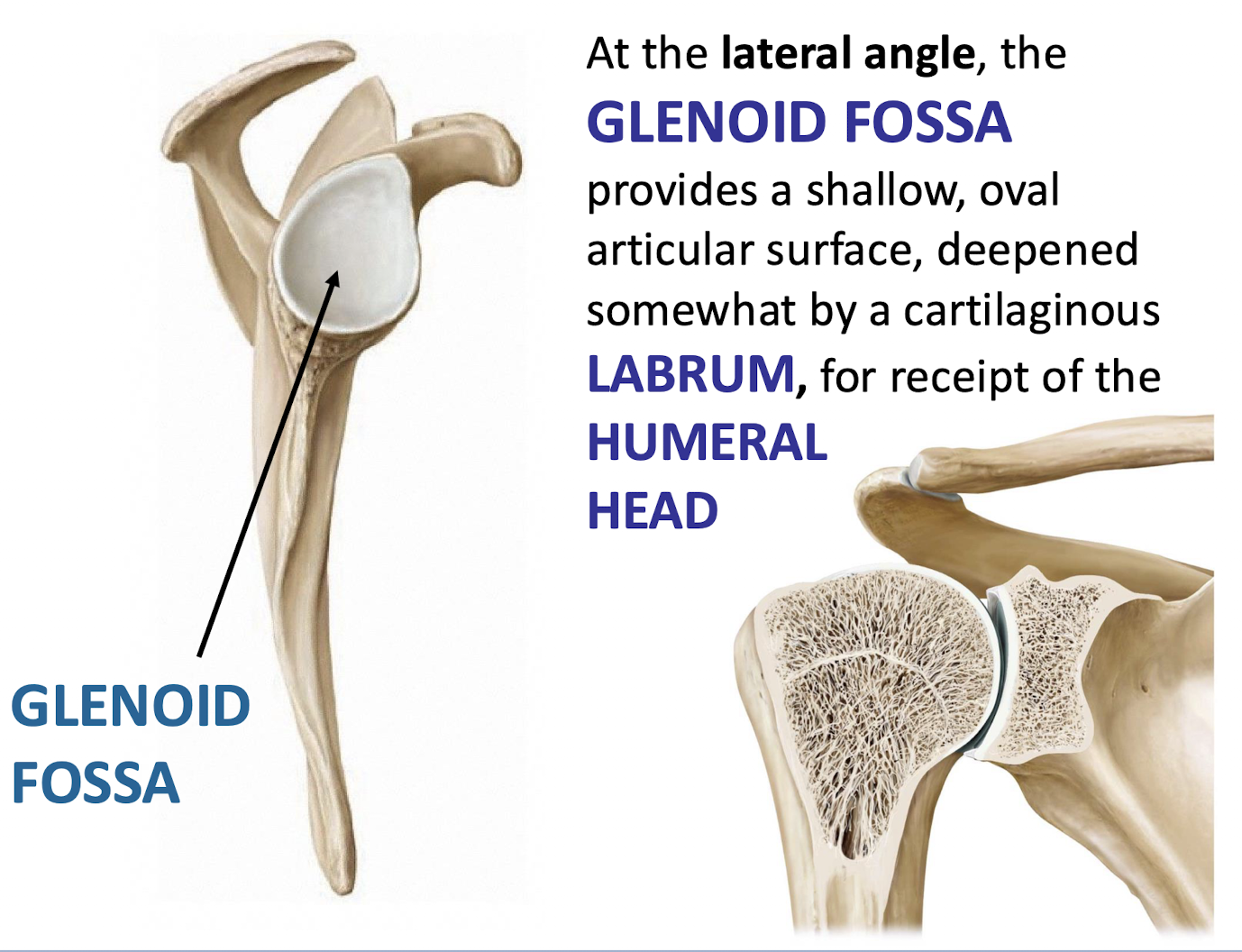
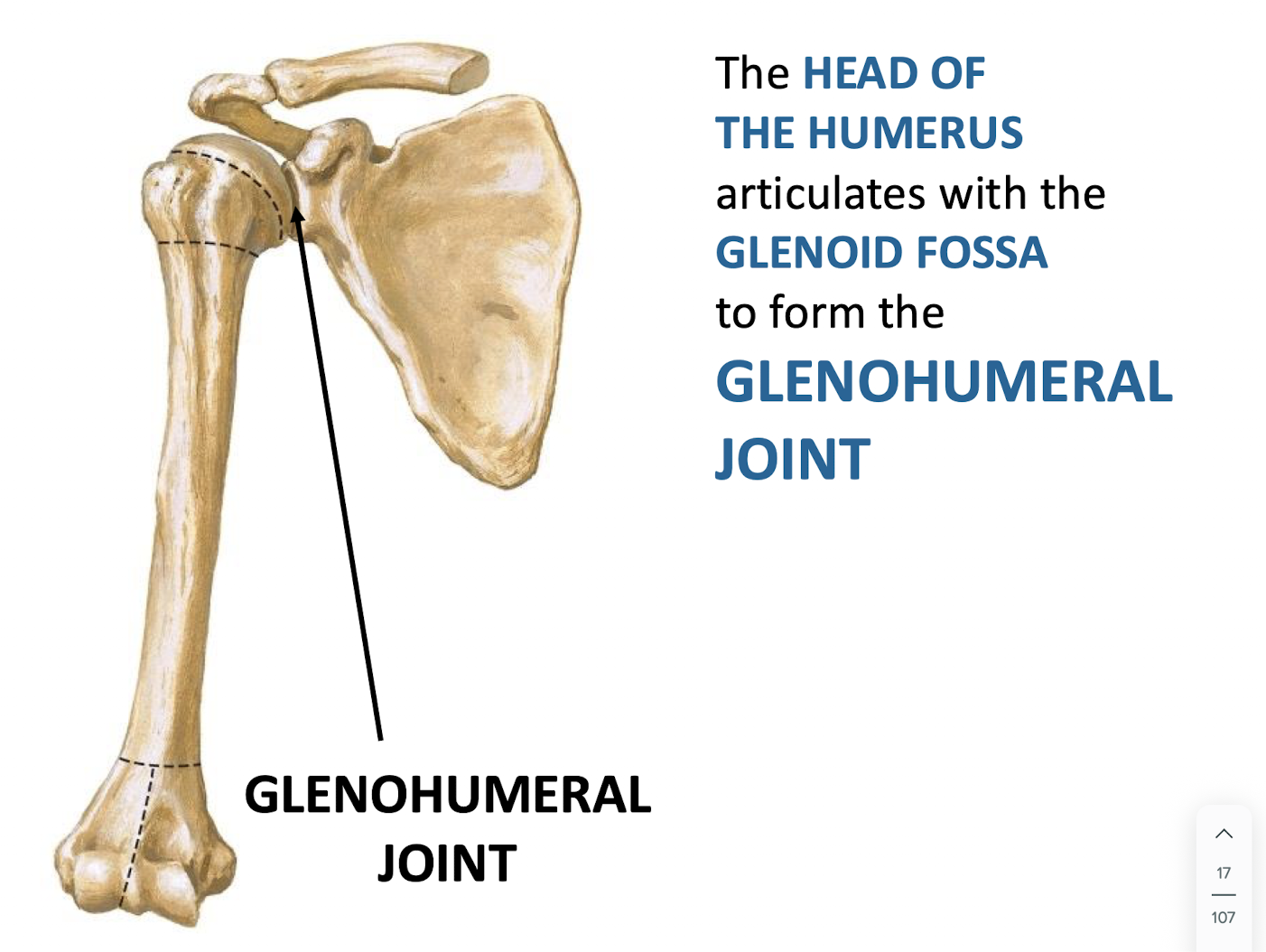
The glenohumeral joint is formed by the articulation of which two structures?
The head of the humerus and the glenoid fossa of the scapula.
Identify the landmarks on the proximal humerus visible in an anterior view.
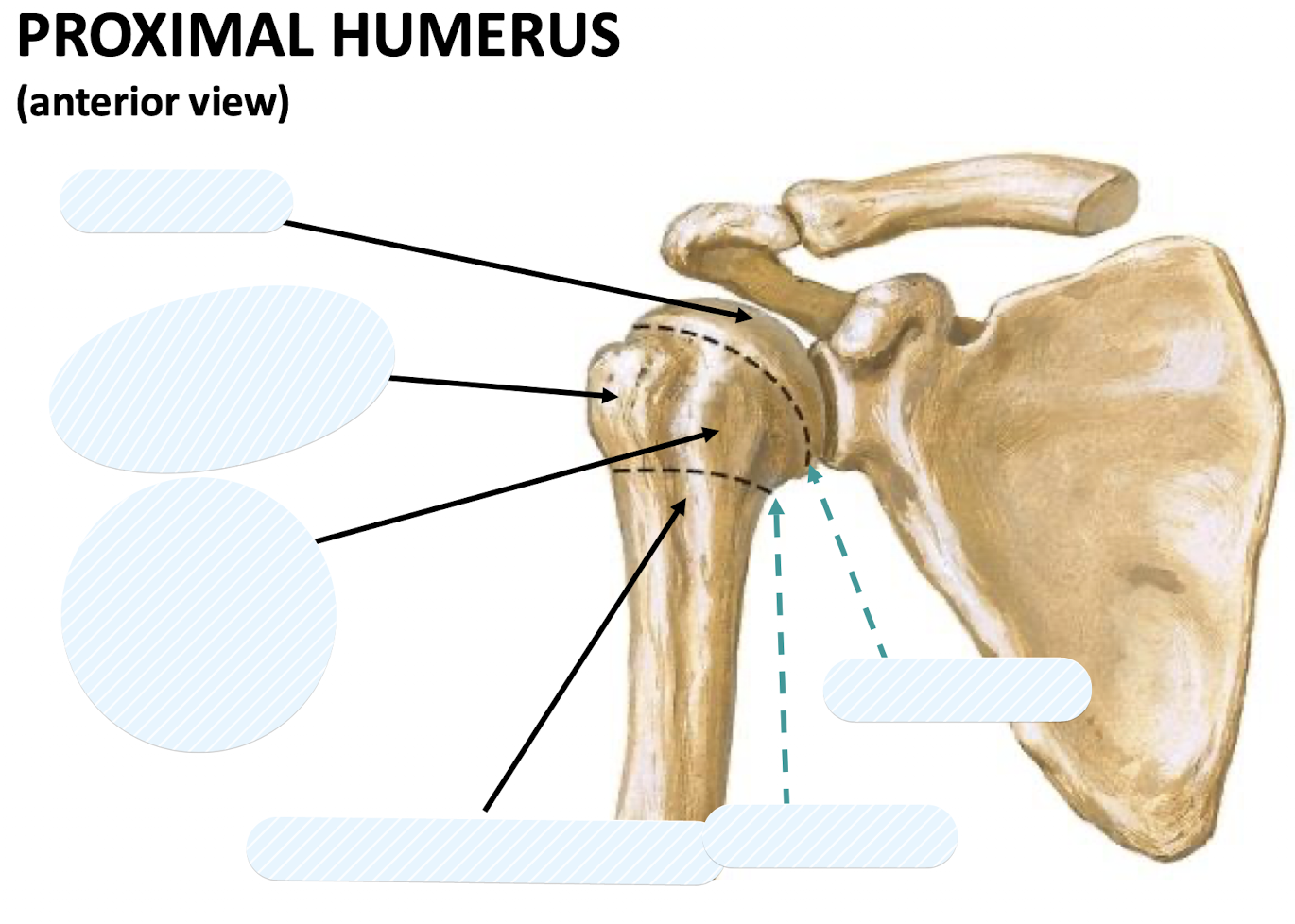
The head, anatomical neck, surgical neck, Intertubercular (Bicipital) sulcus, greater tubercle, and lesser tubercle.
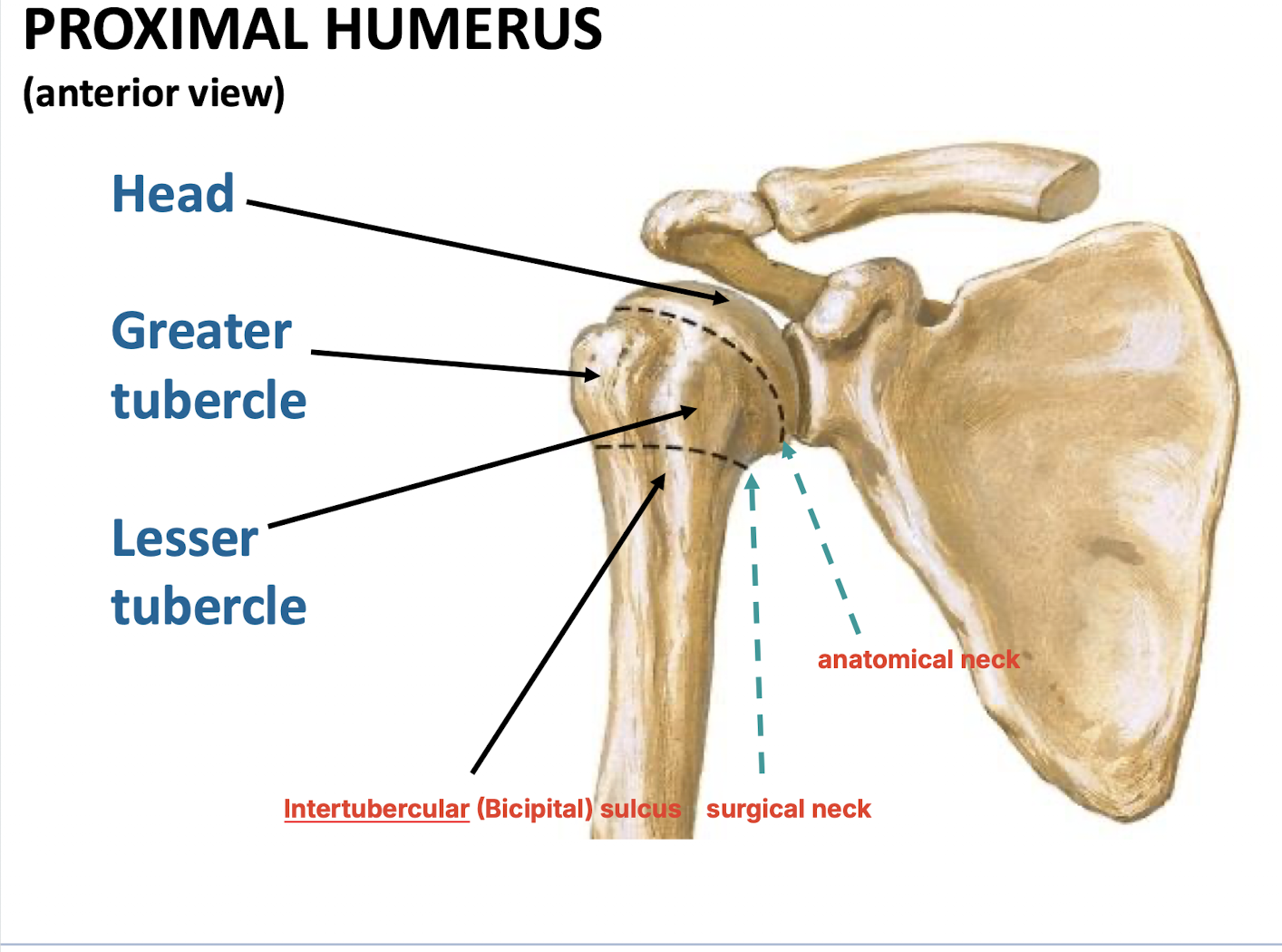
Which landmark on the humerus is found on the lateral aspect of the shaft in a posterior view?
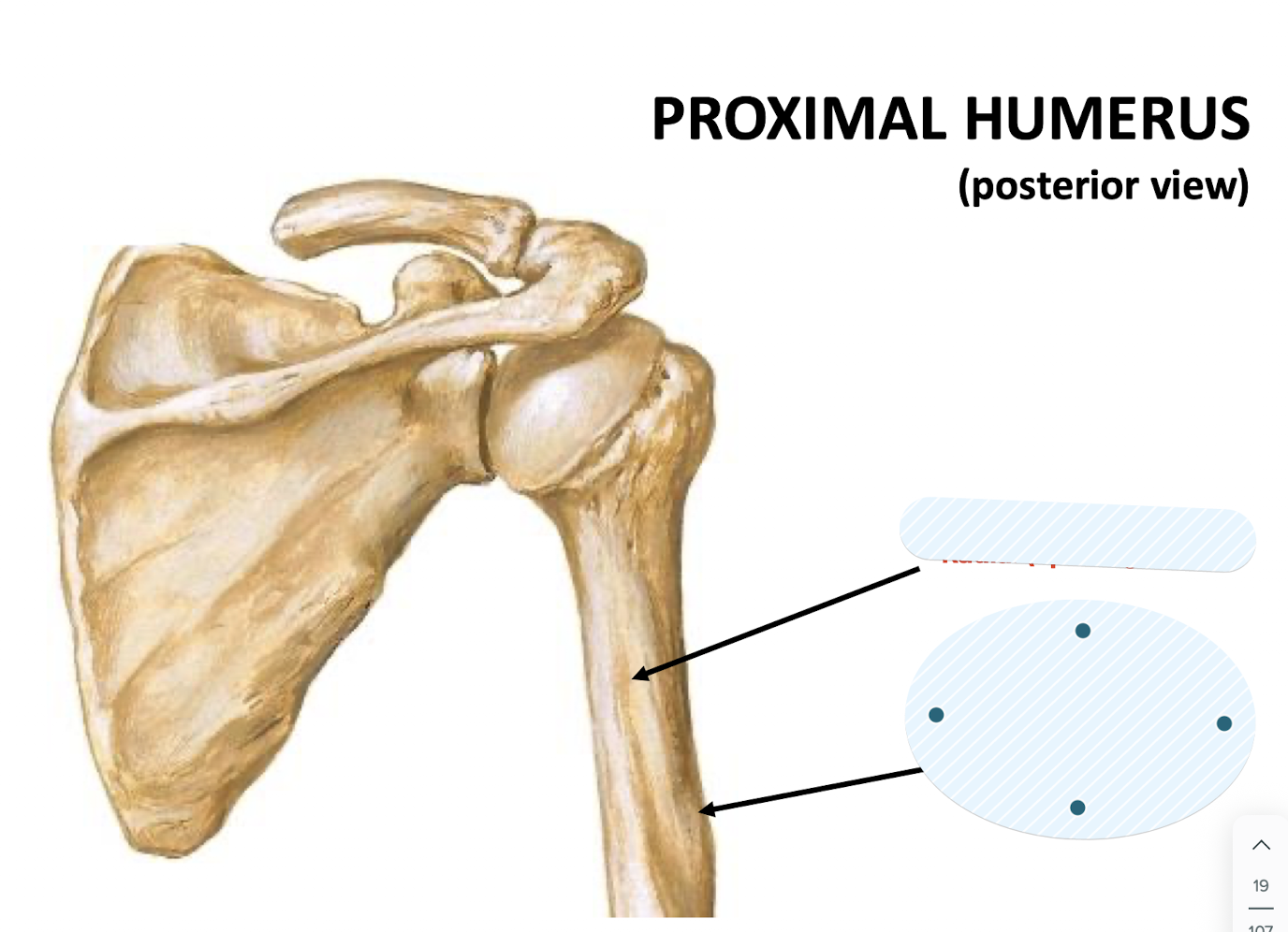
The deltoid tuberosity.
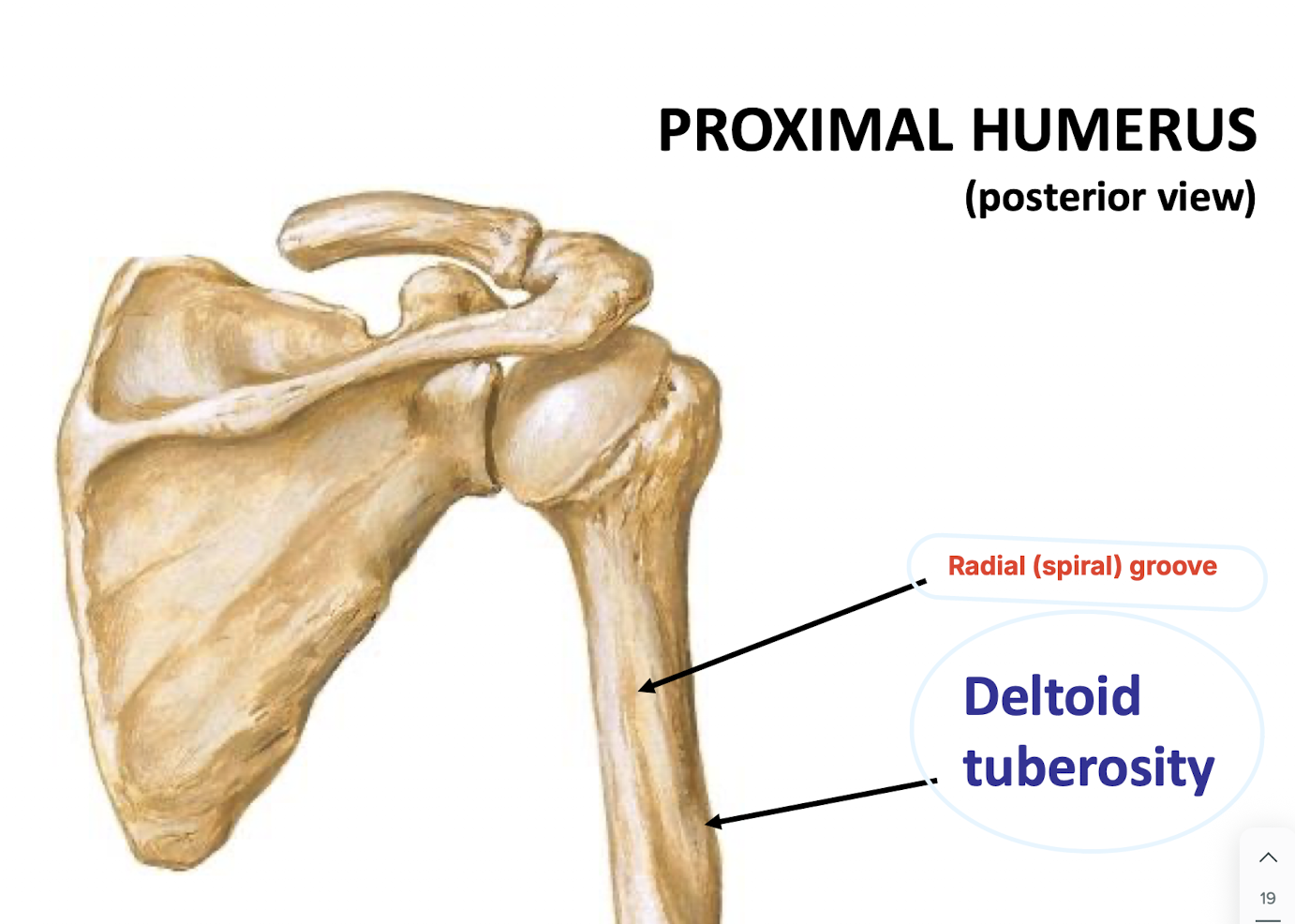
Radial nerve lies in the groove
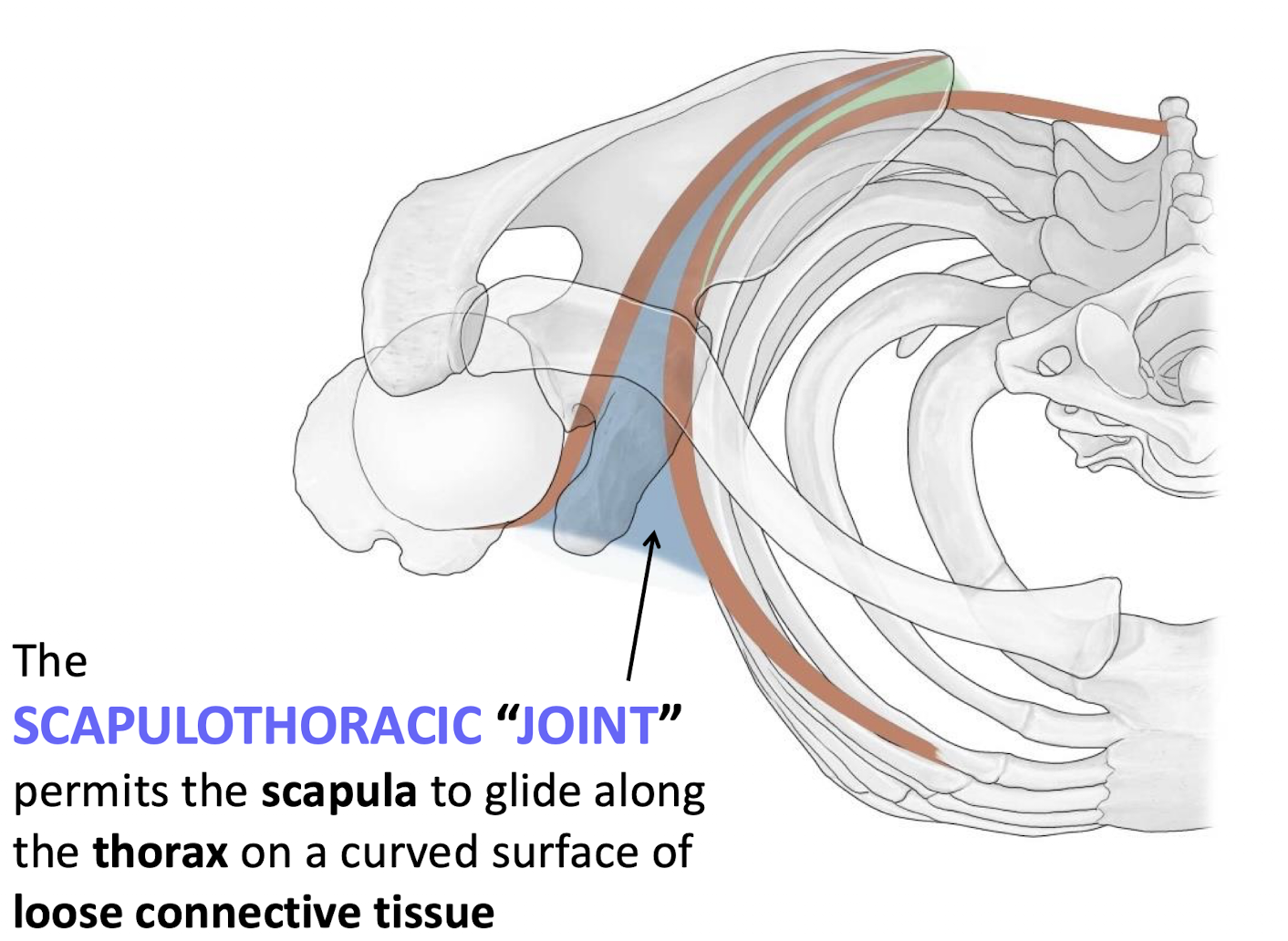
What constitutes the scapulothoracic "joint"?
The space between the ventral (costal) surface of the scapula and the posterior thoracic wall.
What type of muscle contraction results in movement at the scapulothoracic "joint"?
Contraction of extrinsic shoulder (thoracoappendicular) muscles.
What type of muscle contraction results in movement at the glenohumeral joint?
Contraction of intrinsic (scapulohumeral) muscles.
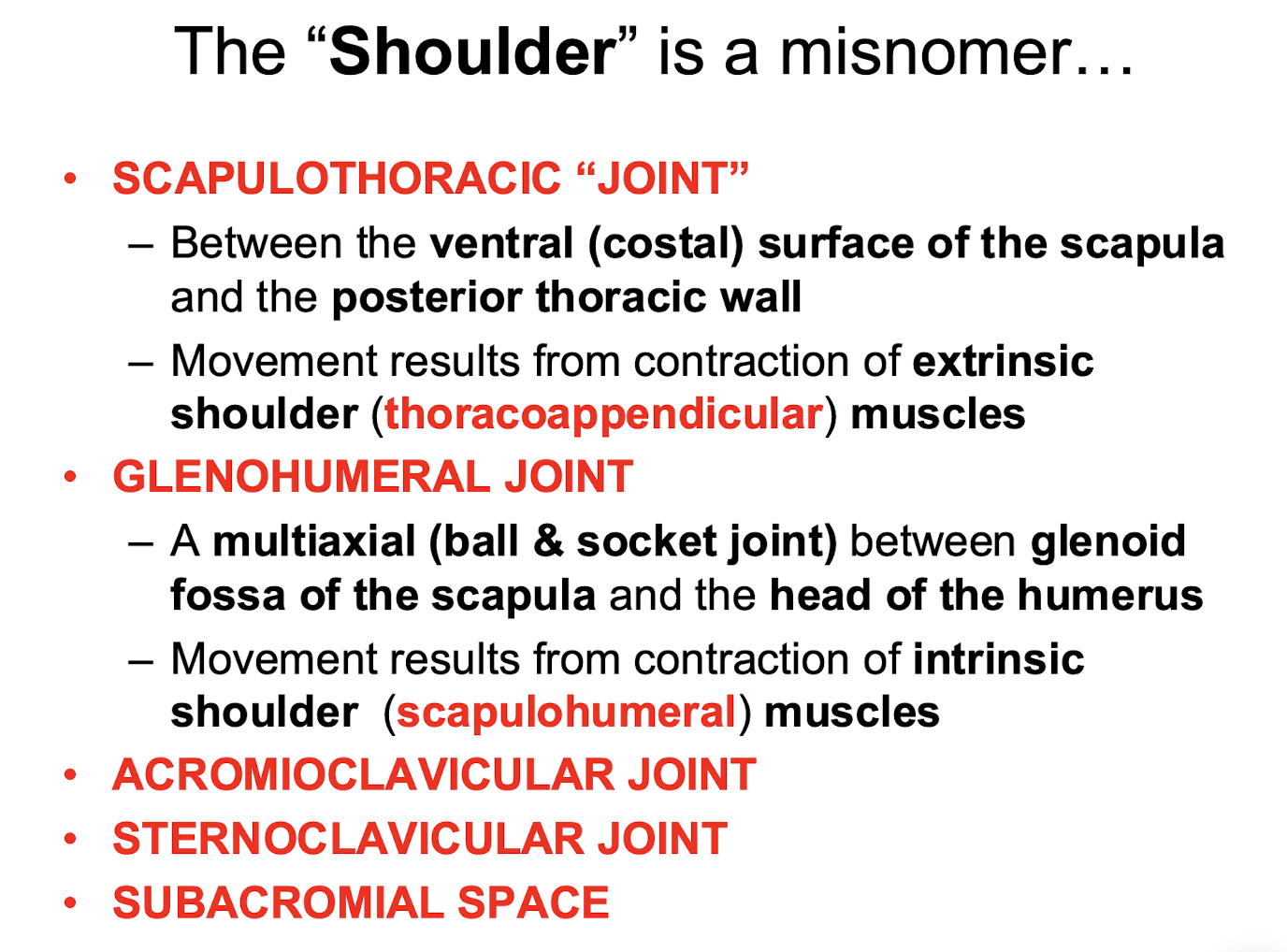
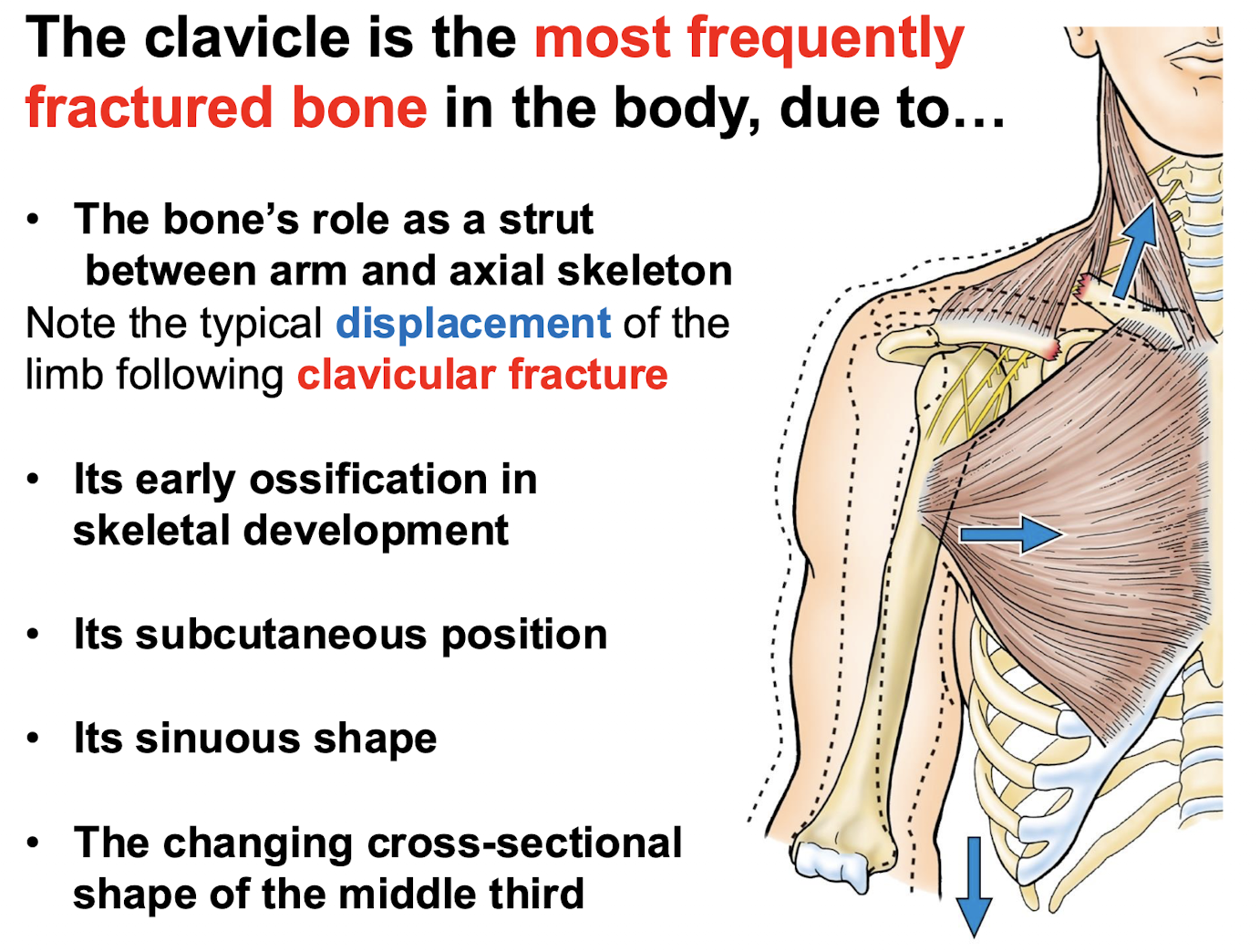
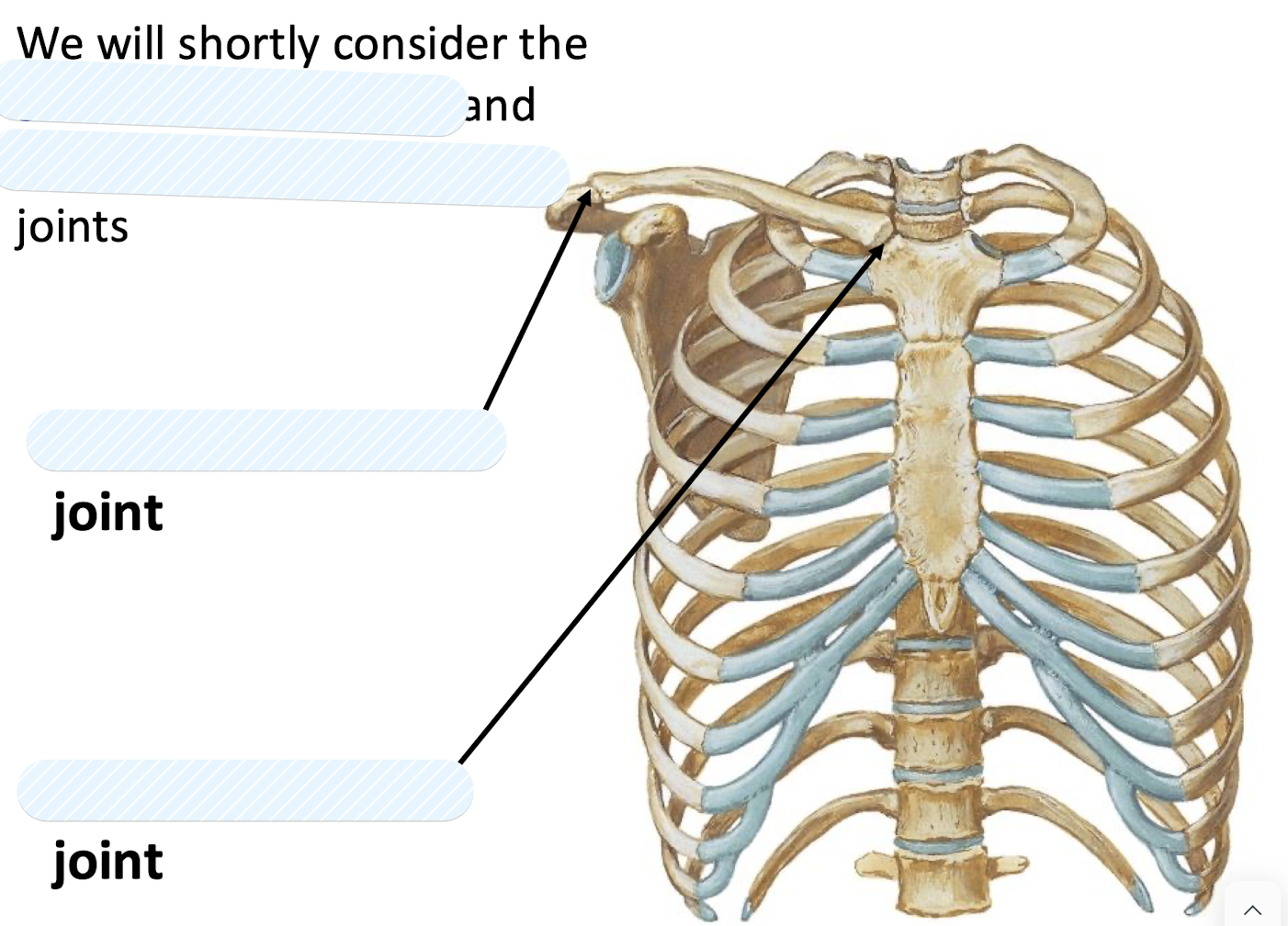
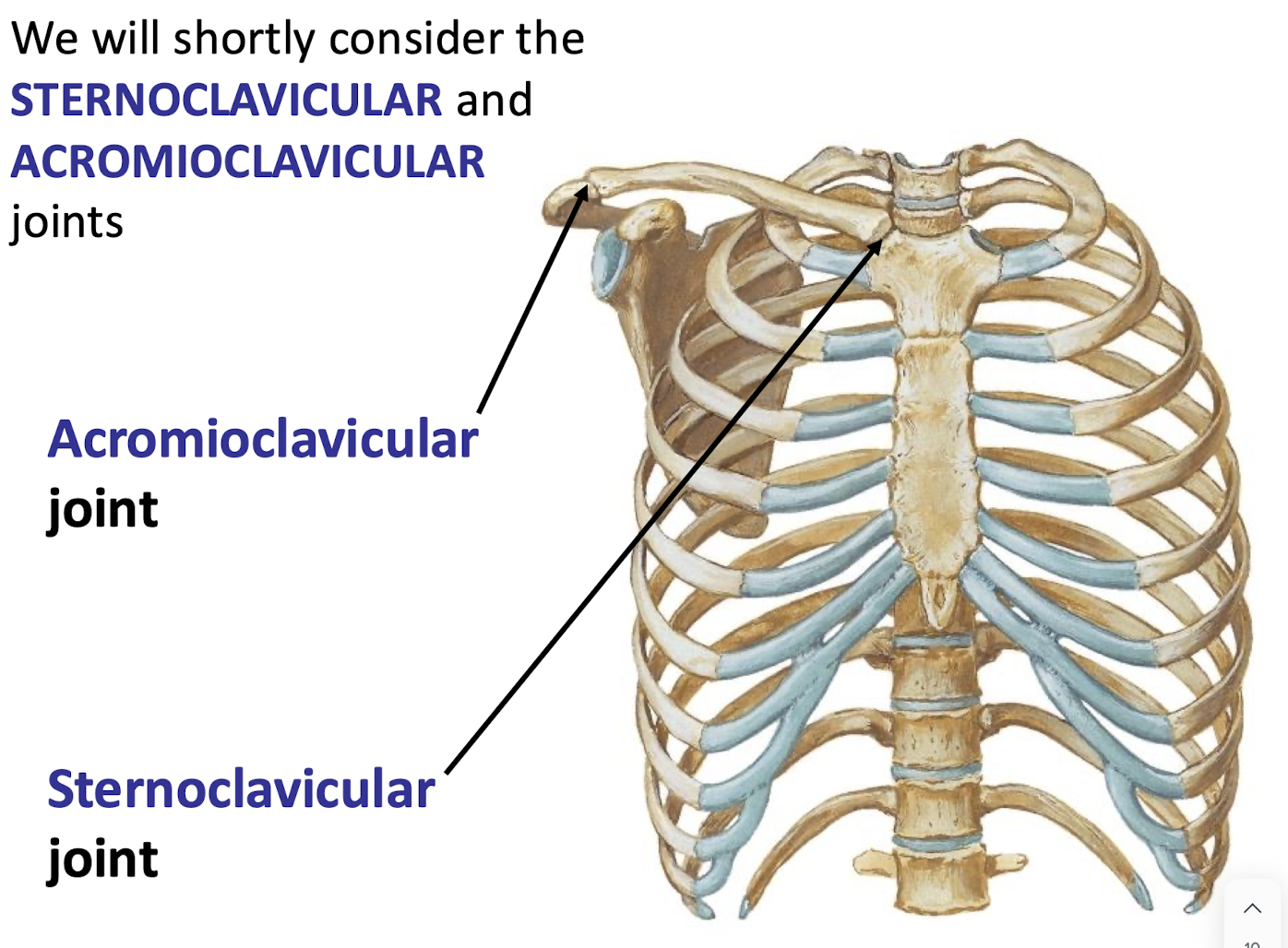
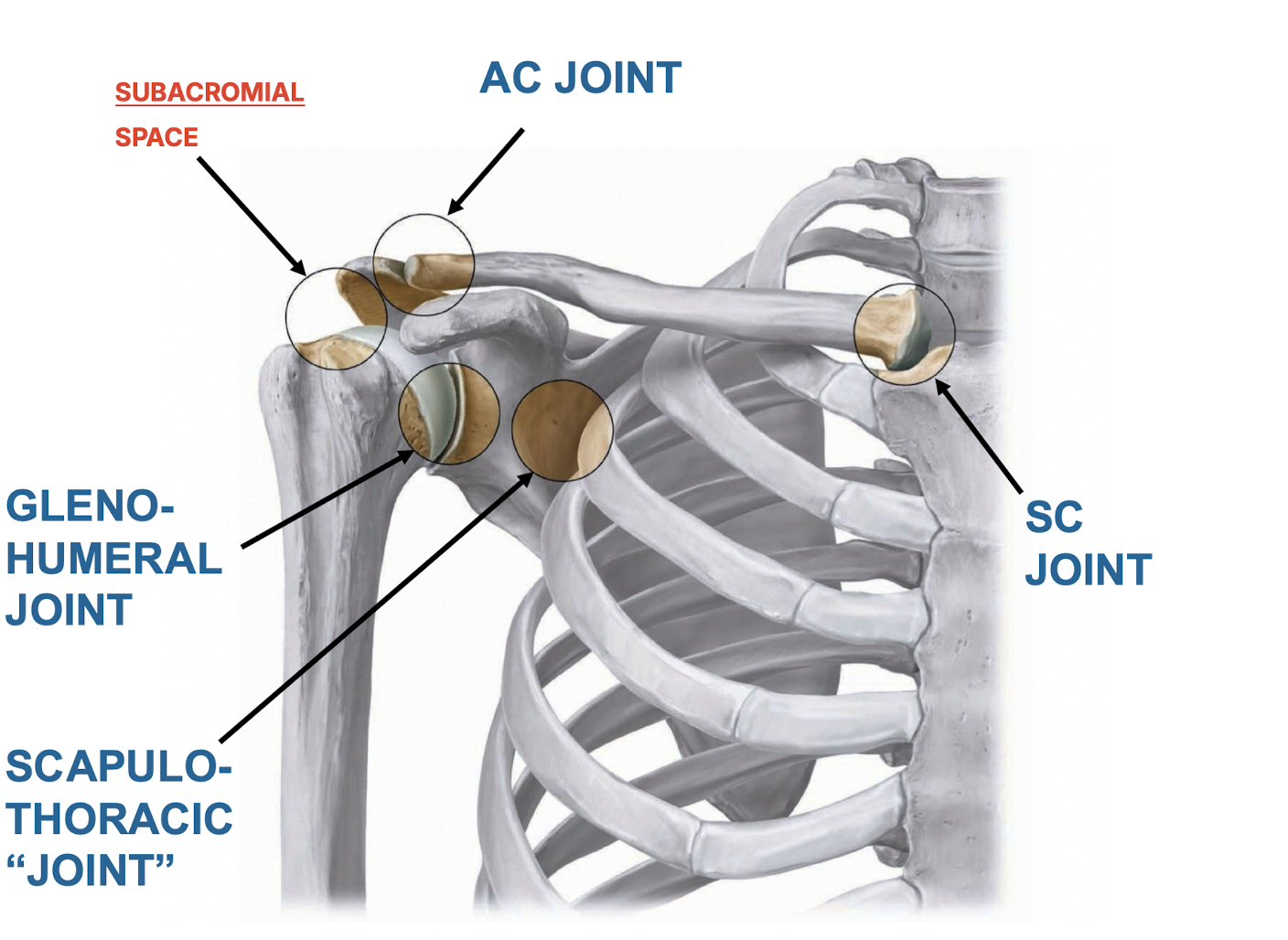
Which four components are often misnamed simply as the "shoulder"?
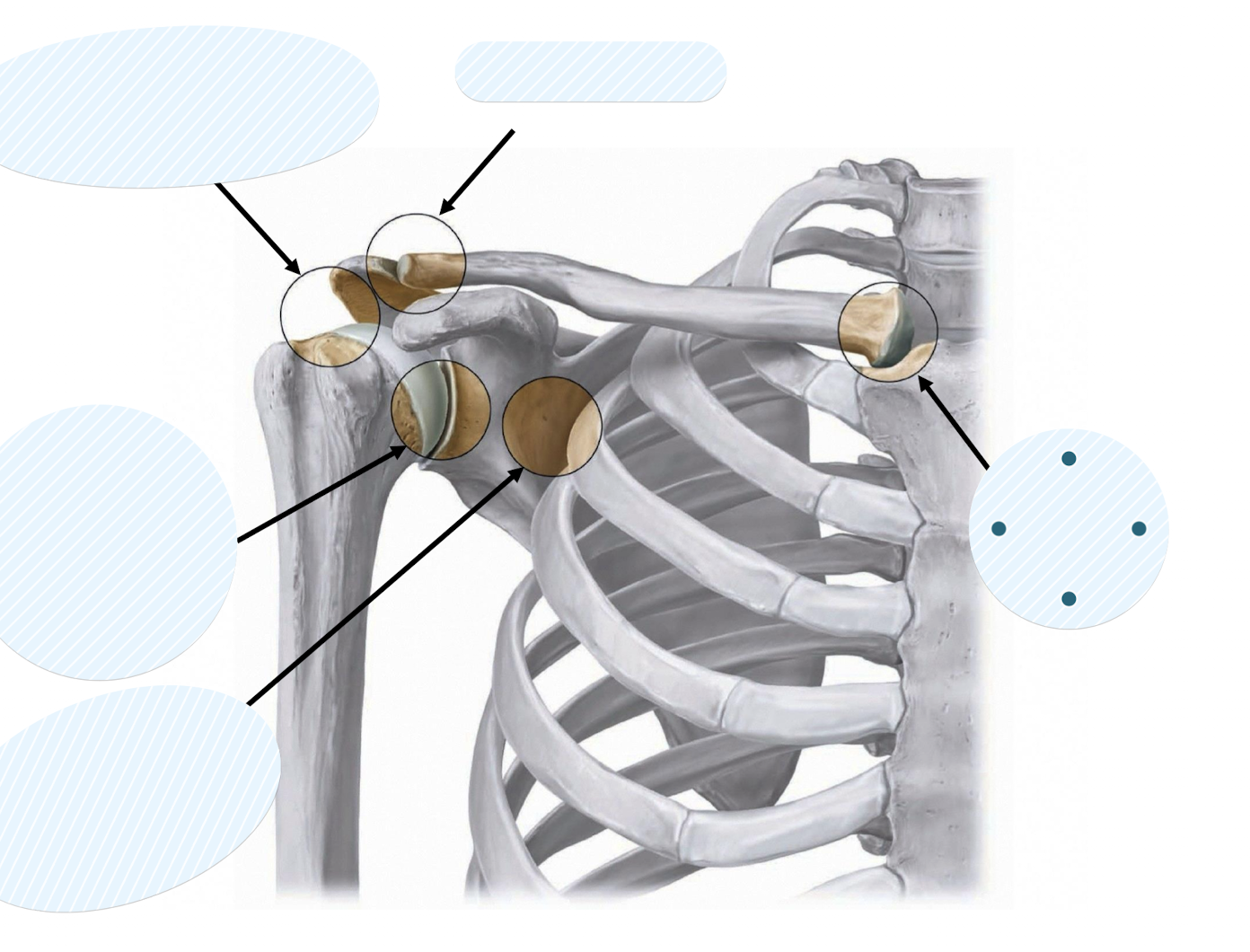
The sternoclavicular (SC) joint, acromioclavicular (AC) joint, glenohumeral joint, and scapulothoracic "joint".
What is the function of the scapulothoracic joint?
The SCAPULOTHORACIC “JOINT” permits the scapula to glide along the thorax on a curved surface of loose connective tissue
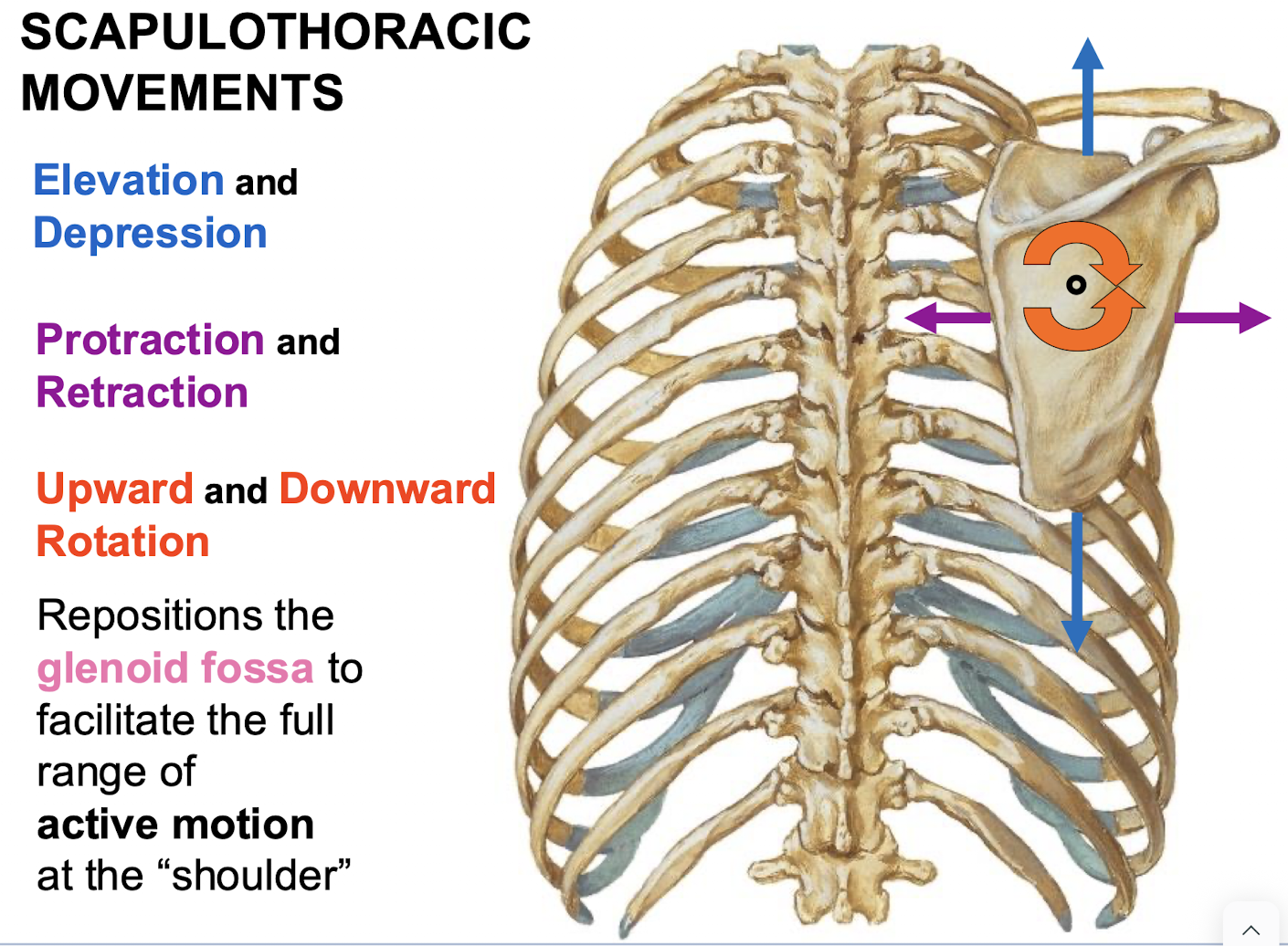
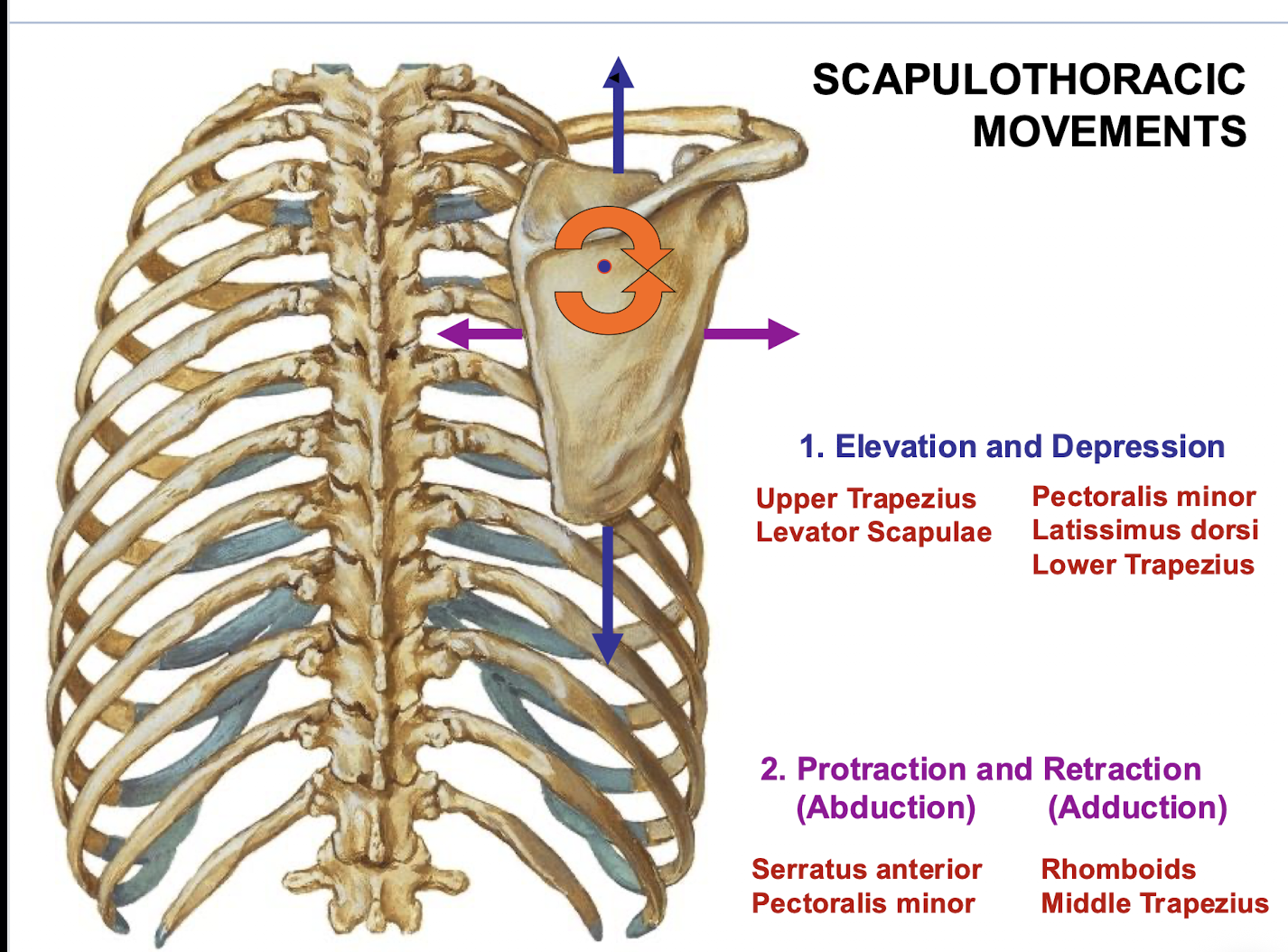
List the three primary pairs of movements allowed by the scapulothoracic joint.
Elevation/depression, protraction/retraction, and upward/downward rotation.
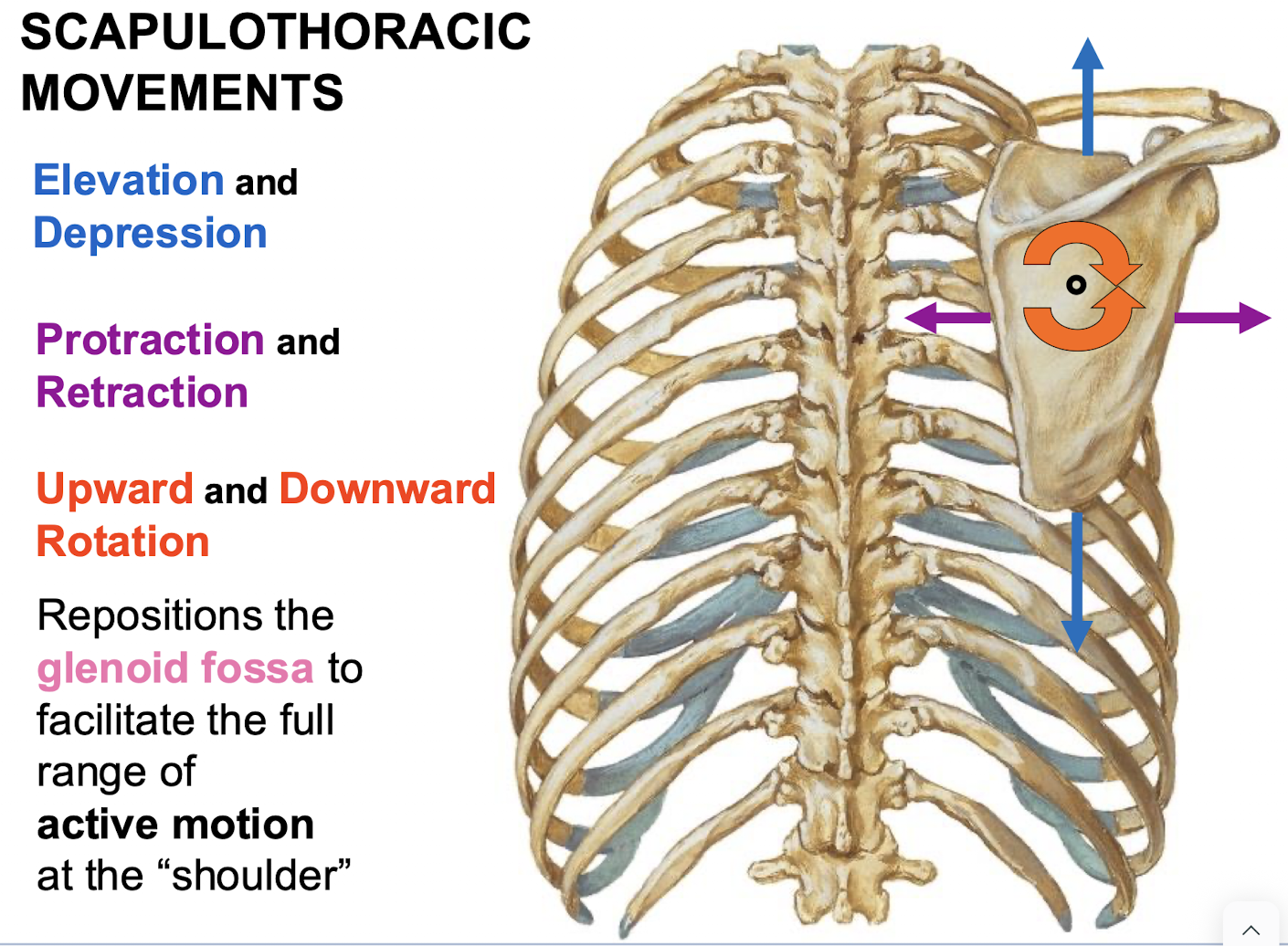
What is the functional purpose of scapulothoracic movements?
To reposition the glenoid fossa to facilitate the full range of active motion at the shoulder.
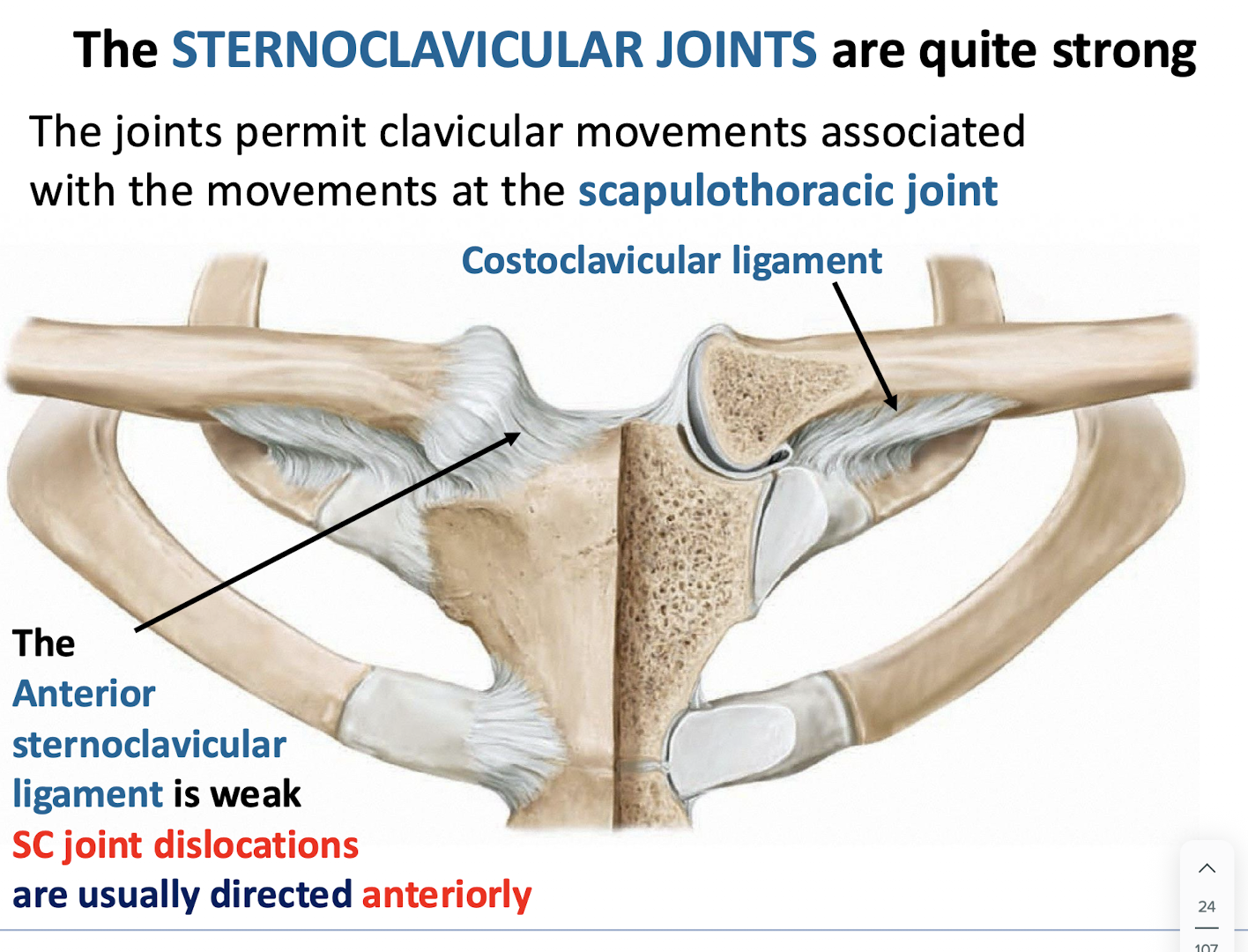
Which ligament is considered weak, making the sternoclavicular joint susceptible to dislocation?
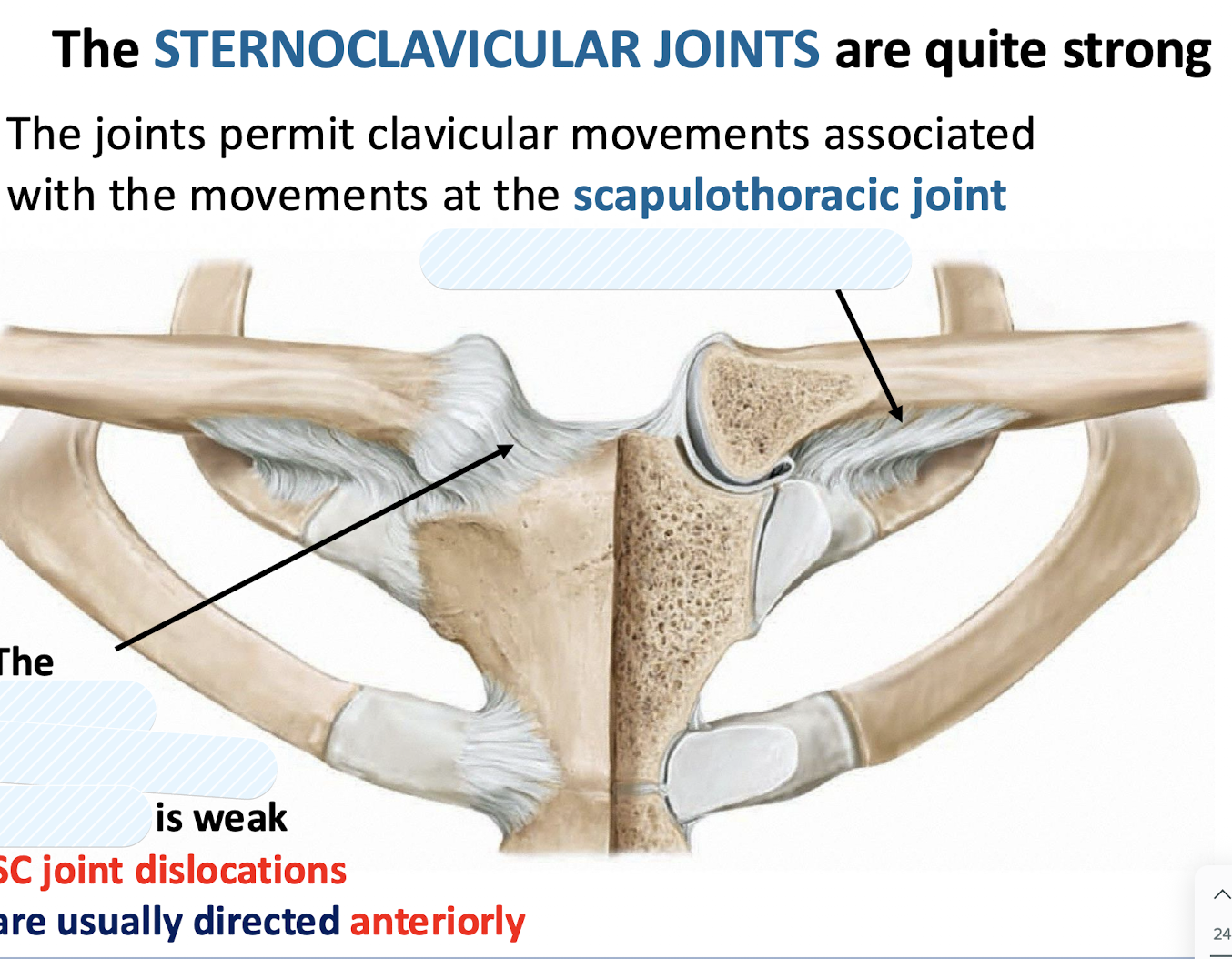
The anterior sternoclavicular ligament. SC joint locations are thus usually directed ANTERIORLY
Posterior ligaments are much stronger to protect the contents of the mediastinum
What is joint at which shoulder separation injuries often ocur? Why is this so?
At the AC joint. This is because the AC ligament is very weak
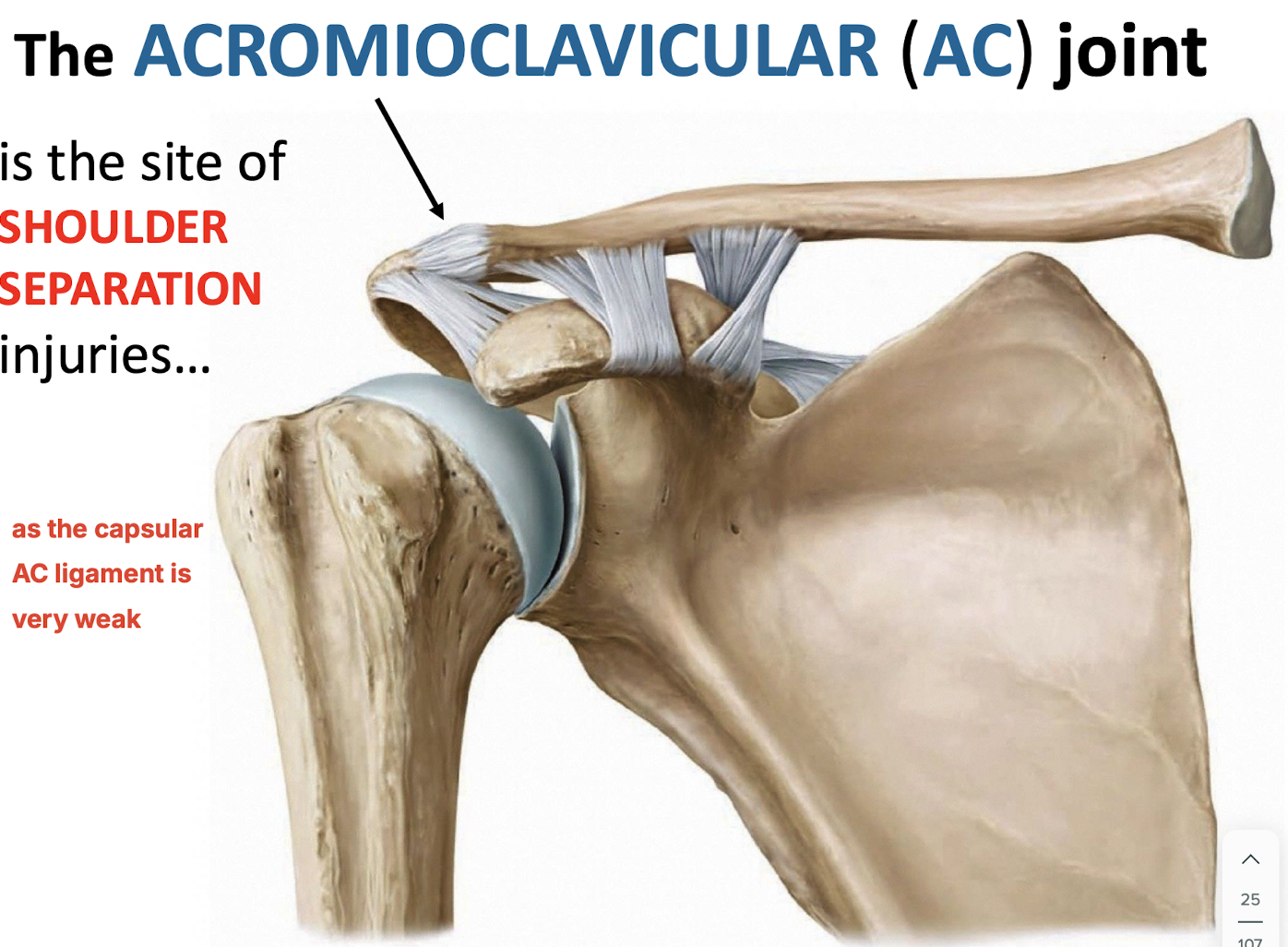
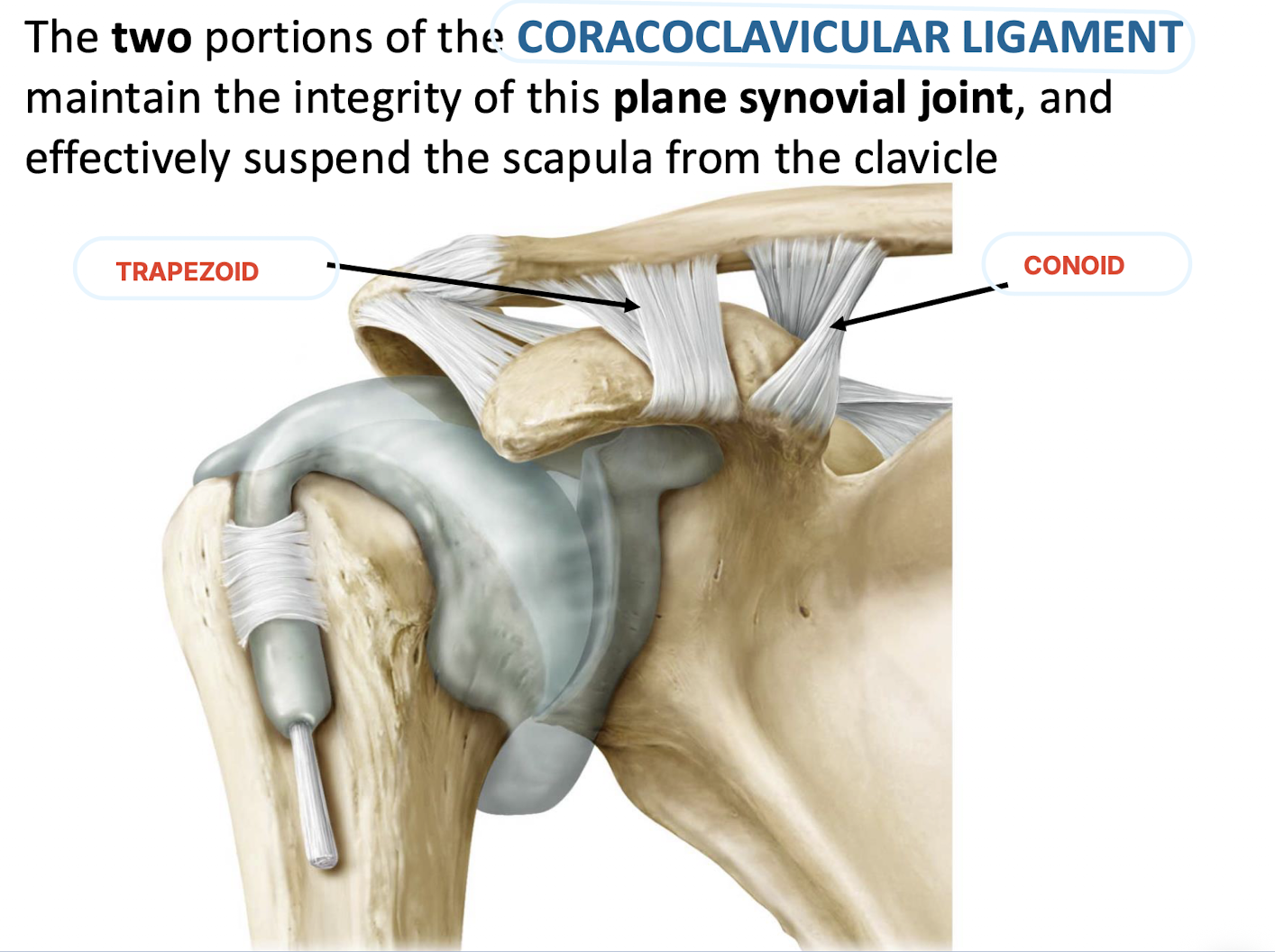
Which ligament maintains the integrity of the AC joint and effectively suspends the scapula from the clavicle?
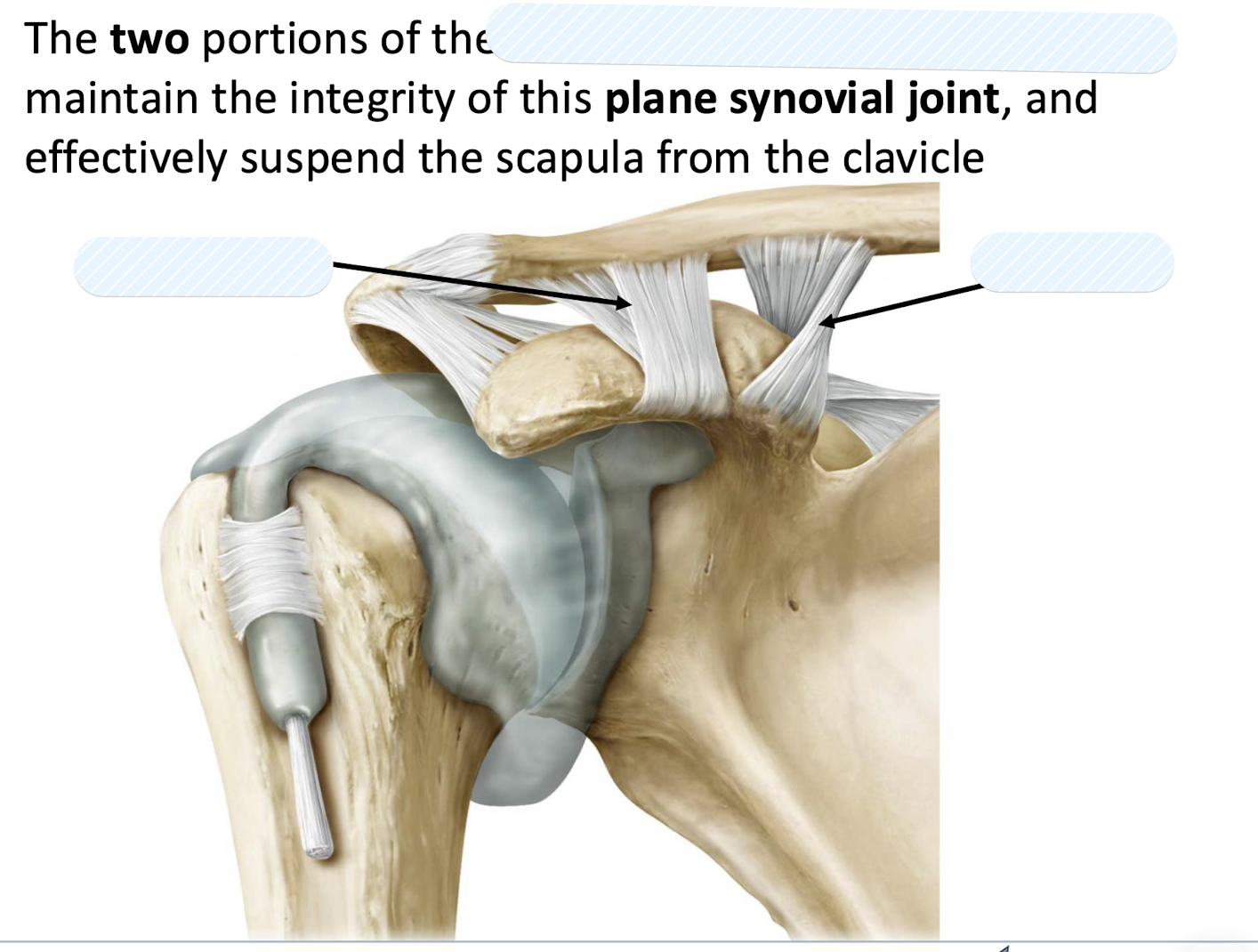
The CORACOCLAVICULAR LIGAMENT (composed of TRAPEZOID AND CONOID LIGAMENT).
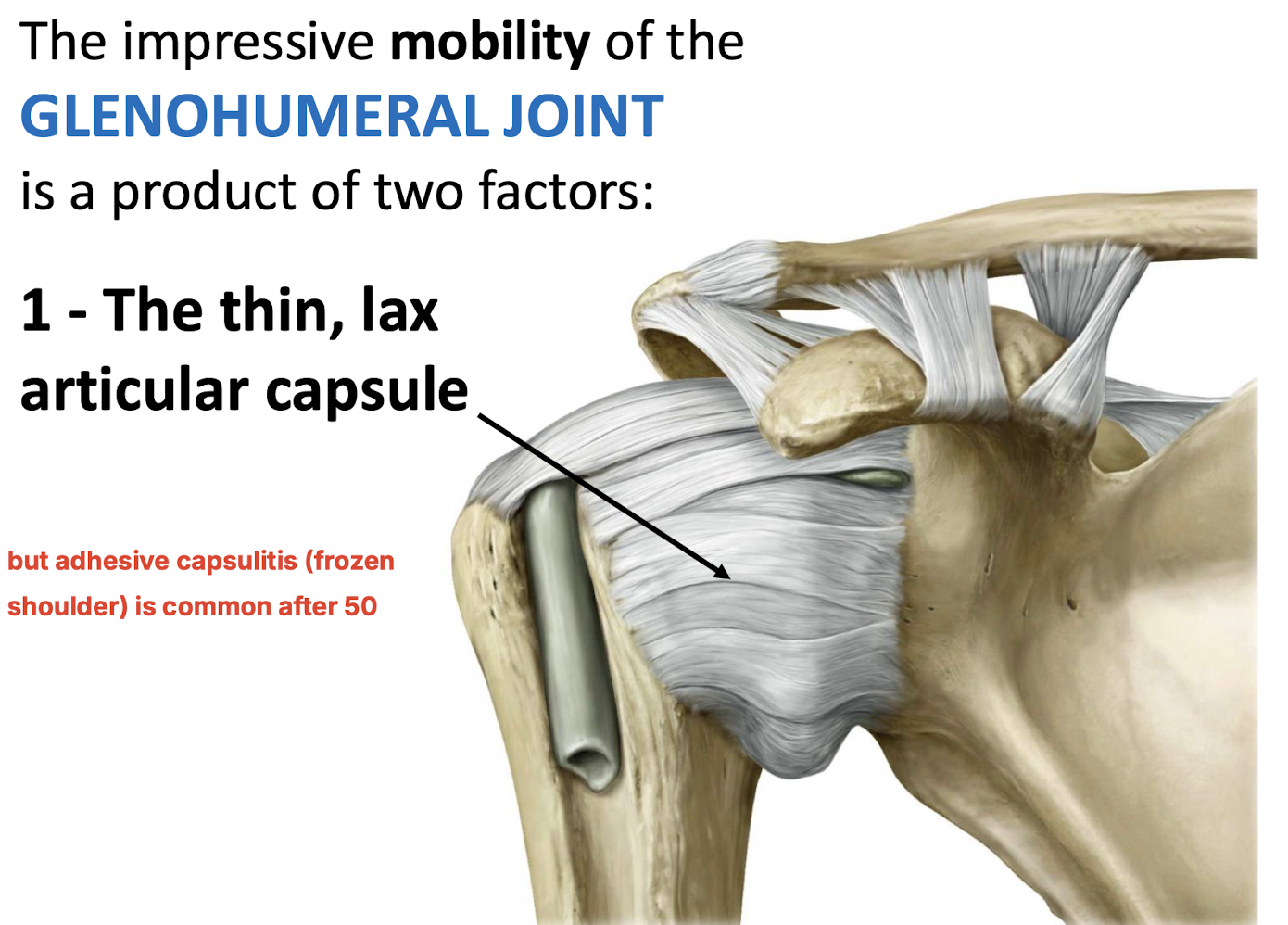
What two factors contribute to the impressive mobility, yet inherent instability, of the glenohumeral joint?
The thin, lax articular capsule and the incongruity of the bony articular surfaces.
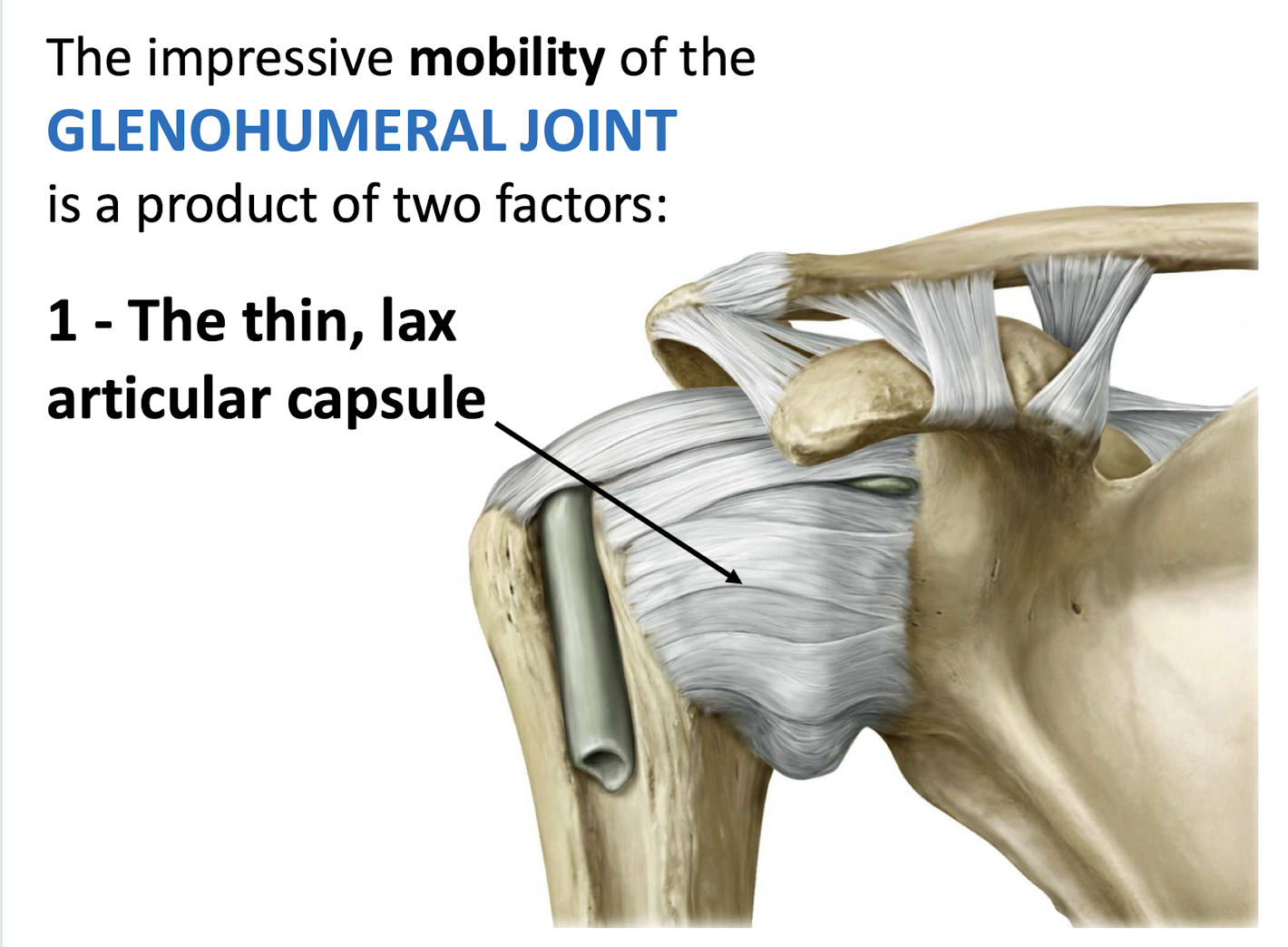
What is adhesive capsulitis and who is commonly affected?
Adhesive capsulitis (frozen shoulder) is a condition causing stiffness and pain in the shoulder joint. It is most common in adults over age 50.
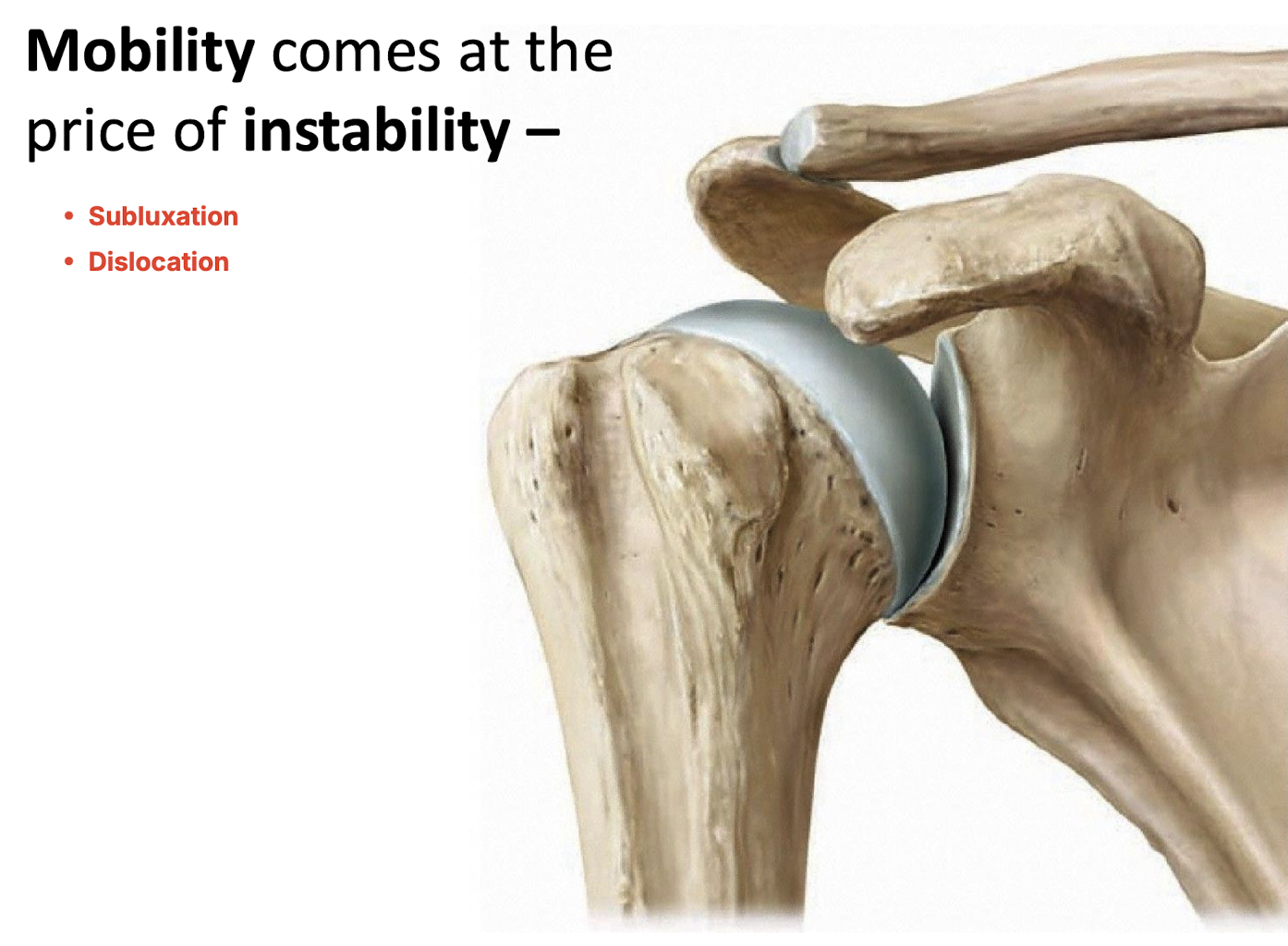
What is the consequence of the mobility of the glenohumeral joint?
Mobility brings instability such as subluxation and dislocation

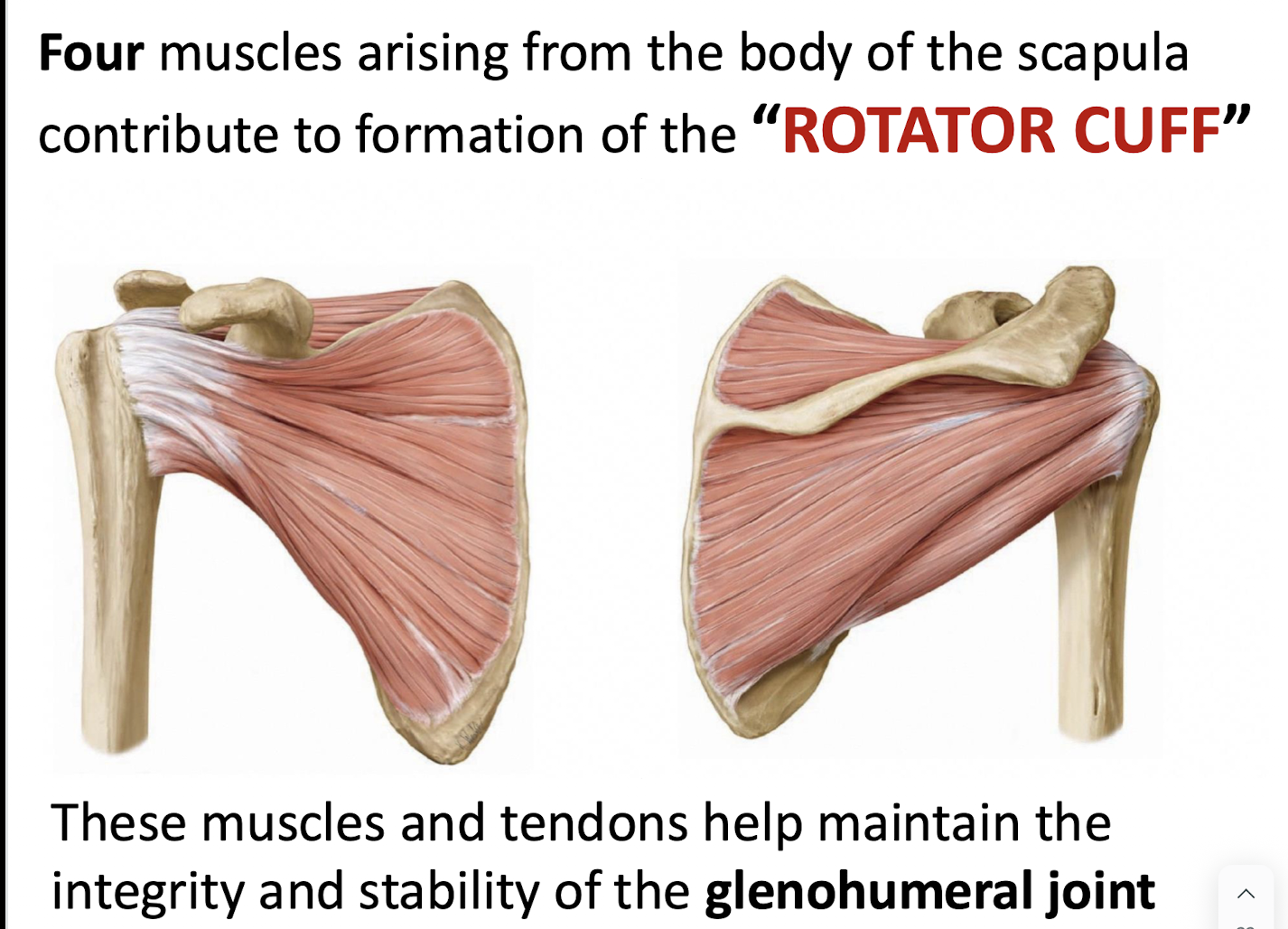
What is the primary function of the four "rotator cuff" muscles?
They help maintain the integrity of the glenohumeral joint and stabilise it during contraction of powerful thoracoappendicular muscles.
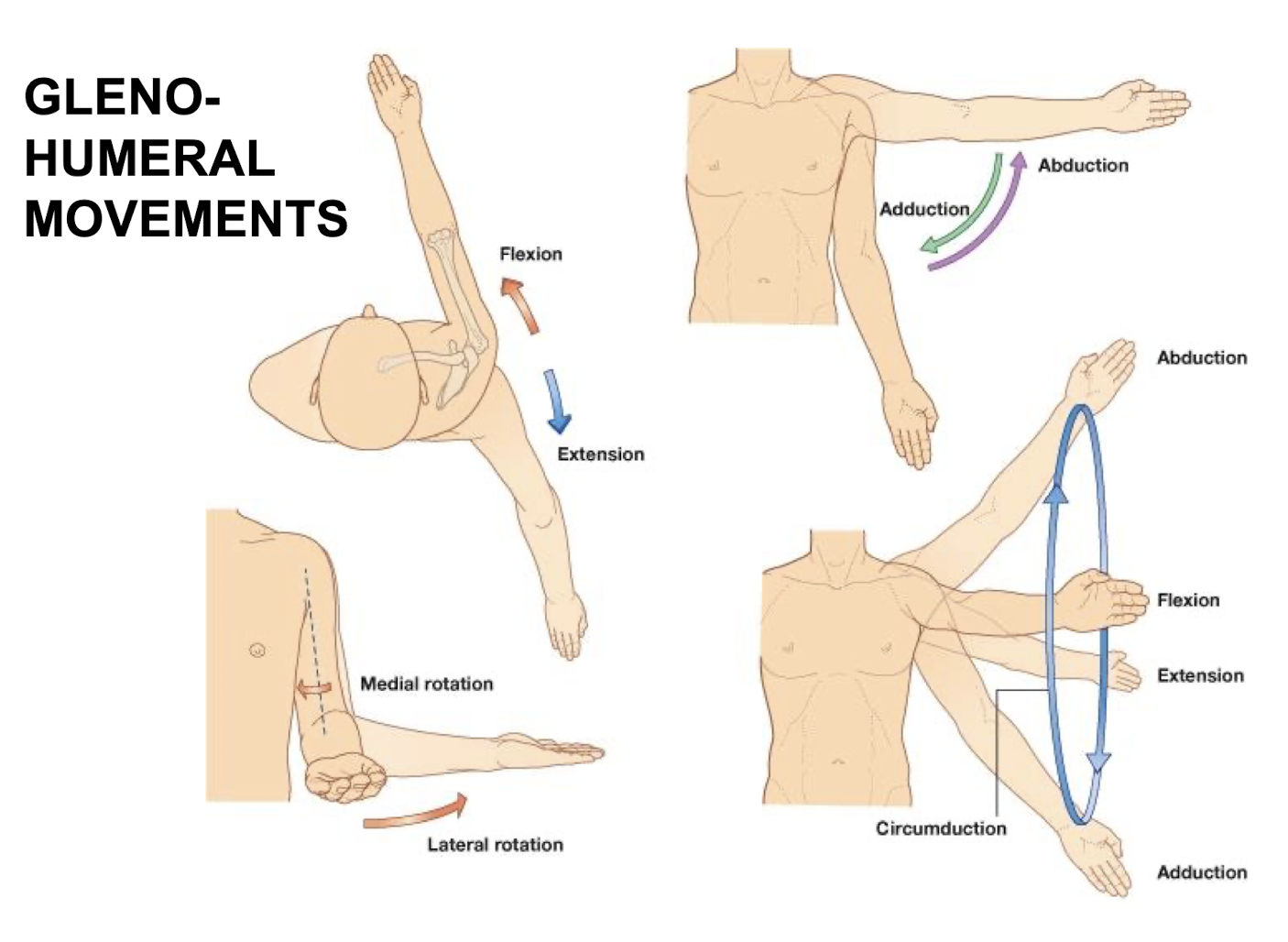
List the six types of movement possible at the glenohumeral joint.
Flexion, extension, abduction, adduction, medial/lateral rotation, and circumduction.
What is the source of virtually all nerves innervating the upper extremity?
The brachial plexus.
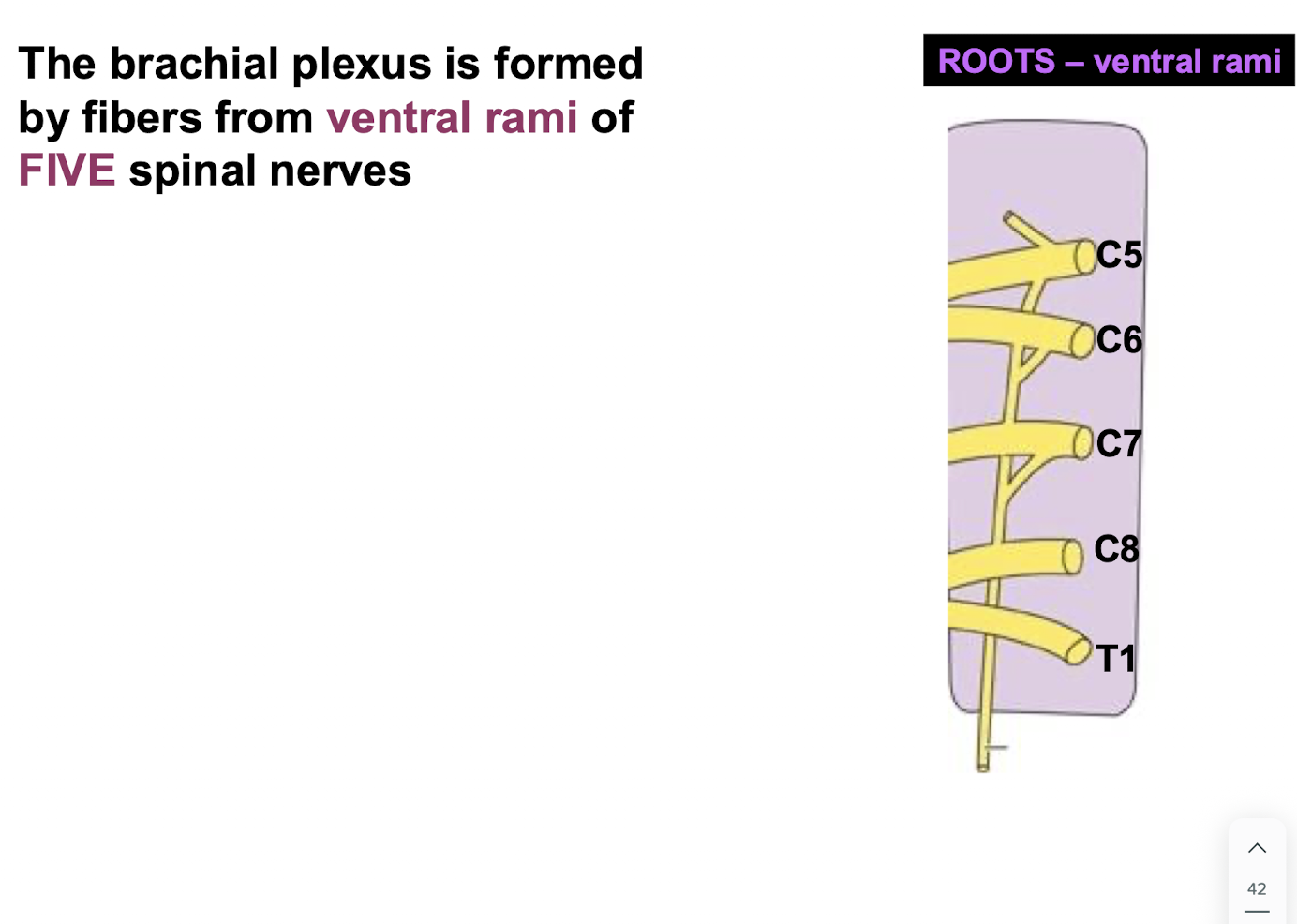
From which part of the spinal nerves does the brachial plexus arise, and what fibres do they contain?
The ventral rami, which contain both somatic afferent and somatic efferent fibres.
How many ventral rami typically contribute to a named peripheral nerve of the plexus?
At least two adjacent ventral rami of lower cervical or upper thoracic spinal nerves
What is the larger of the two branches arising from each spinal nerve?
ventral rami
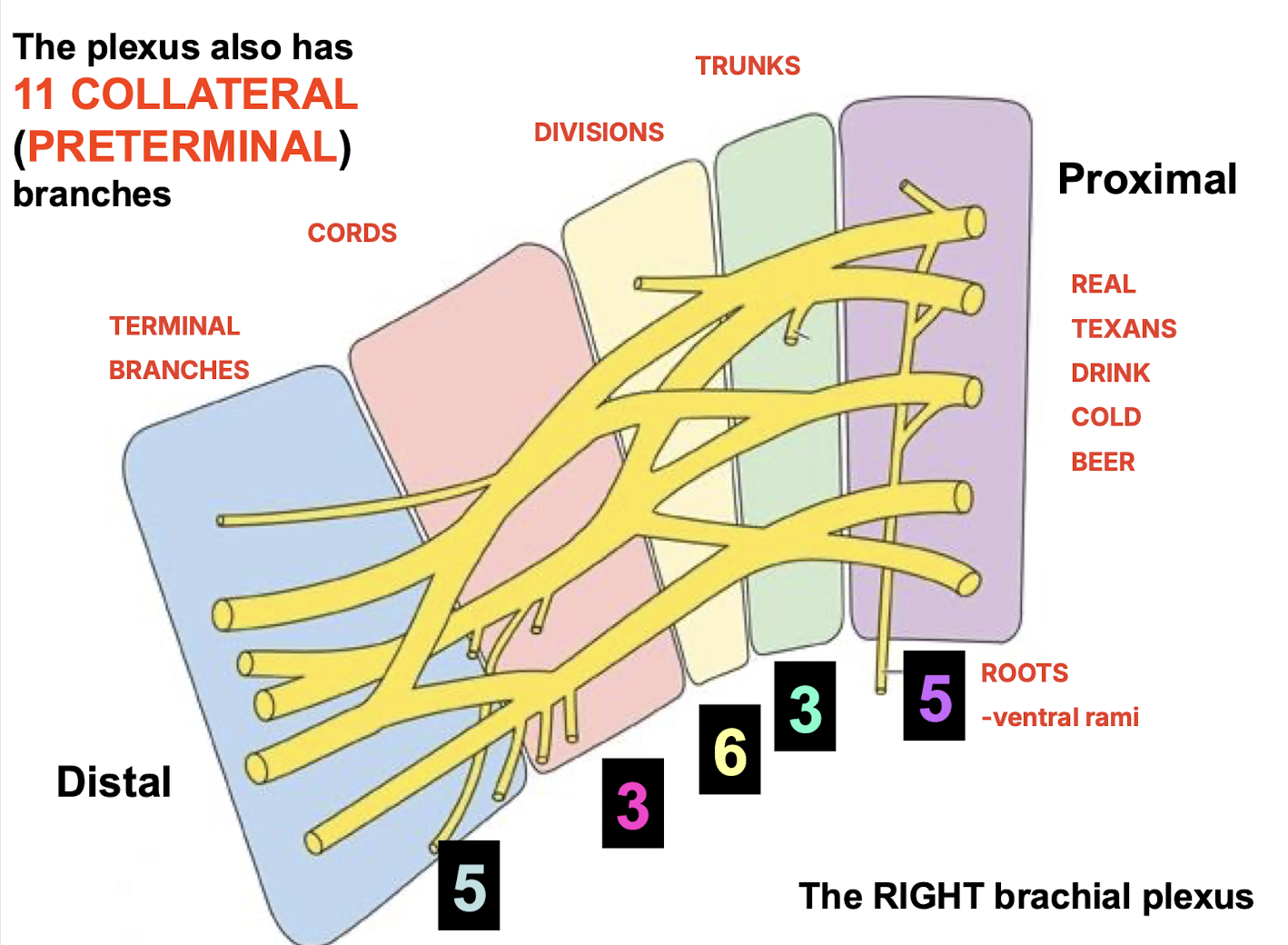
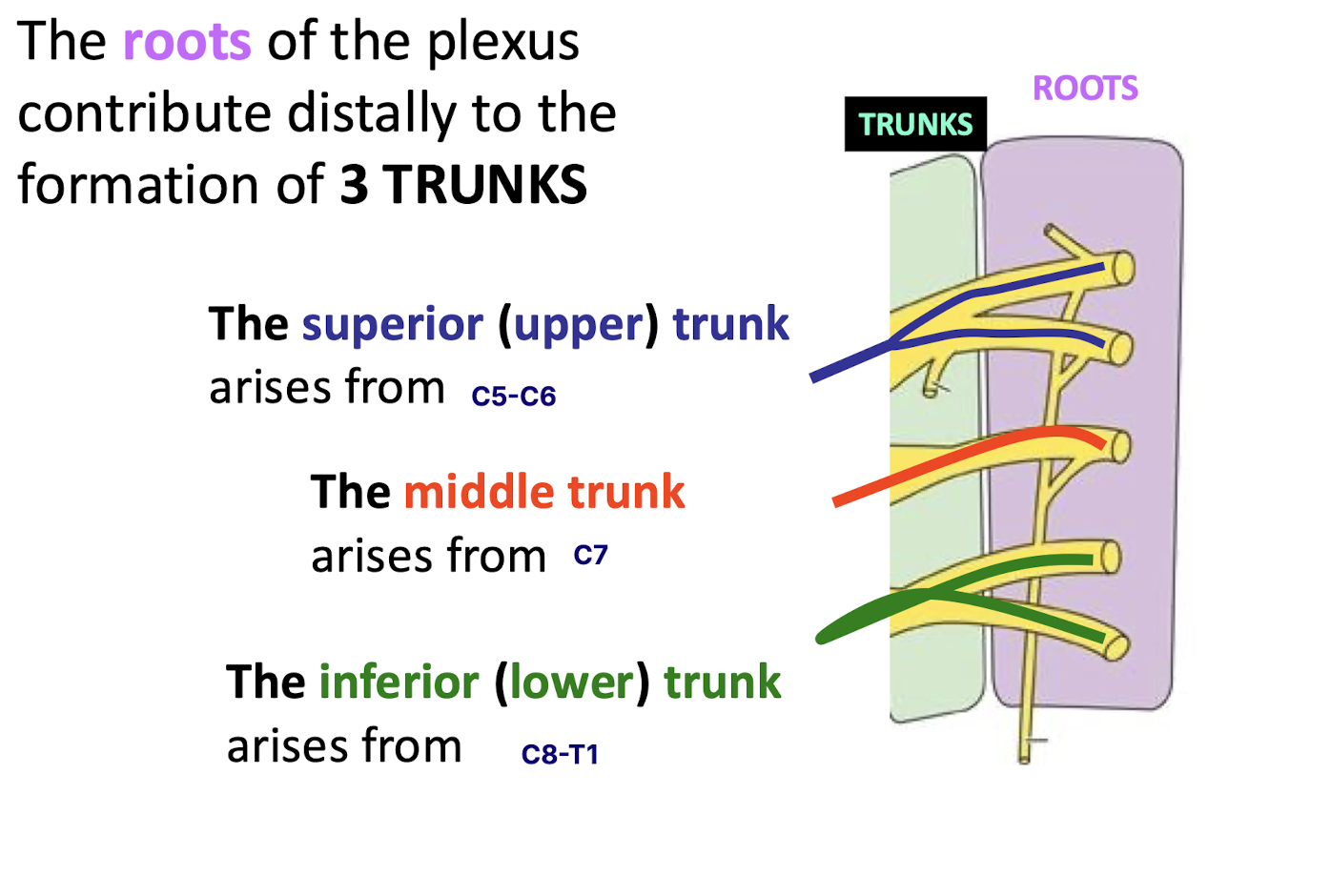
List the five parts of the brachial plexus from proximal to distal. How many of each part is there?
5 Roots, 3 Trunks, 6 Divisions, 3 Cords, and 5 Terminal Branches.
REAL
TEXANS
DRINK
COLD
BEER
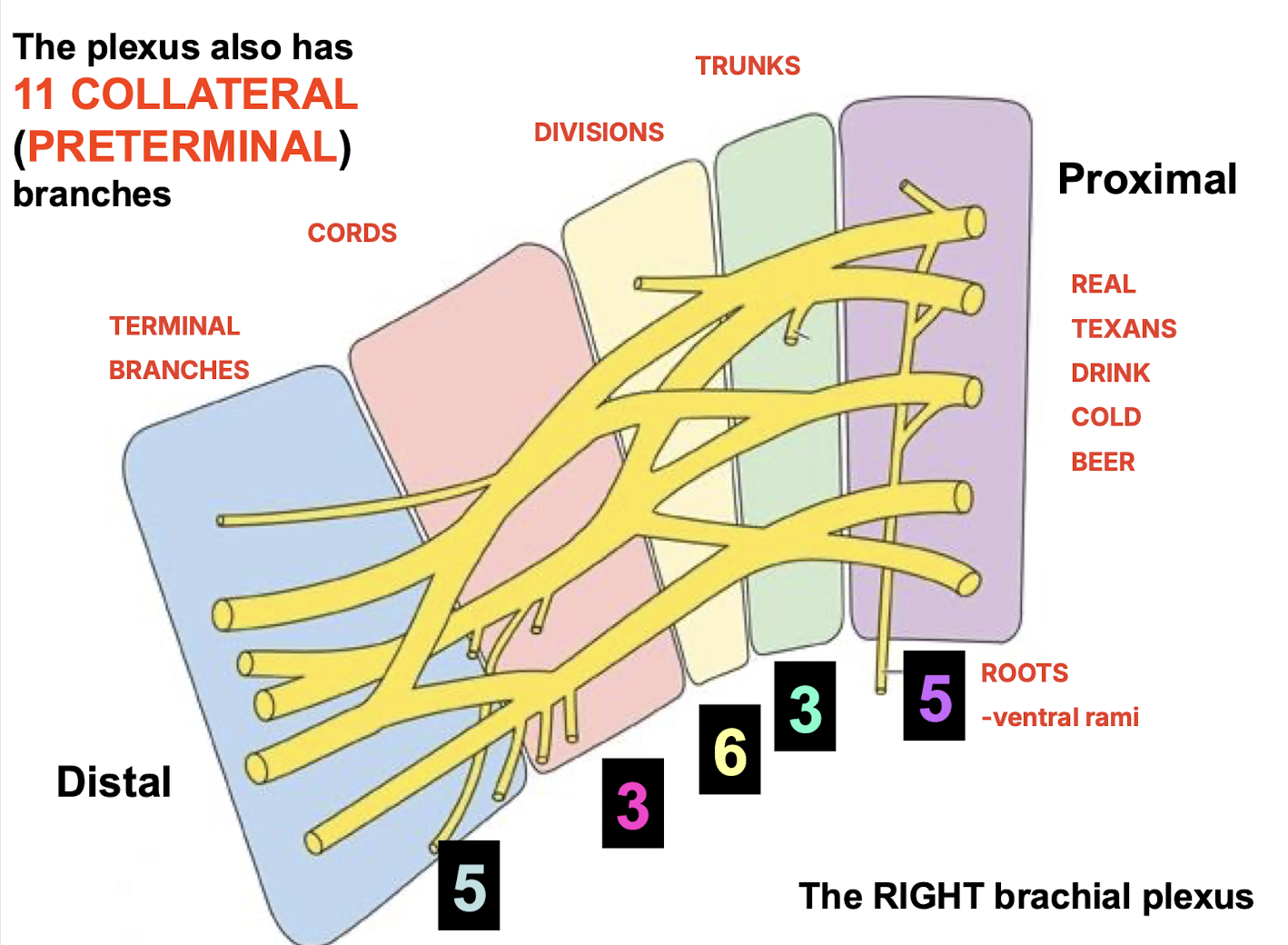
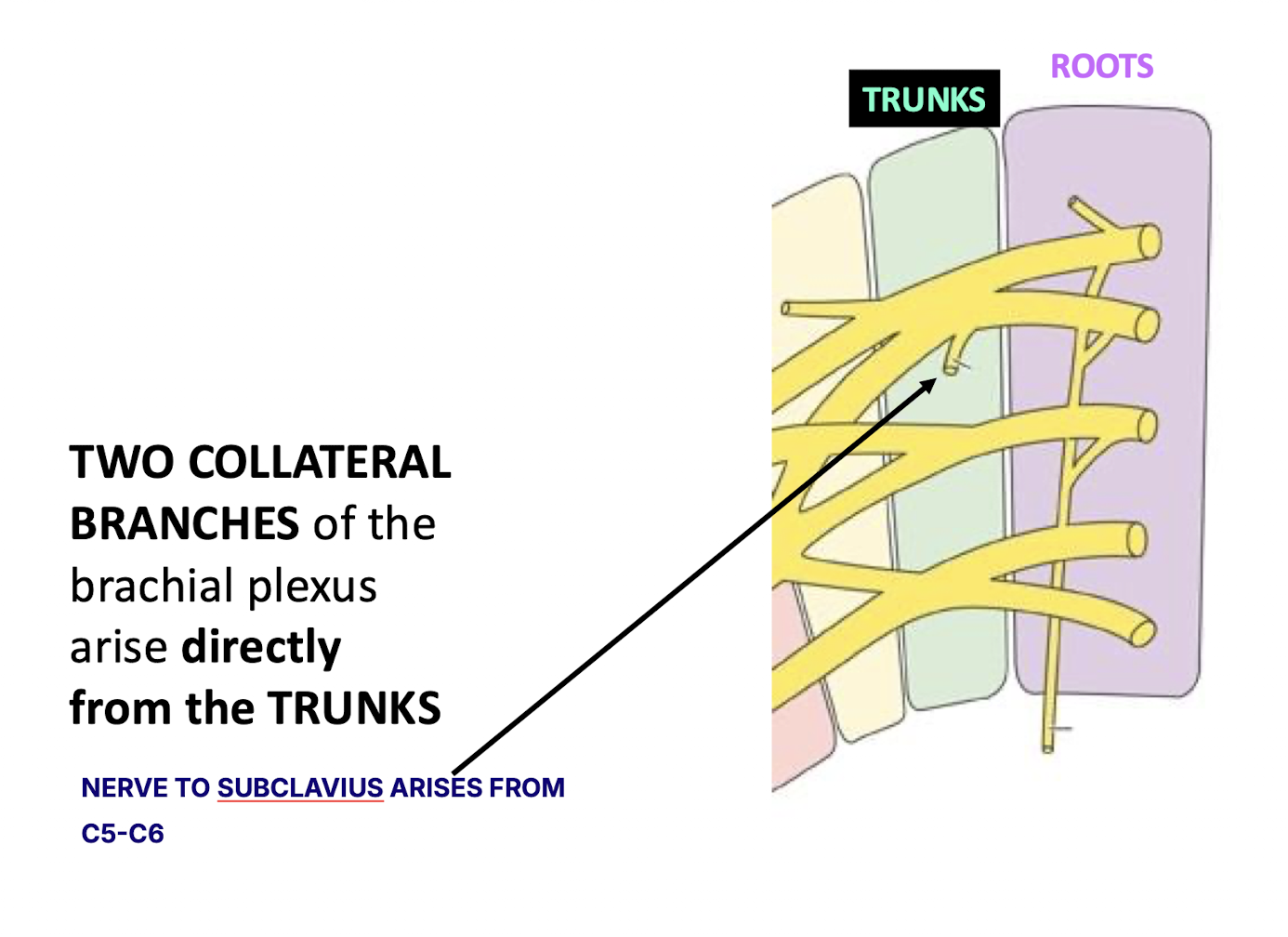
How many collateral (preterminal) branches does the plexus have?
The plexus has 11 collateral (preterminal) branches.
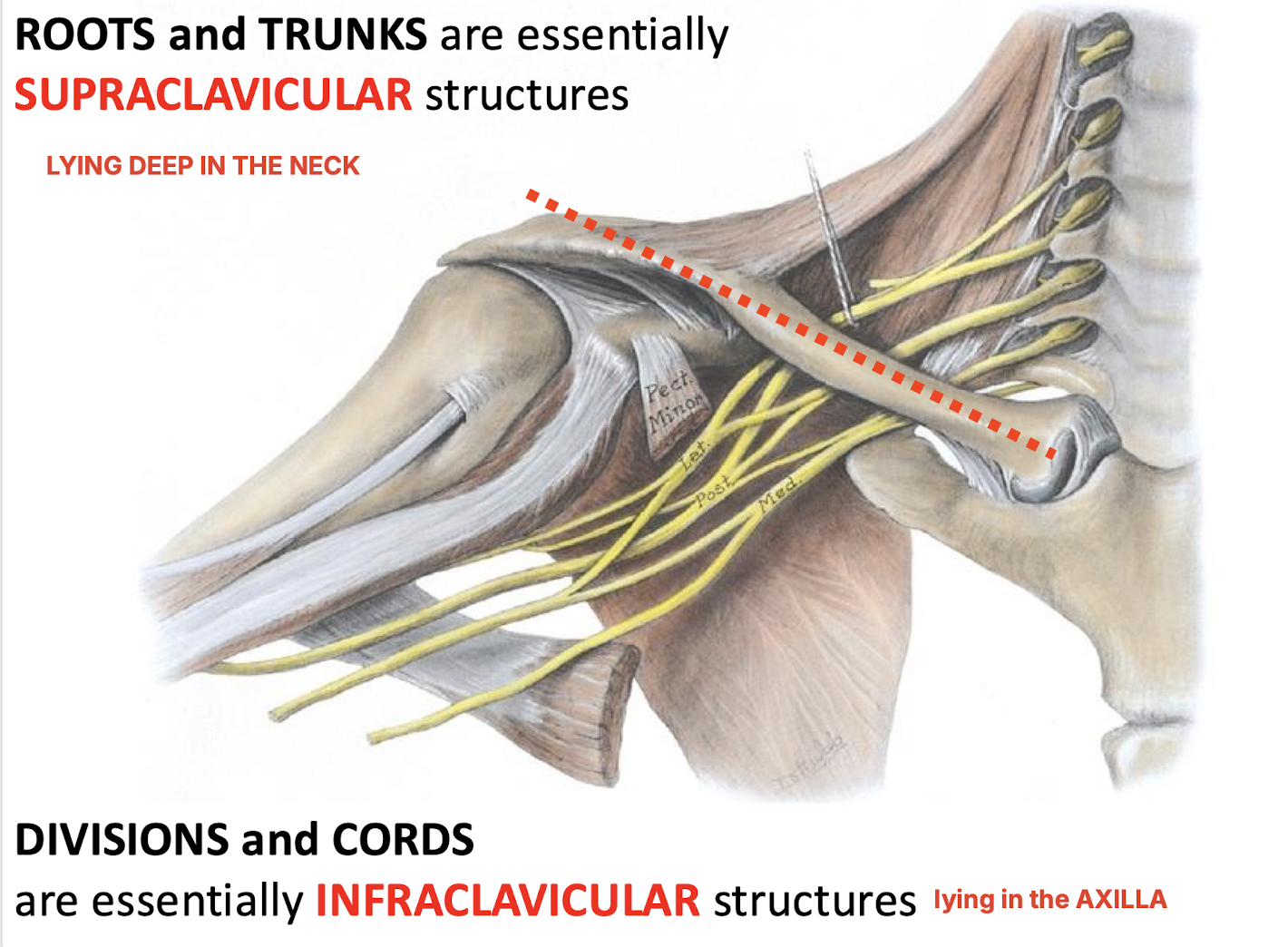
Topographically, which parts of the brachial plexus are considered supraclavicular AND where are they found? What is considered infraclavicular?
The roots and trunks lying deep in the neck
DIVISIONS and CORDS are essentially INFRACLAVICULAR structures lying in the AXILLA
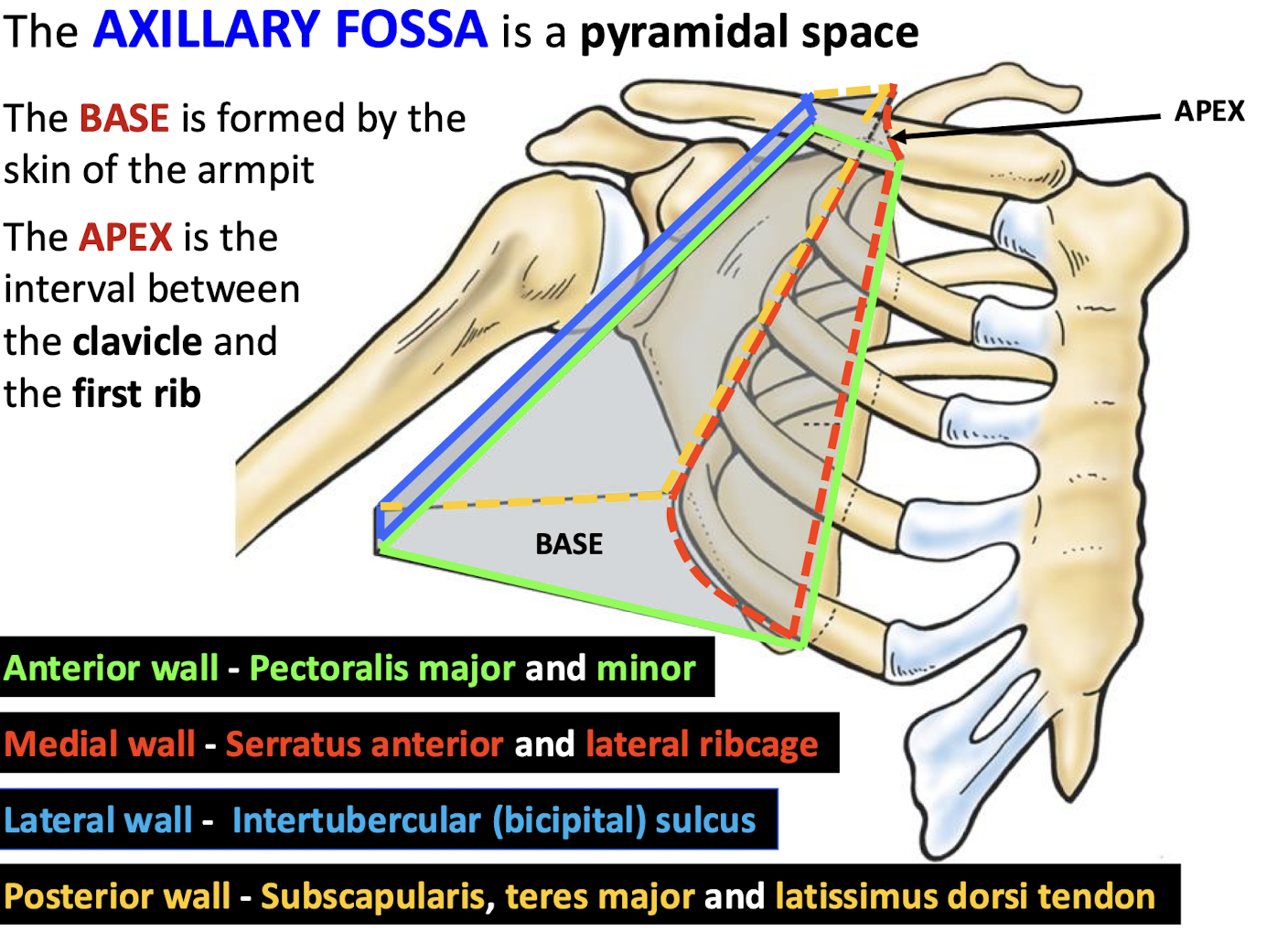
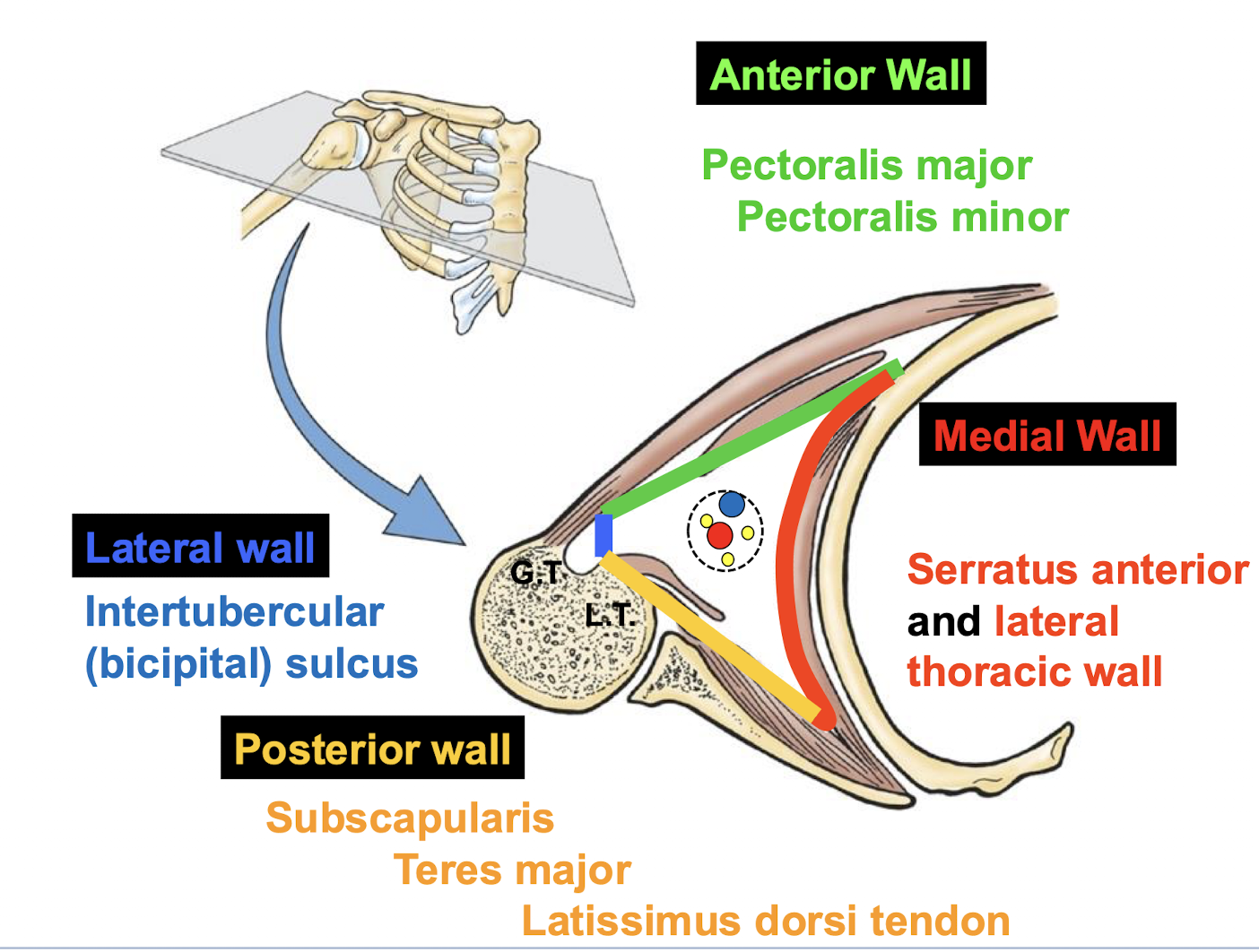
Which walls (anterior, medial, lateral, psterior) form the pyramidal axillary fossa?
Anterior (pectoralis major and minor), Medial (serratus anterior/lateral ribcage), Lateral (intertubercular sulcus), and Posterior (subscapularis, teres major, latissimus dorsi tendon).
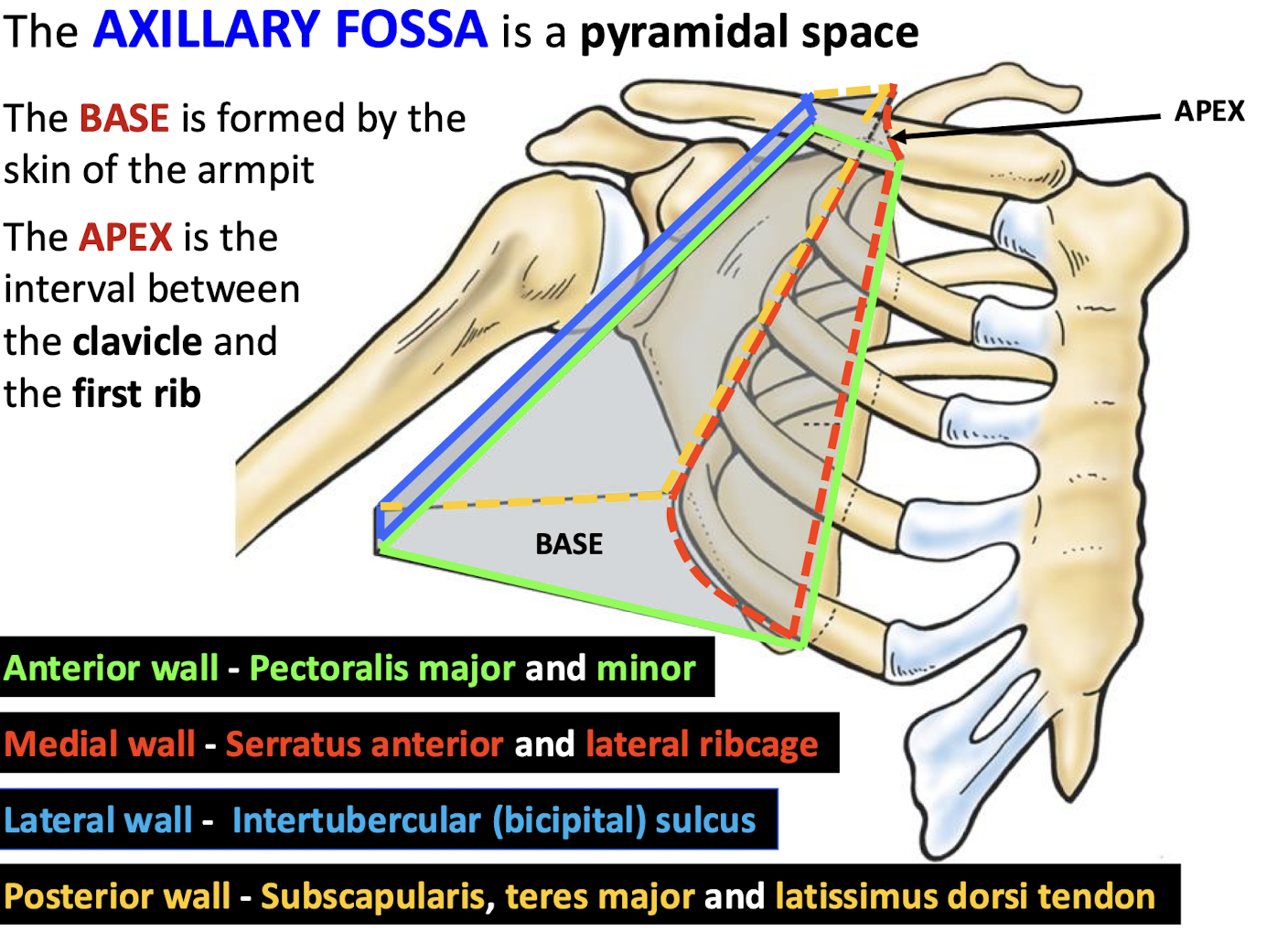
What defines the apex and base of the axillary fossa?
The apex is the interval between the clavicle and first rib; the base is the skin of the armpit.
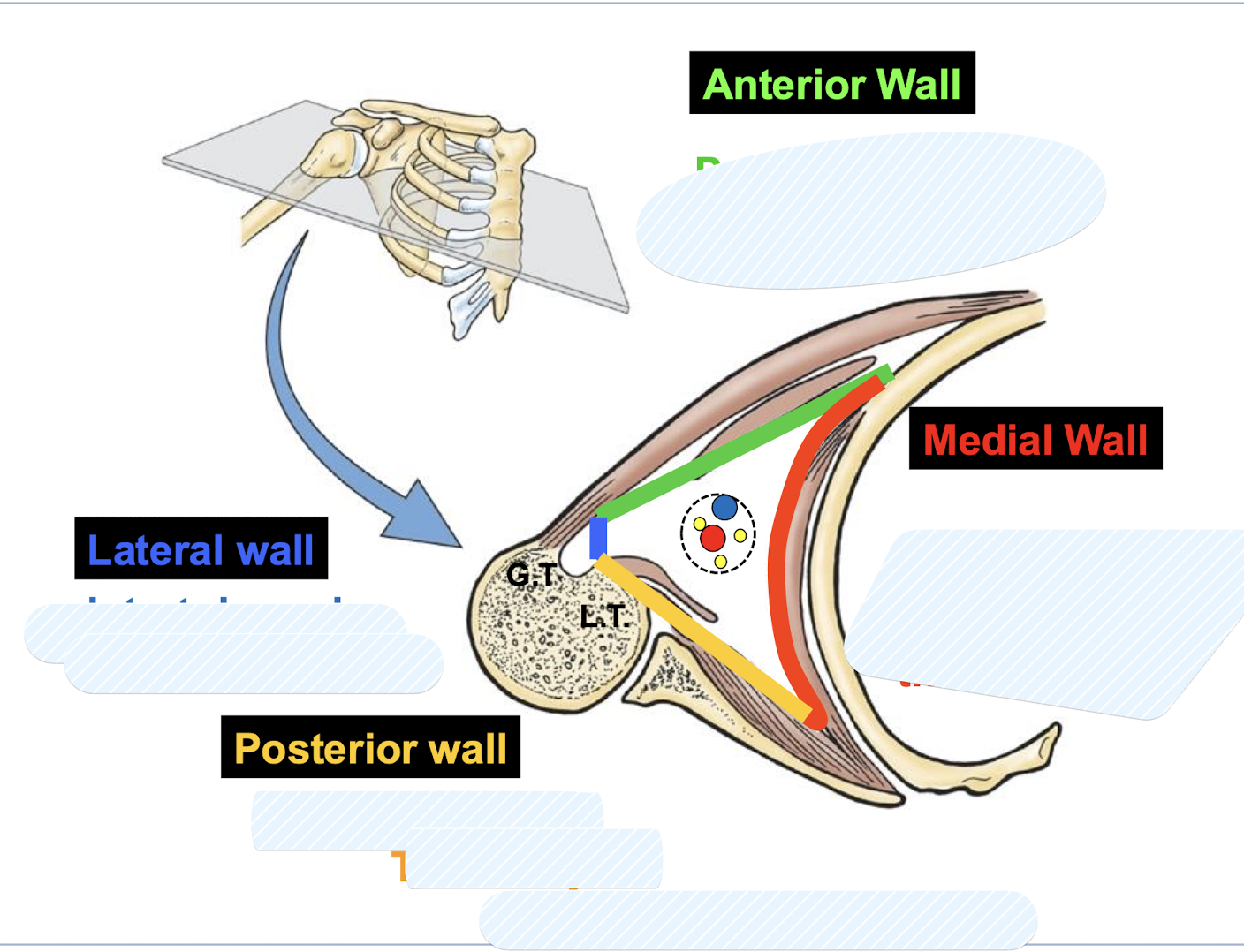
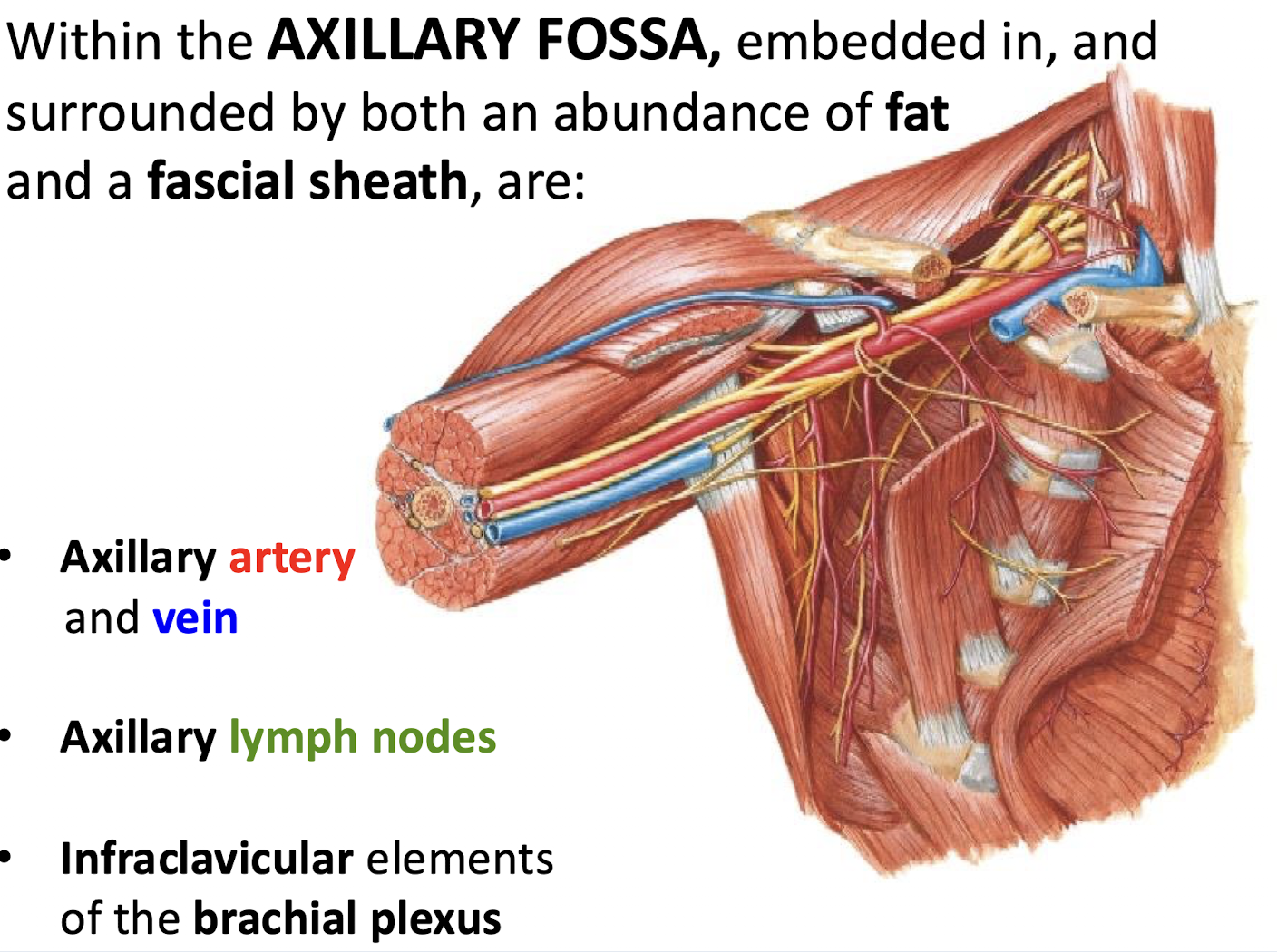
What are the primary contents of the axillary fossa?
The axillary artery and vein, axillary lymph nodes, and infraclavicular elements of the brachial plexus.
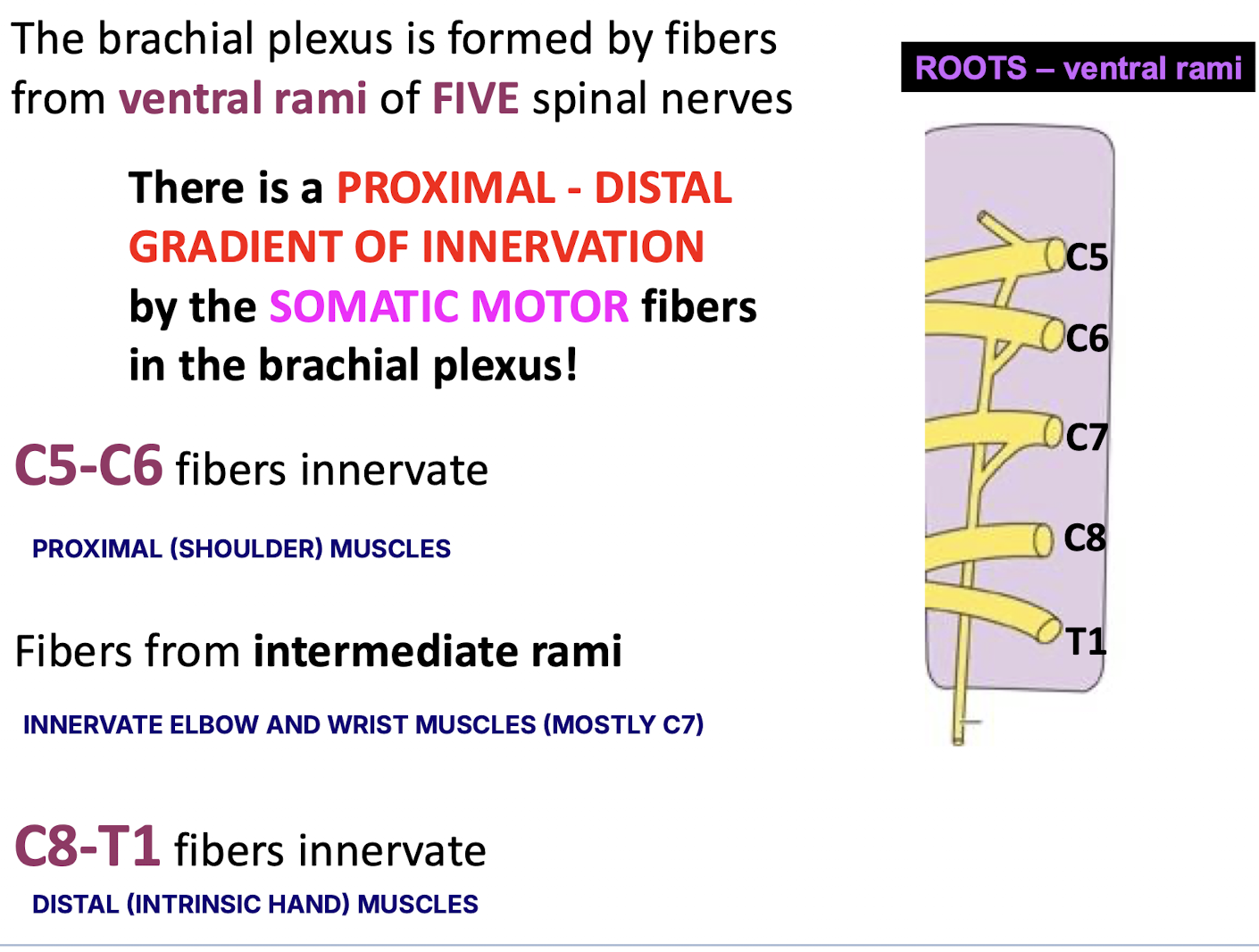
Which spinal nerves form the roots of the brachial plexus?
Ventral rami of C5, C6, C7, C8, and T1.
Why does the brachial plexus span C5–T1?
Because the upper limbs develop as buds from the venterolateral body wall adjacent to the caudal cervical and upper thoracic segments of the embryo (somites) toward the end of the 4th week of development.
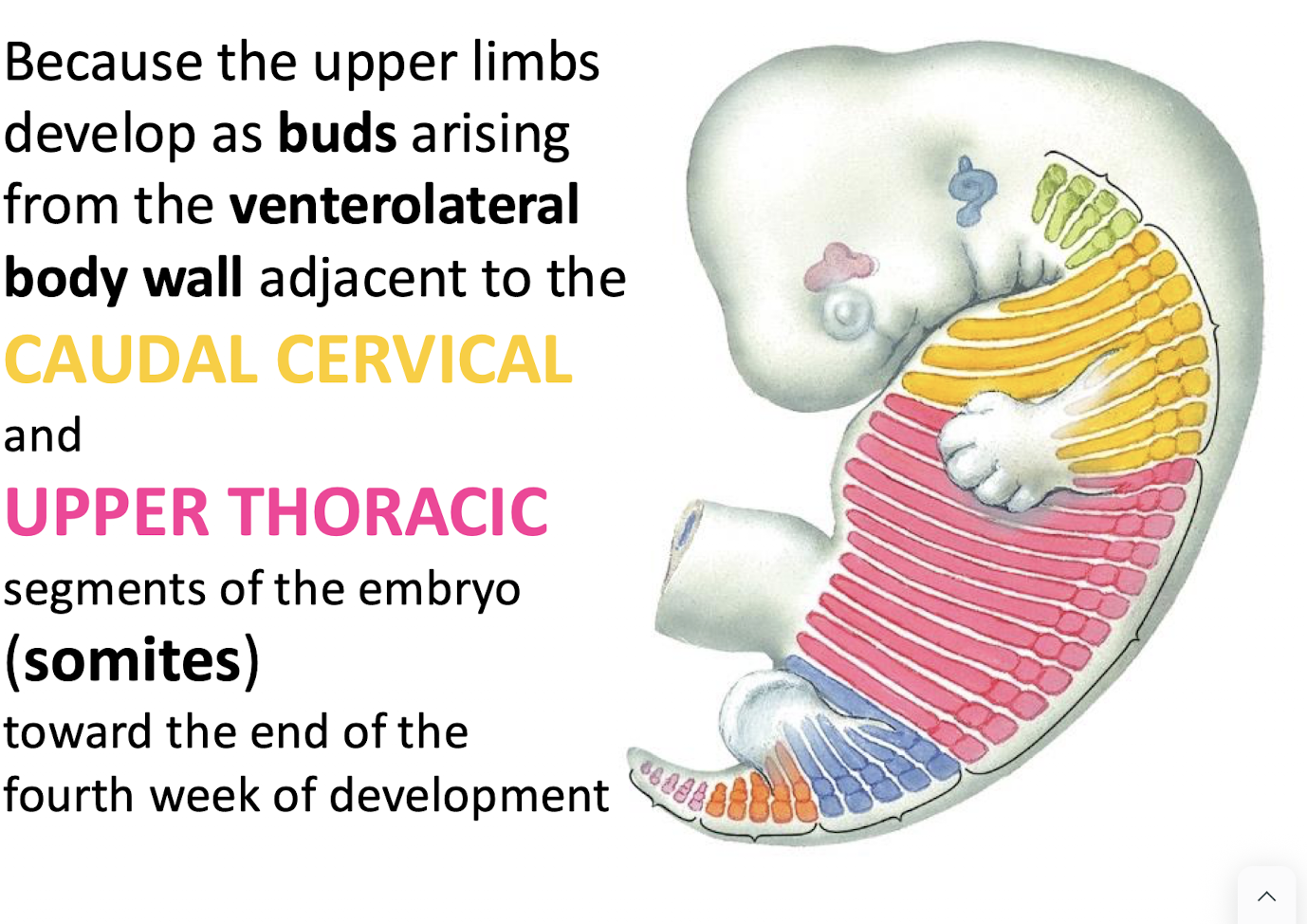
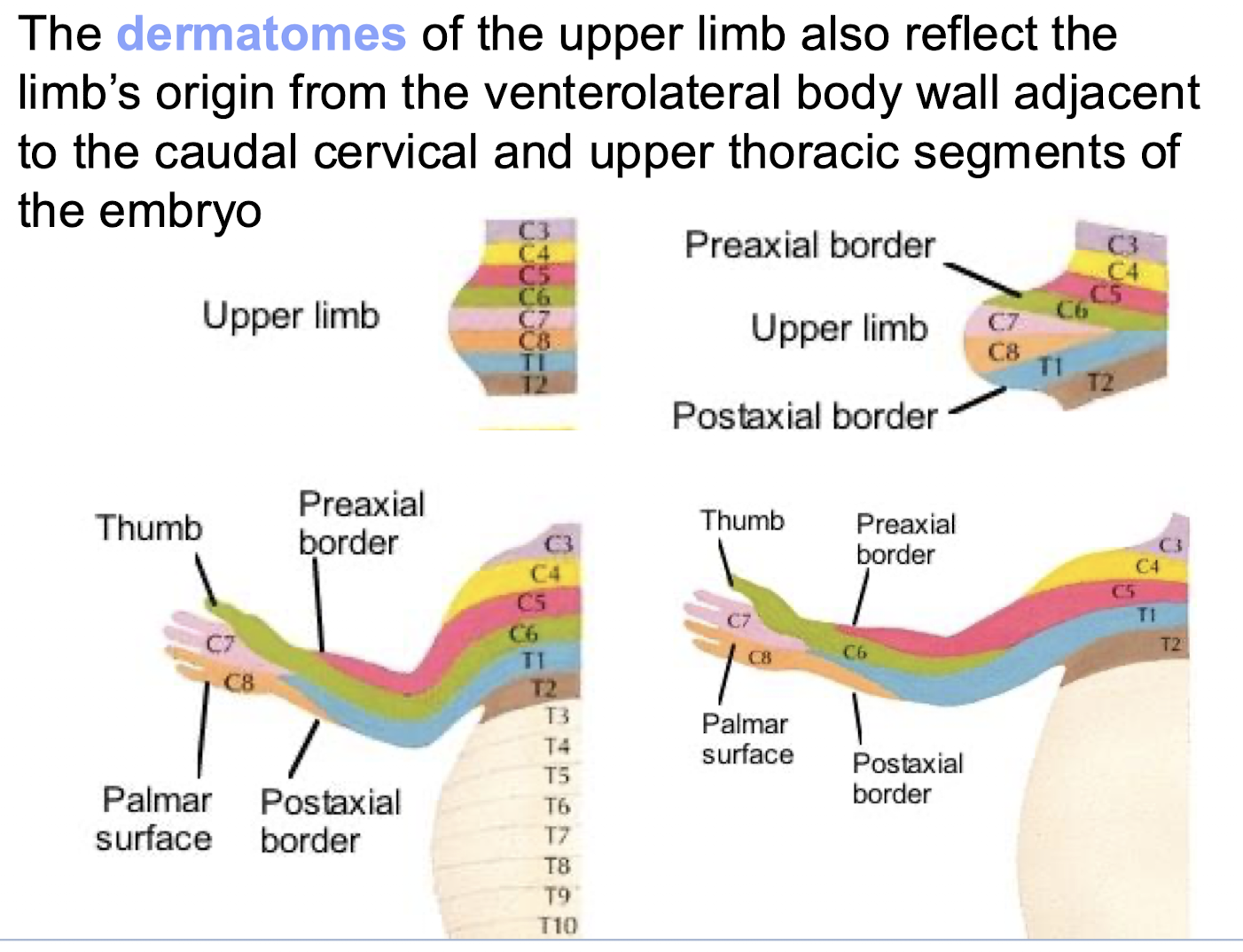
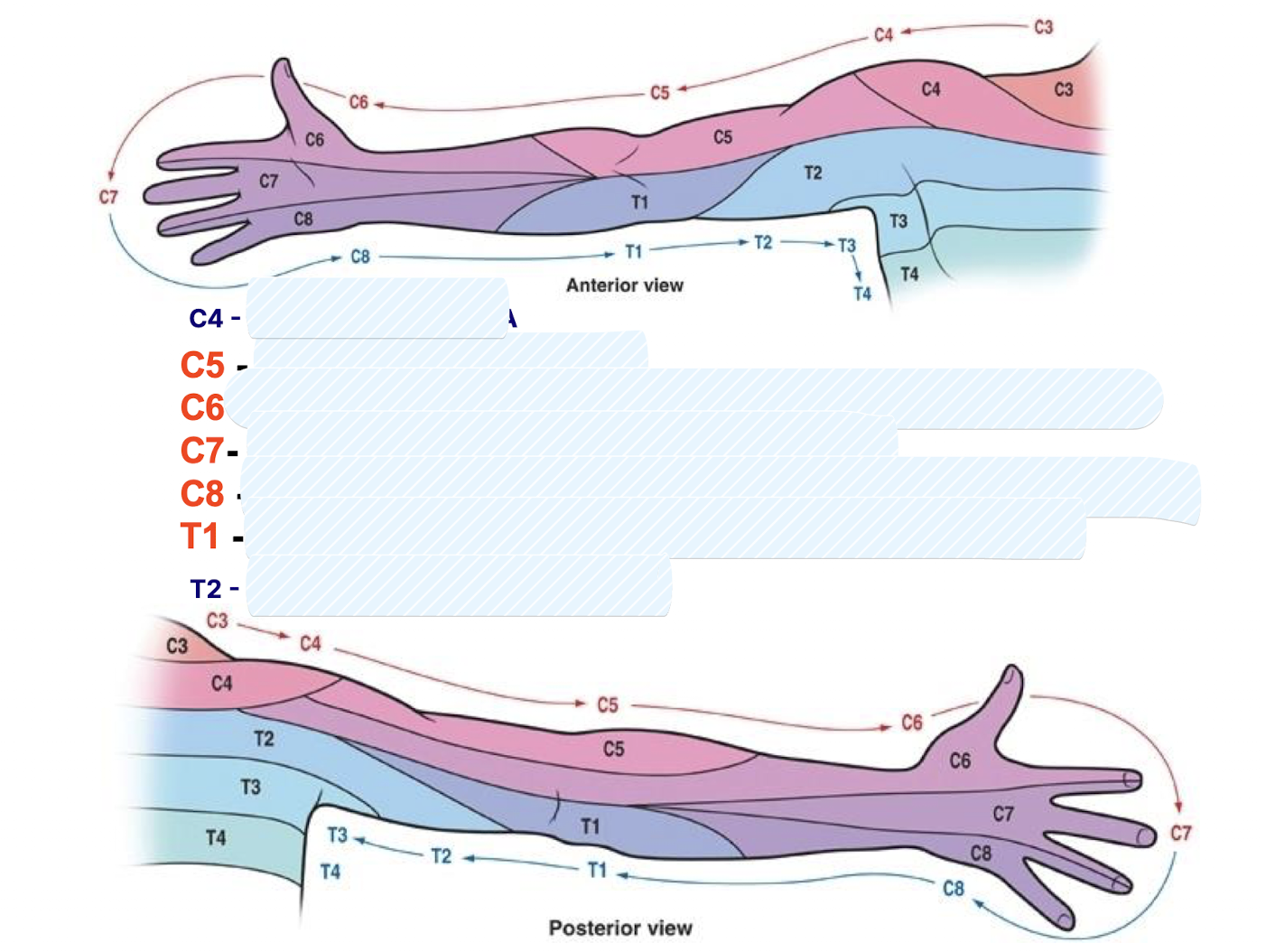
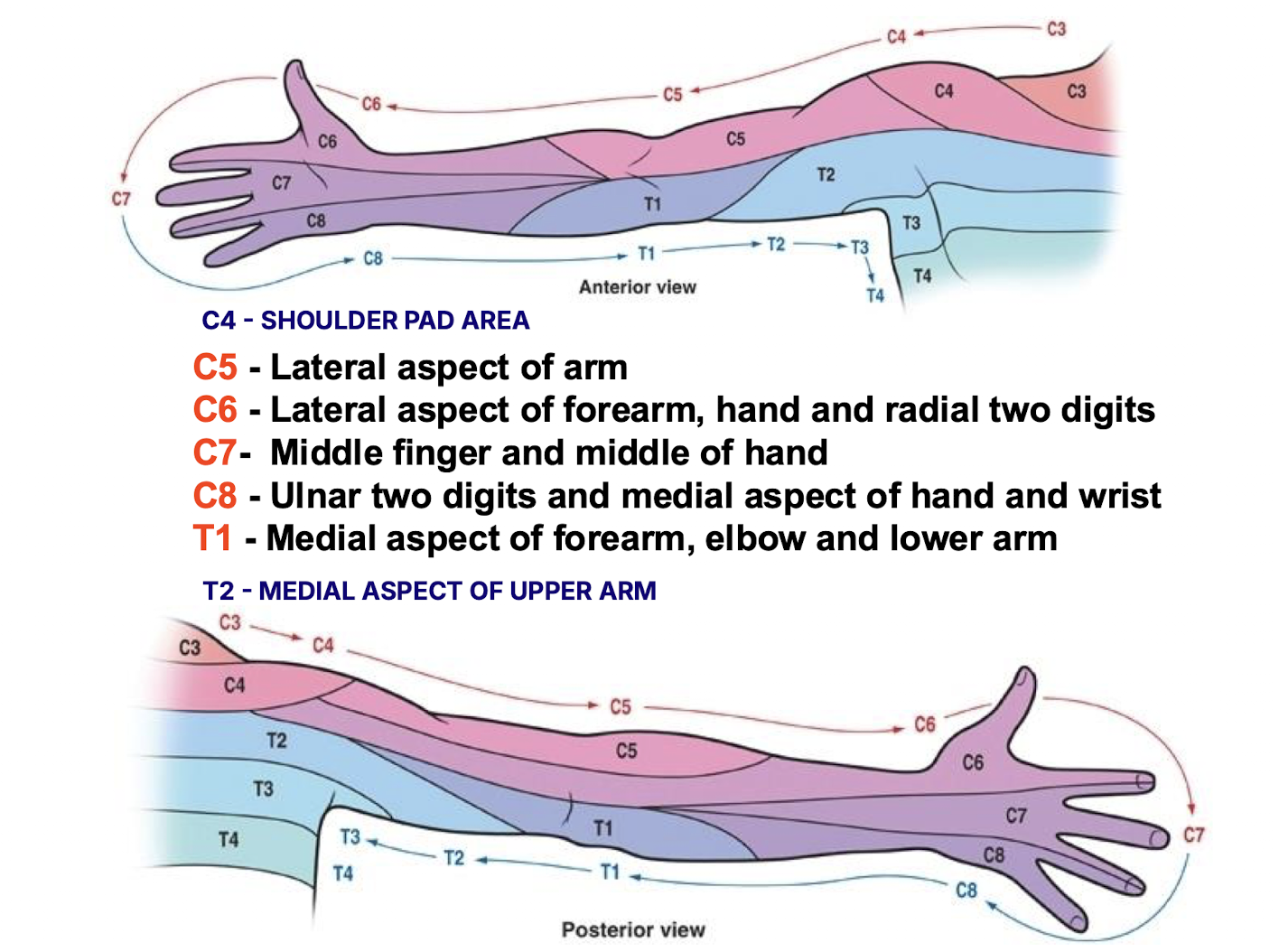
Why do the dermatomes of the upper limb follow the C5–T1 pattern?
Because the upper limb originates from the venterolateral body wall adjacent to the caudal cervical and upper thoracic segments of the embryo, which is reflected in the dermatome distribution.
Identify the dermatomes for the following
What is the proximal-distal motor innervation gradient in SOMATIC MOTOR fibers of the brachial plexus?
C5-C6 fibres innervate proximal (SHOULDER) muscles; intermediate rami innervate elbow and wrist muscles; C8-T1 fibres innervate distal (intrinsic hand) muscles.
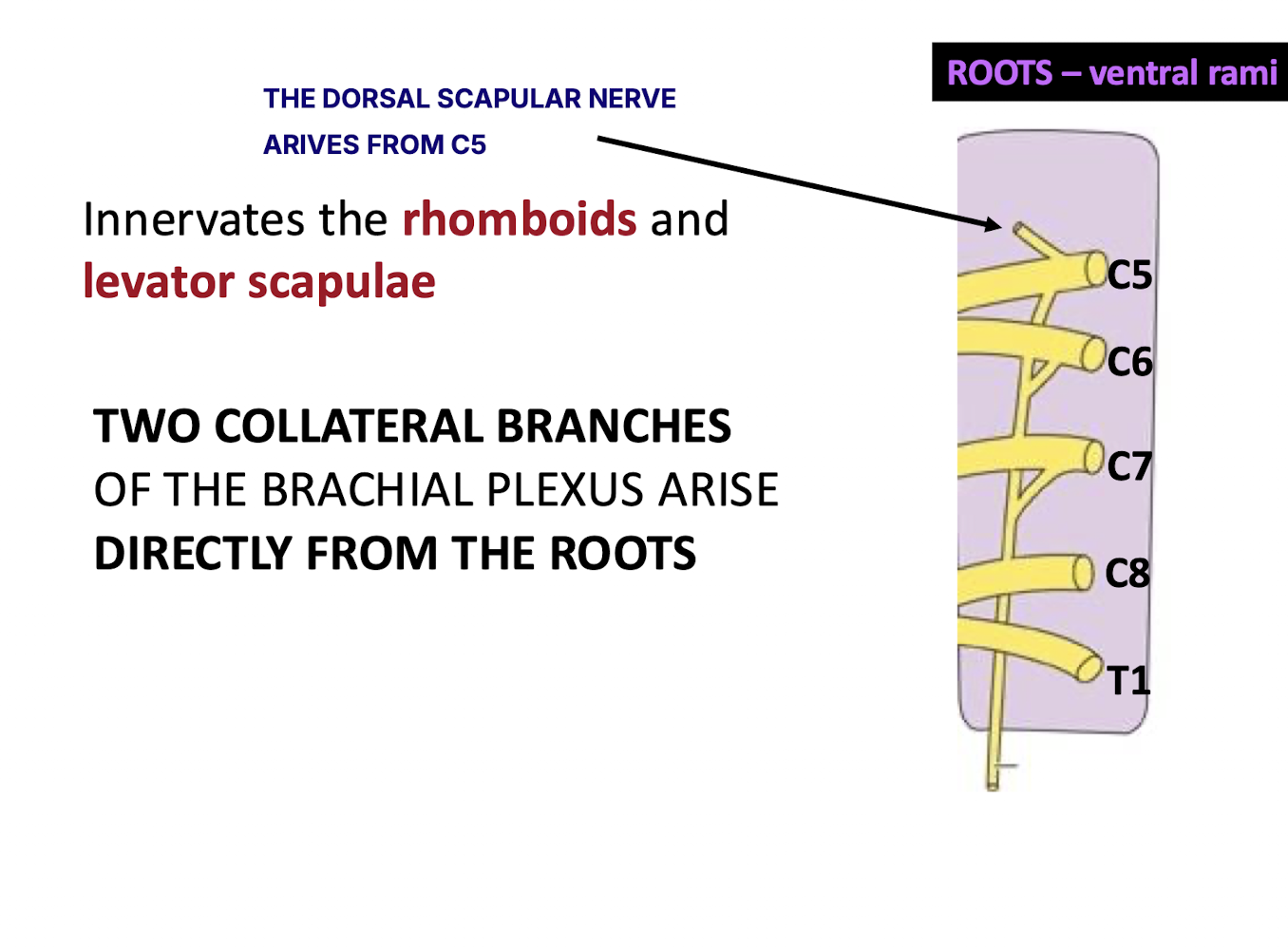
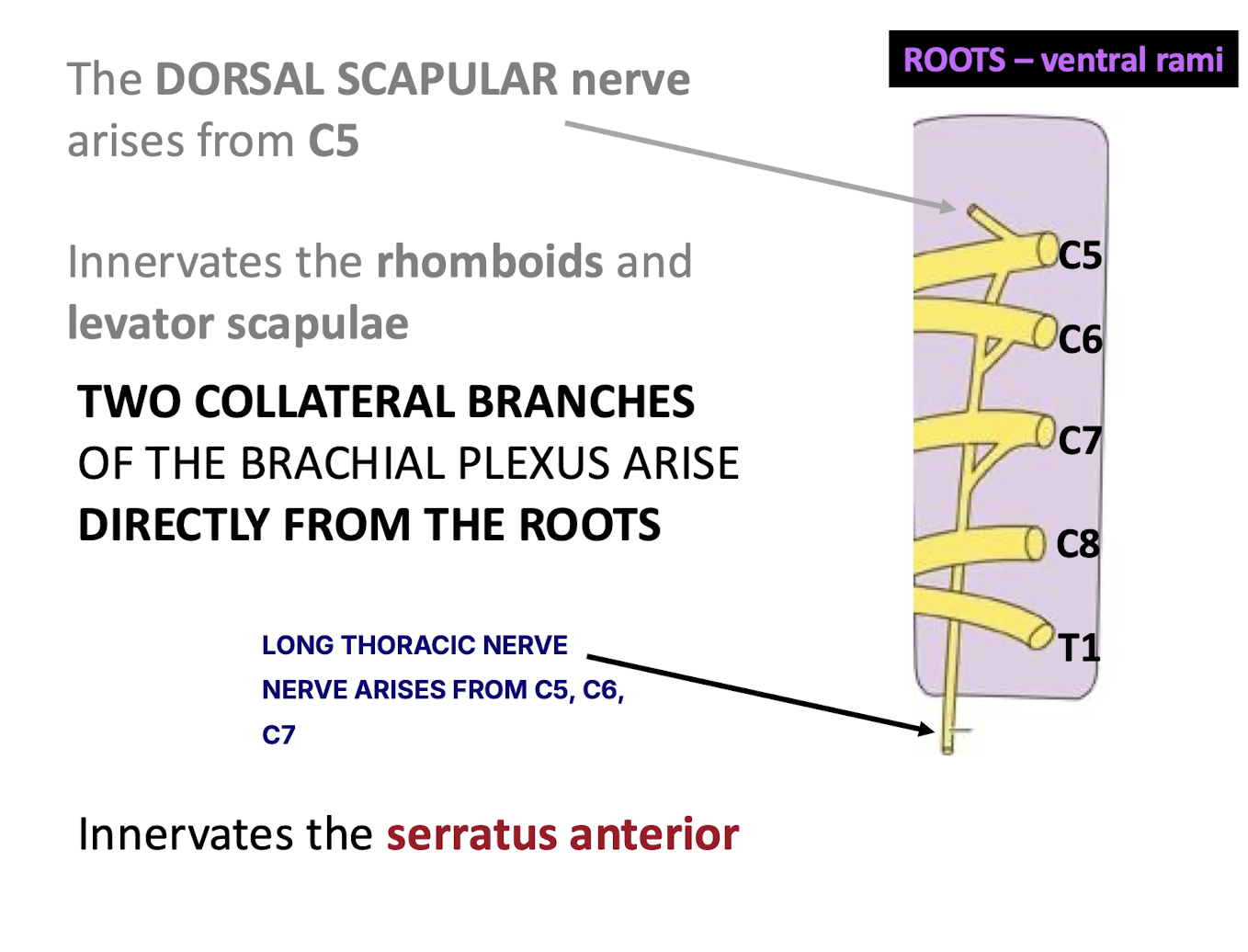
Which two collateral branches arise directly from the roots of the brachial plexus? What nerves do these come from?
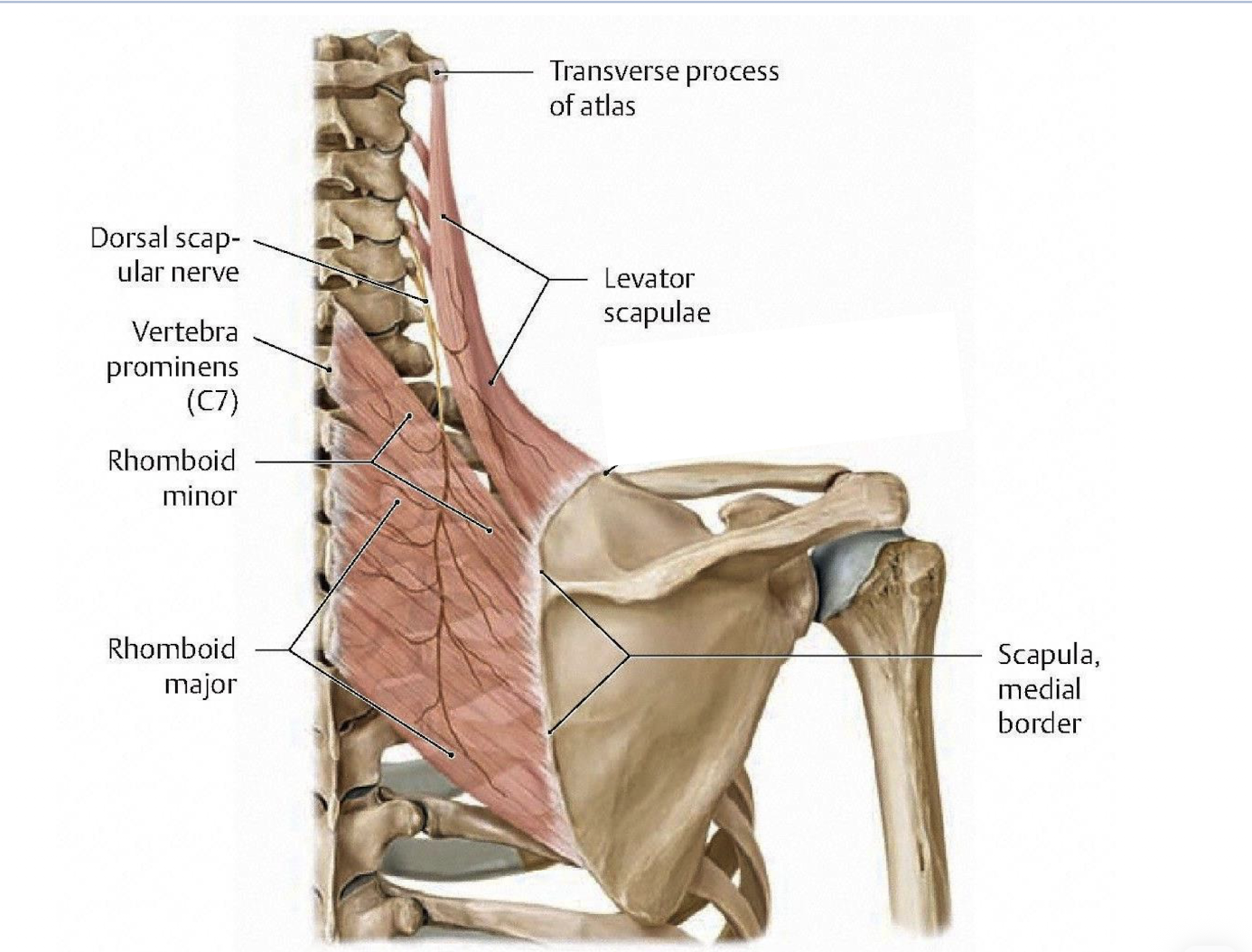
The dorsal scapular nerve (C5) and the long thoracic nerve (C5-C7).
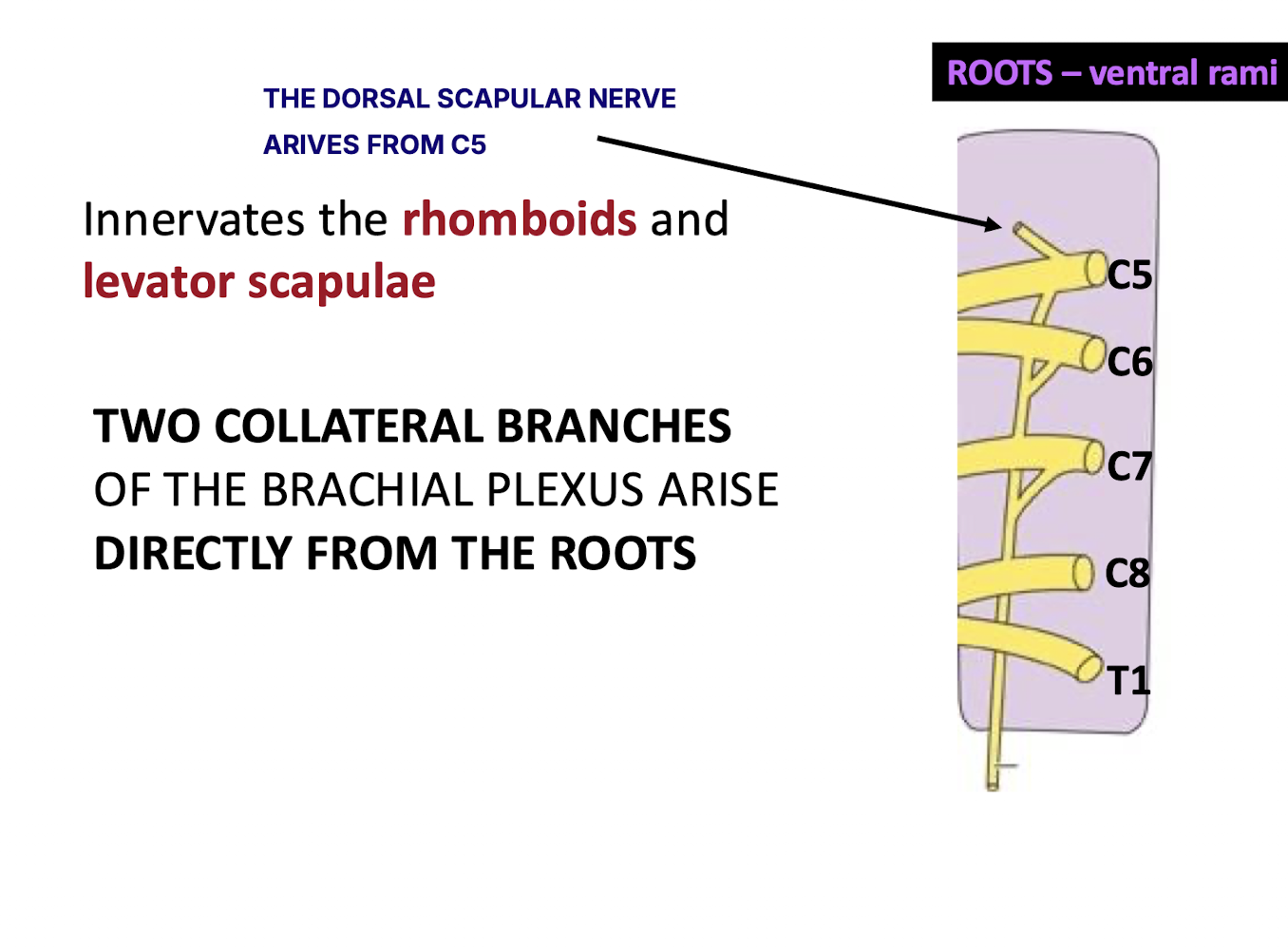
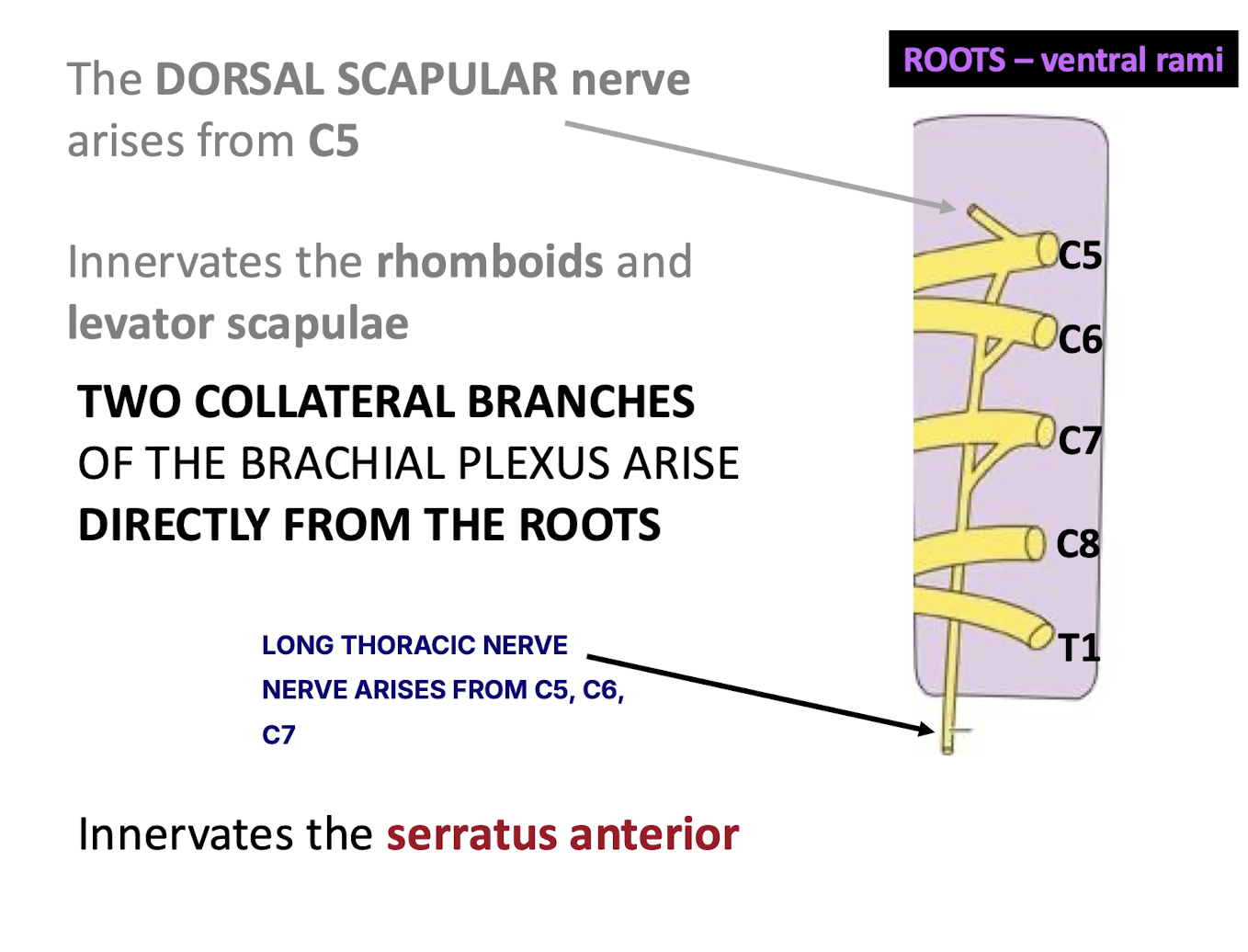
Which muscles are innervated by the dorsal scapular nerve?
The rhomboids (major and minor) and the levator scapulae.
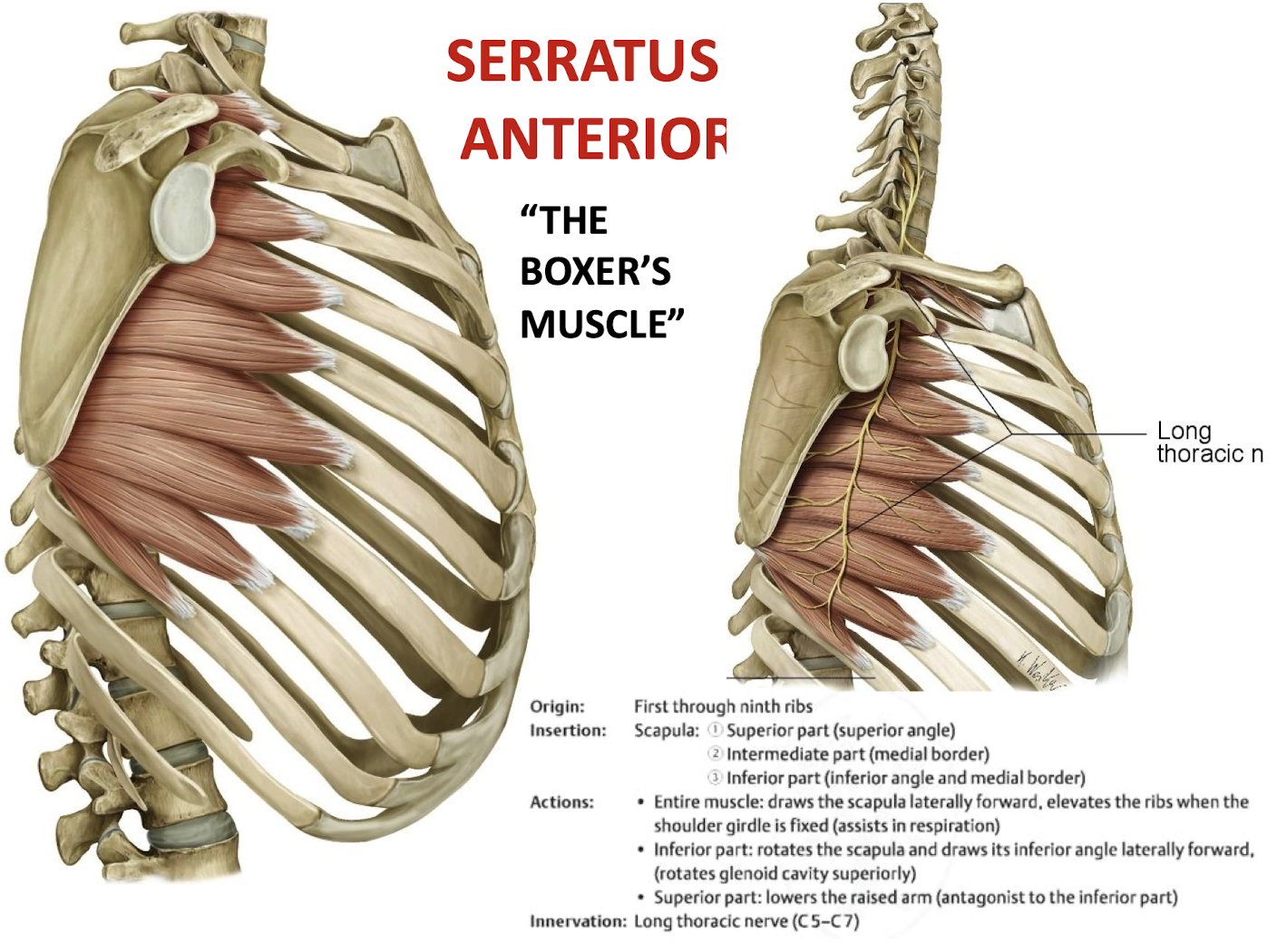
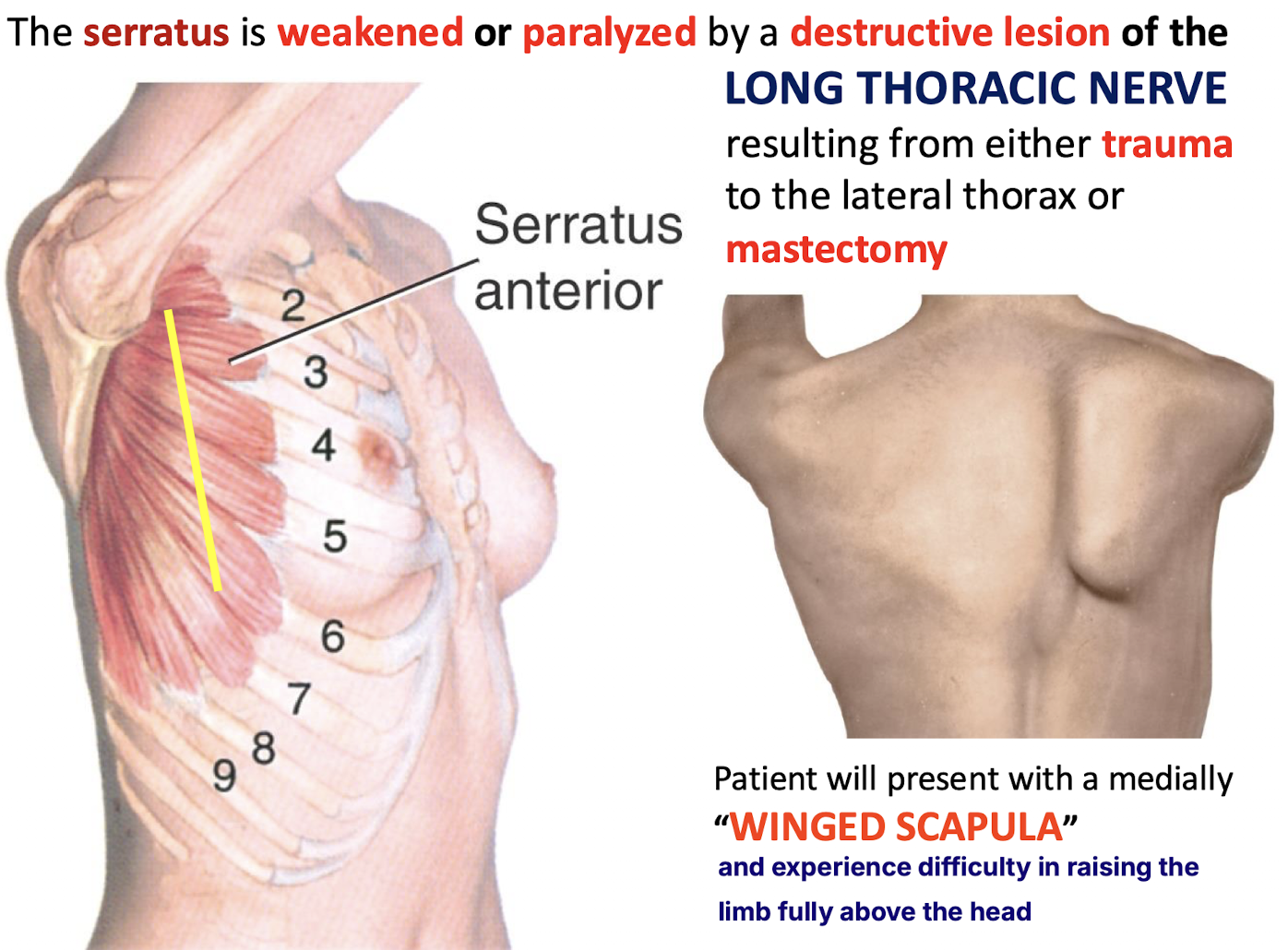
What is the "Boxer's muscle," and what is its innervation?
The serratus anterior (called boxer’s because its the principal protractor of the scapula), innervated by the long thoracic nerve (C5-C7).
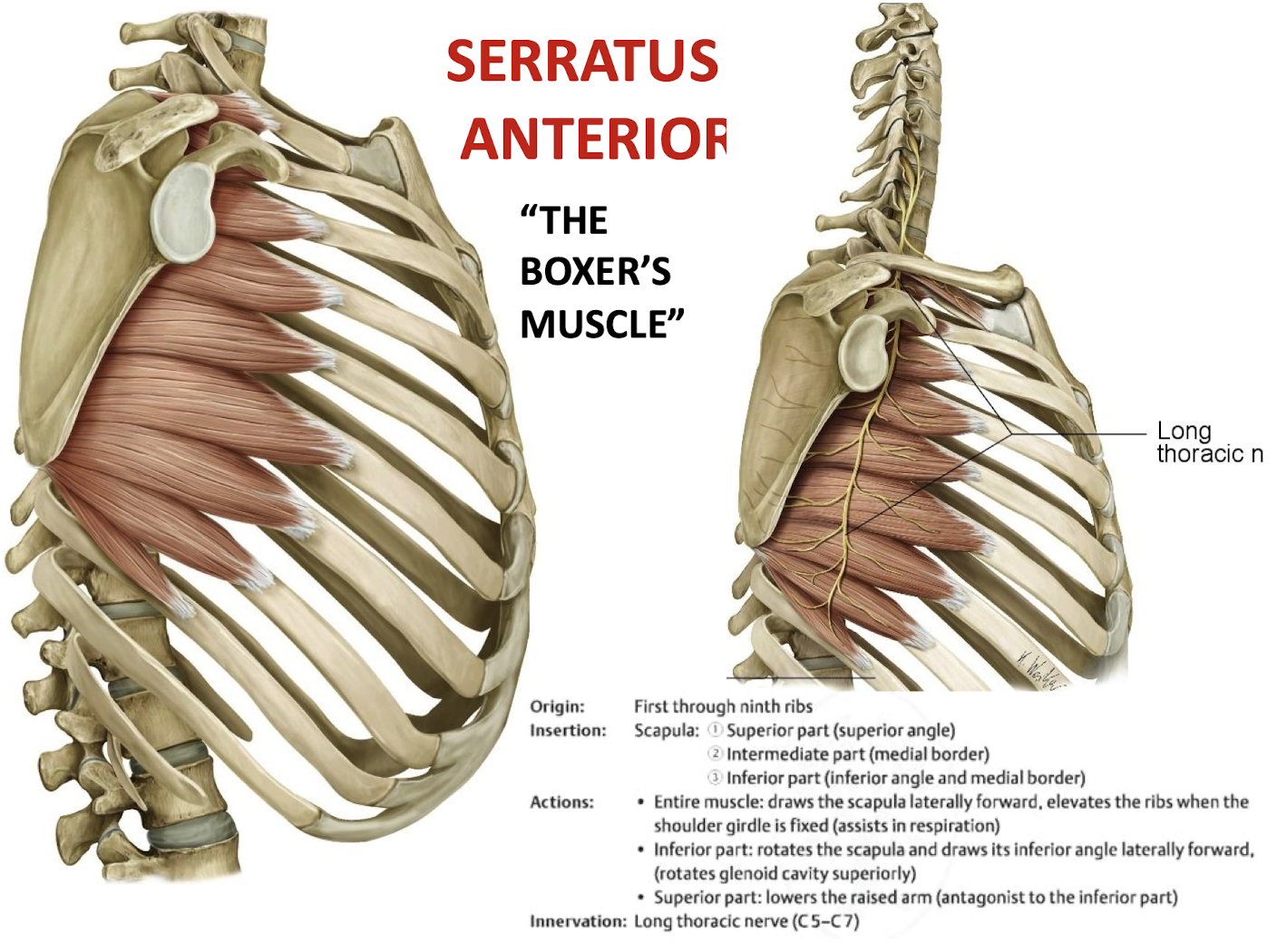
What makes the relationship between the serratus anterior and the long thoracic nerve unique?
The long thoracic nerve runs on the superficial aspect of the serratus anterior, just deep to the skin, making it vulnerable to injury during trauma or surgery.
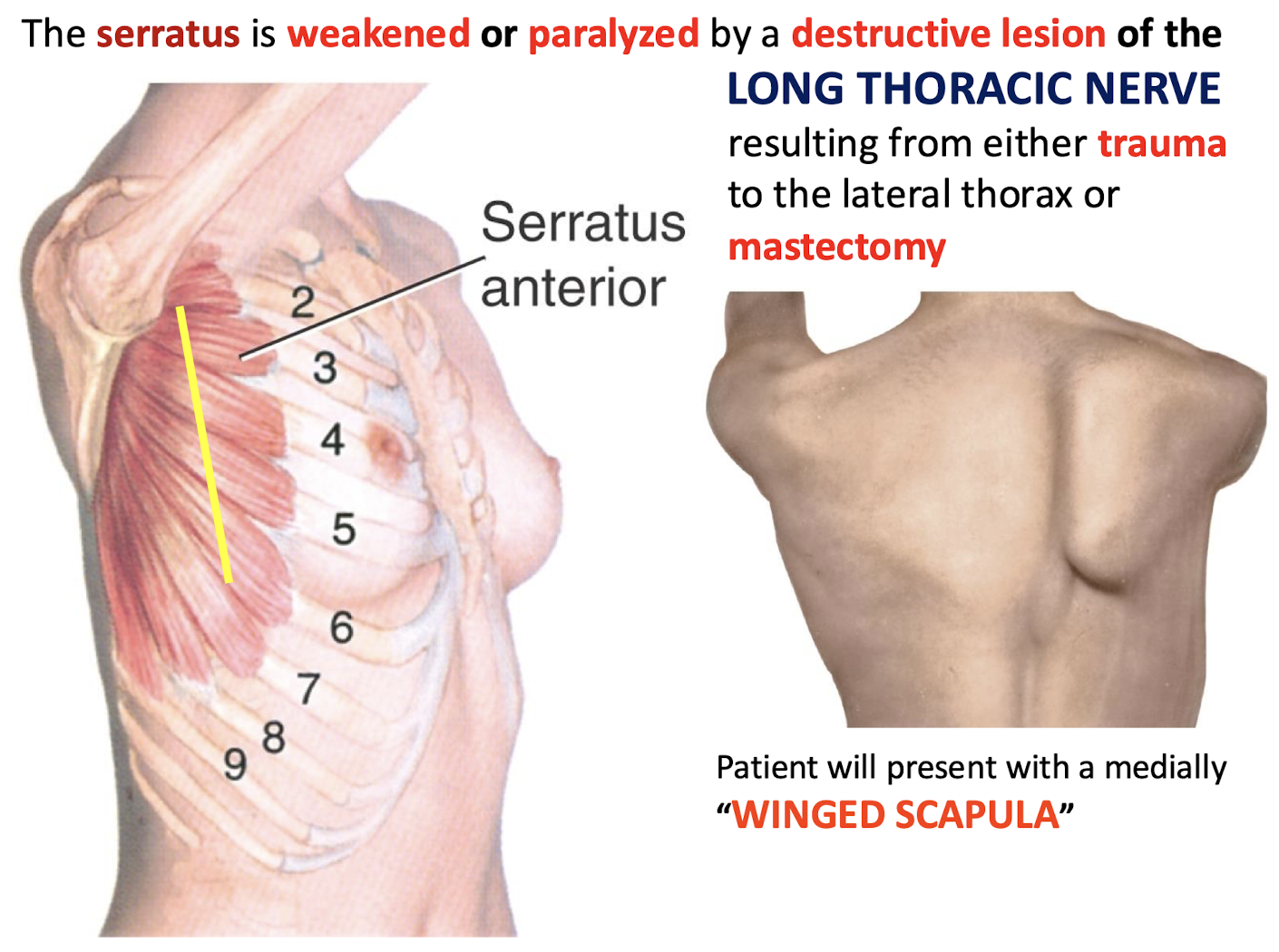
What clinical sign results from a destructive lesion of the long thoracic nerve? What could cause this destruction?
A medially "winged scapula" and experience difficulty in raising the limb fully above the head from the weakened or paralyzed serratus
Resulting from either trauma to the lateral thorax or mastectomy
Scapular rotation is required for abduction and flexion of the arm beyond how many degrees?
Beyond the initial 30 degrees.
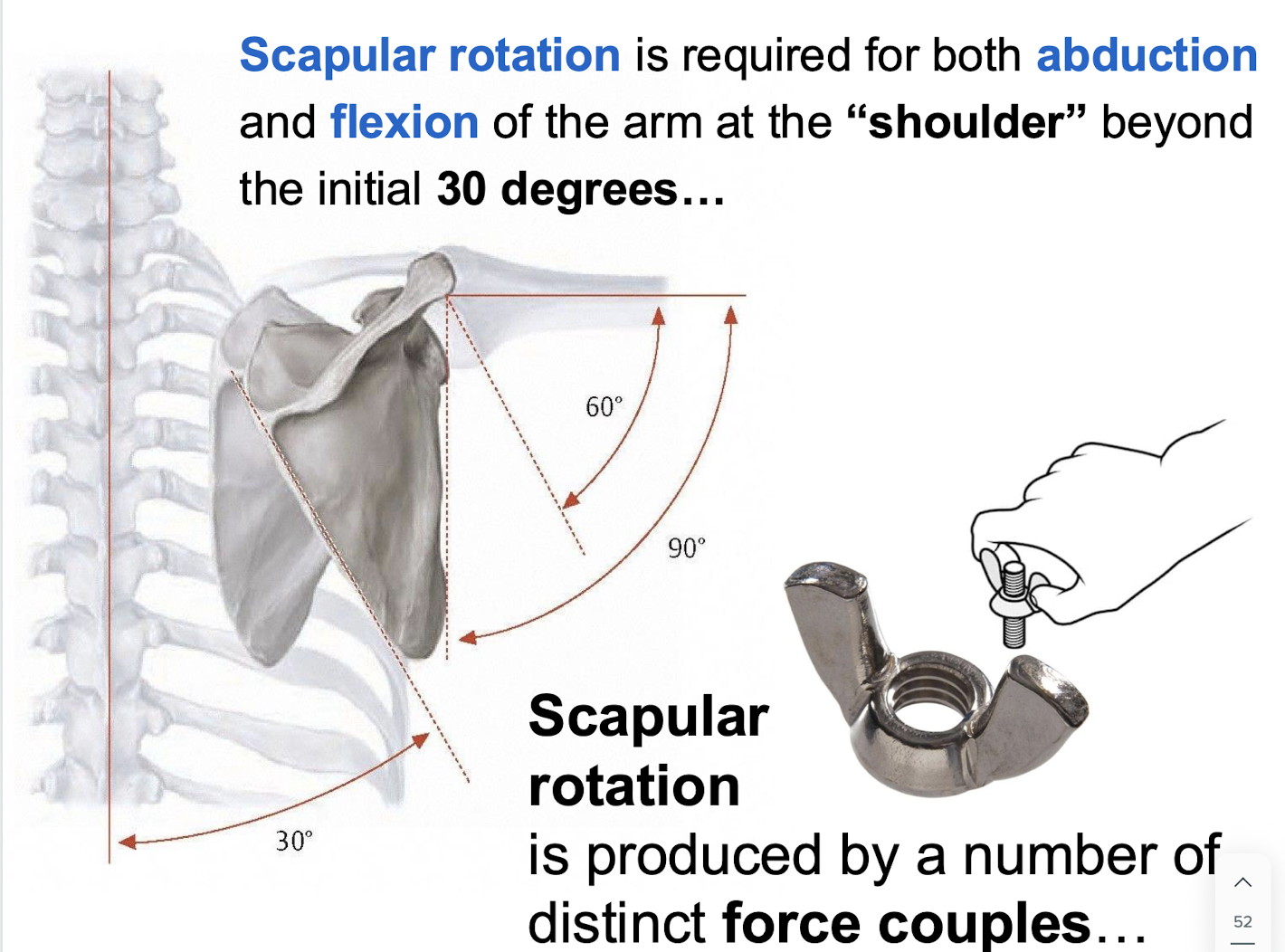
List the muscles involved in scapular rotation.
Upper/lower trapezius, serratus anterior, levator scapulae, rhomboids, pectoralis minor, and latissimus dorsi.
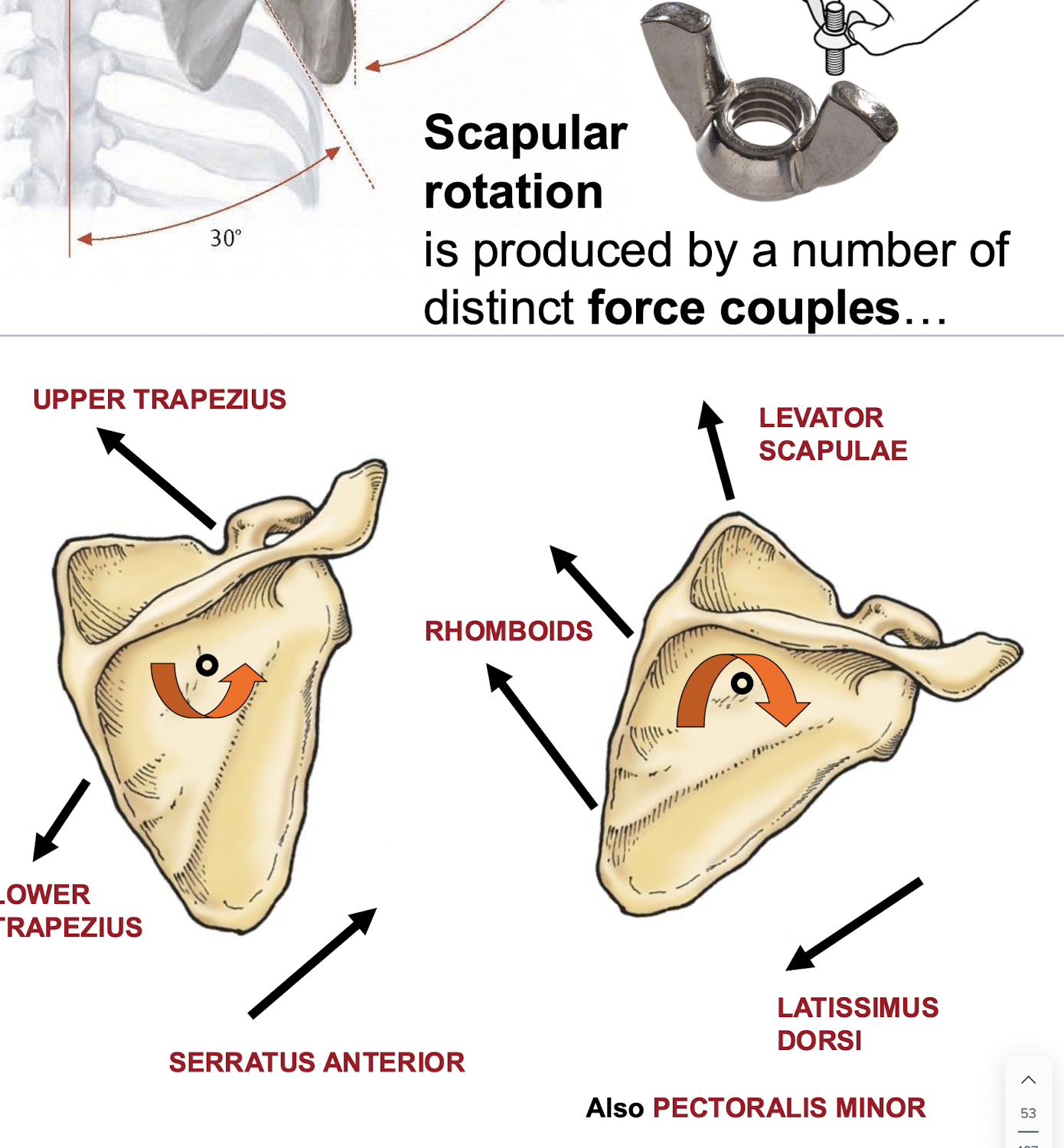
Which muscles are the primary elevators of the scapula?
Upper trapezius and levator scapulae.
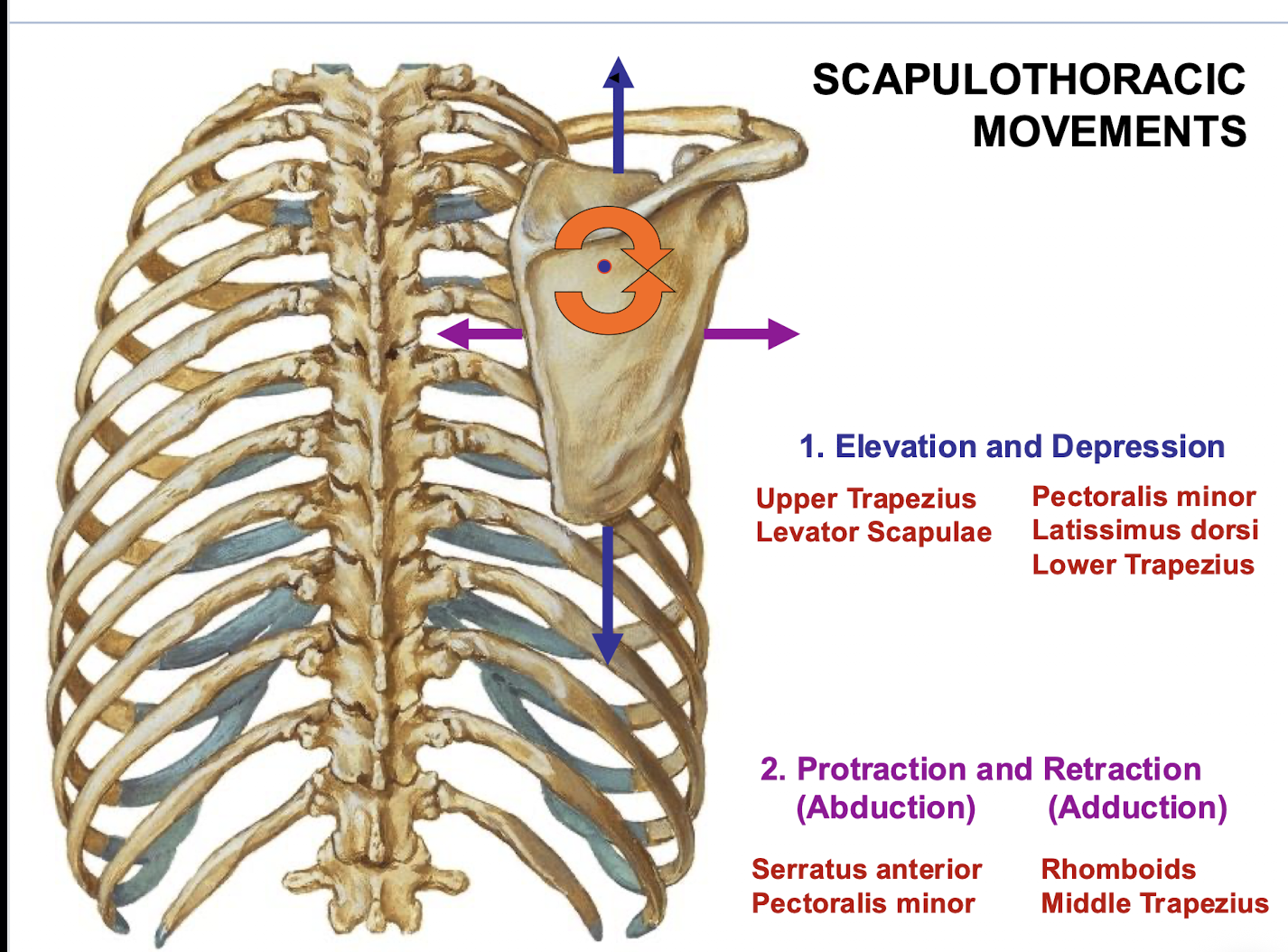
Which muscles are the primary depressors of the scapula?
Pectoralis minor, latissimus dorsi, and lower trapezius.
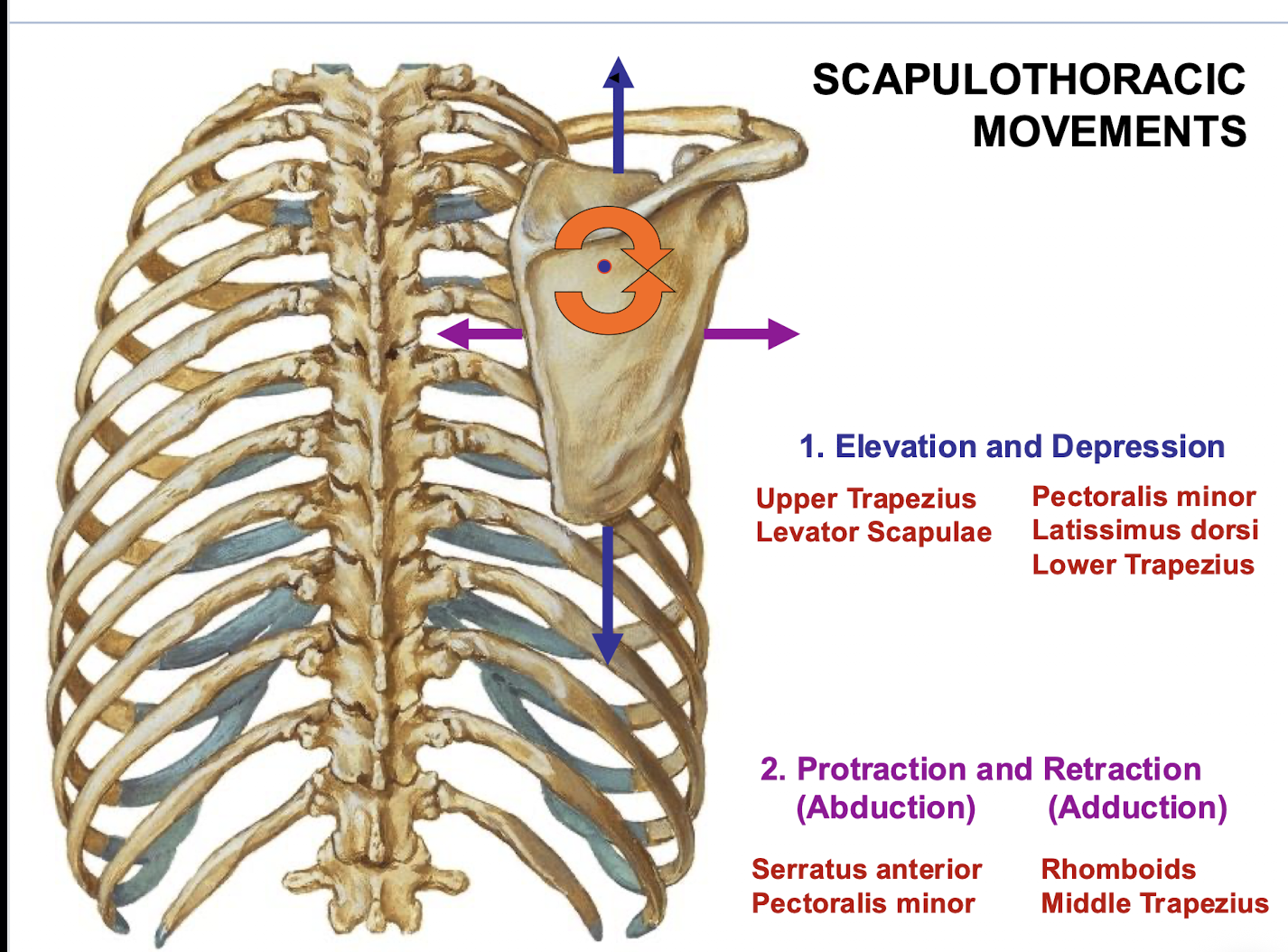
Which muscles are responsible for scapular protraction (abduction)?
Serratus anterior and pectoralis minor.
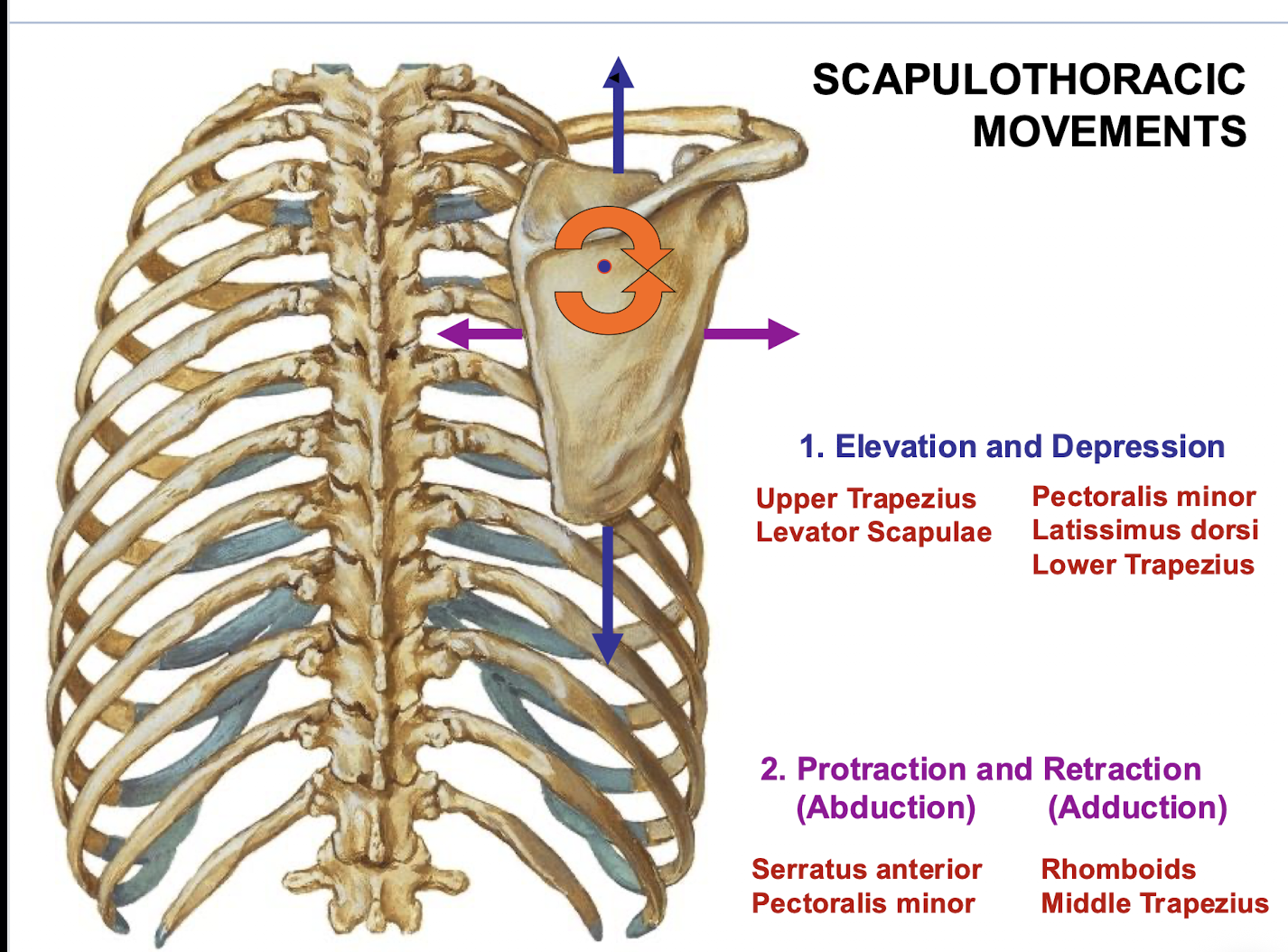
Which muscles are responsible for scapular retraction (adduction)?
Rhomboids and middle trapezius.
How are the three trunks of the brachial plexus formed?
Superior (C5-C6), Middle (C7), and Inferior (C8-T1).
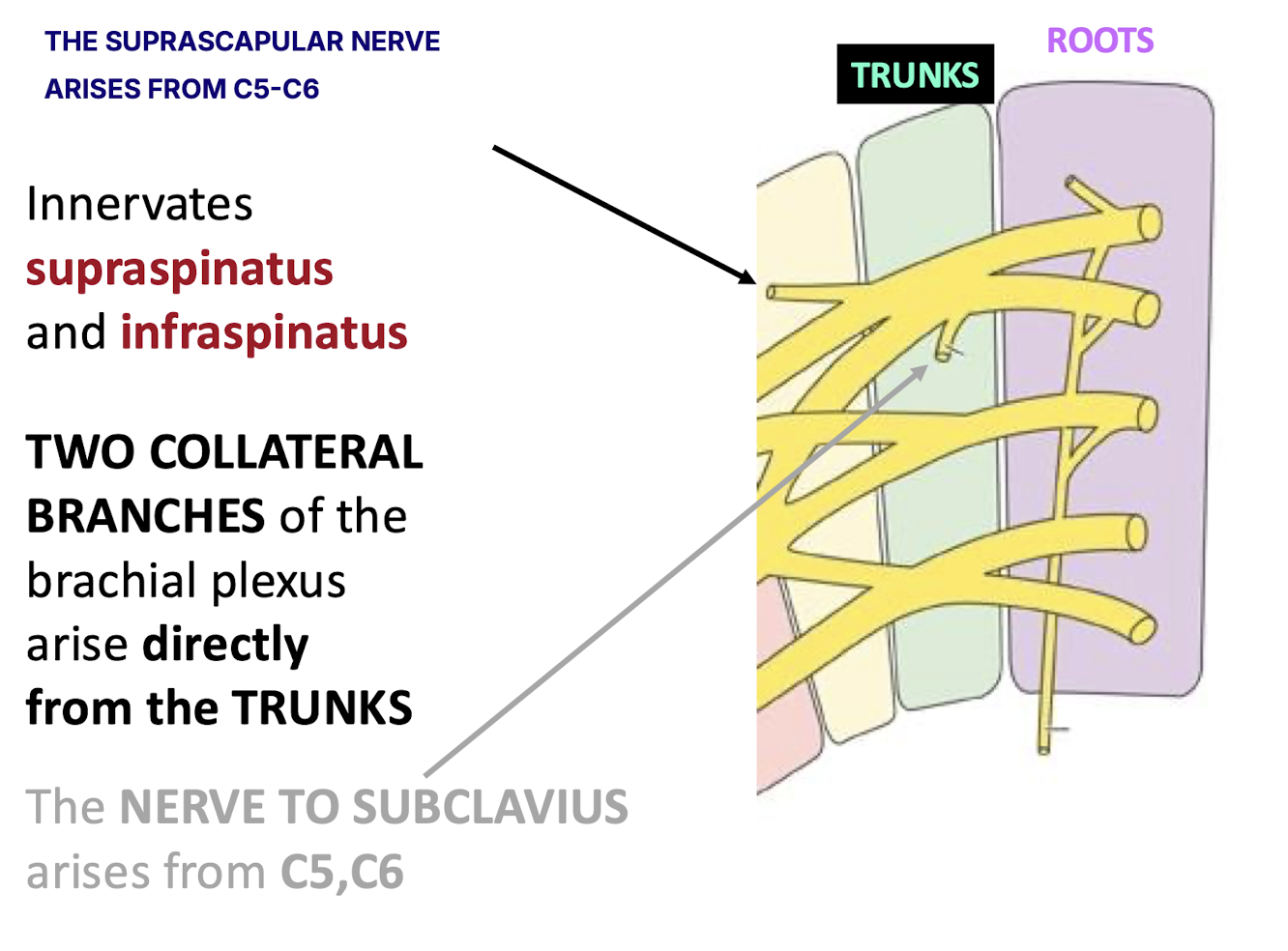
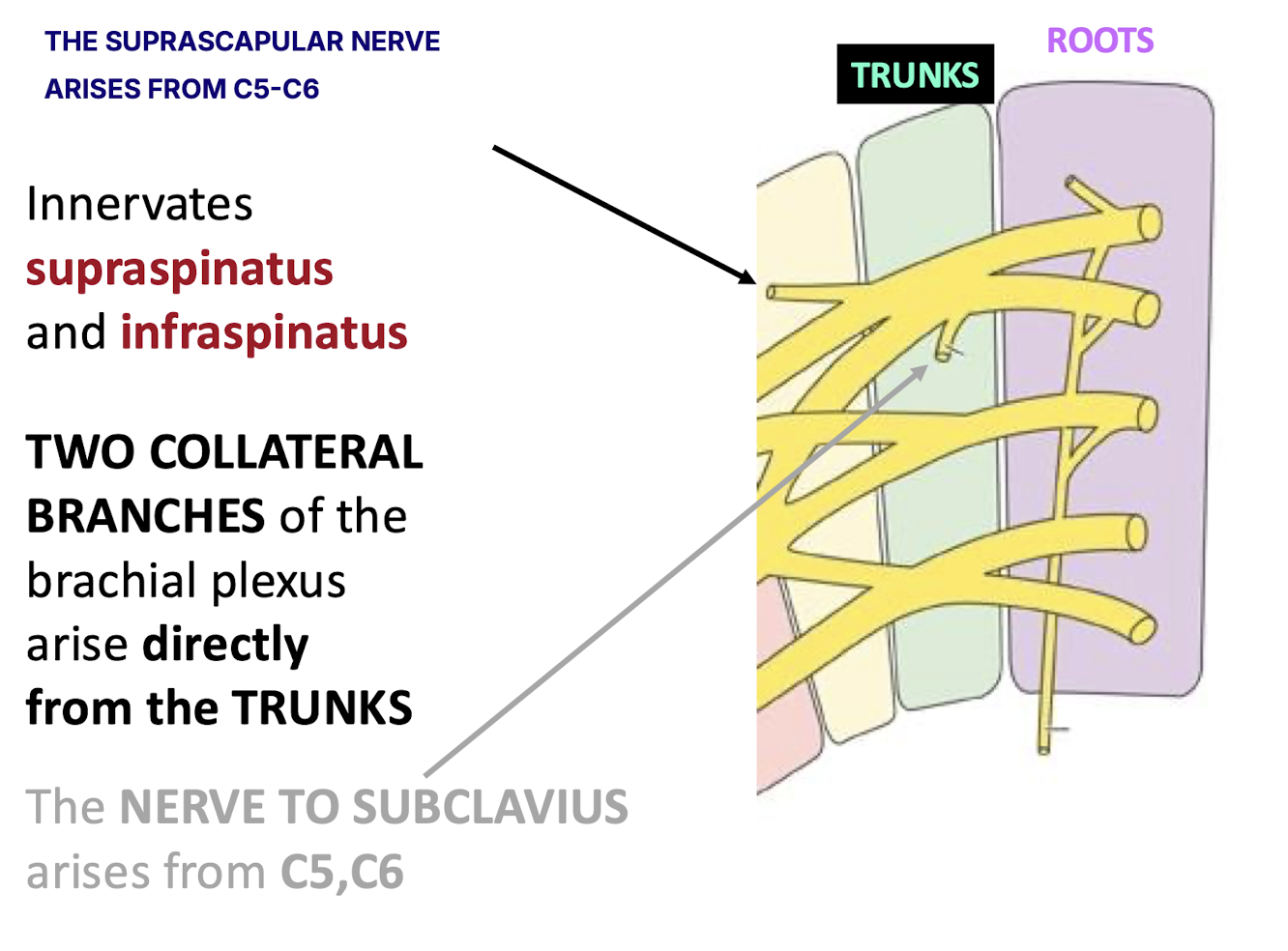
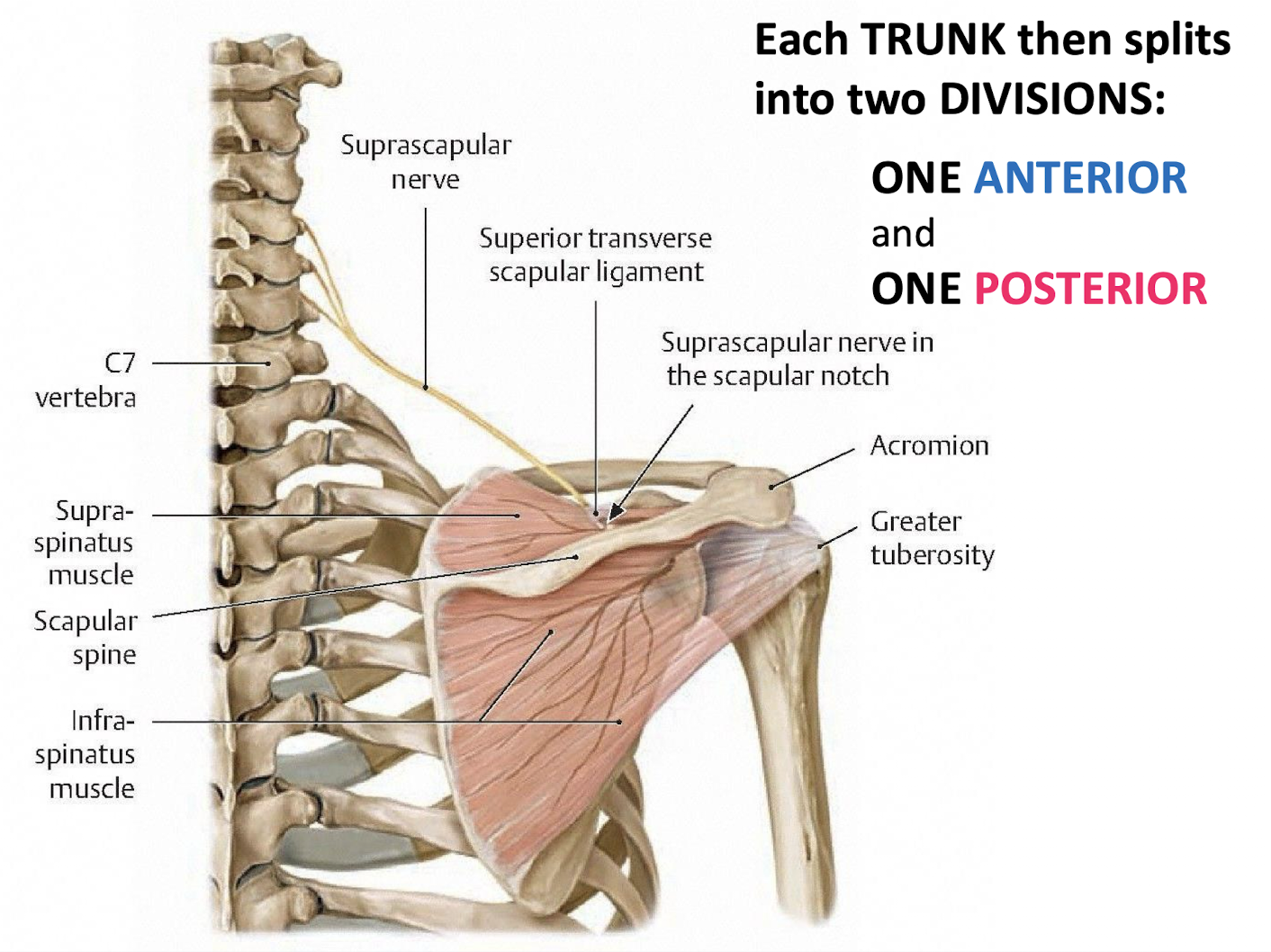
Which two collateral branches arise directly from the superior trunk? Include nerve number
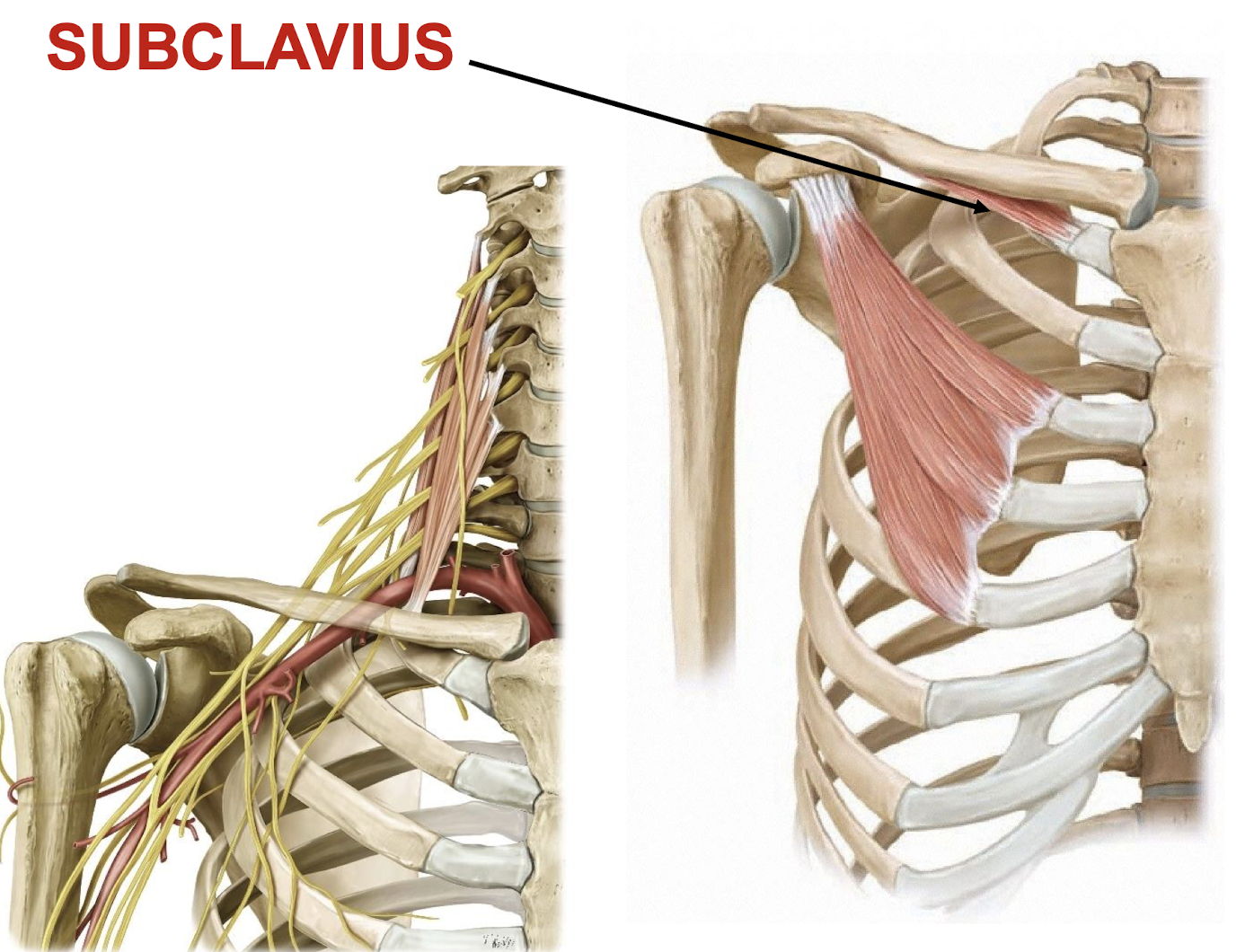
The nerve to subclavius (C5-C6) and the suprascapular nerve (C5-C6).
What is the function of the subclavius muscle?
Provides minimal contribution to movement of the sternoclavicular (SC) joint.
Protects neurovascular structures of the upper extremity as they transition beneath the clavicle.
Which muscles are innervated by the suprascapular nerve?
The supraspinatus and infraspinatus.
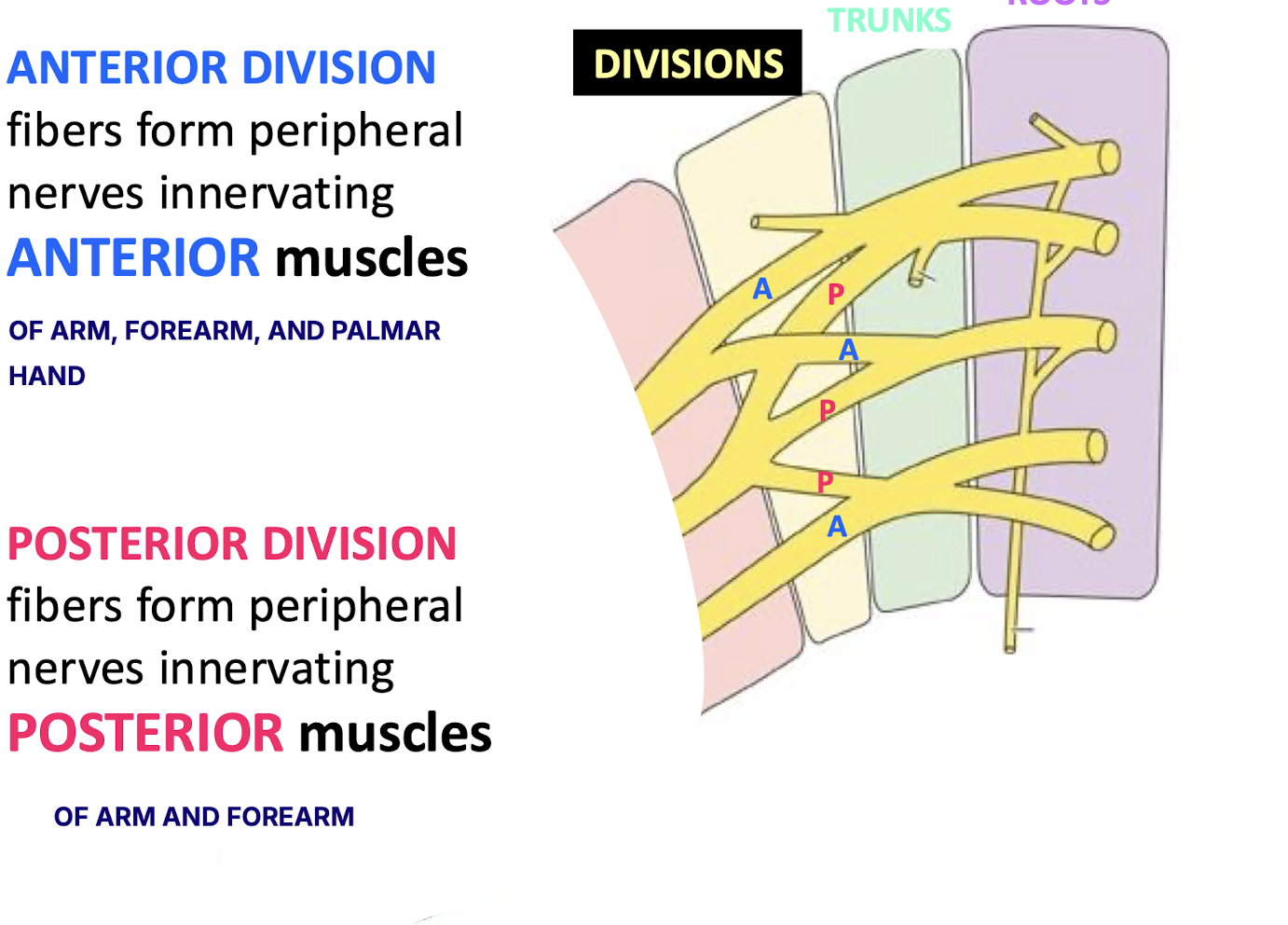
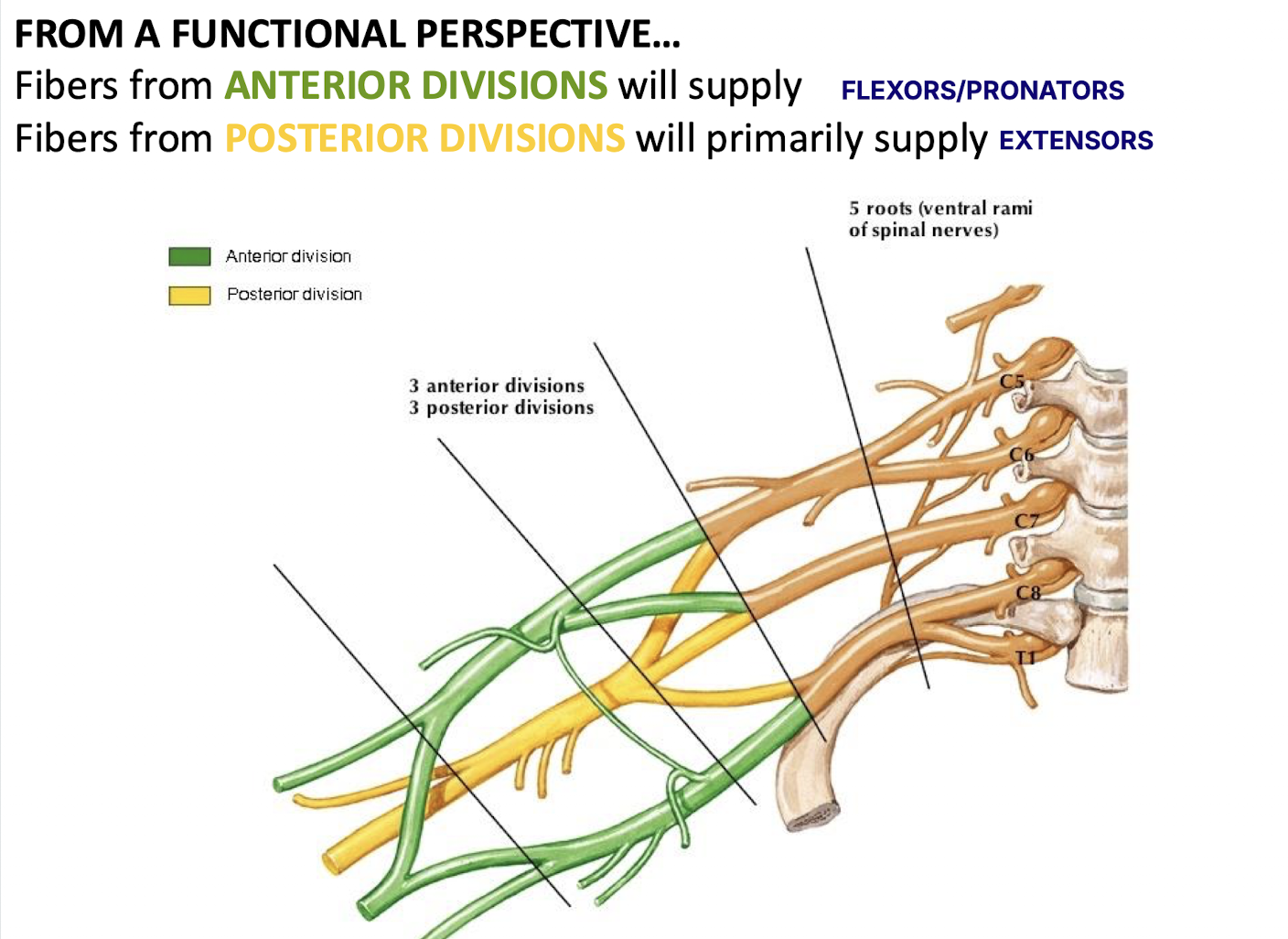
Functionally, what do the anterior and posterior divisions of the plexus supply?
Anterior supply flexor/pronator muscles (ARM, FOREARM, AND PALMAR HAND); Posterior supply extensor muscles (ARM AND FOREARM).
How are the lateral, medial, and posterior cords of the plexus formed?
Lateral: ant. divisions of sup./mid. trunks;
Medial: ant. division of inf. trunk;
Posterior: post. divisions of all three trunks.
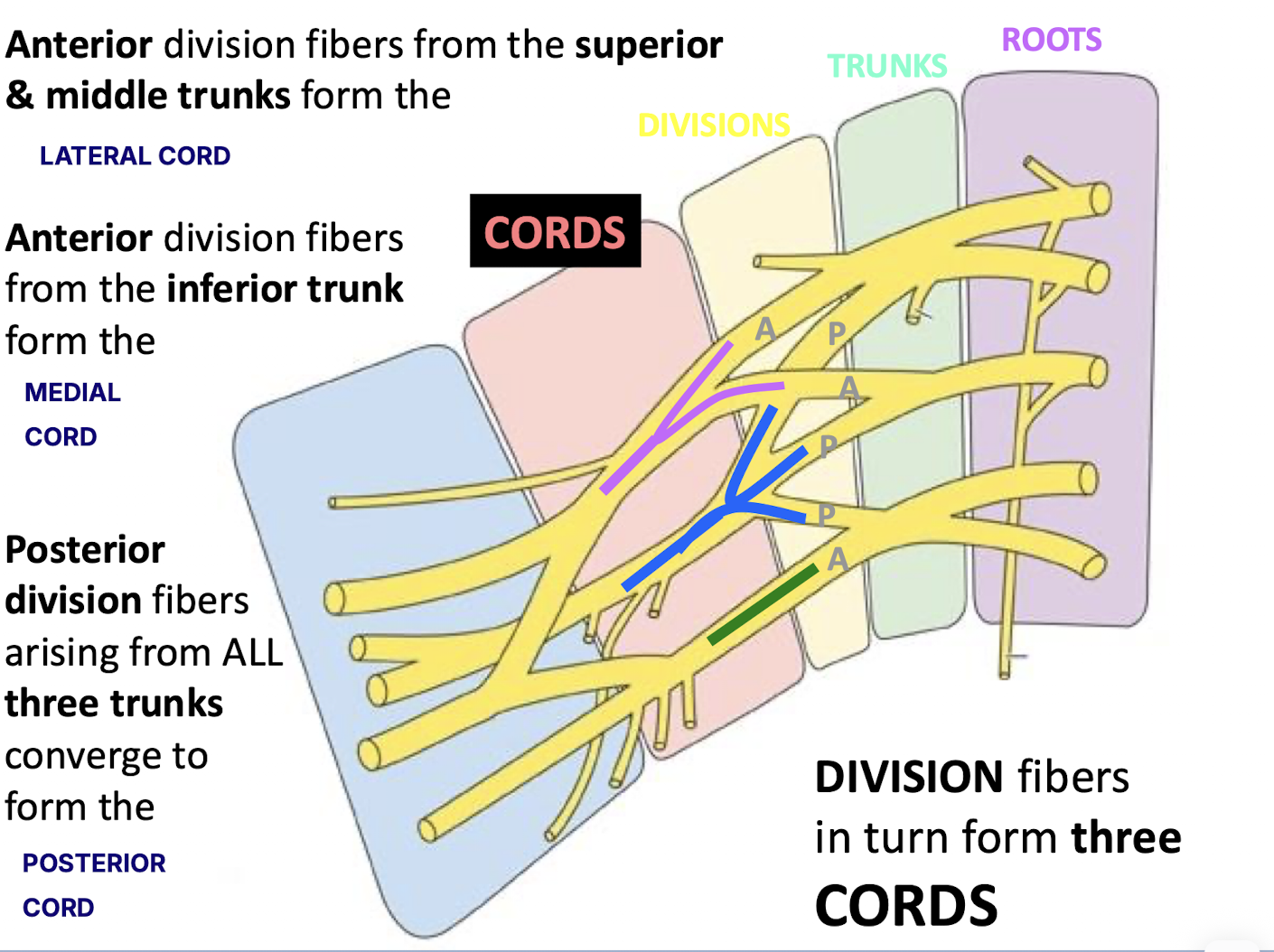
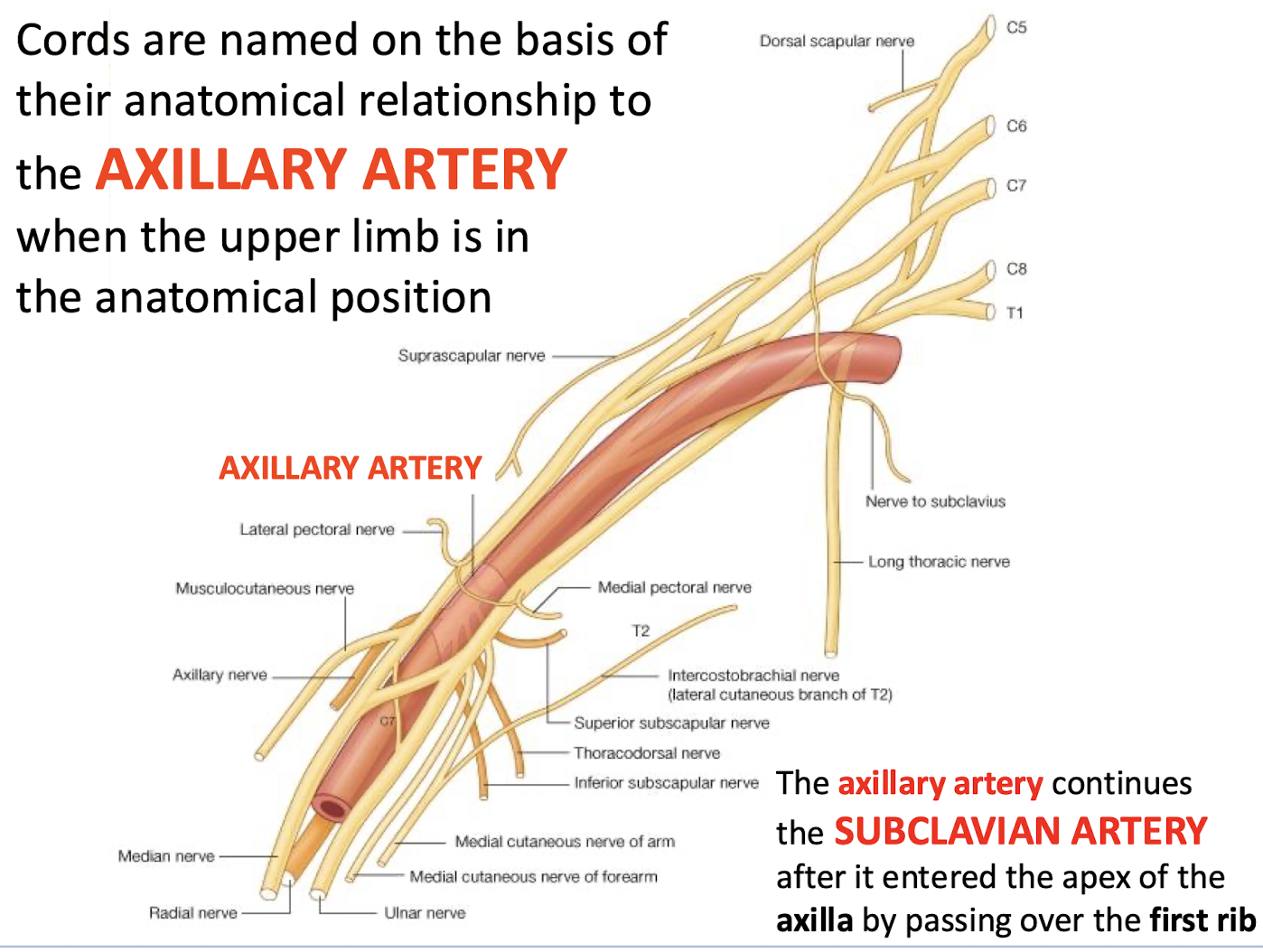
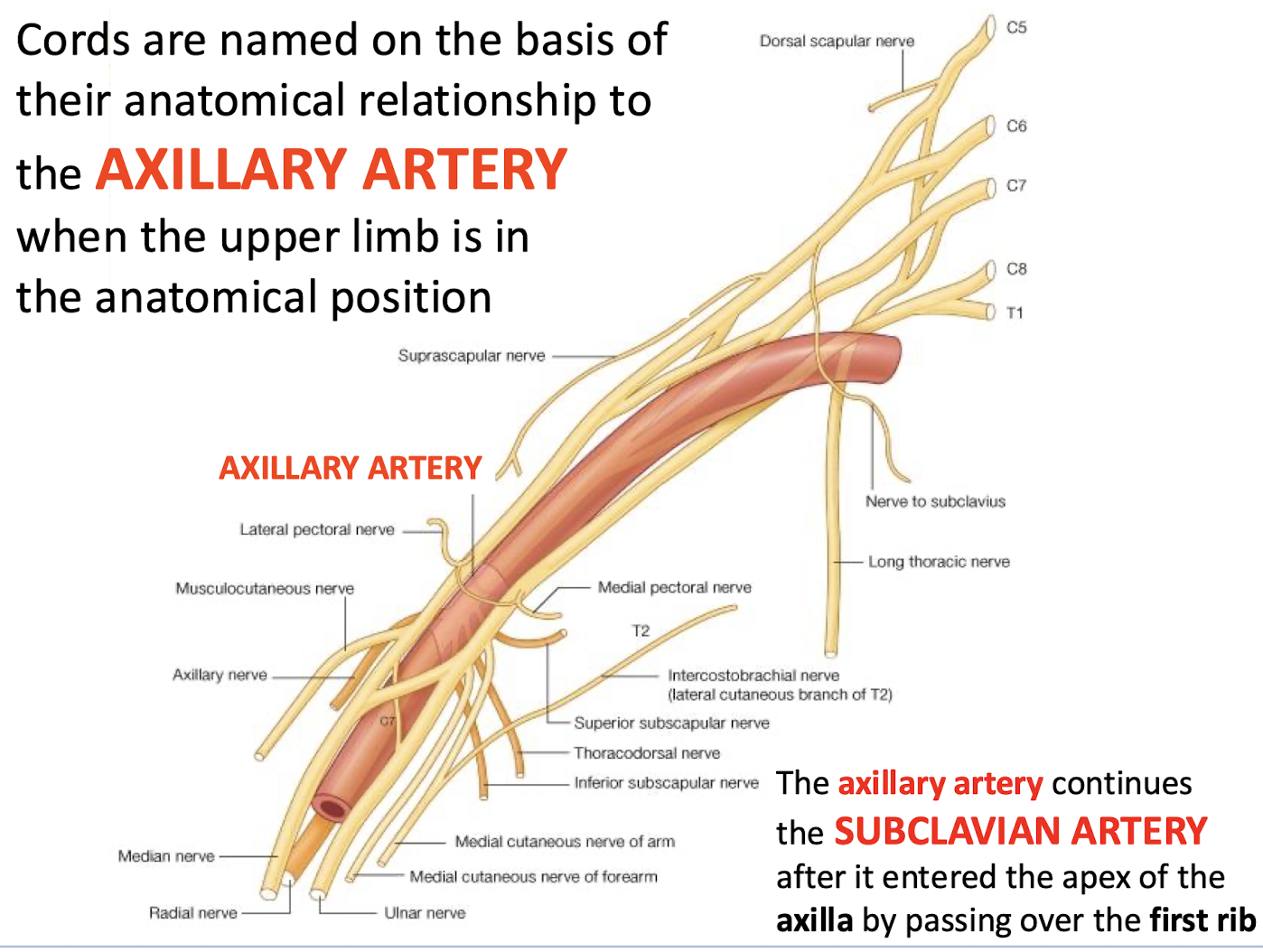
On what basis are the cords of the brachial plexus named?
Their anatomical relationship to the axillary artery in the anatomical position
.
When does the axillary artery begin and continue?
The axillary artery is a continuation of the subclavian artery after it enters the apex of the axilla by passing over the first rib.
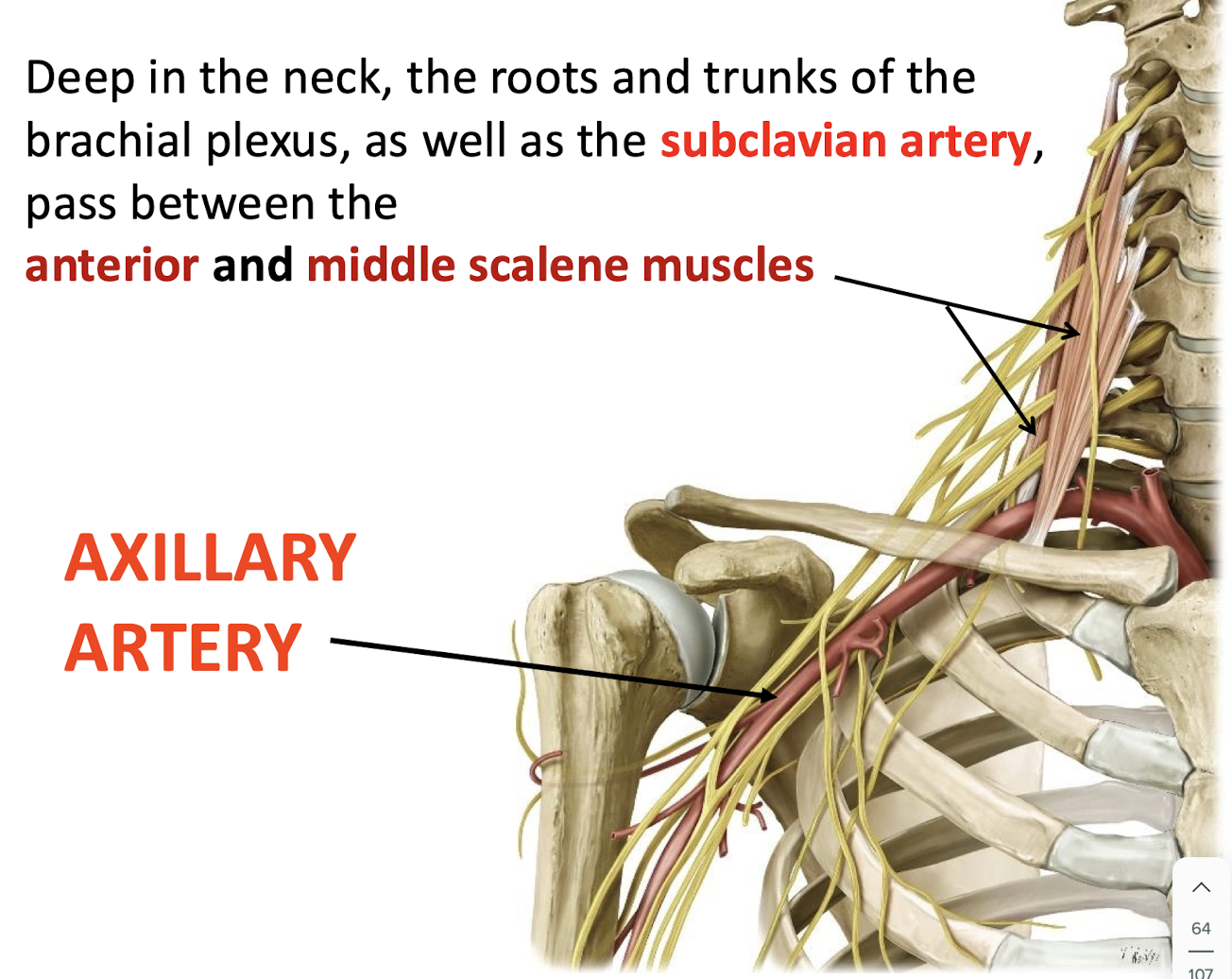
Between which two muscles do the roots/trunks and the subclavian artery pass?
The anterior and middle scalene muscles.
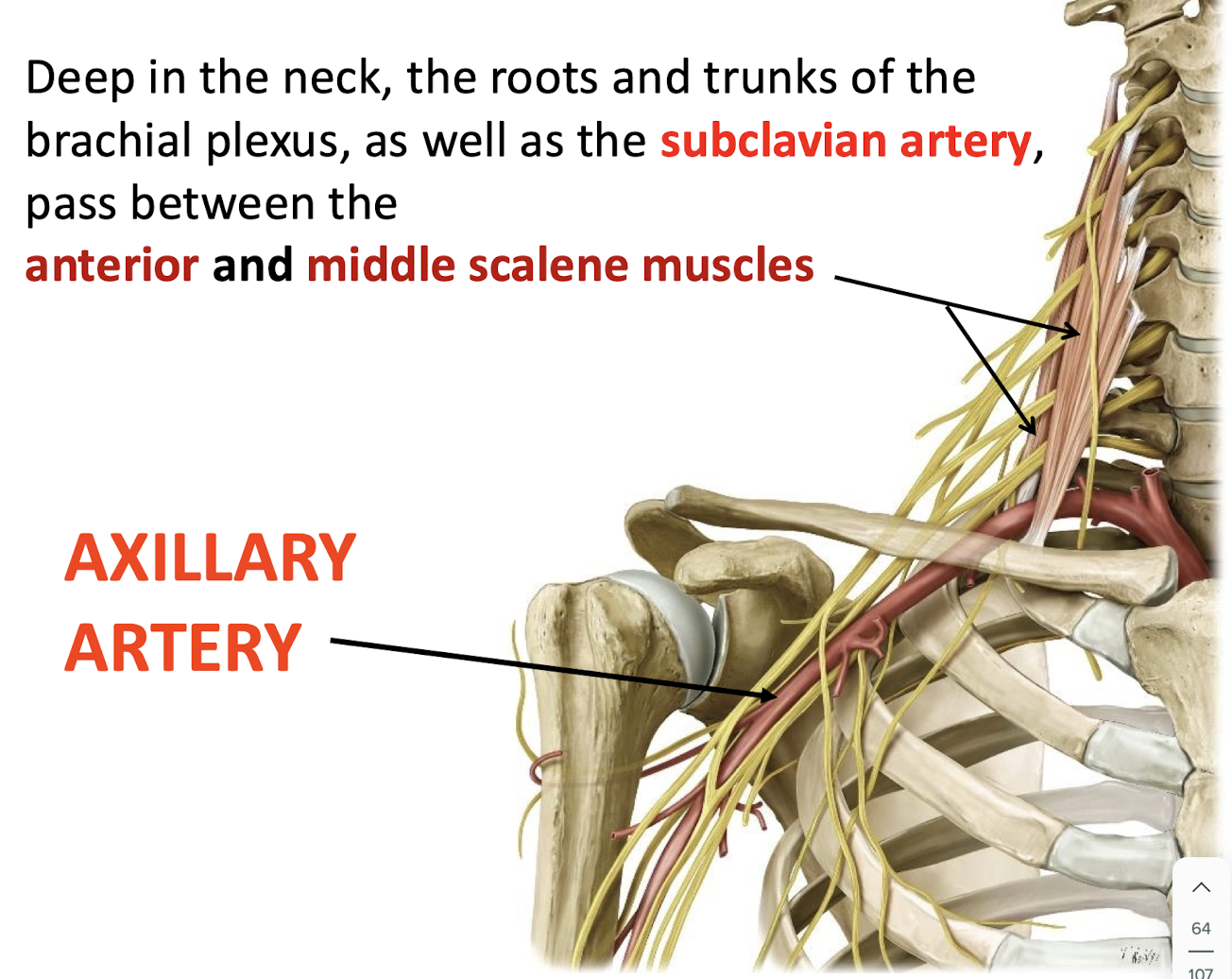
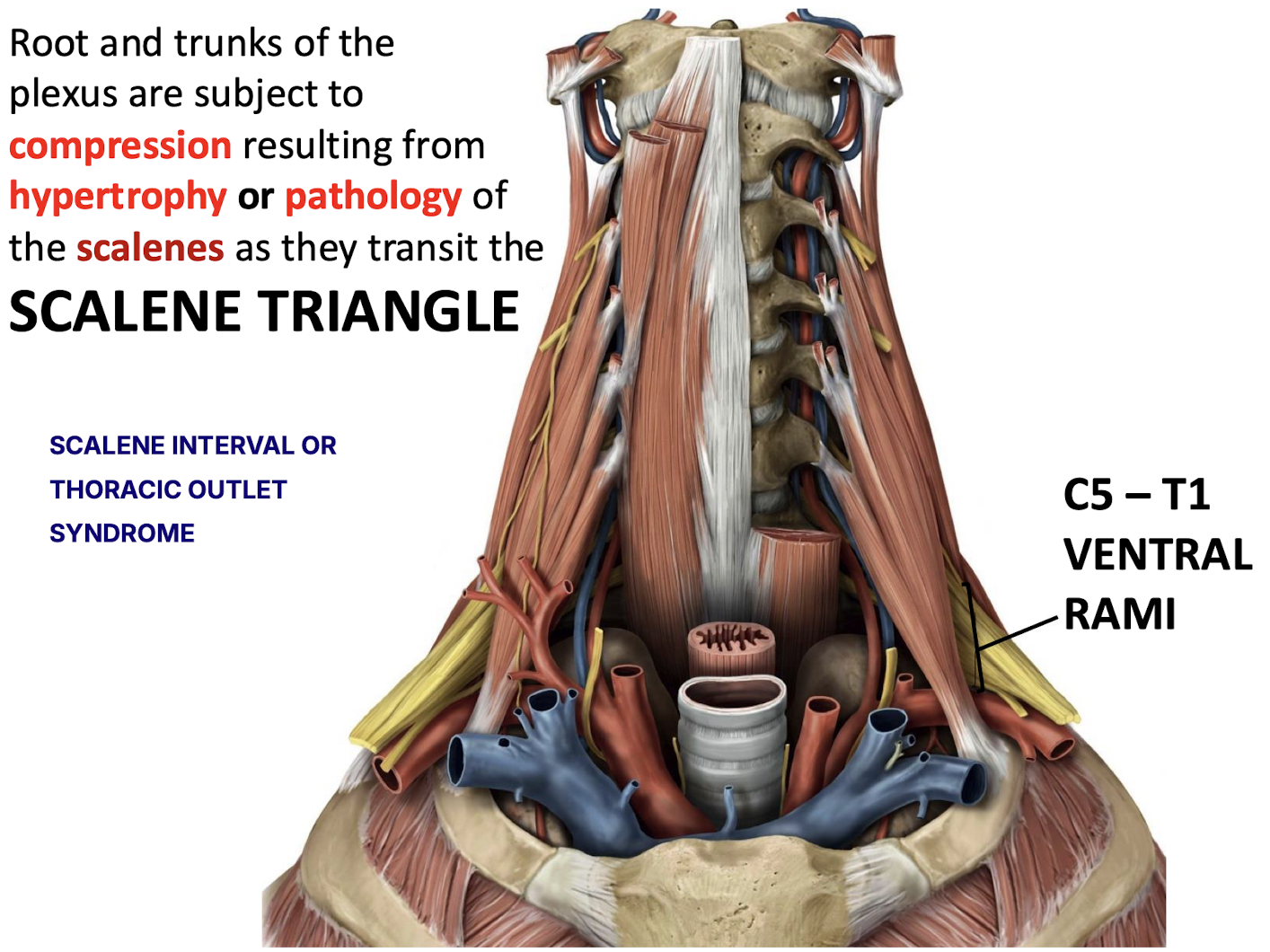
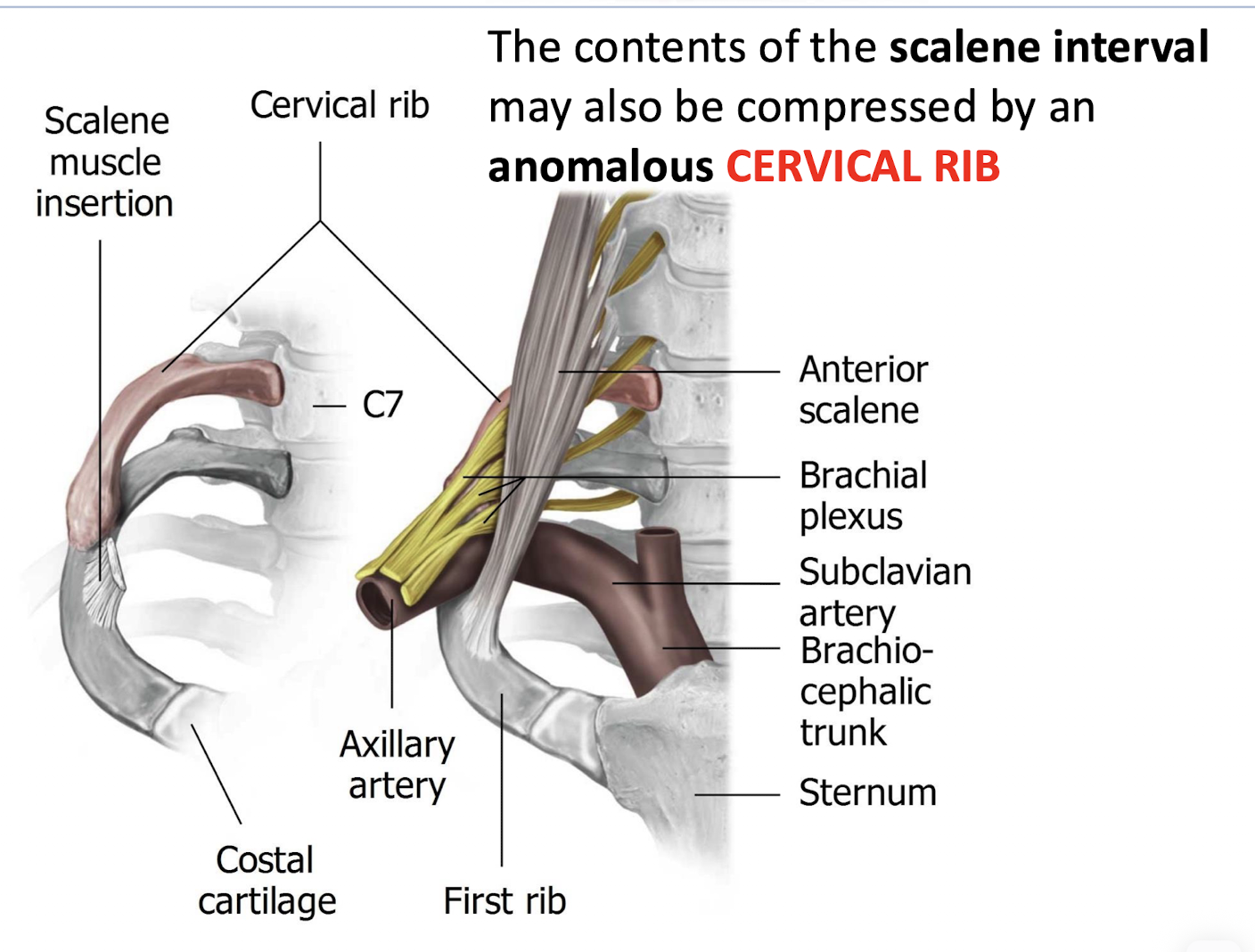
Where can the roots and trunks of the brachial plexus be compressed, and what is this condition called? How might this be treated?
Compression occurs in the scalene triangle (scalene interval) as the C5–T1 ventral rami pass through.
Caused by hypertrophy or pathology of the scalenes.
This can lead to SCALENE INTERVAL OR Thoracic Outlet Syndrome (TOS).
Can treat by removing the first rib
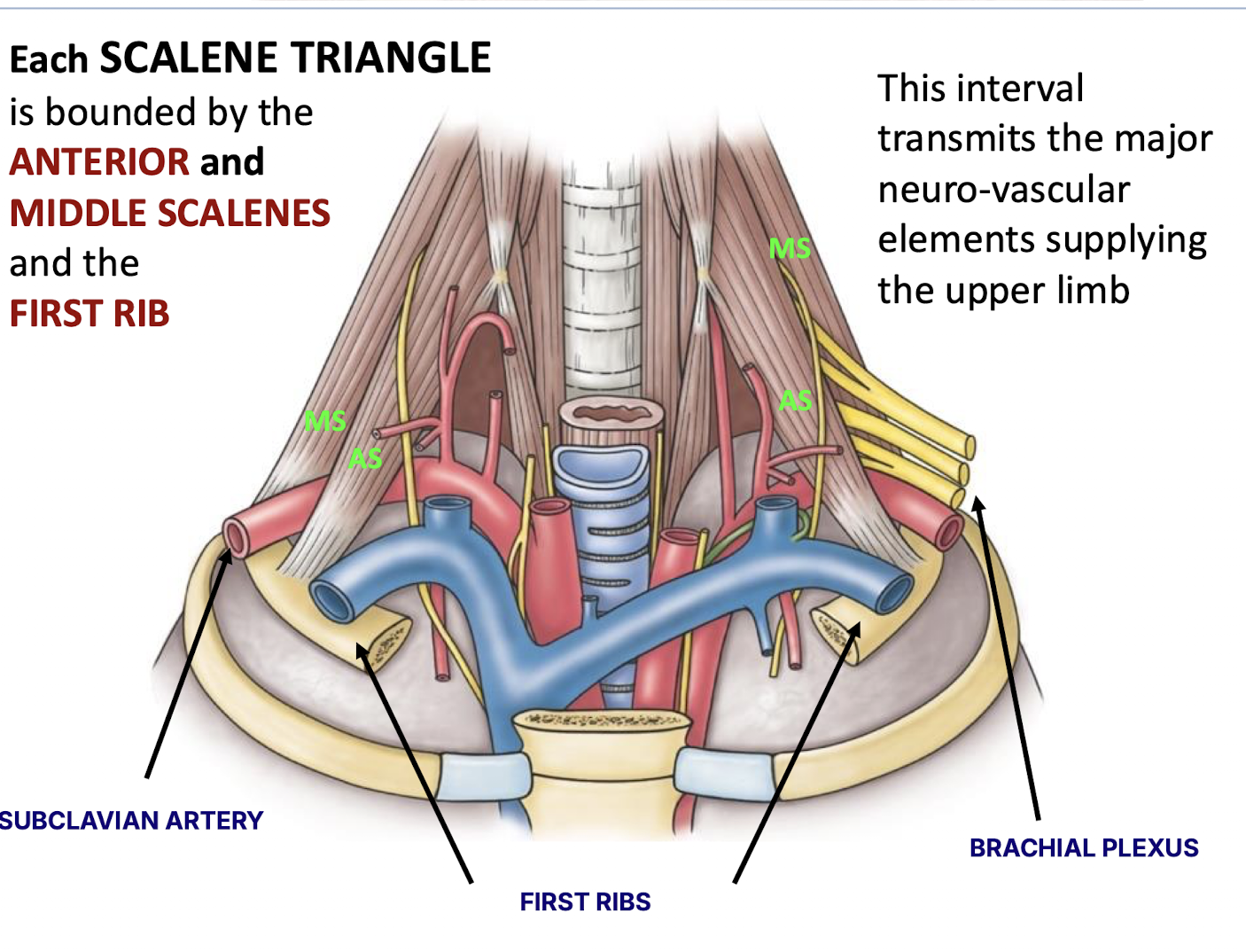
What are the boundaries of the scalene triangle?
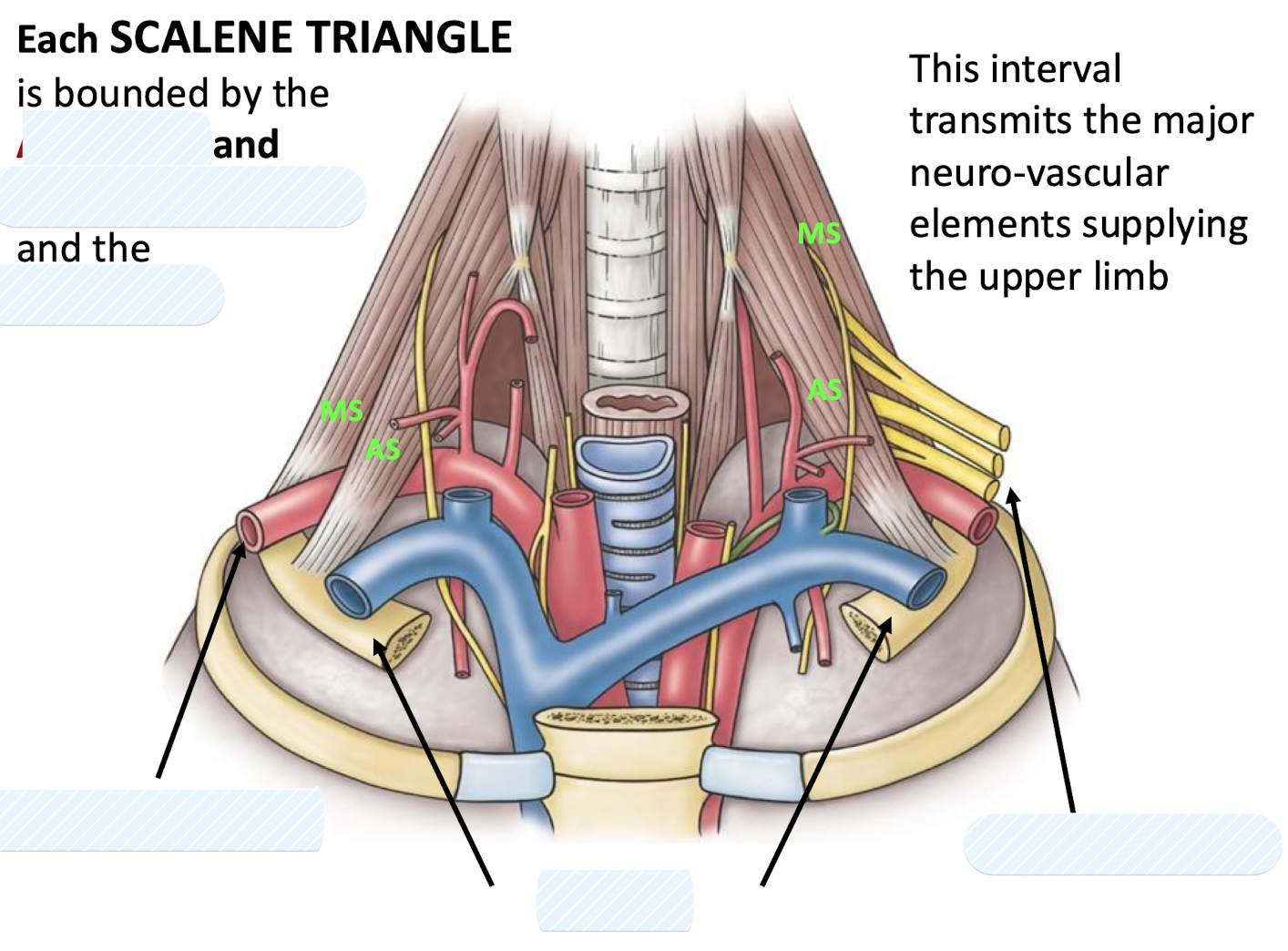
The anterior scalene, middle scalene, and the first rib.
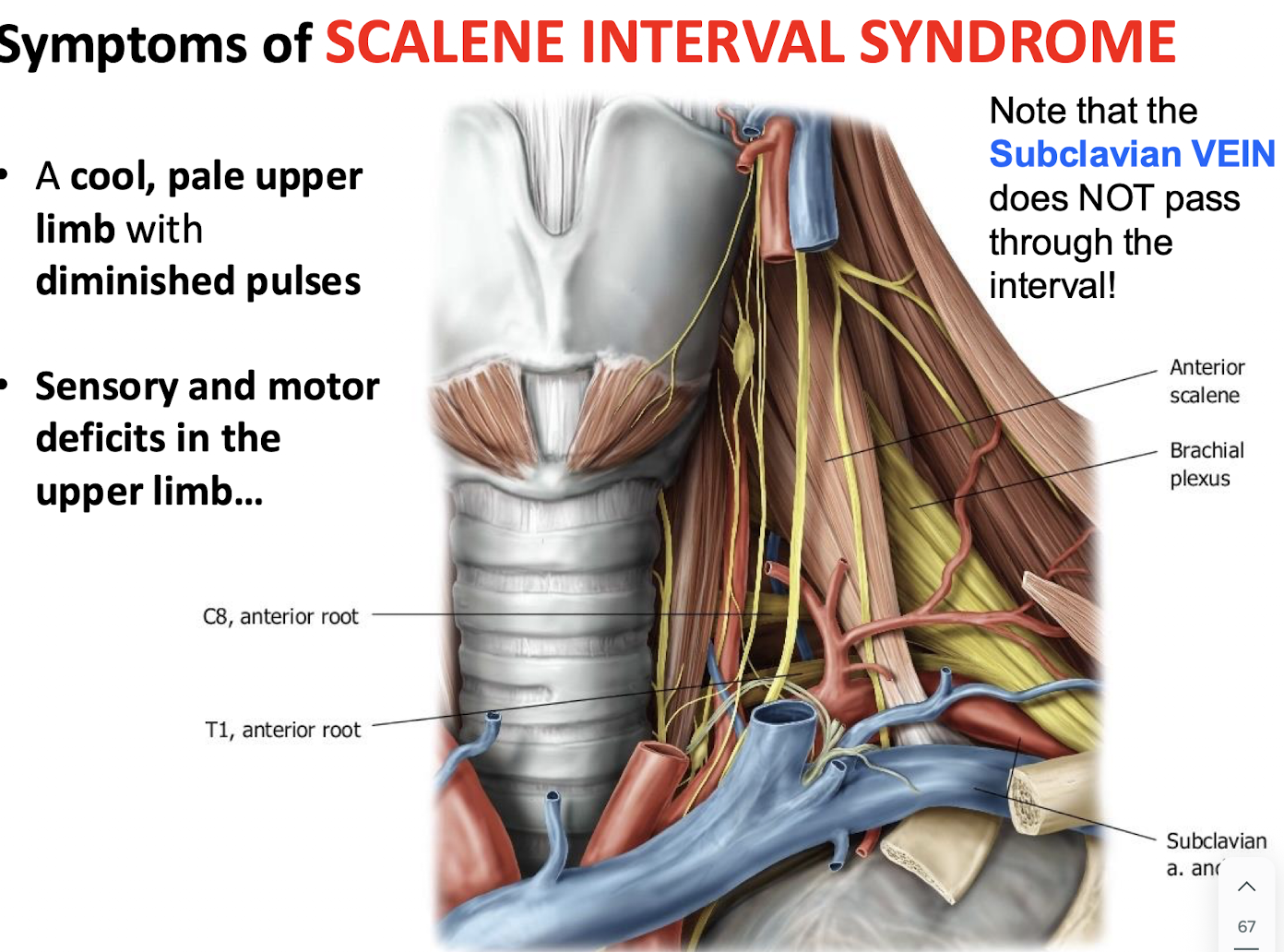
What are the three symptoms of Scalene Interval Syndrome?
Vascular: A cool, pale limb with diminished pulses due to subclavian artery compression.
Neurologic:
Sensory and motor deficits in the upper limb from brachial plexus compression.
Motor deficits concentrated distally (hand/forearm) due to compression near the first rib.
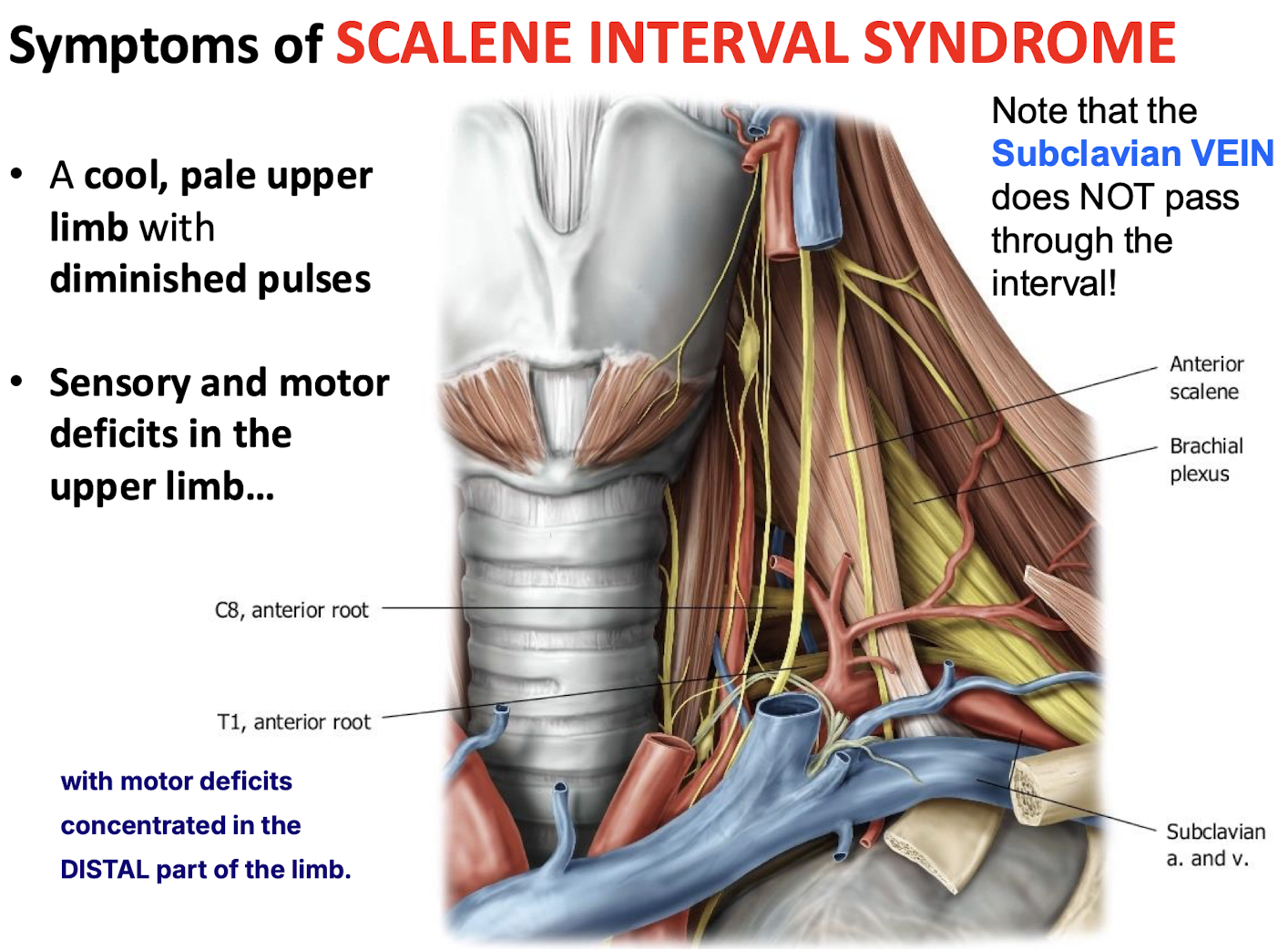
Which major vessel does NOT pass through the scalene triangle?
The subclavian vein.
What anomalous condition can compress the contents of the scalene interval?
The contents of the scalene interval may also be compressed by an anomalous CERVICAL RIB
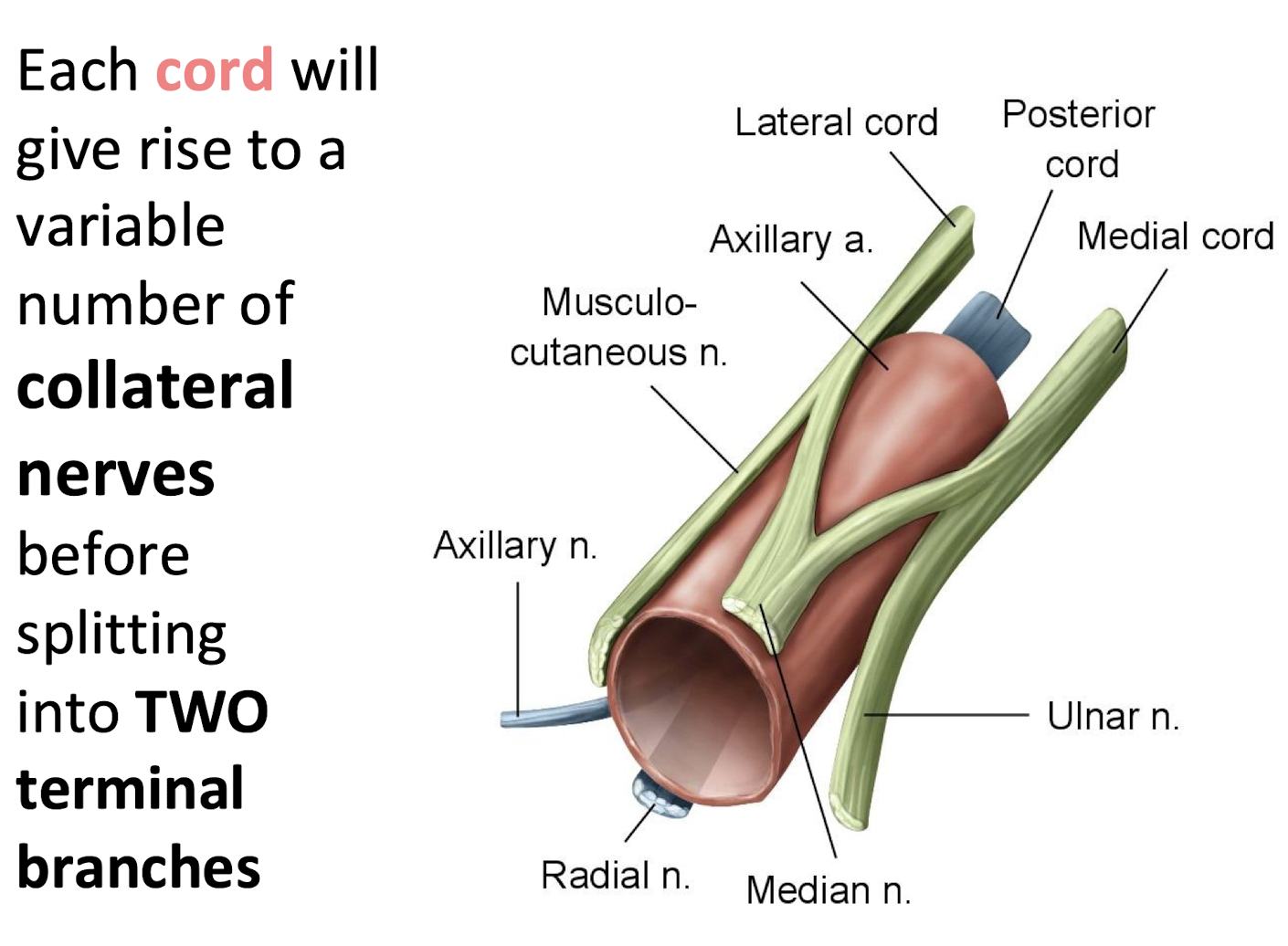
What do the cords of the brachial plexus give rise to before forming terminal branches?
Each cord gives rise to a variable number of collateral (preterminal) nerves.
Then splits into two terminal branches.
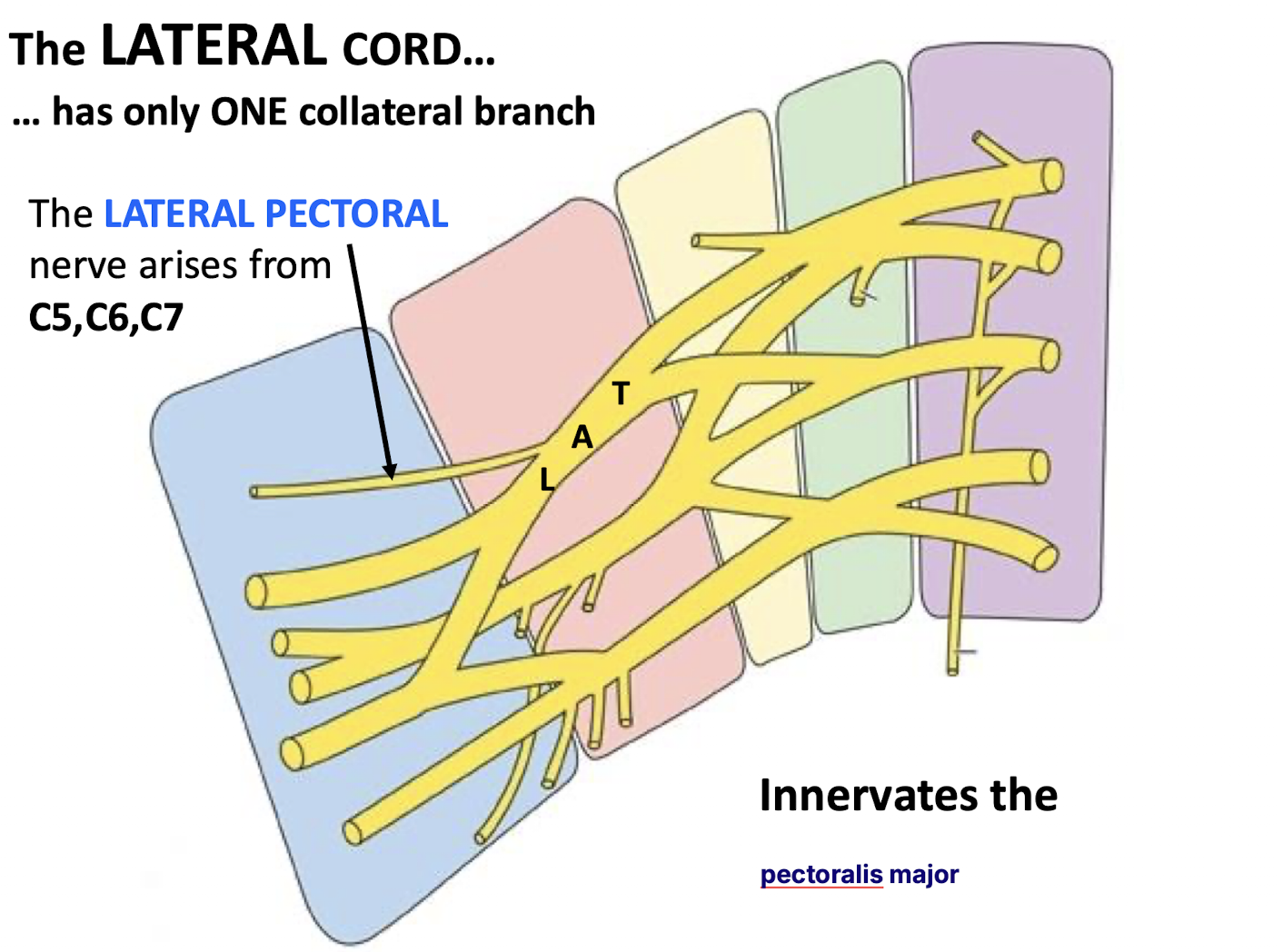
Identify the single collateral branch of the lateral cord and what it innervates. Identify the Nerve Roots associated with this nerve.
The lateral pectoral nerve (C5-C7). Innervates the pectoralis major
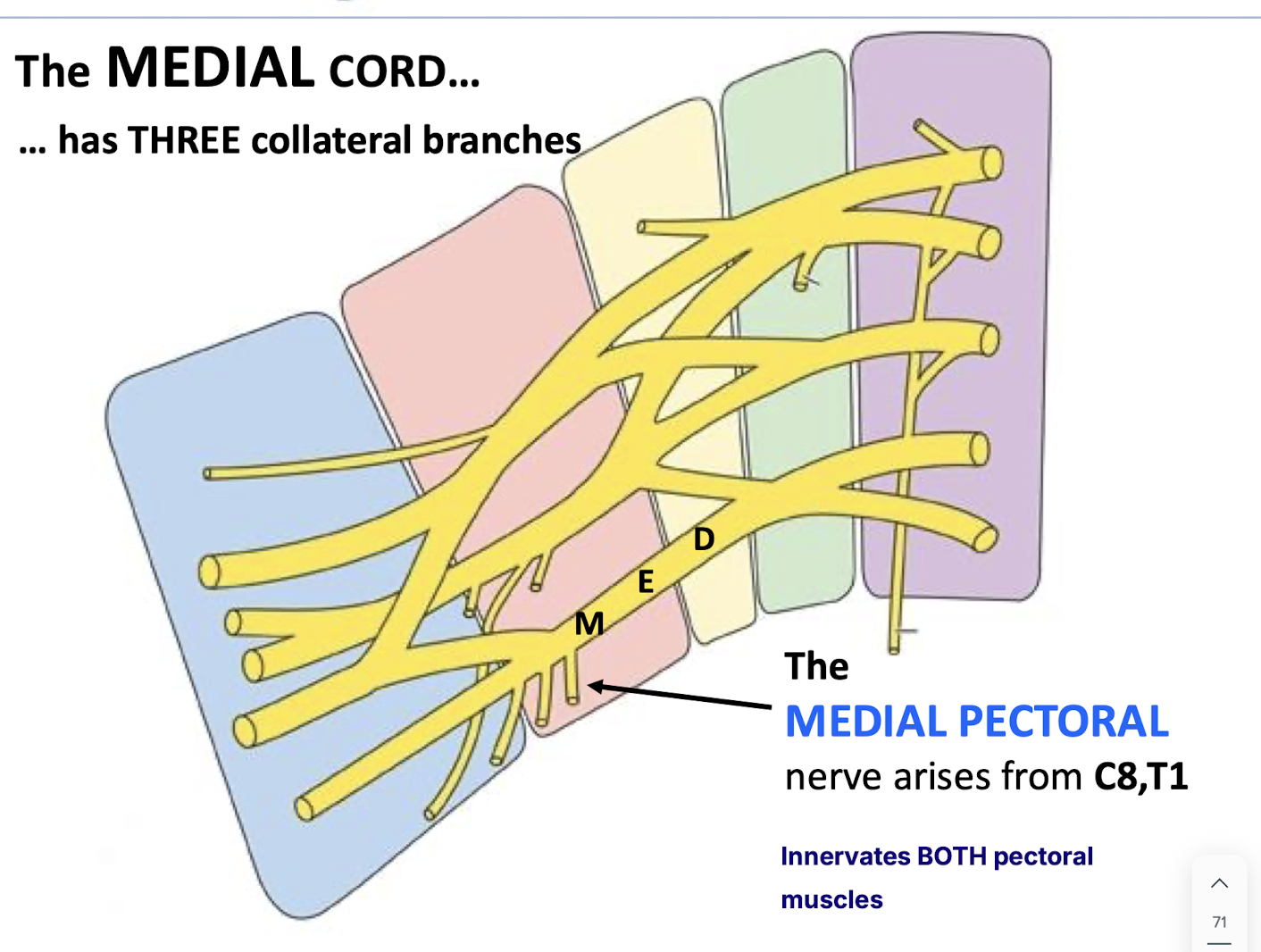
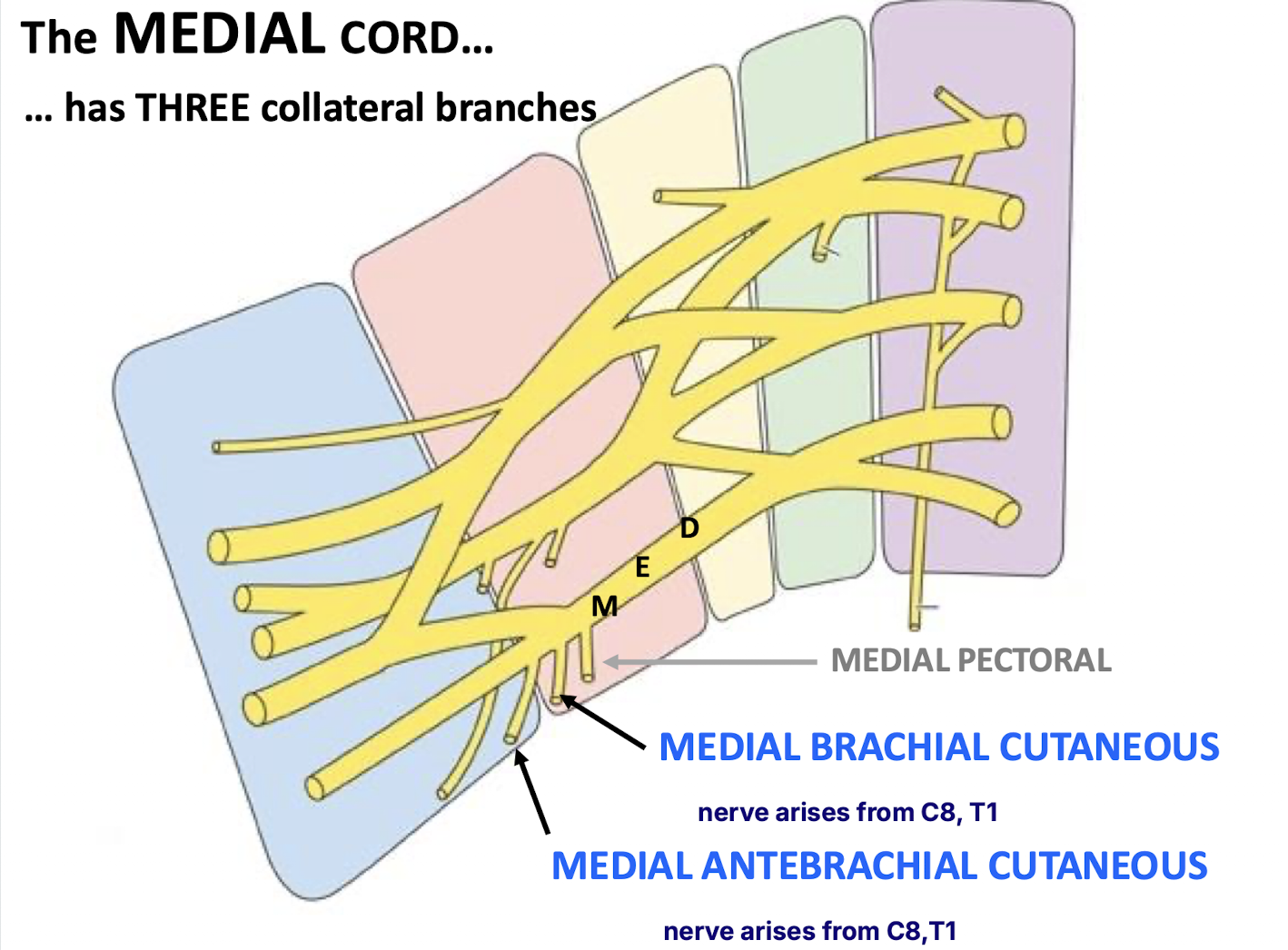
How many collateral branches does the medial cord of the brachial plexus have, and what is the origin and function of the medial pectoral nerve?
Collateral Branches: The medial cord has three collateral branches
Medial Pectoral Nerve:
Arises from C8–T1.
Innervates both pectoral muscles (pectoralis major and minor).
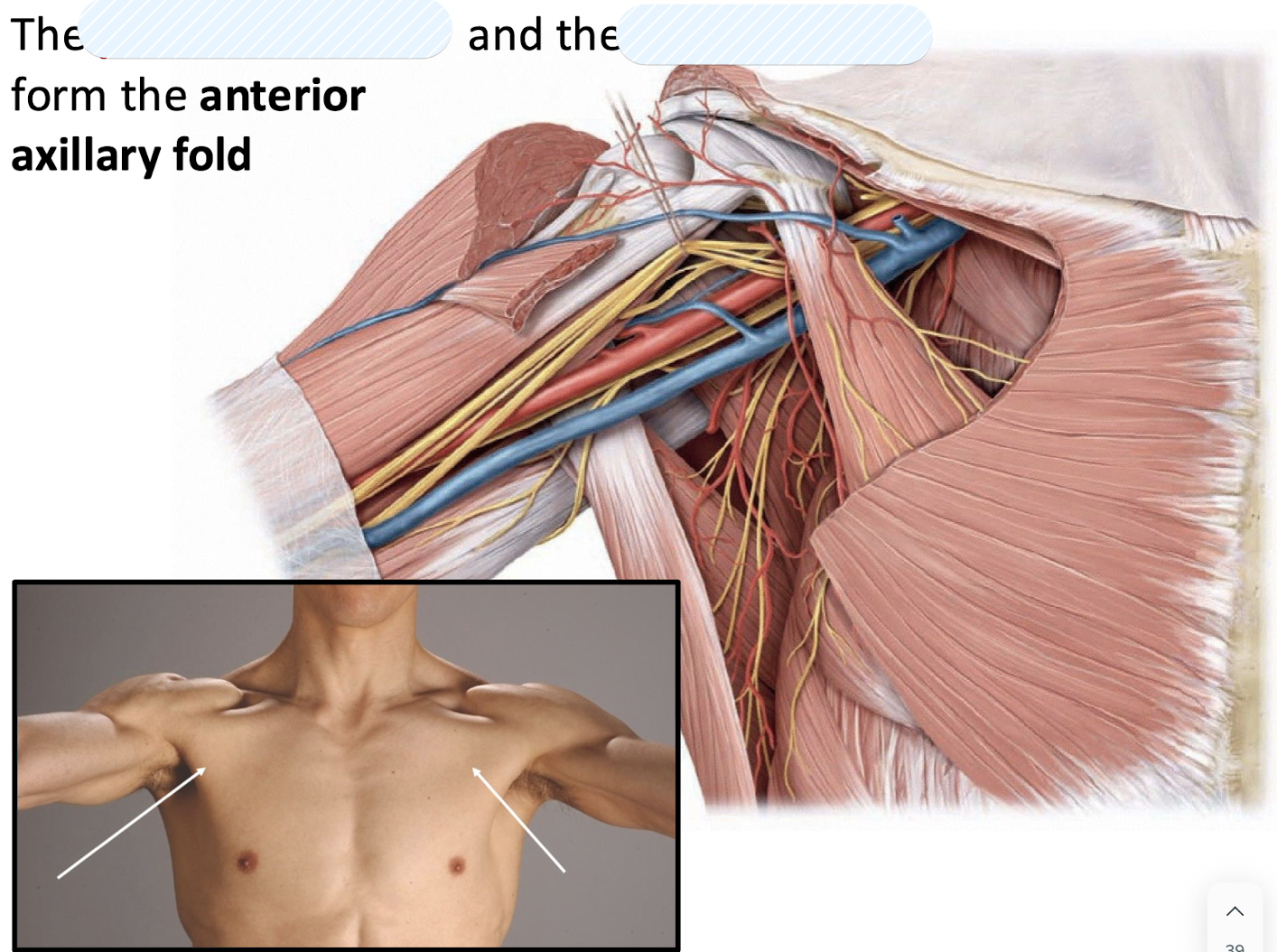
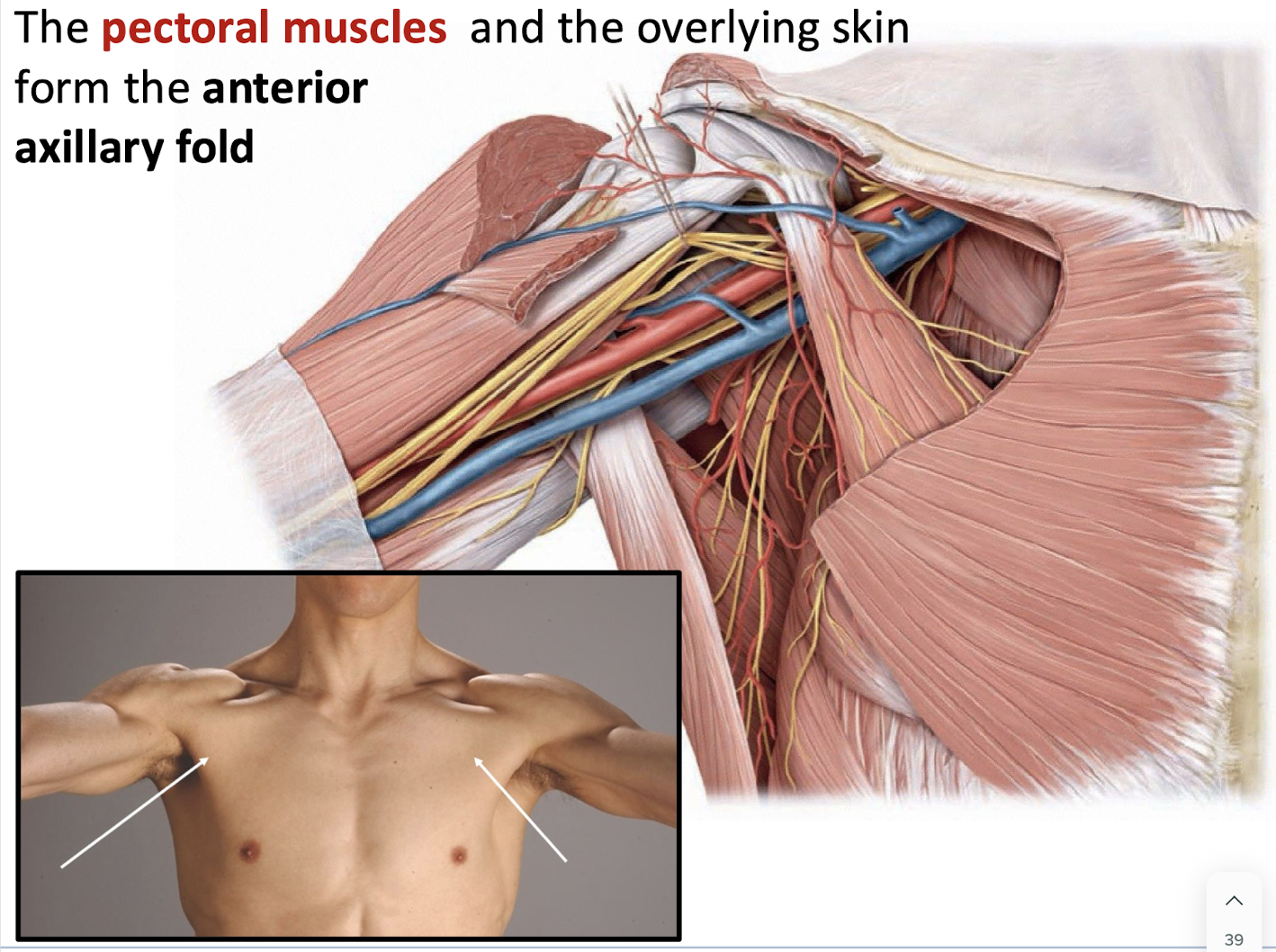
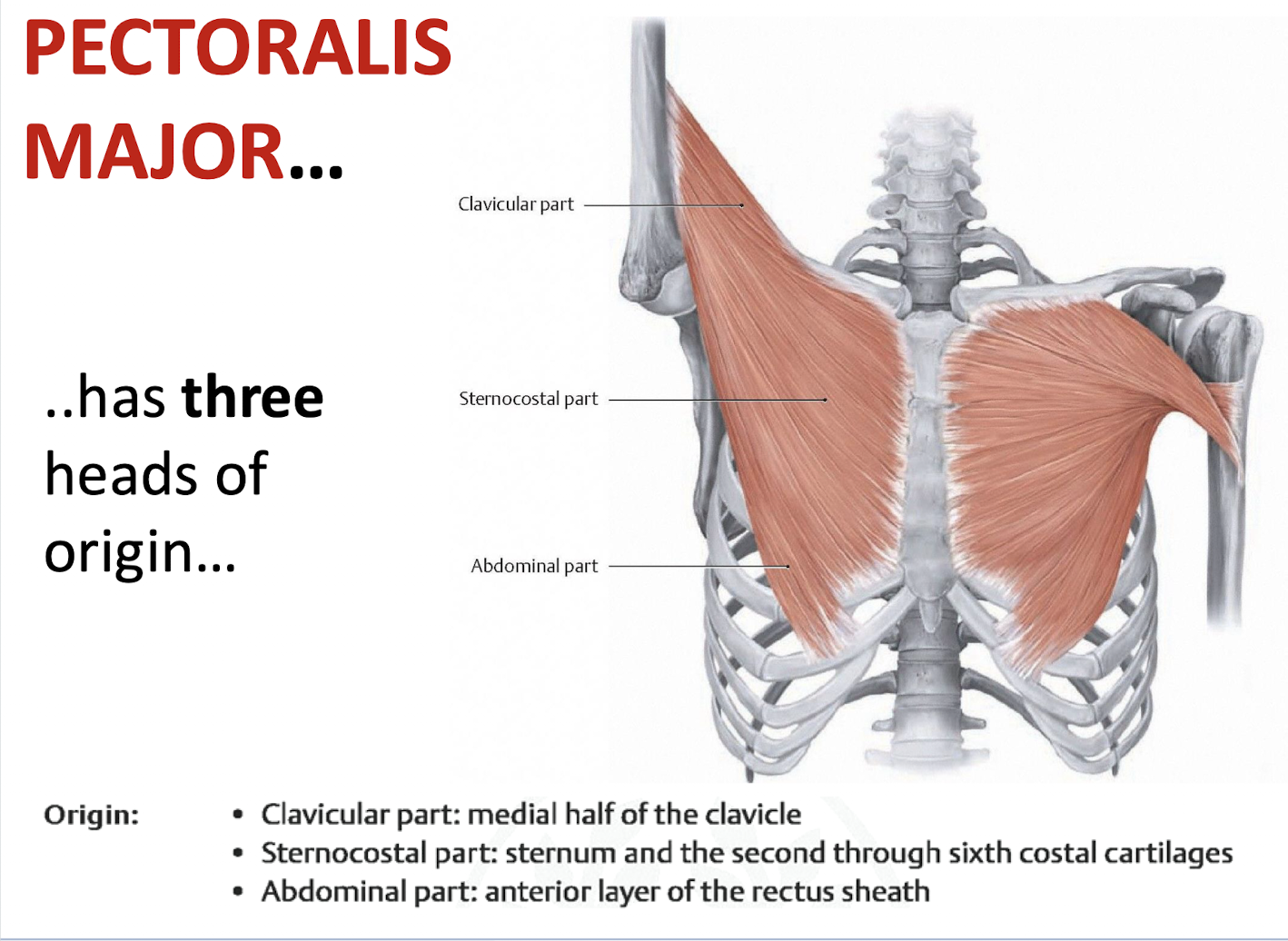
Identify the three heads of origin for the pectoralis major.
Clavicular, sternocostal, and abdominal.
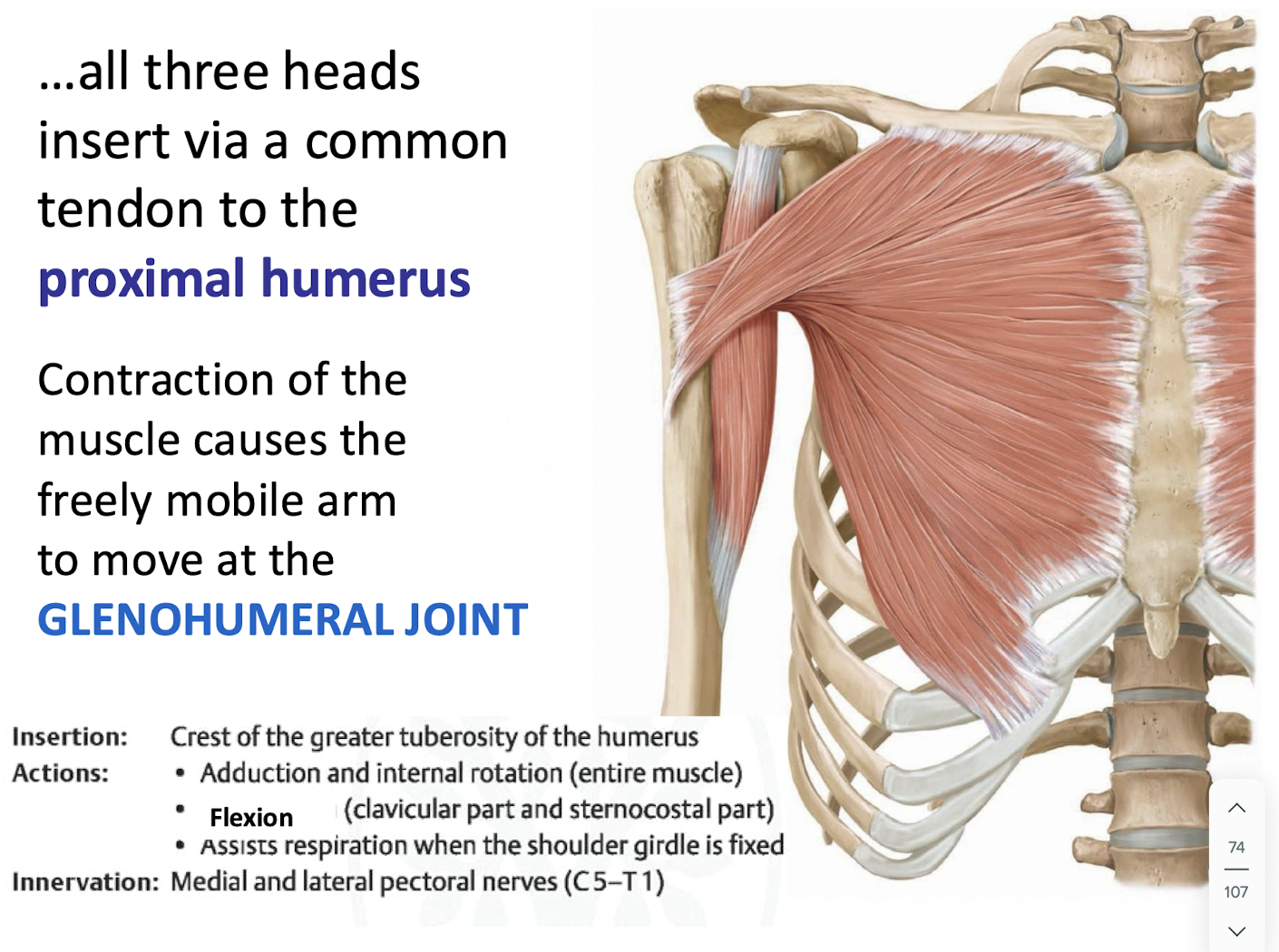
What is the insertion and action of the pectoralis major muscle
Insertion: All three heads insert via a common tendon on the proximal humerus.
Action: Contraction moves the freely mobile arm at the glenohumeral joint.
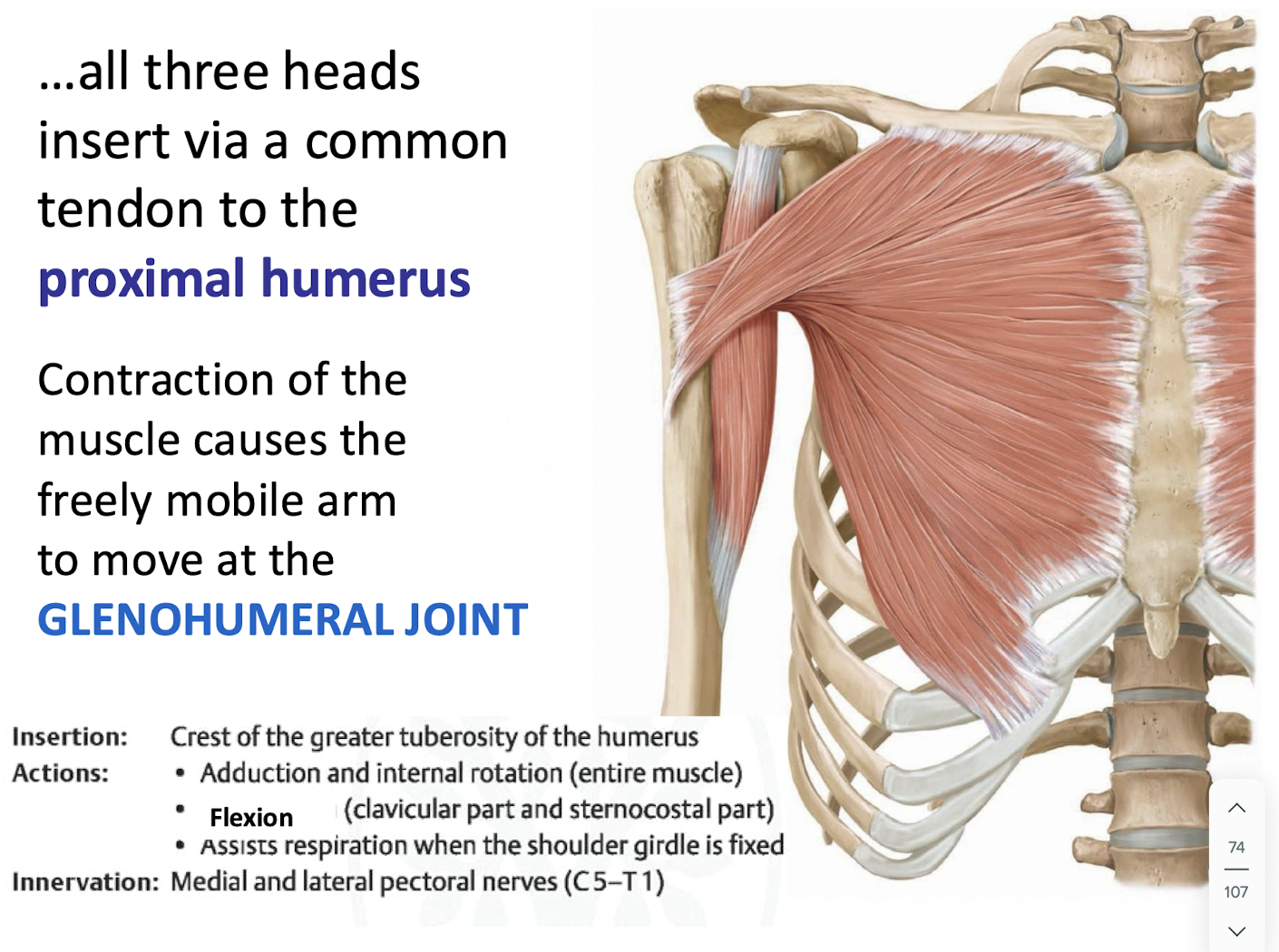
Where does the pectoralis major insert?
The crest of the greater tuberosity of the humerus.
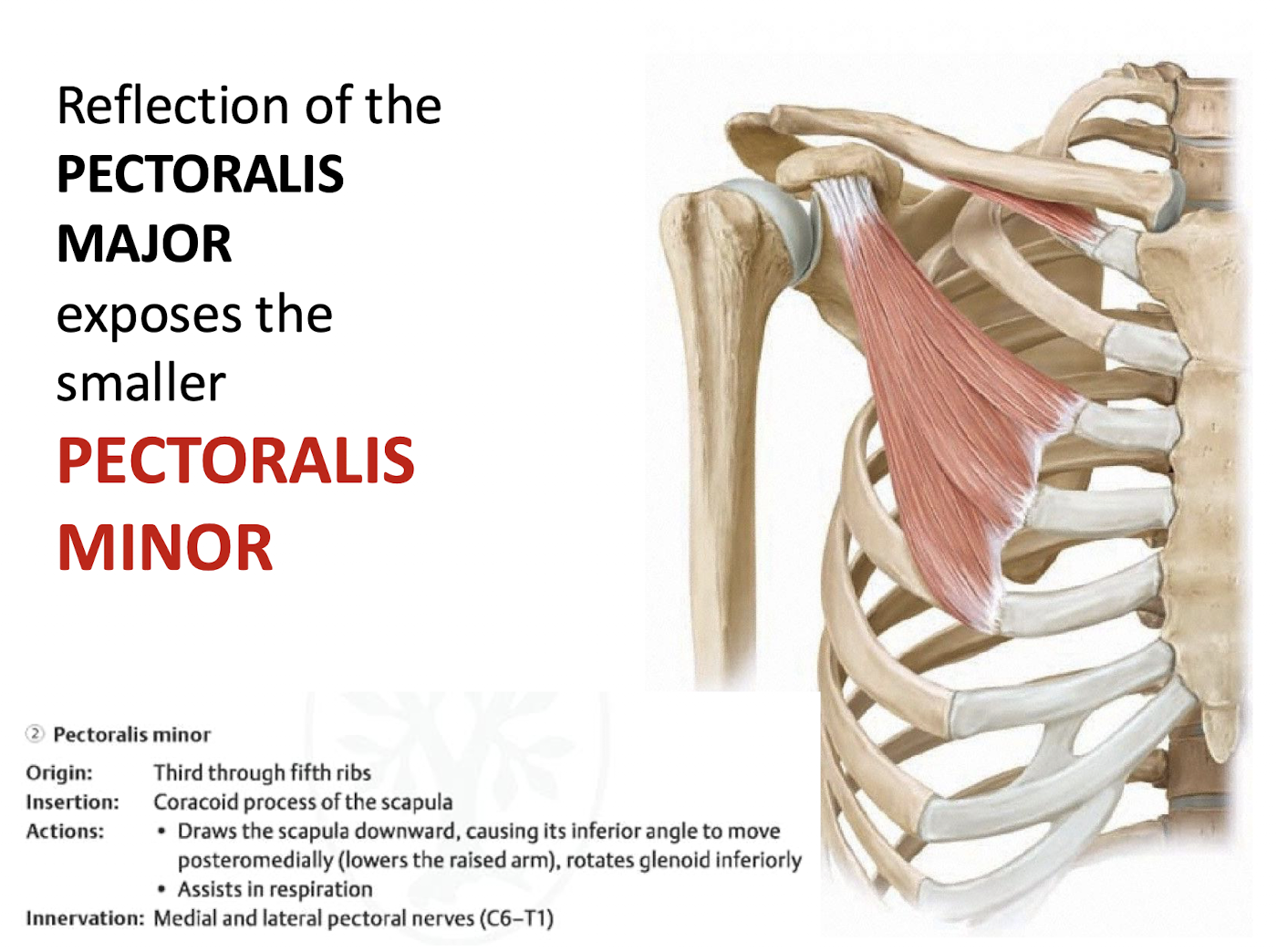
What are the actions of the pectoralis minor?
It draws the scapula downward, rotates the glenoid inferiorly, and assists in respiration.
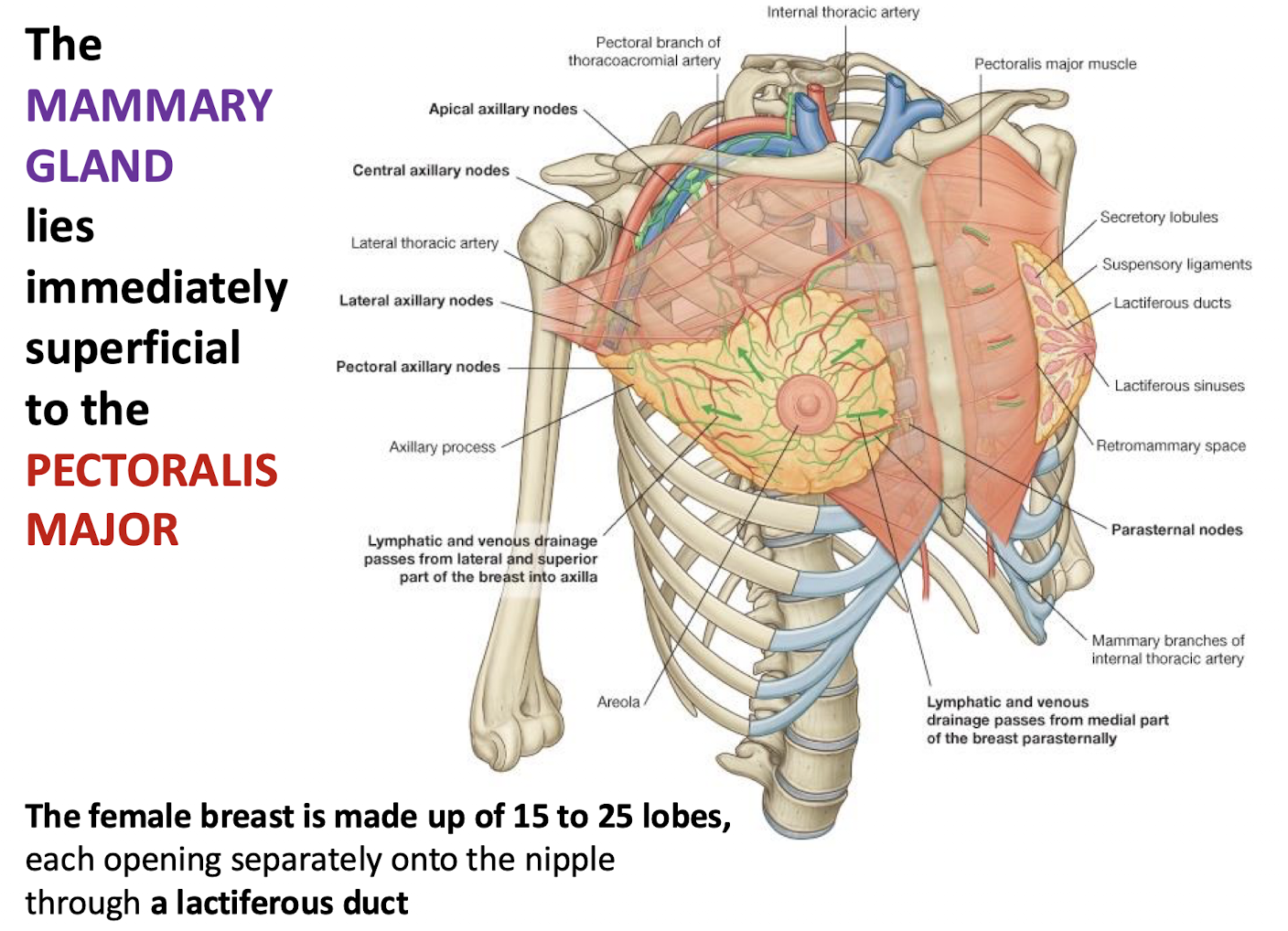
Where is the mammary gland located, and how is the female breast structured?
Location: The mammary gland lies immediately superficial to the pectoralis major muscle.
Structure: The female breast consists of 15–25 lobes, each opening separately onto the nipple through a lactiferous duct.
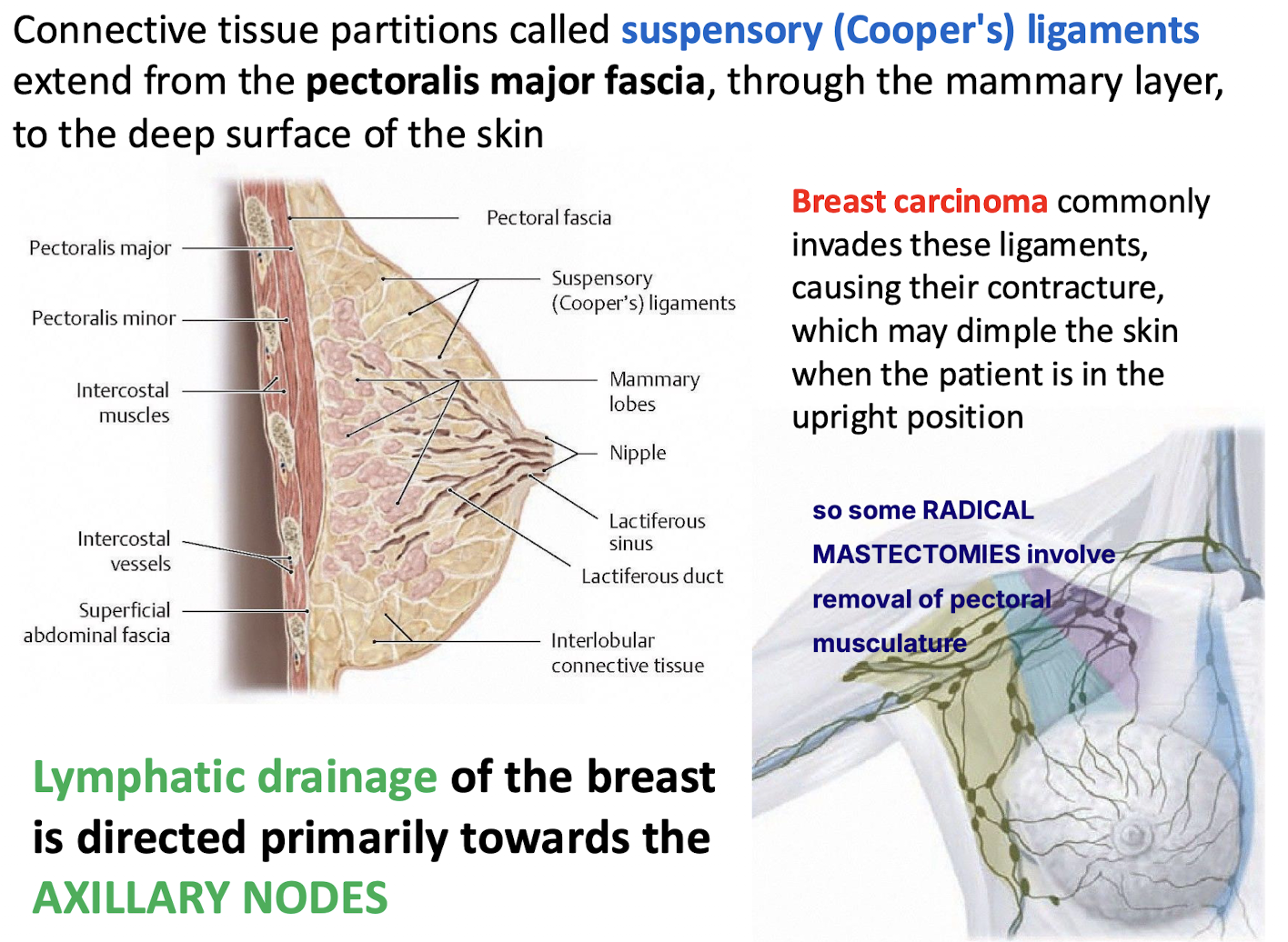
Which structures connect the mammary layer to the skin and can cause dimpling in carcinoma?
Suspensory (Cooper's) ligaments.
Extend from pectoral fascia → through mammary layer → deep surface of skin.
Breast carcinoma often invades these ligaments, causing contracture and skin dimpling (especially upright).
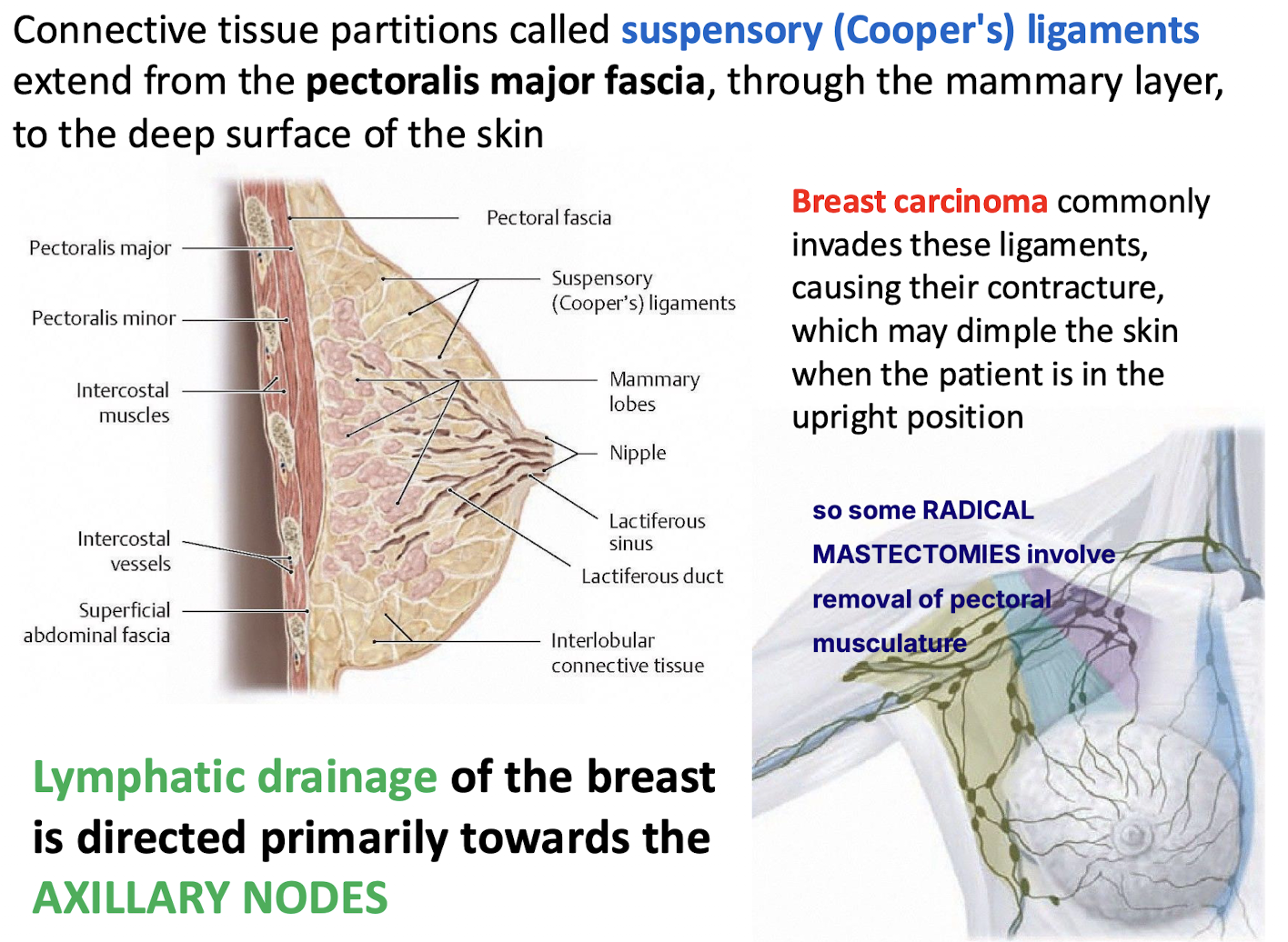
Where is the majority of the breast's lymphatic drainage directed?
Towards the axillary lymph nodes.
Some radical mastectomies involve removal of pectoral musculature due to lymphatic spread.
How many collateral branches does the medial cord of the brachial plexus have, and what are they?
The medial cord has three collateral branches:
Medial Pectoral Nerve (C8–T1) – innervates both pectoral muscles.
Medial Brachial Cutaneous Nerve (C8–T1) – sensory to medial arm.
Medial Antebrachial Cutaneous Nerve (C8–T1) – sensory to medial forearm.
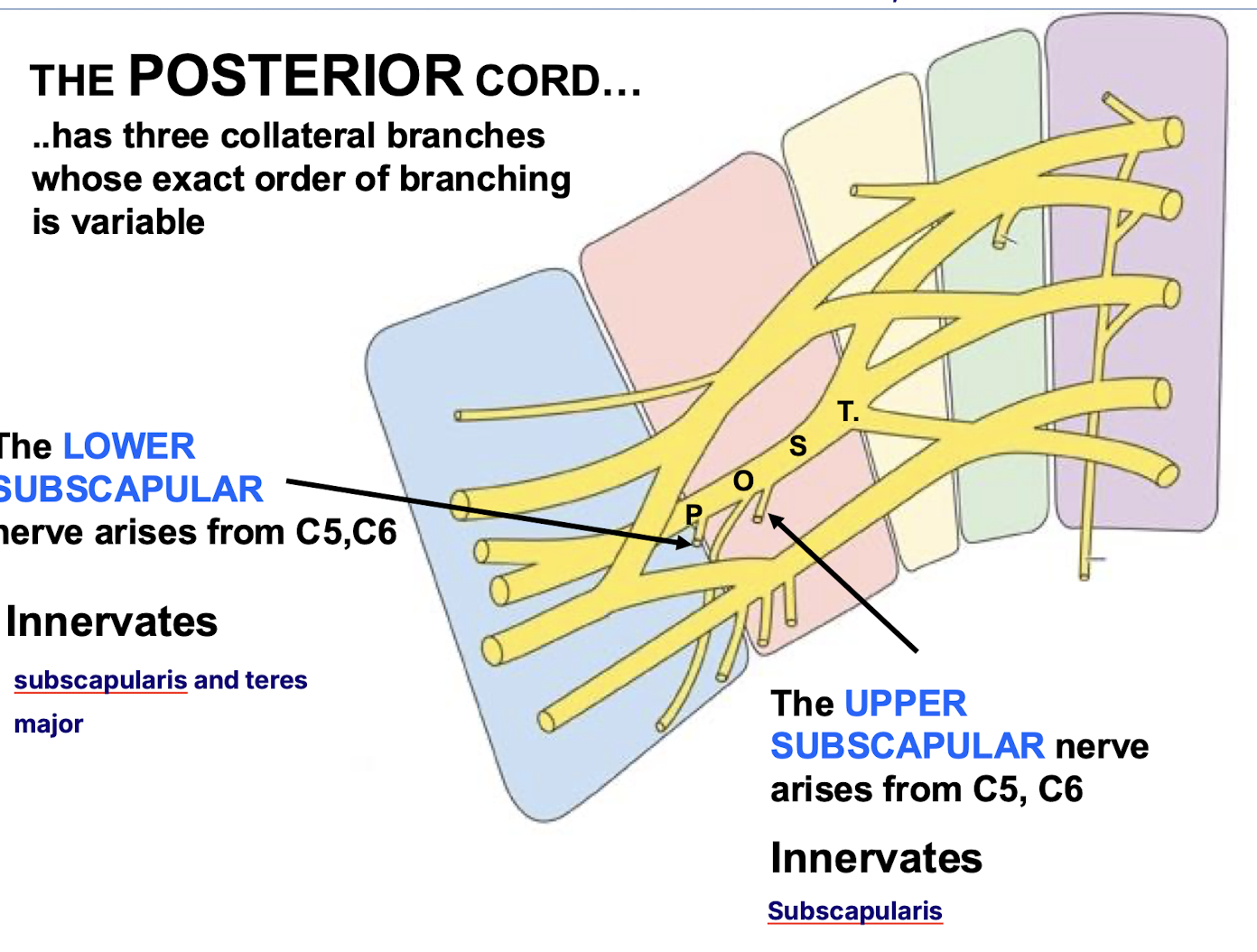
Identify the three collateral branches of the posterior cord.
The upper subscapular (C5,C6), lower subscapular (C5,C6) and thoracodorsal (C6,C7,C8) nerves.
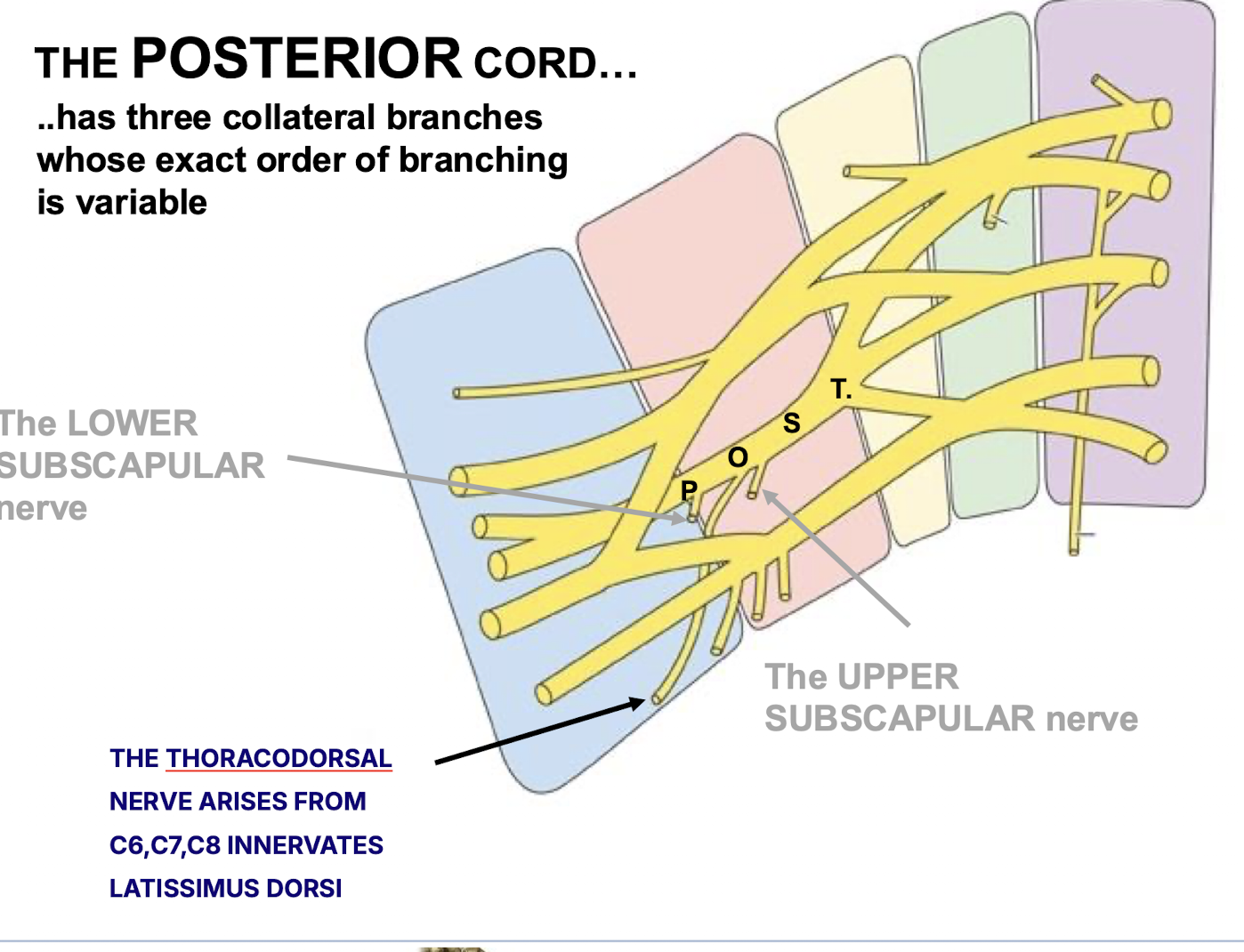
Which muscles are innervated by the lower and upper subscapular nerves from C8-T1?
Upper Subscapular: subscapularis
Lower Subscapular: subscapularis and teres major.
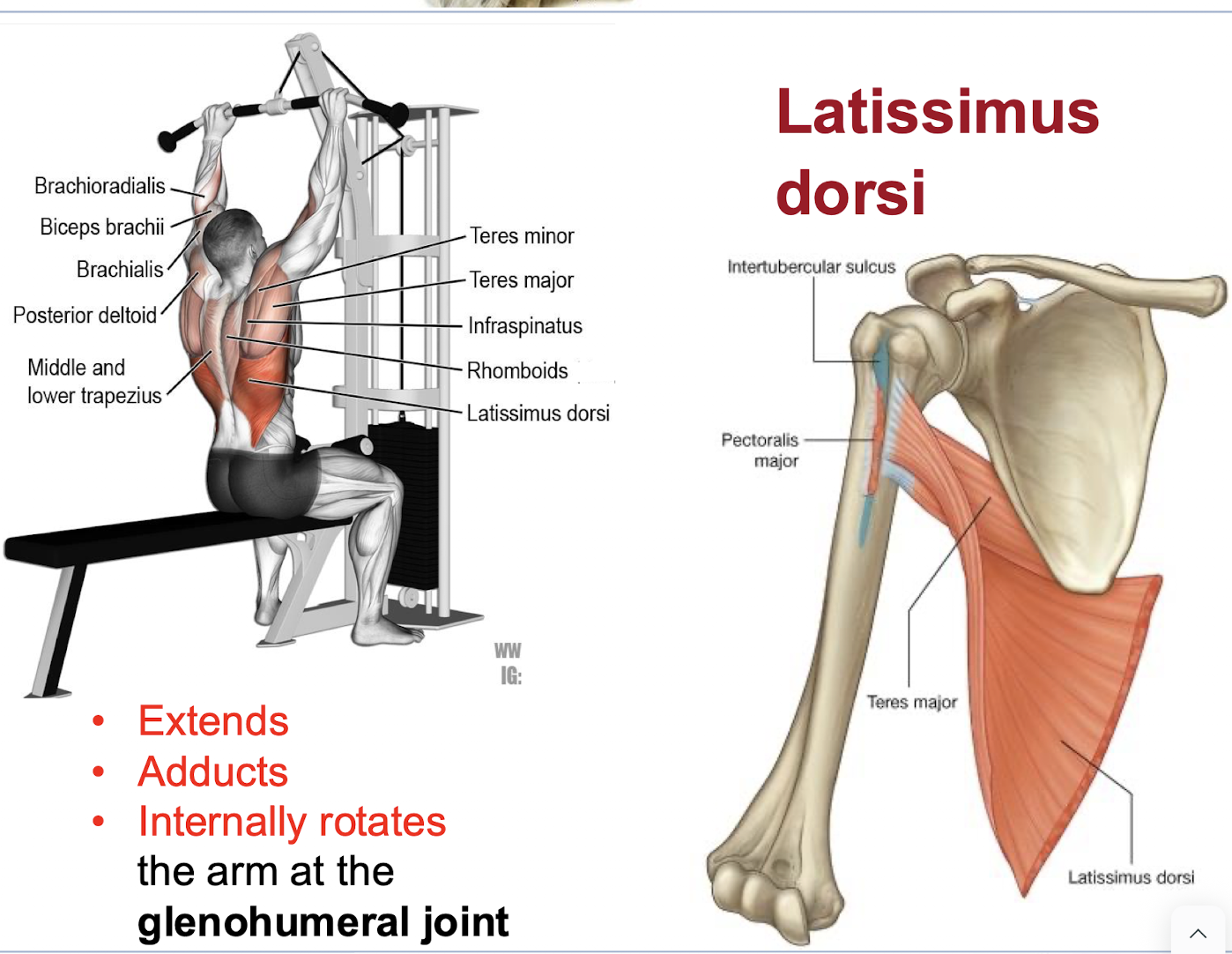
What are the actions of the latissimus dorsi?
It extends, adducts, and internally rotates the arm AT THE GLENOHUMERAL JOINT.
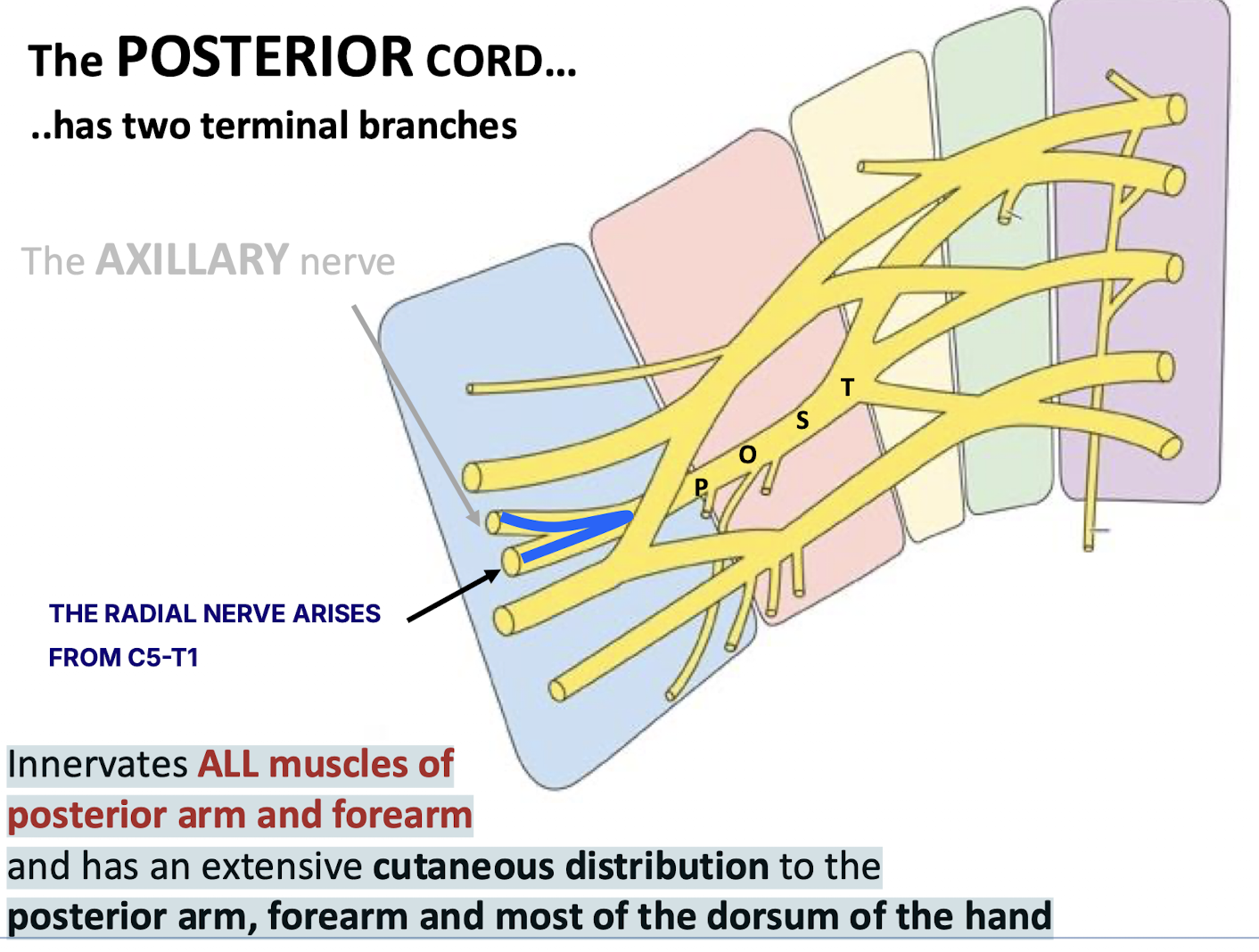
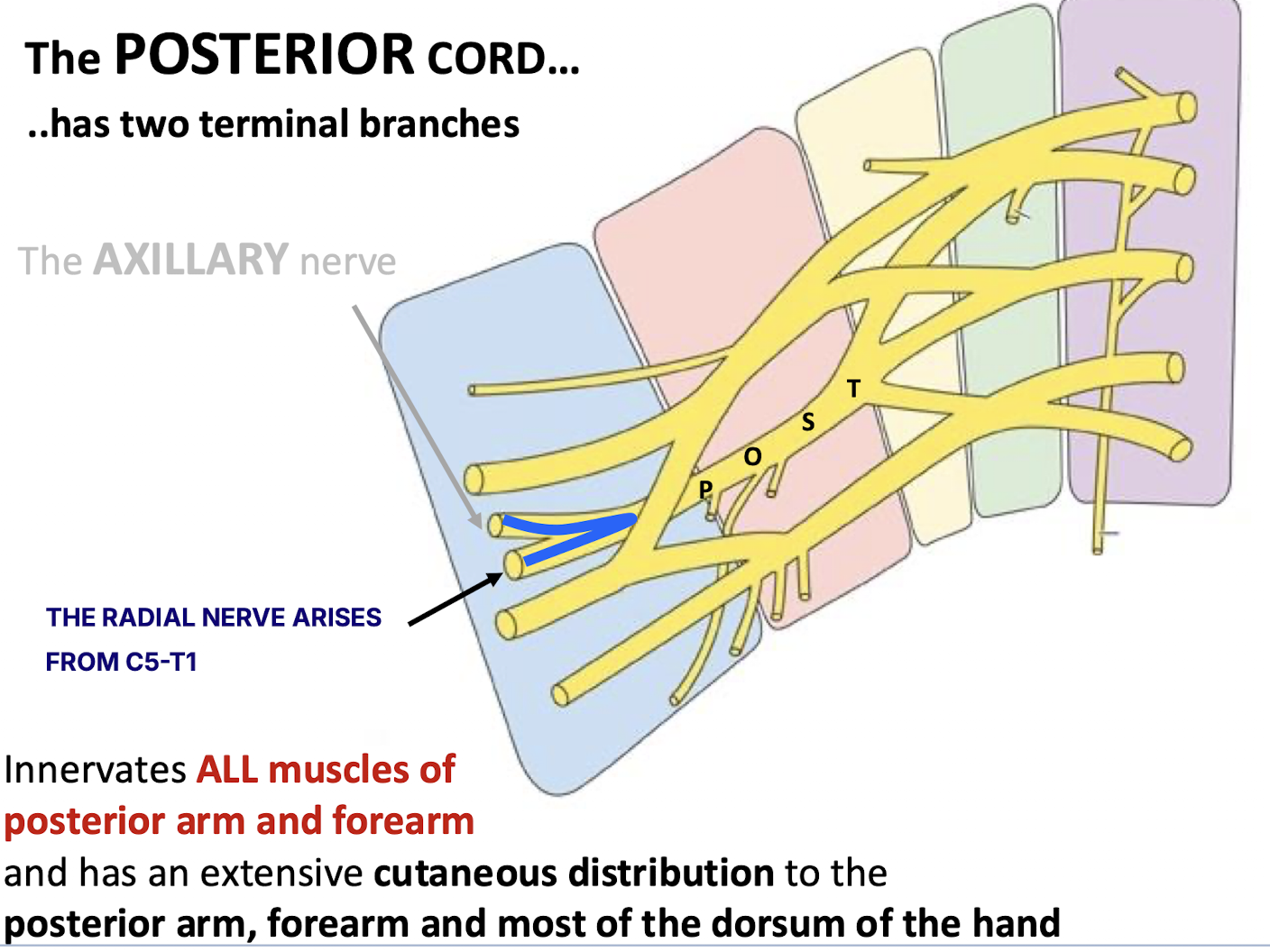
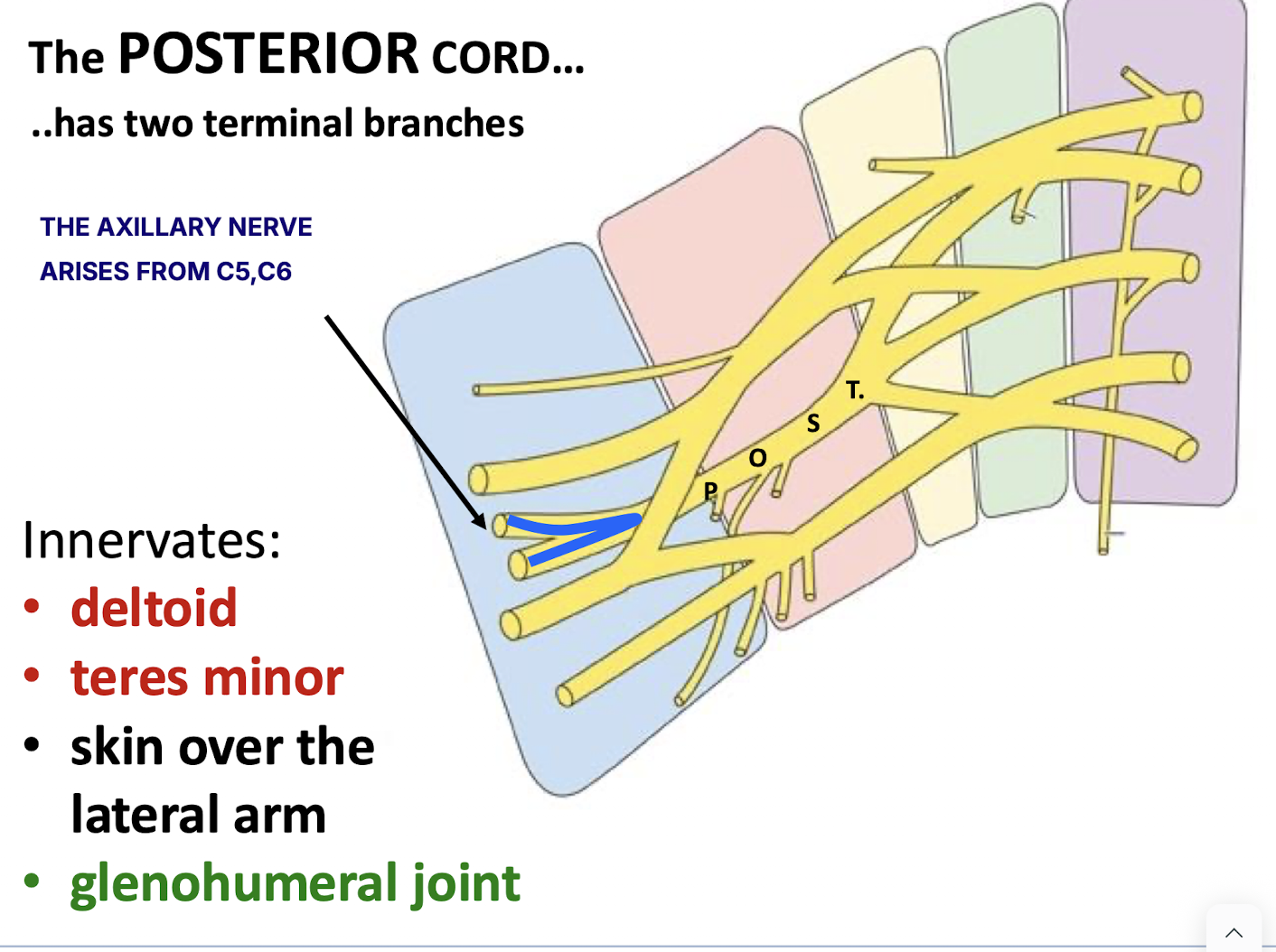
Identify the two terminal branches of the posterior cord. Include nerve numbers
The axillary nerve (C5,C6) and the radial nerve. (C5-T1)
radial large because it has all five roots
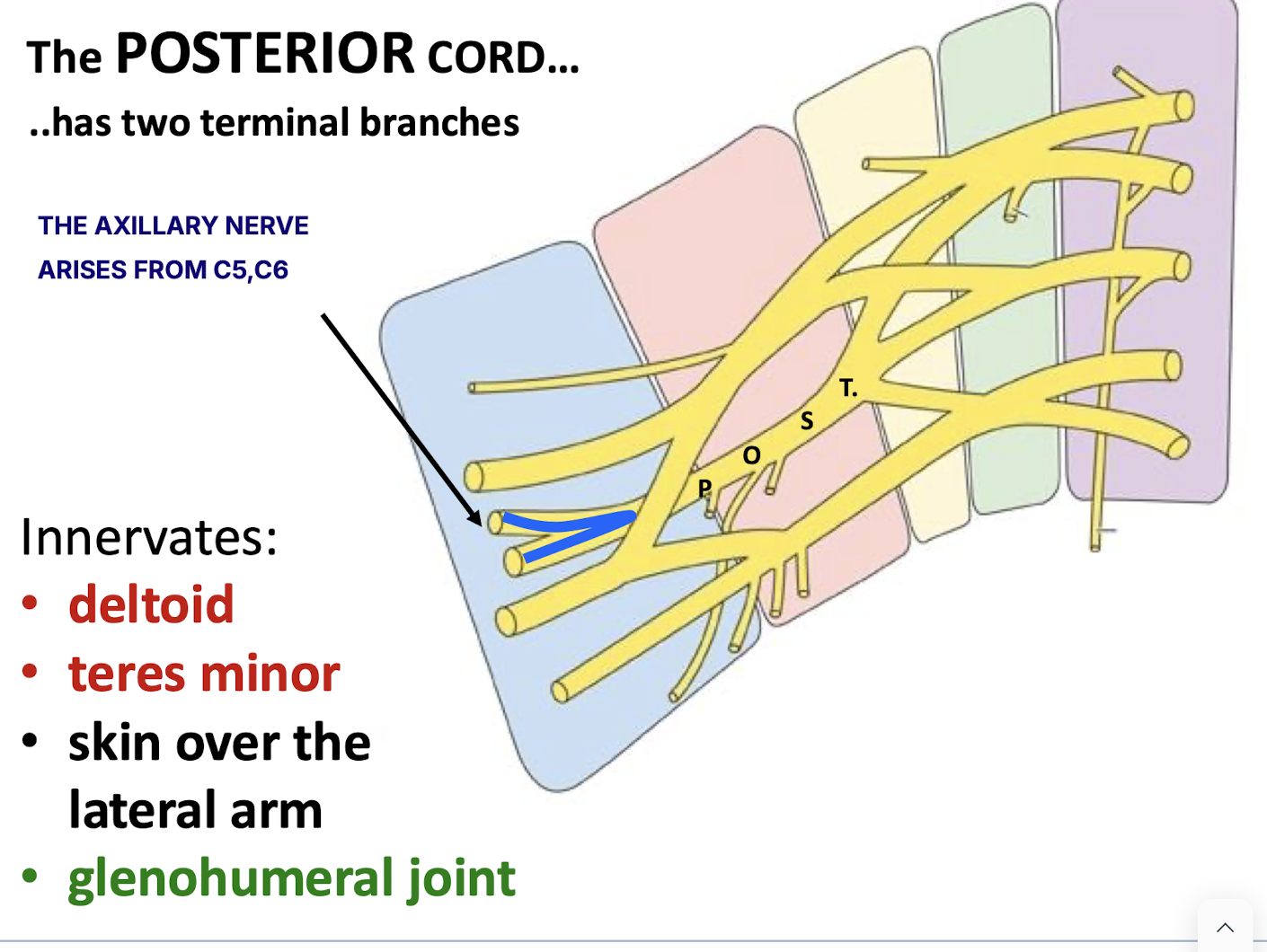
Which muscles and structures are innervated by the axillary nerve?
The deltoid and teres minor.
Skin over the lateral arm
Glenohumeral joint
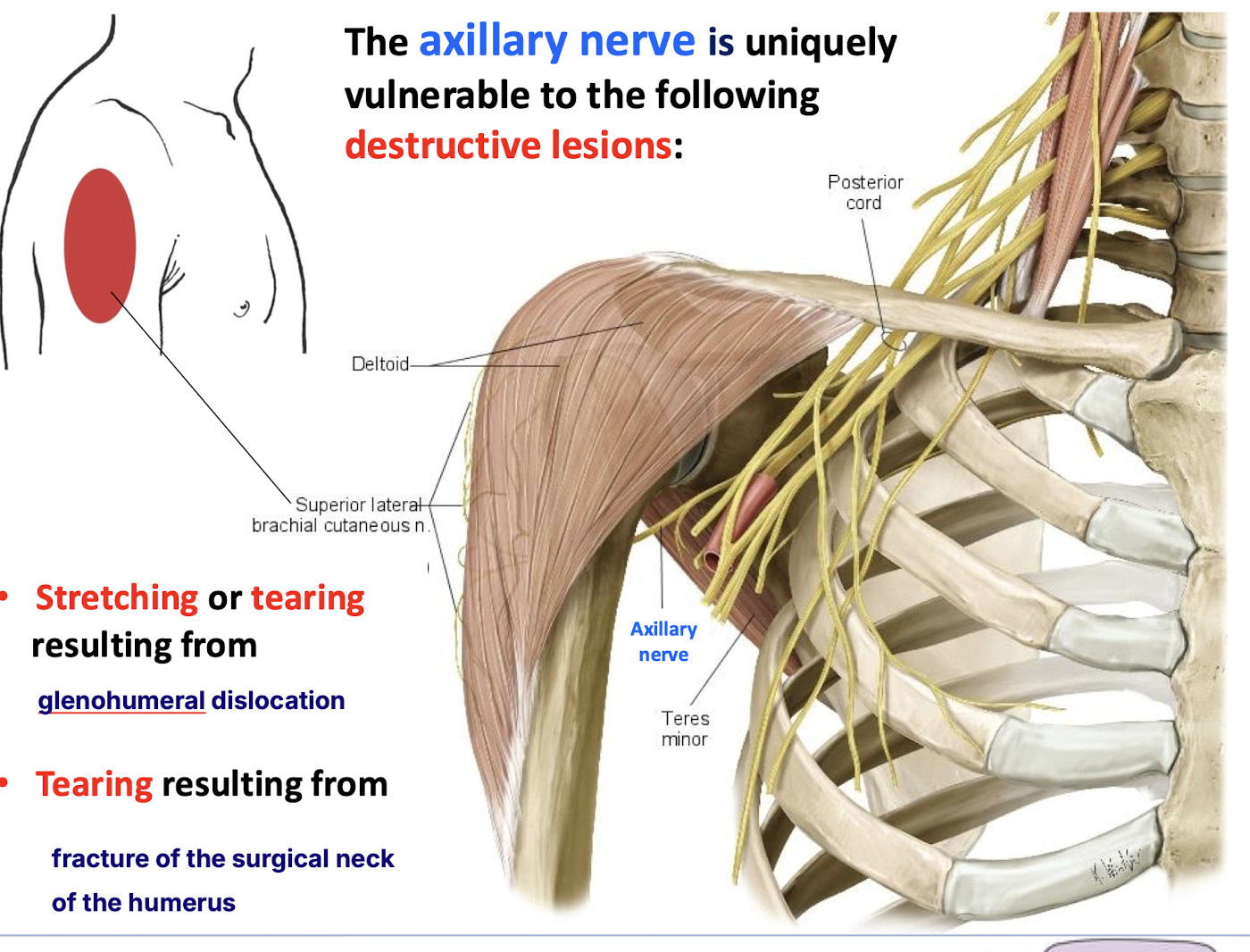
Where is the axillary nerve uniquely vulnerable to injury?
At the surgical neck of the humerus (tearing) and during glenohumeral dislocation (stretching/tearing).
What does the radial nerve innervate?
Innervates ALL muscles of posterior arm and forearm and has an extensive cutaneous distribution to the posterior arm, forearm and most of the dorsum of the hand