Biology (Topic 6) Nephron and blood water potential
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
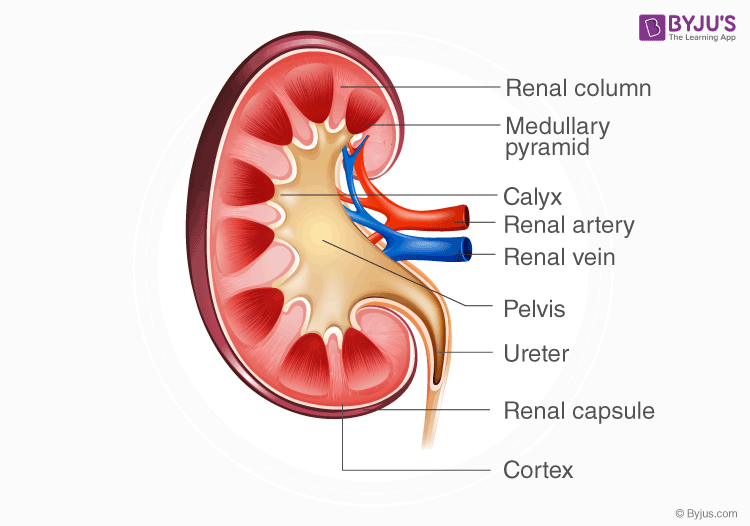
Name the structures of the kidney.
Renal cortex
Inner renal medulla
renal pelvis
Nephrons
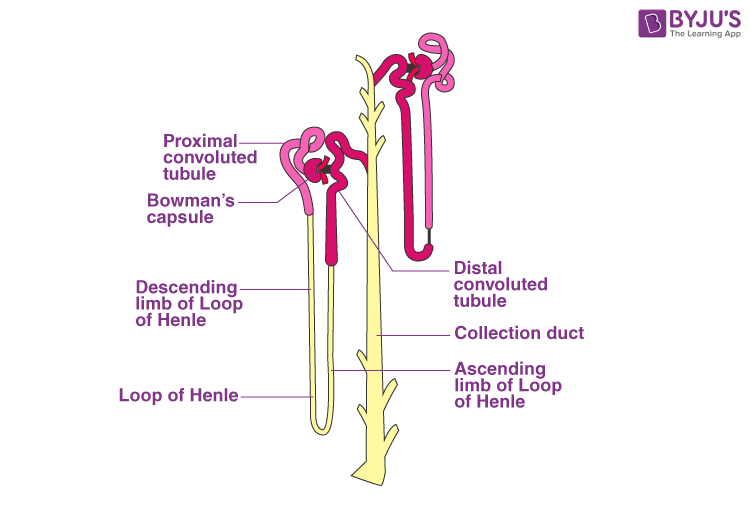
Name structures in the nephron.
Glomerulus
Bowmans capsule
Proximal convoluted tubule
Loop of Henley
Distil convoluted tubule
Collecting duct
What are the two processes that the nephron does to form urine?
Ultrafiltration
Selective reabsorption
What is ultrafiltration?
When small molecules are filtered out of the blood into the bowman’s capsule of the kidney nephron, forming glomerate filtrate
What is glomerate filtrate?
Fluid that is filtered out of the blood in the glomelurs and enters the bowman’s capsule
It is made of:
water
Glucose
Amino acids
Ions
Small hormones
Urea
What is selective reabsorption ?
When useful molecules are taken back from the filtrate and released into the blood
Includes :
Water
Glucose
Ions
(in the proximal convlutedtubels
What are arterioles?
Small blood vesicles that branch off the renal artery and supply blood to each nephron
What is an afferent arteriole?
Small arteriole that brings blood into the artery from the glomerulus (they have a larger diameter)
What are efferent arterioles?
Small arterioles that bring blood away from the glomerulus (they have a smaller diameter)
Why is there high hydrostatic pressure in the glomlurous?
Efferent arterioles have a narrower diameter than those of afferent arterioles
How is glomerate filtrate formed?
High hydrostatic pressure causes smaller molecules to be forced out of the capillaries of the glomerulus into the bowman’s capsule (because of the change in the diameter from afferent to efferent arteriole)
What remains in the blood after ultrafiltration?
Blood cells and large protines as they are too large to be forced out
What separates the glomerular capillaries from the lumen and the bowman’s capsule?
Capillary endothelium , basement membrane and epithelial cells
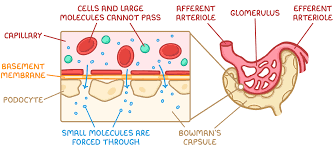
What about the capillary endothelium allows filtration?
Gaps between endothelial cells allows small molecules to pass through
What about the basement membrane allows for filtration?
Collagen and glycoproteins stop large molecules and allows small molecules to pass through
What about the epithelial cells allows for filtration?
Gaps between Podocytes
Where does most abortion of water occur?
Proximal convoluted tubule , loop of Henley and collecting duct
How are the epithelial cells on the lining of the proximal convoluted tubule adapted for reabsorption?
They have:
Fold in membrane making microvilli (increase the surface area)
Co transport protines (increase permeability of membrane , allowing glucose and amino acids to move against there concentration gradient)
Many mitochondria (to produce ATP used in the sodium potassium pump
What are the three ways that reabsorption occurs from the proximal convoluted tubules into the blood?
Active transport of sodium ions from proximal convoluted tubules into the blood , creating a sodium concentration gradient allowing for co transport
Co transport for glucose and amino acids to move against there concentration gradient (from filtrate into the PCT)
Water via osmosis
What are passive movements of substances from the proximal convoluted tubes into the blood?
Chloride ions: diffuse after sodium due to the electrochemical gradient.
Water: moves by osmosis as solute reabsorption lowers water potential.
Urea: diffuses down its concentration gradient as its filtrate concentration increases.
Where does the reabsorption of water and salt occur?
Proximal convoluted tubule , loop of Henley and collecting duct
What surrounds the loop of Henley?
medulla
What occurs at the ascending limb of the loop of Henley?
Sodium and chloride ions are pumped out of the limb to the medulla . This causes the water potential of the medulla to decrease allowing water in the descending limb to leave
why does water not move into the ascending limb?
The ascending limb of the loop of Henle is impermeable to water, so water cannot leave or enter by osmosis.
Why does water move out of the descending limbs? where does it go?
The descending limb is permeable to water, so water leaves the filtrate by osmosis into the surrounding tissue fluid and then into the capillaries.
Tissue fluid in the medulla has a lower water potential than in the filtrate
What is osmoregulation and what is it an example of?
Example of homeostasis
Osmoregulation is the process by which organisms regulate the water potential of the blood and tissue fluid by controlling water and ion levels
How does the loop of Henley decrease the water potential of the medulla?
Pumps sodium and chloride ions into the medulla decreasing the water potential
Why is water reabsorbed from the proximal convoluted tubule ?
Loop of Henley decreases the water potential in the renal medulla so water can move down the water potential gradient
What are osmoreceptors? Where are they located?
Receptors located in the hypothalamus that monitor the water potential of blood
What happens to osmoreceptors when the blood water levels decrease?
Osmoreceptors shrink as water leaves them by osmosis (because blood water potential is low). This stimulates the hypothalamus, which signals the posterior pituitary to release ADH.
After osmoreceptors shrink , what does the hypothalamus signal ?
Osmoreceptors shrink stimulating the hypothalamus, which signals the posterior pituitary to release ADH.
What happens when there is high blood water content?
Osmoreceptors swell as water enters them by osmosis when blood water potential is high. This reduces stimulation of the hypothalamus, so the posterior pituitary releases less ADH
What is ADH and what does it stand for?
Antidiuretic Hormone
ADH is a hormone that increases the permeability of the distal convoluted tubule and collecting duct to water, allowing more water to be reabsorbed
How does ADH increase the permeability of the cells lining the collecting duct?
ADH binds to receptors on the cells lining the collecting duct. This causes vesicles containing aquaporins to fuse with the cell membrane. The increased number of aquaporins makes the collecting duct more permeable to water.
What happens when a high water potential / water content has been detected
Osmoreceptors in the hypothalamus detect the rise in blood water potential (blood becomes more dilute).
Water enters the osmoreceptors by osmosis, causing them to swell.
This reduces their stimulation of the hypothalamus, so fewer nerve impulses are sent to the posterior pituitary.
The posterior pituitary releases less ADH into the bloodstream.
Lower ADH levels make the distal convoluted tubule and collecting duct less permeable to water (fewer aquaporins inserted).
Less water is reabsorbed, so more dilute urine is produced,