Medical Imaging Exam 1
1/163
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
164 Terms
Why are more dense objects white on x-ray films?
More X-rays reaching film --> more dark
More dense --> less x-rays reaching film--> more white
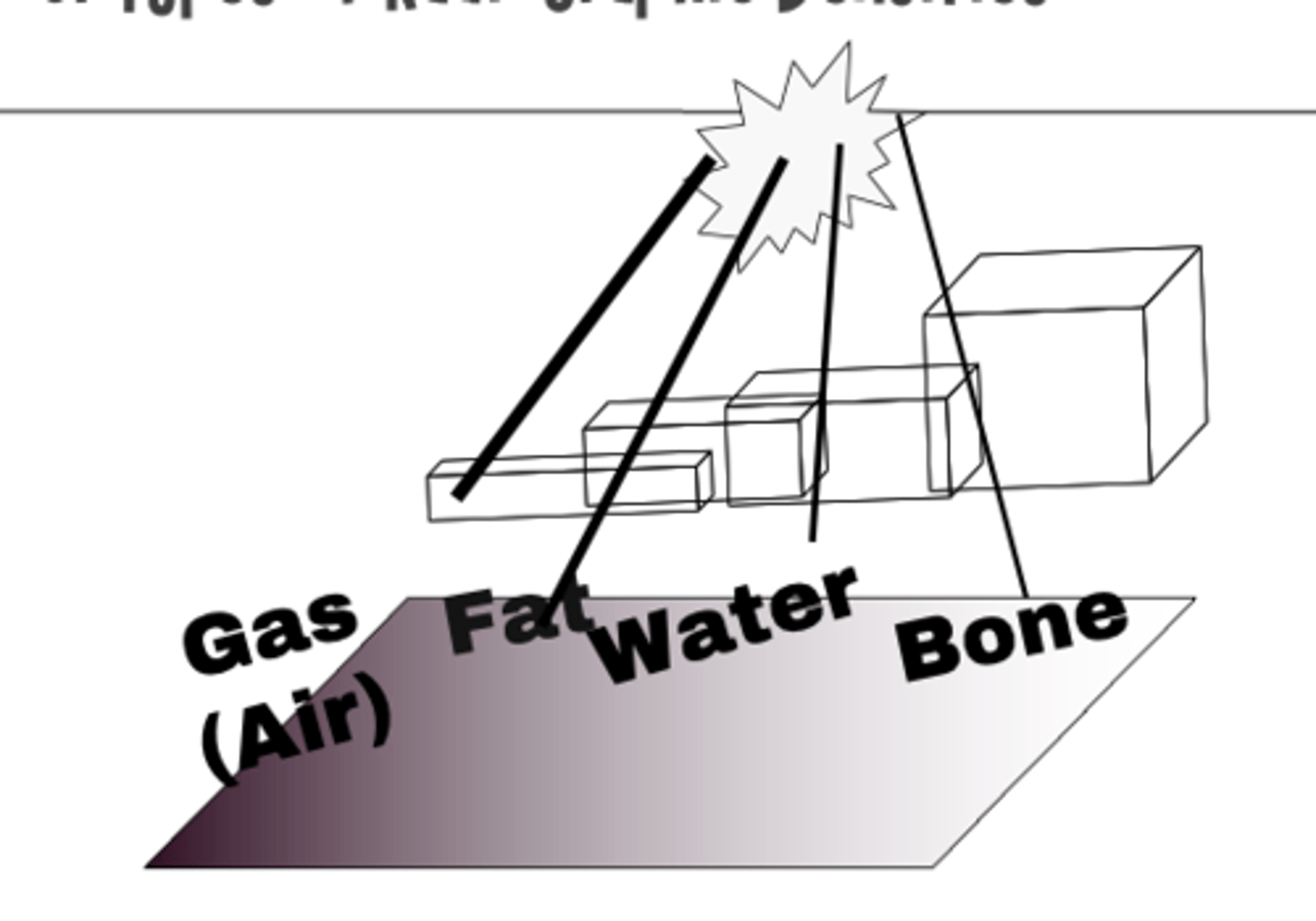
Order from least dense to most dense (gas, fat, water, bone)
(least) gas → fat → water → bone (most)
What 4 factors affect image quality?
⚬Thickness of the body part
⚬Motion
⚬Magnification
⚬Distortion
What are distortion and magnification?
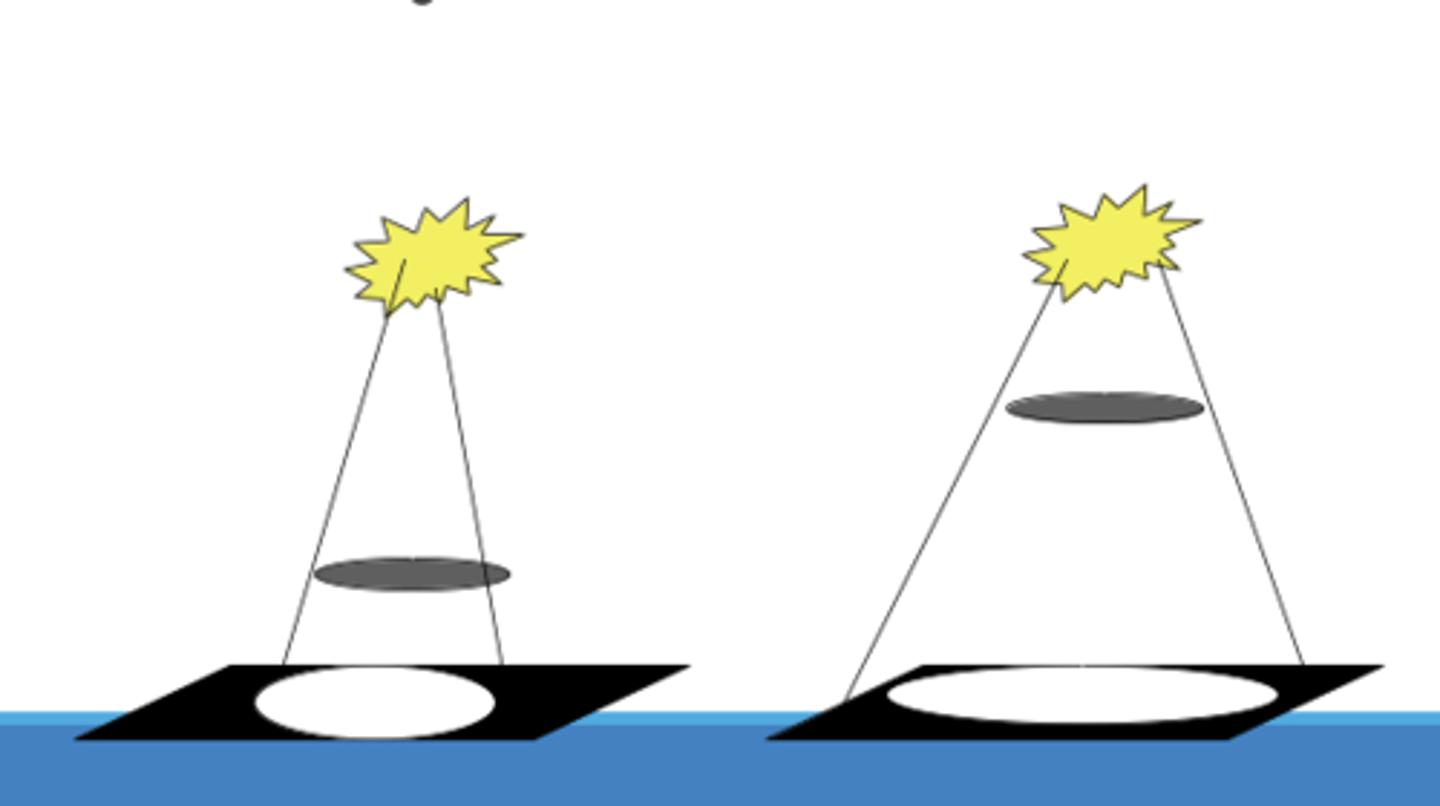
•Magnification: As an object moves toward the source of the x-ray beam, its shadow becomes larger
•Distortion occurs when the object is not perpendicular to the x-ray beam
What is the most common diagnostic x-ray format? What are two variations?
plain films
Fluorosopy and tomography
When is fluoroscopy used?
•Uses an X-ray tube and a fluorescent screen
•Used for watching real-time motion
•Used for viewing motion of the heart, diaphragm, esophagus or abdomen
⚬Can also be used for guided placement of GI tubes
When should you use contrast?
•Contrast agents are often used with plain films to highlight adjacent structures of similar densities
•Indications – Plain films - evaluation of GI tract, urinary system or blood vessels.
What is tomography? what is it used for?
•X-ray tube and film move synchronously around a focal point
•Objects in the focal point remain in focus, but other aspects are blurred
•Images are slices of the area scanned
•Most useful in evaluating the lungs, kidneys, and bony structures
What is computerized tomography? What are indications
•X-ray beam and detector system move in a 360 degree arc around the organ
•A very fine x-ray beam is directed through the patient to the detector system
•The detector system measures the amount of radiation passing through the patient
The data is analyzed and varying shades of gray are assigned to different radiation level
•Indications - evaluation of internal organs, infections, injuries, masses, and suspected tumors
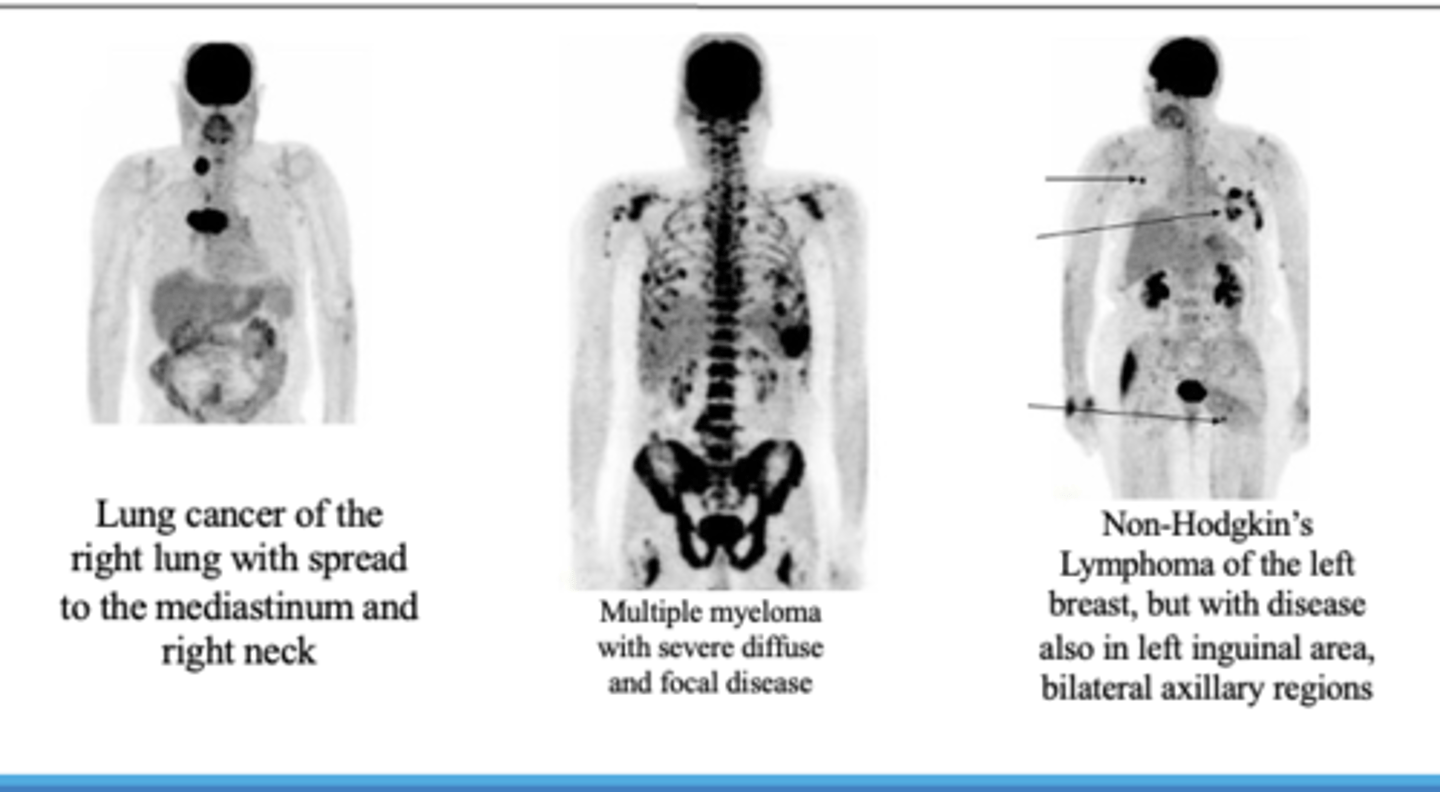
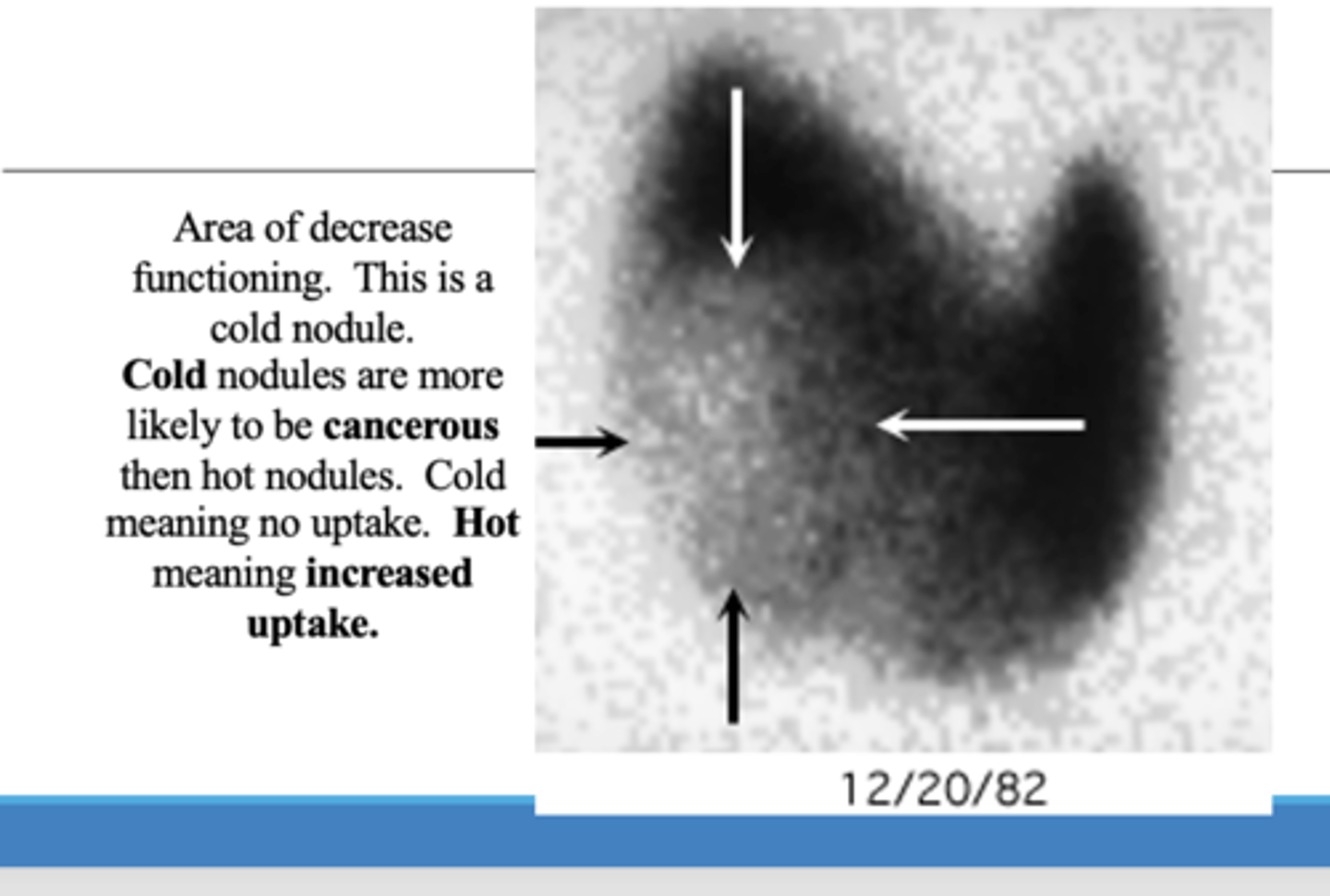
What is the radioisotope used for nuclear imaging radionuclide scans? What are nuclear imaging scans used for?
Technetium-99. Evaluate physiology of organs such as bone, heart, lungs, thyroid and kidneys
What are PET scans used for?
•PET scan measures important body functions, such as blood flow, oxygen use, and glucose metabolism
•PET can be used to evaluate tumors and cancers, myocardial functioning and brain functioning.
What is a tagged RBC used for? How is the test performed?
•Indication
⚬Occult bleed --> slow bleed from unknown location, allows you to track where it's coming from
•How
⚬Tag RBCs with Tc99m-pertechnetate
■Once inside the cell, Tc99-pertechnetate is reduced and can not diffuse back out.
Contradindications for thyroid scan
⚬No CT scan or contrast media within the last 8 weeks.
How does a renal scan work?
⚬Kidneys absorbs the material and it is cleared by glomerular filtration
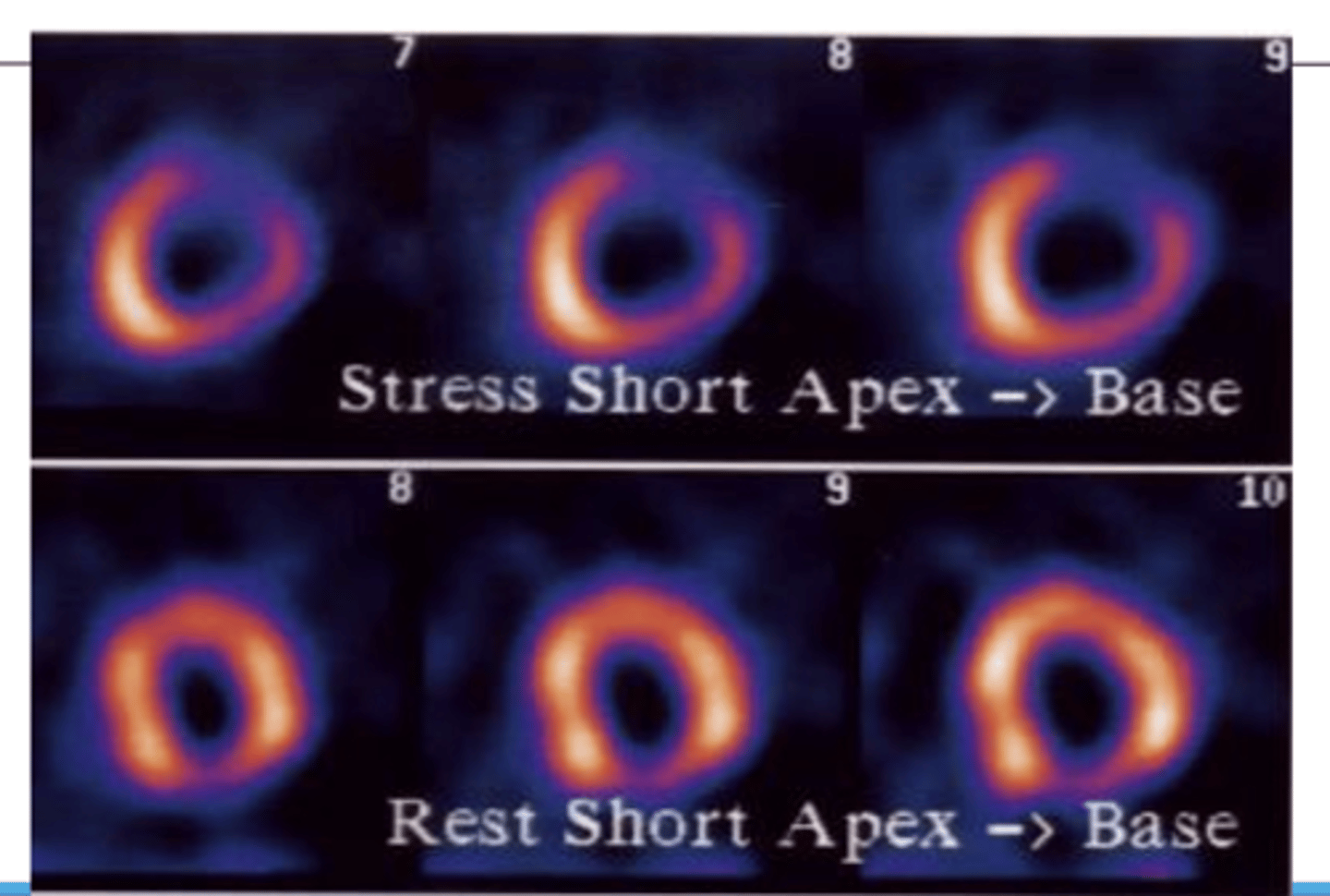
What is a thallium stress test used for?
⚬Assess regional blood flow of the coronary arteries-blood supply to heart muscle
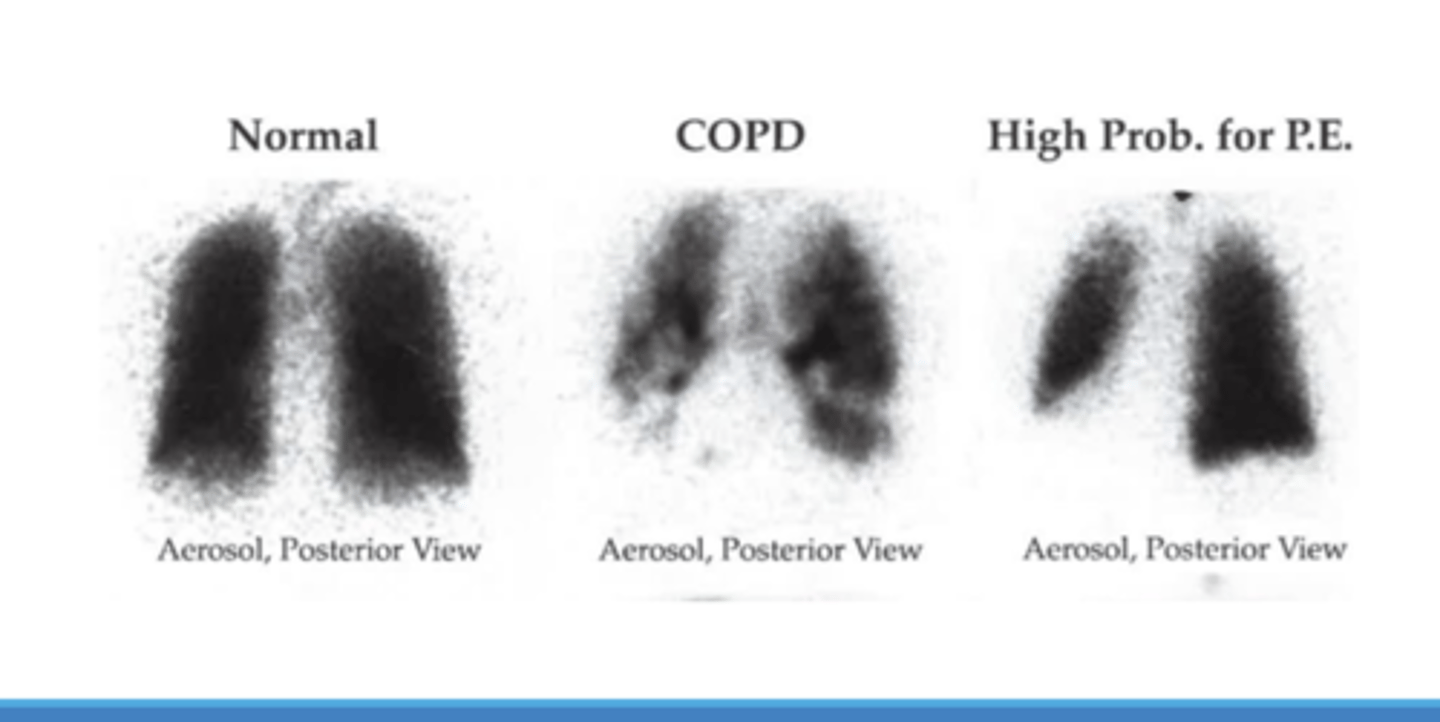
What is ventilation/perfusion scan used for?
How much RBC is being taken up at the capillaries and how much O2 is being taken up. (tagged RBCs also used)
When is gastric emptying study used?
Indication: suspect delayed gastric emptying
- tag food, have pt eat and see how long food remains in stomach.
What is always the first step of XRay interpretation?
CONFIRM PT details!! (name, dob, etc)
What does RIPE stand for?
Acronym used to assess image quality
Rotation
• The medial aspect of each clavicle should be
equidistant from the spinous processes. The spinous processes should also be vertically aligned.
•Inspiration
⚬The 5-6 anterior ribs, lung apices, both costophrenic angles and the lateral rib edges should be visible.
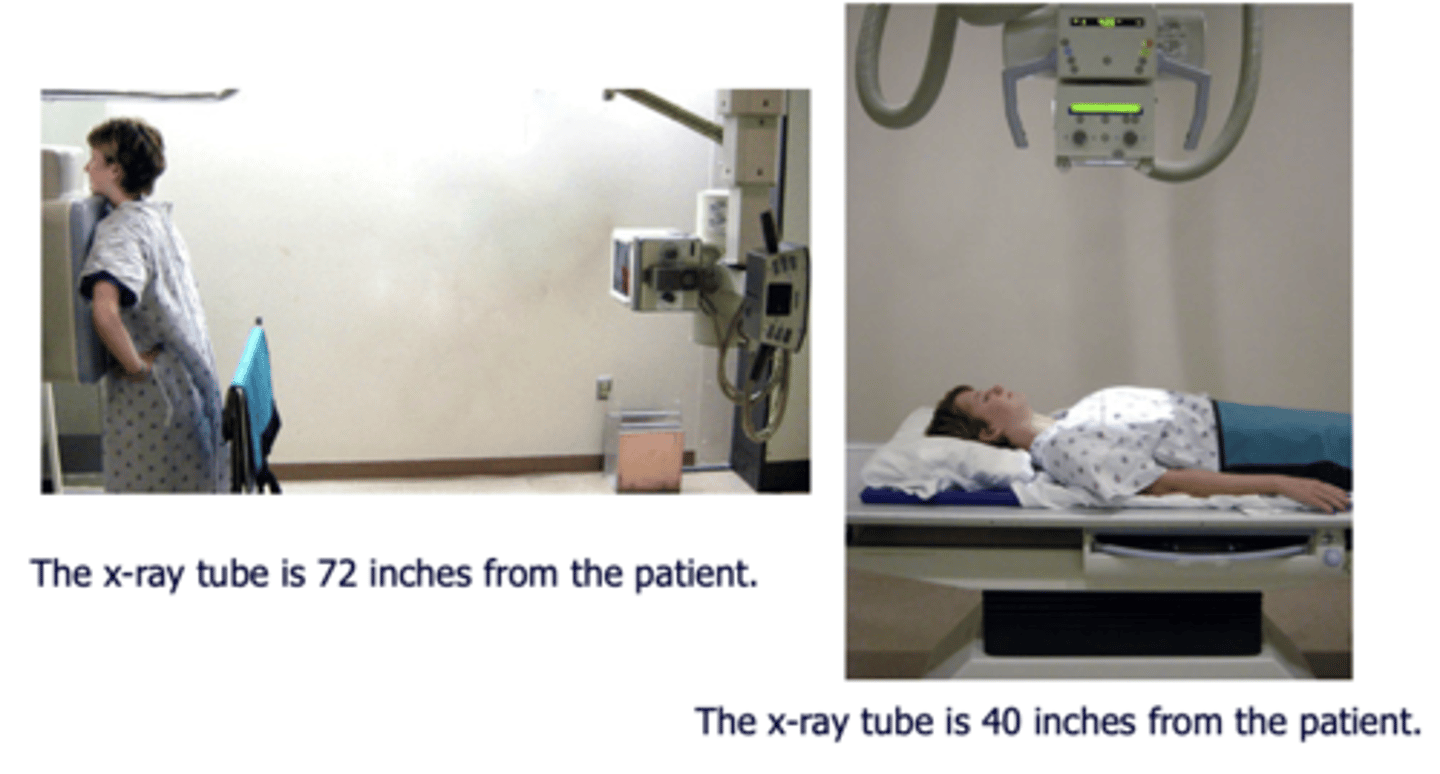
•Projection
⚬Note if the film is AP or PA: if there is no label, then assume it’s a PA film
⚬PA = XR beam is posterior (patient’s back)
XR film is anterior (patient’s chest)
⚬AP = XR beam is anterior (patient’s chest)
XR film is posterior (patient’s back)
•Exposure)
⚬The left hemidiaphragm should be visible to the spine, and the vertebrae should be visible behind the heart.
What does ABCDE stand for?
•Airway:
⚬trachea, carina, bronchi and hilar structures.
•Breathing:
⚬lungs and pleura.
•Cardiac:
⚬heart size and borders.
•Diaphragm:
⚬including assessment of costophrenic angles.
•Everything else:
⚬ mediastinal contours, bones, soft tissues, tubes, valves, pacemakers and
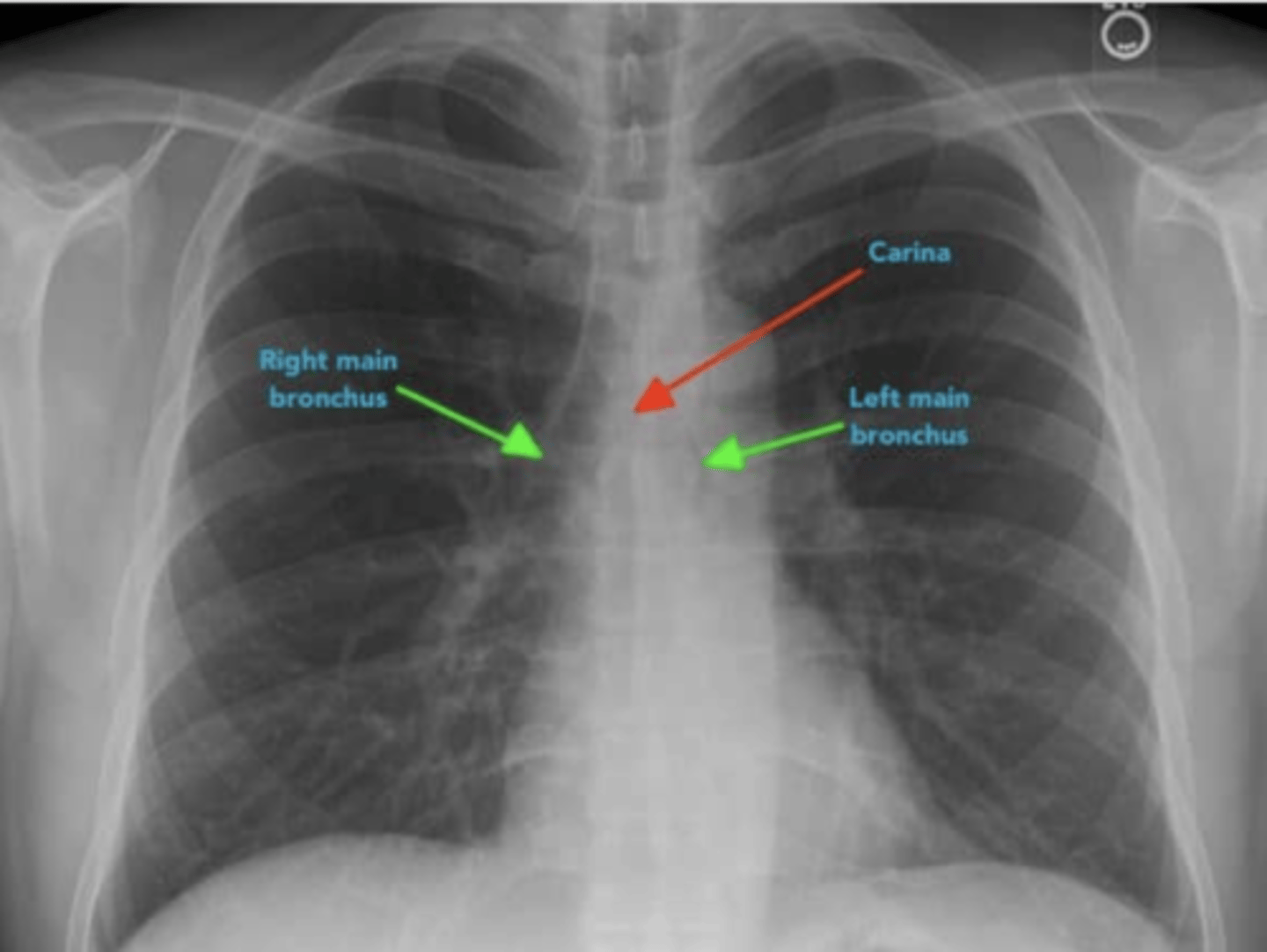
For airway, what are 2 main structures to identify and why?
1.Carina and bronchi
⚬The carina is cartilage situated at the point at which the trachea divides into the left and right main bronchus.
•On appropriately exposed chest X-ray, this division should be clearly visible.
•The carina is an important landmark when assessing nasogastric (NG) tube placement, as the NG tube should bisect the carina if it is correctly placed in the gastrointestinal tract.
2. The right main bronchus is wider, shorter and more vertical than the left main bronchus.
•As a result of this difference in size and orientation, it is more common for inhaled foreign objects to become lodged in the right main bronchus.
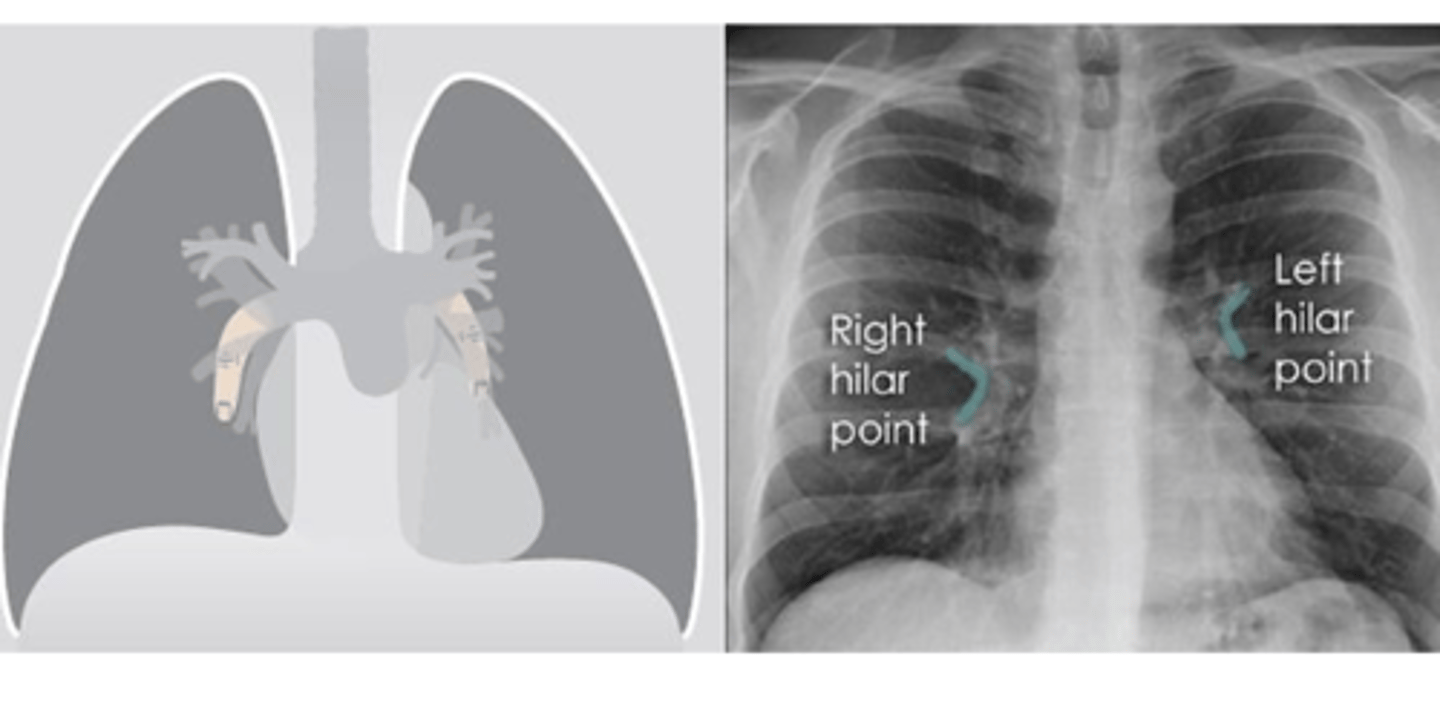
What do the Hilar structures consist of? Is the L or R positioned higher? Why is it important to ID this structure?
•The hilar consist of the main pulmonary vasculature and the major bronchi. (wedge shaped area on central portion of each lung)
•Each hilar also has a collection of lymph nodes which aren’t usually visible in healthy individuals.
•The left hilum is often positioned slightly higher than the right, but there is a wide degree of variability between individuals.
•The hilar are usually the same size, so asymmetry should raise suspicion of pathology.
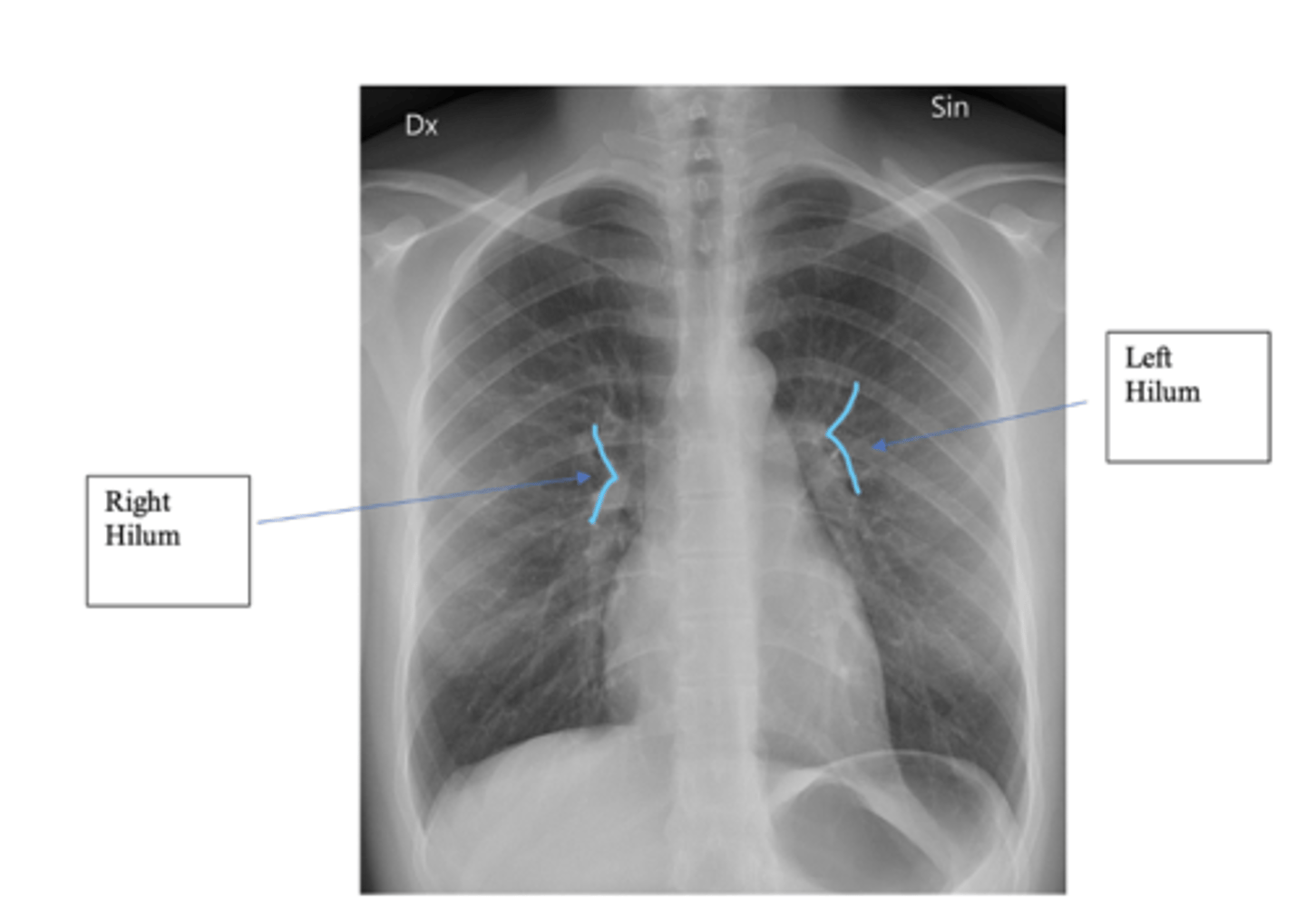
What is the significance of the hilar point?
⚬where the descending pulmonary artery intersects the superior pulmonary vein.
⚬When this is lost, consider the possibility of a lesion here (e.g. lung tumour or enlarged lymph nodes).
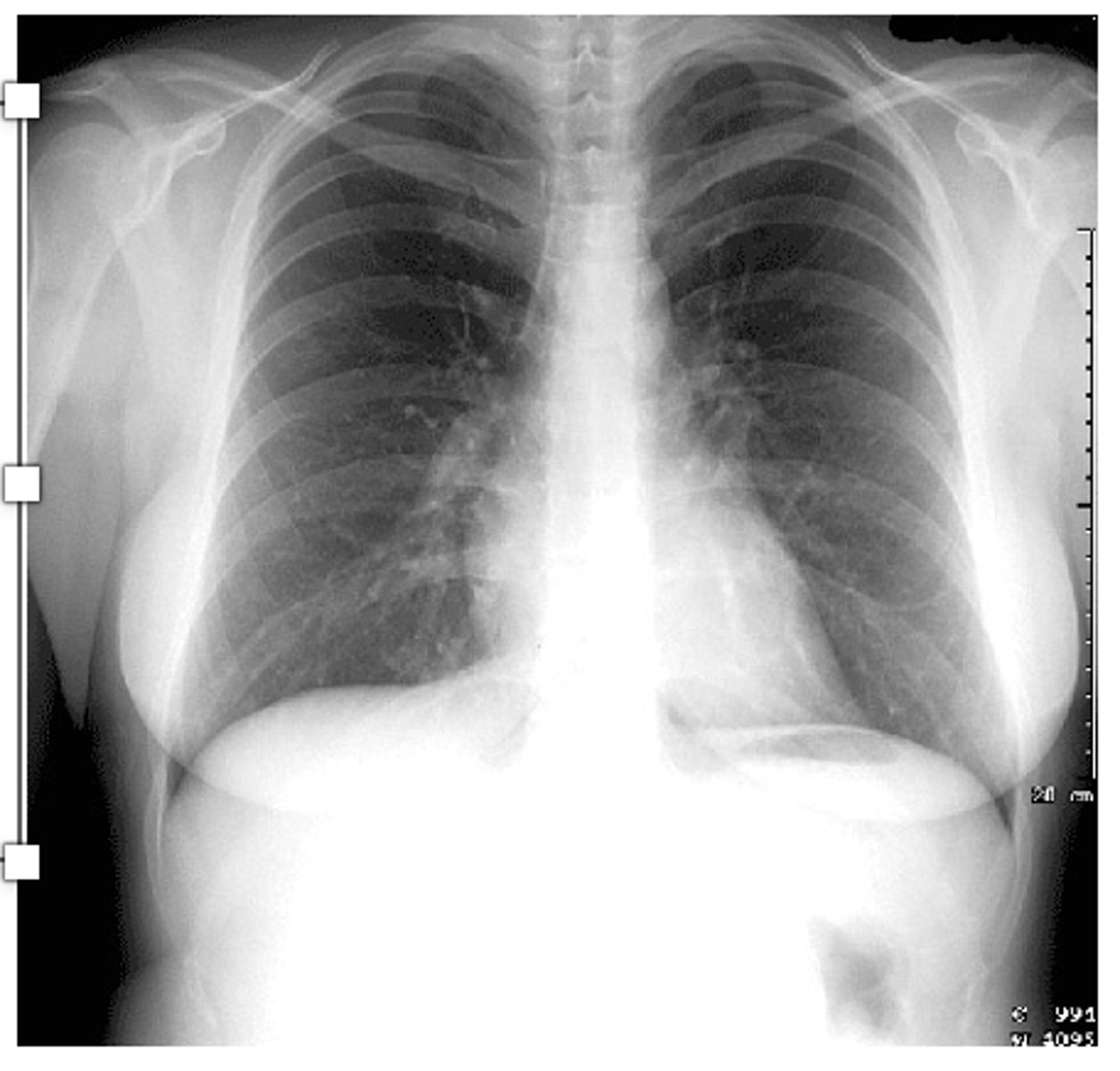
What are 8 things to remember when reading a CXR?
•1. Determine age, sex and history
•2. What type of film? AP, PA, portable or lateral? Correct exposure?
•3. What is position of patient? Upright, supine or decubitus?
•4. Is there good inspiratory effort? Is the diaphragm below the 7th rib?
•5. Identify structures and abnormalities
•6. Recheck "Blind spots" •7. Check old films for any changes
•8. Decide what your findings are and a differential diagnosis.
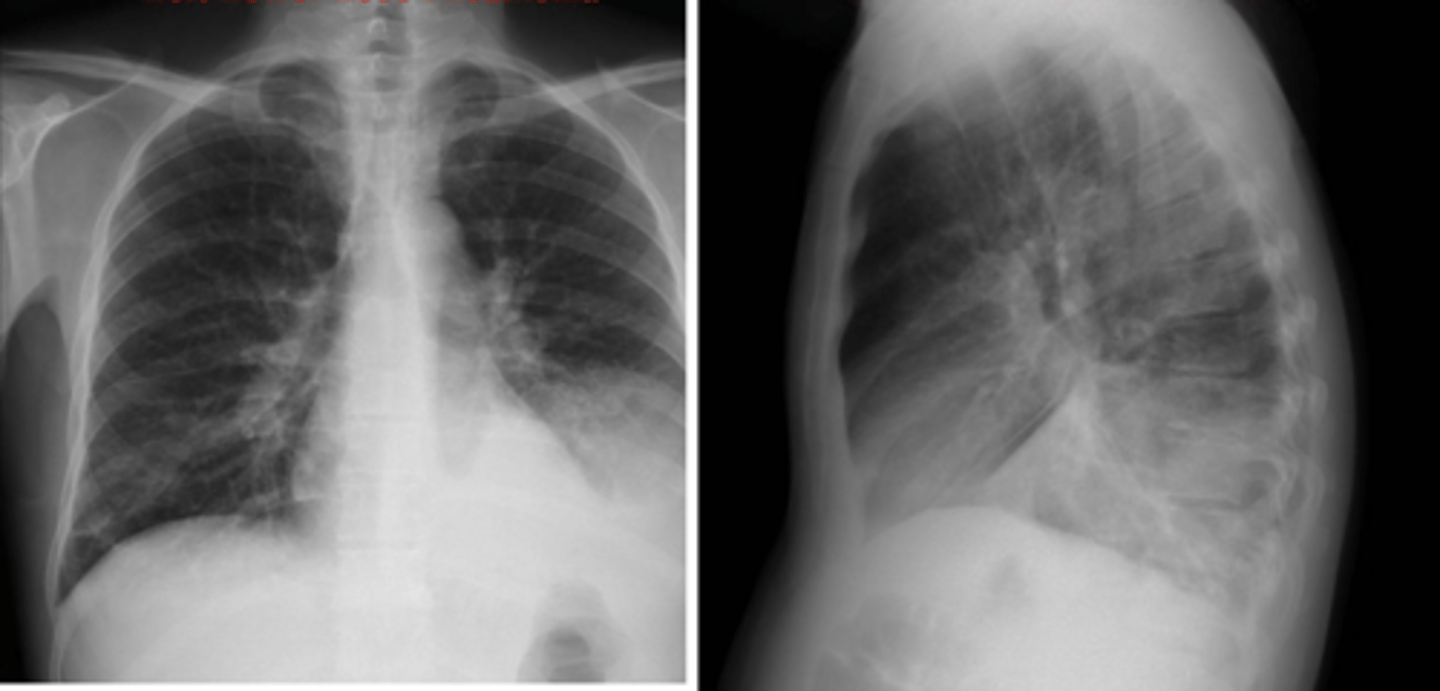
What do routine CXRs inculde and what are 4 other types of CXRs?
•Routine CXRs include PA and lateral views with the patient in the upright position.
Other types of CXRs
⚬AP and supine (portable) films make the heart appear enlarged and the lungs hypoinflated.
⚬A lateral decubitus film can aid in identifying a pleural effusion.
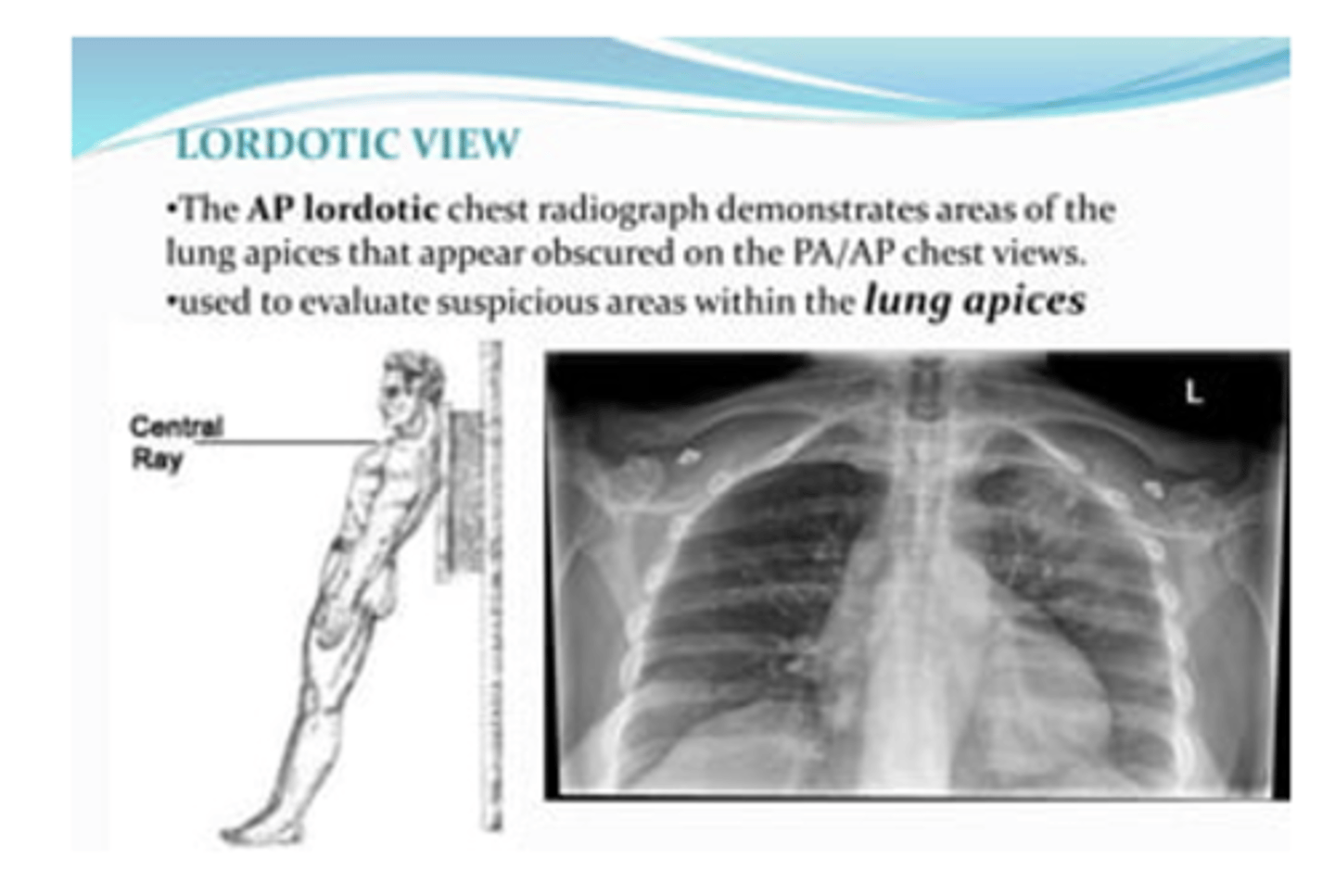
⚬Lordotic films are used to view the apices of the lungs
⚬Expiratory view may be helpful for pneumothorax
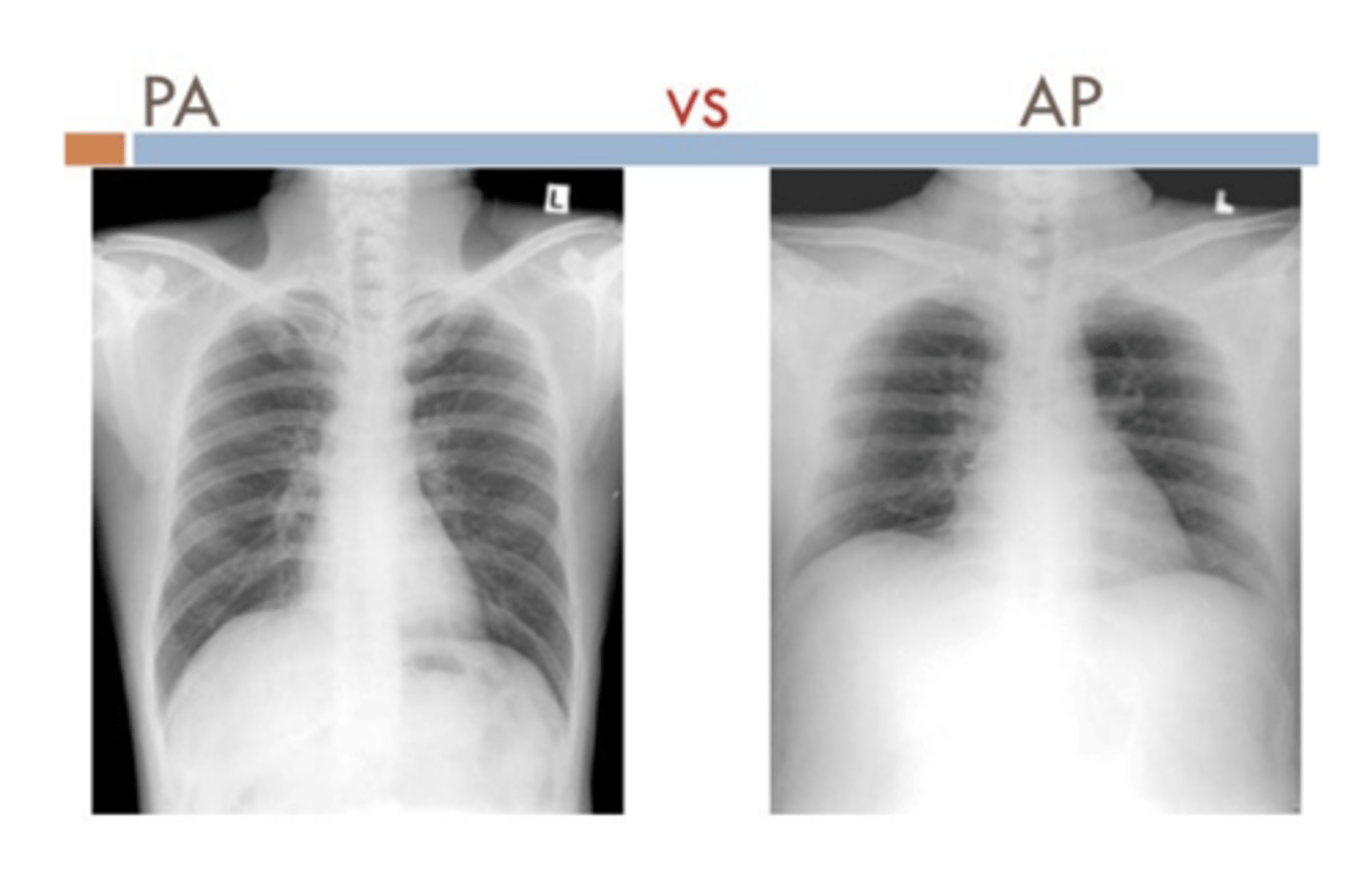
What structures are more visible PA vs AP?
PA
⚬Scapula in periphery
⚬Clavicles project over lung fields
⚬Posterior ribs are distinct
AP
⚬Scapula are over the lung field
⚬Clavicles above apex of lung
⚬Anterior ribs are distinct
What is a lordotic view CXR typicallyl used for?
To evaluate suspicious areas within the lung apices
What is the standard for normal exposure?
visualization of the vessels to at least the peripheral 2/3 of the lung.
What is normal visualization of inspiratory efffort?
Visualization of more than 7 ribs indicates adequate inspiratory effort.
What is mediastinal shift? How can you ID?
Left hilum should be higher than the right hilum. Often due to mediastinal mass

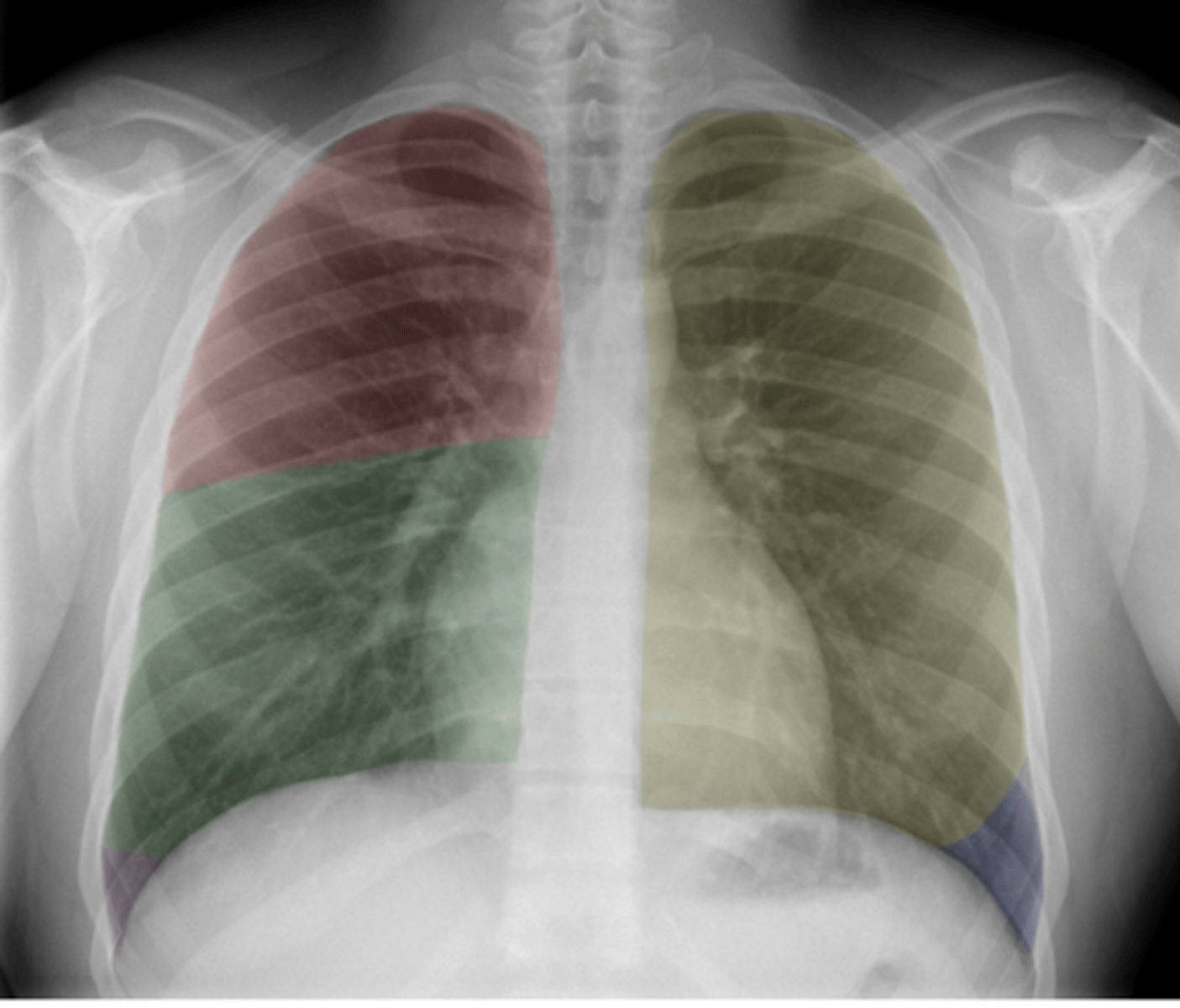
ID lobes of lungs on back (anterior)
•Red: Right upper lobe (RUL)
•Green: Right middle lobe (RML)
•Purple: Right lower lobe (RLL)
•Yellow: Left upper lobe (LUL)
•Blue: Left lower lobe (LLL)
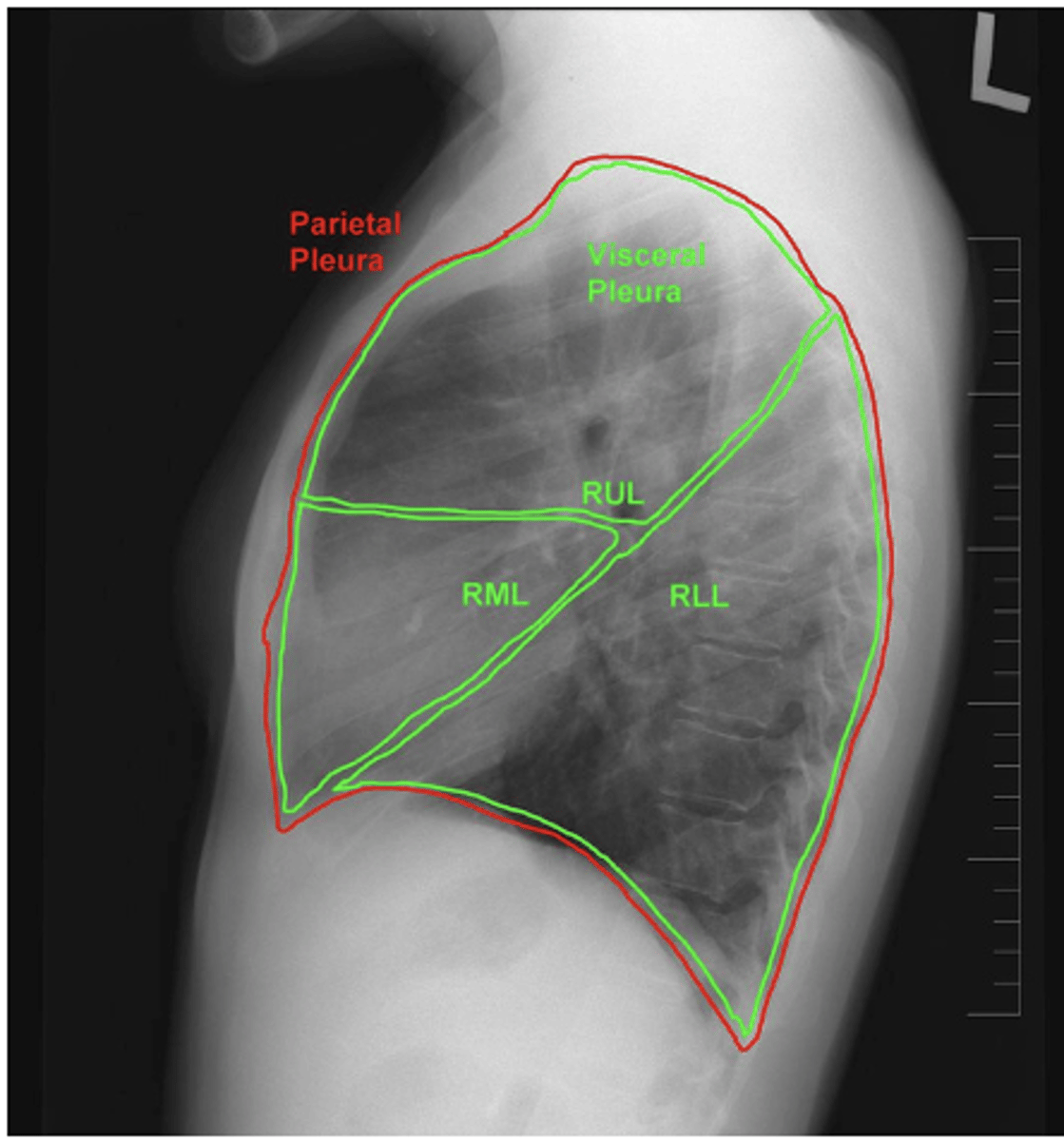
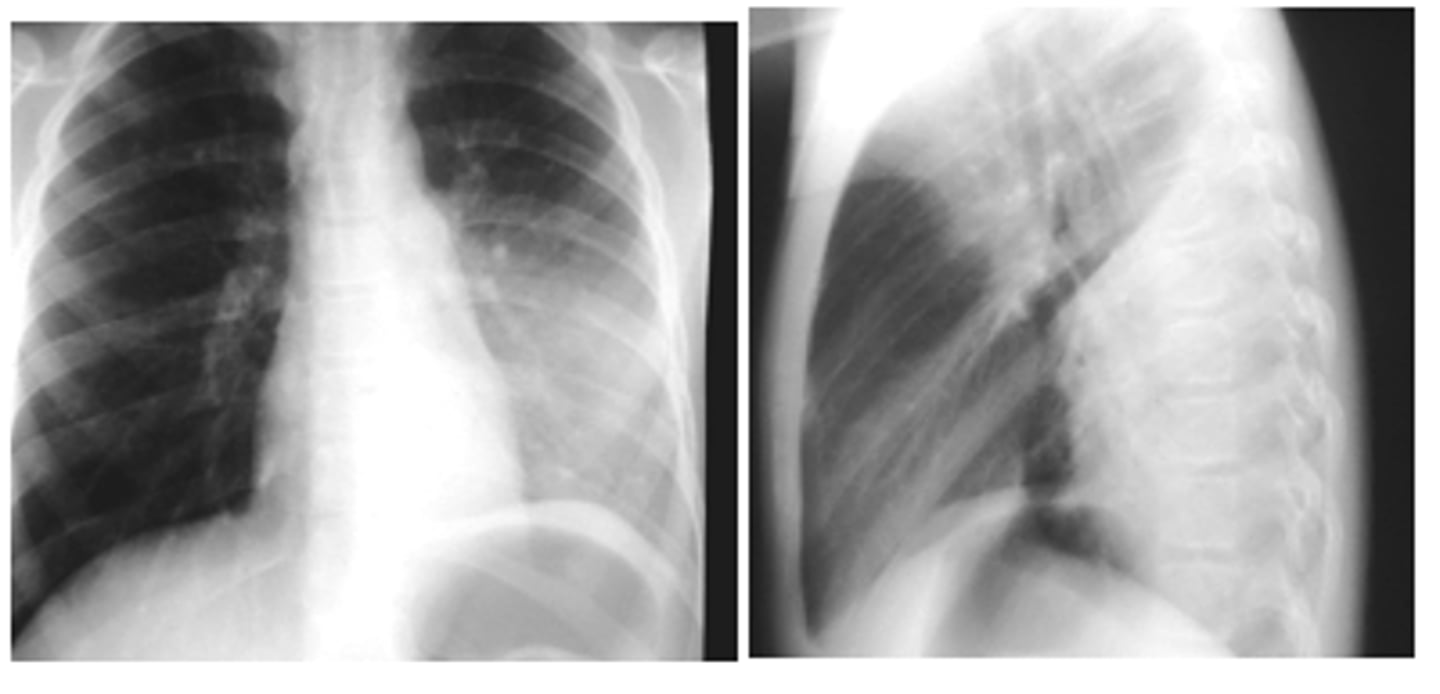
ID lobes of lungs on back of card (lateral right)
refer to picture
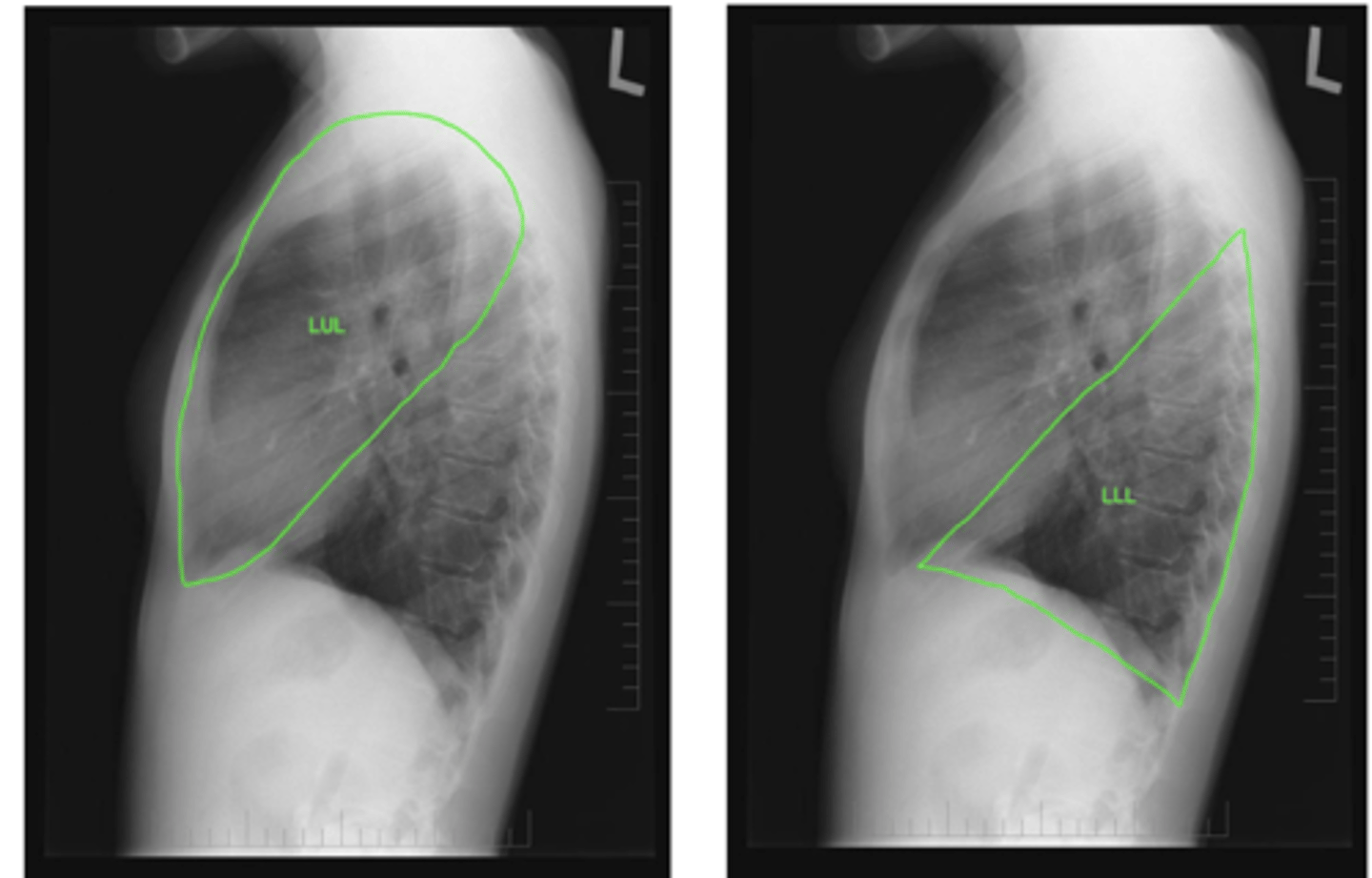
ID lobes of lungs on back of card (lateral left)
refer to pic
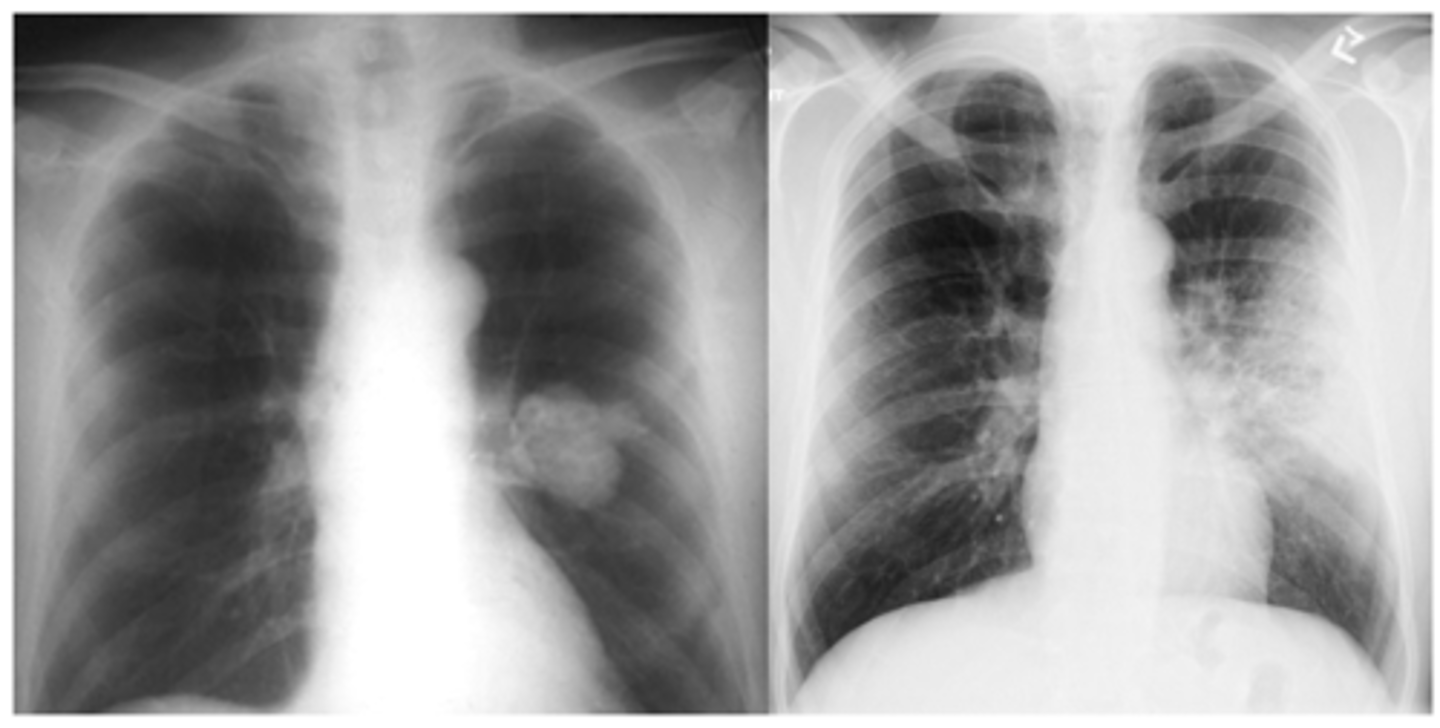
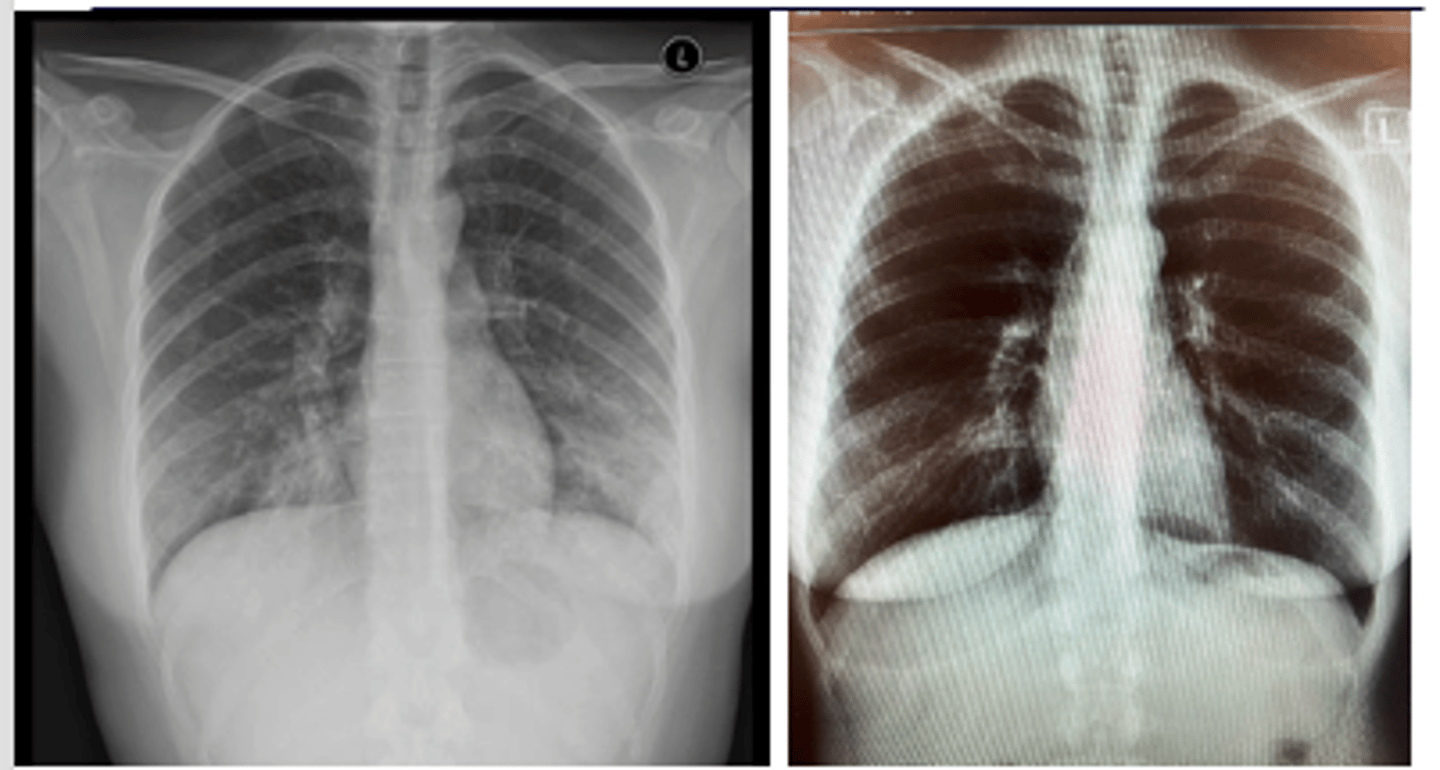
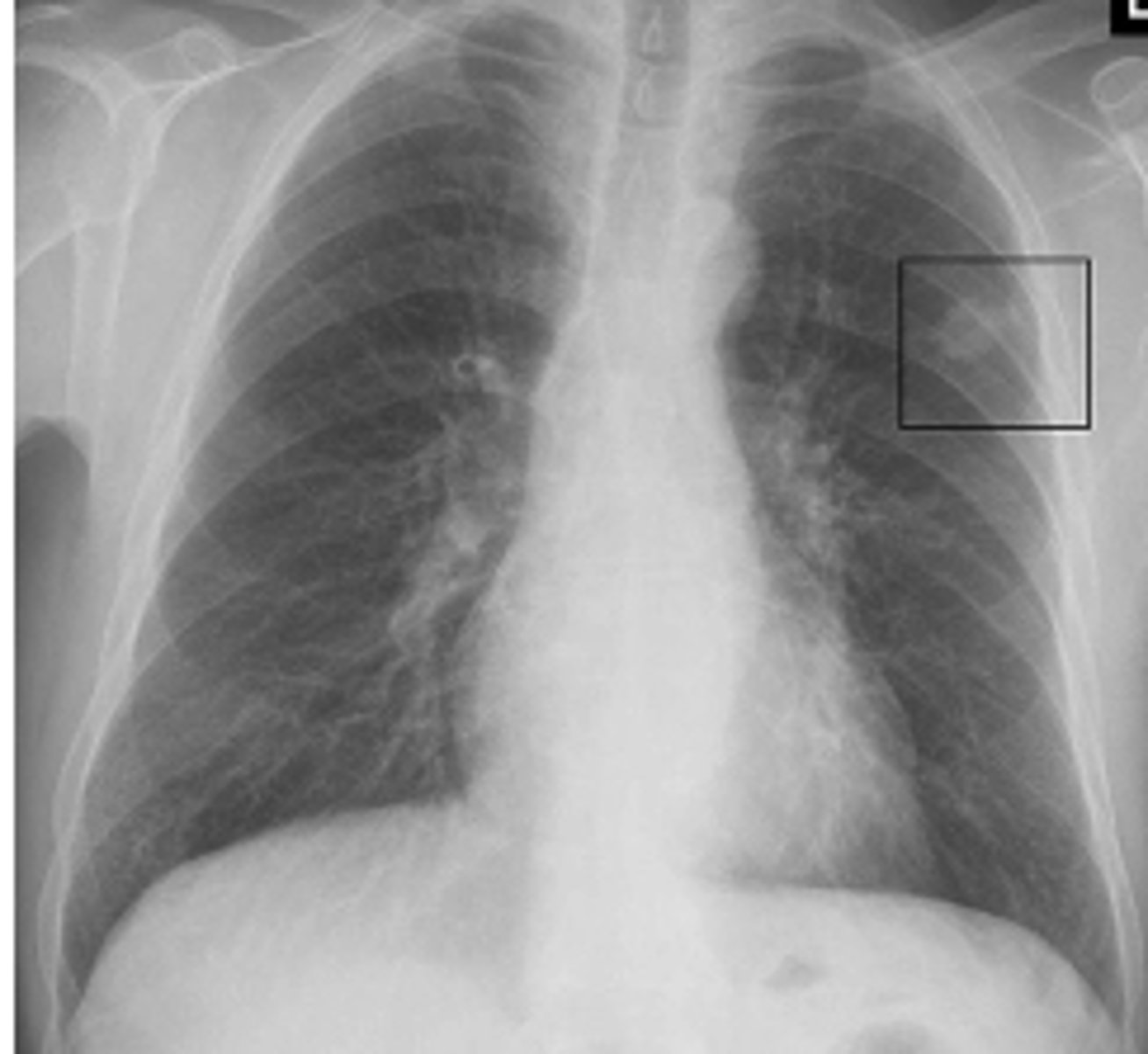
dx on back
left lower lobe pneumonia
ID mass and infiltrate on back
mass Left
infiltrate R
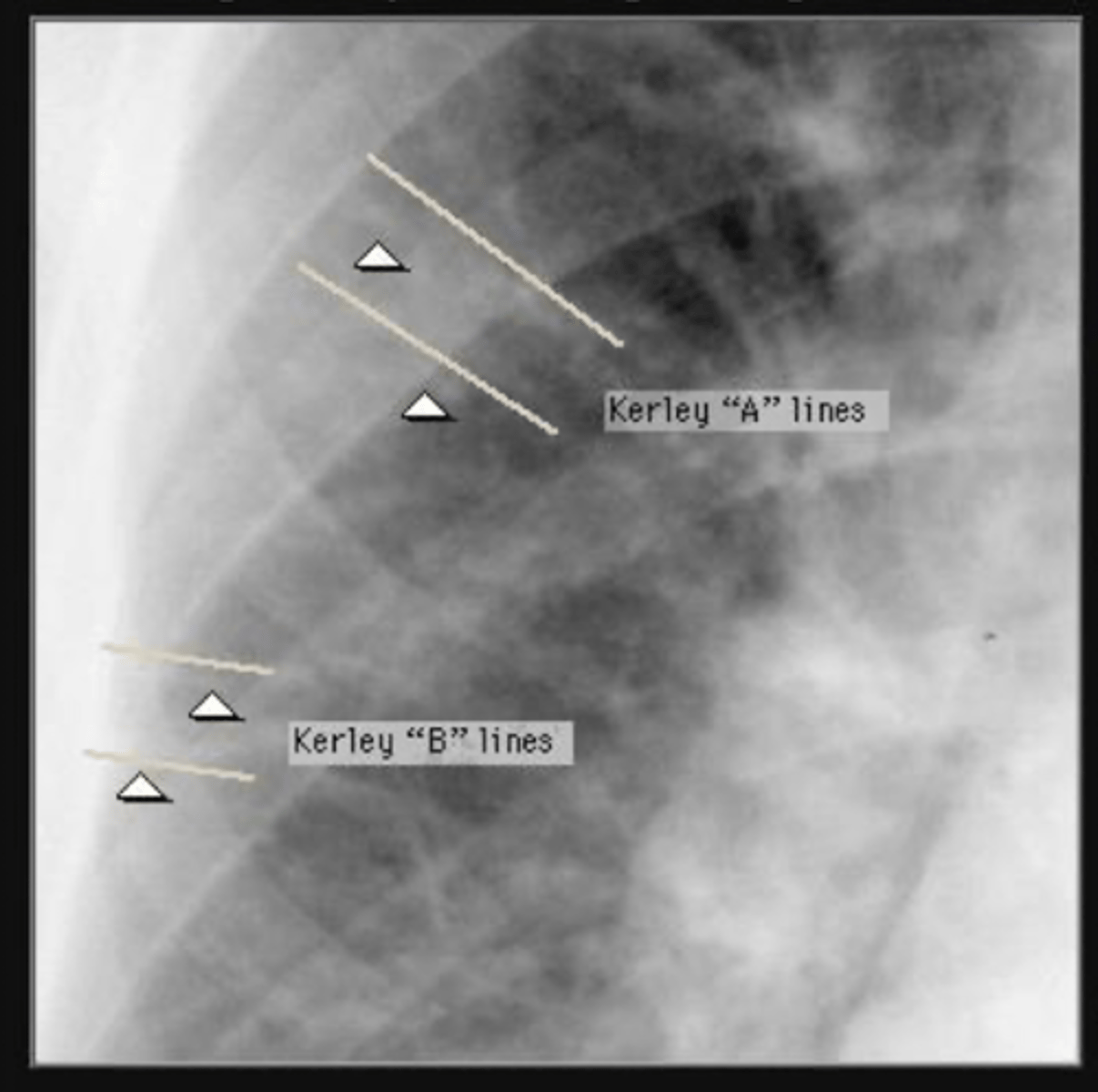
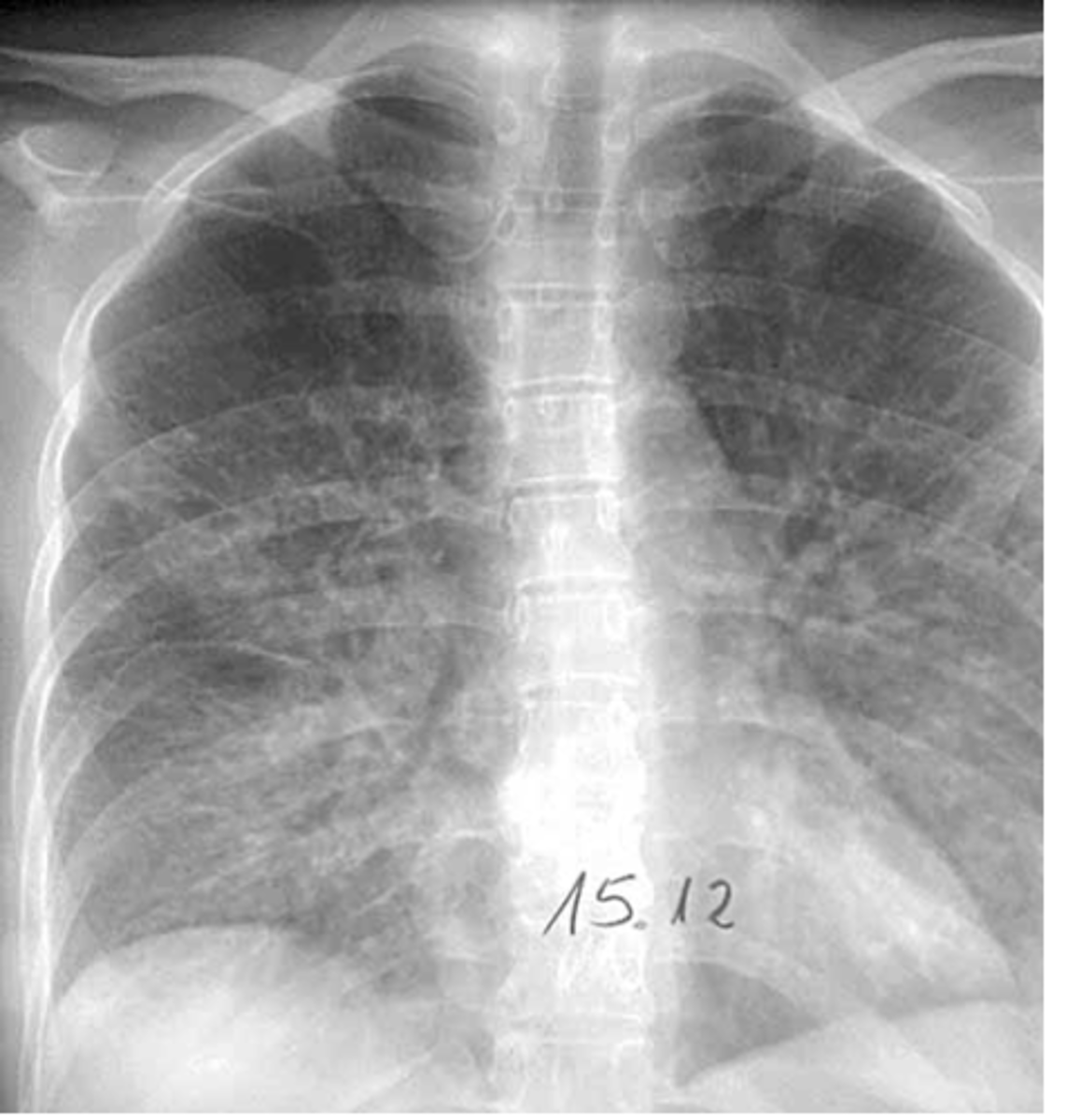
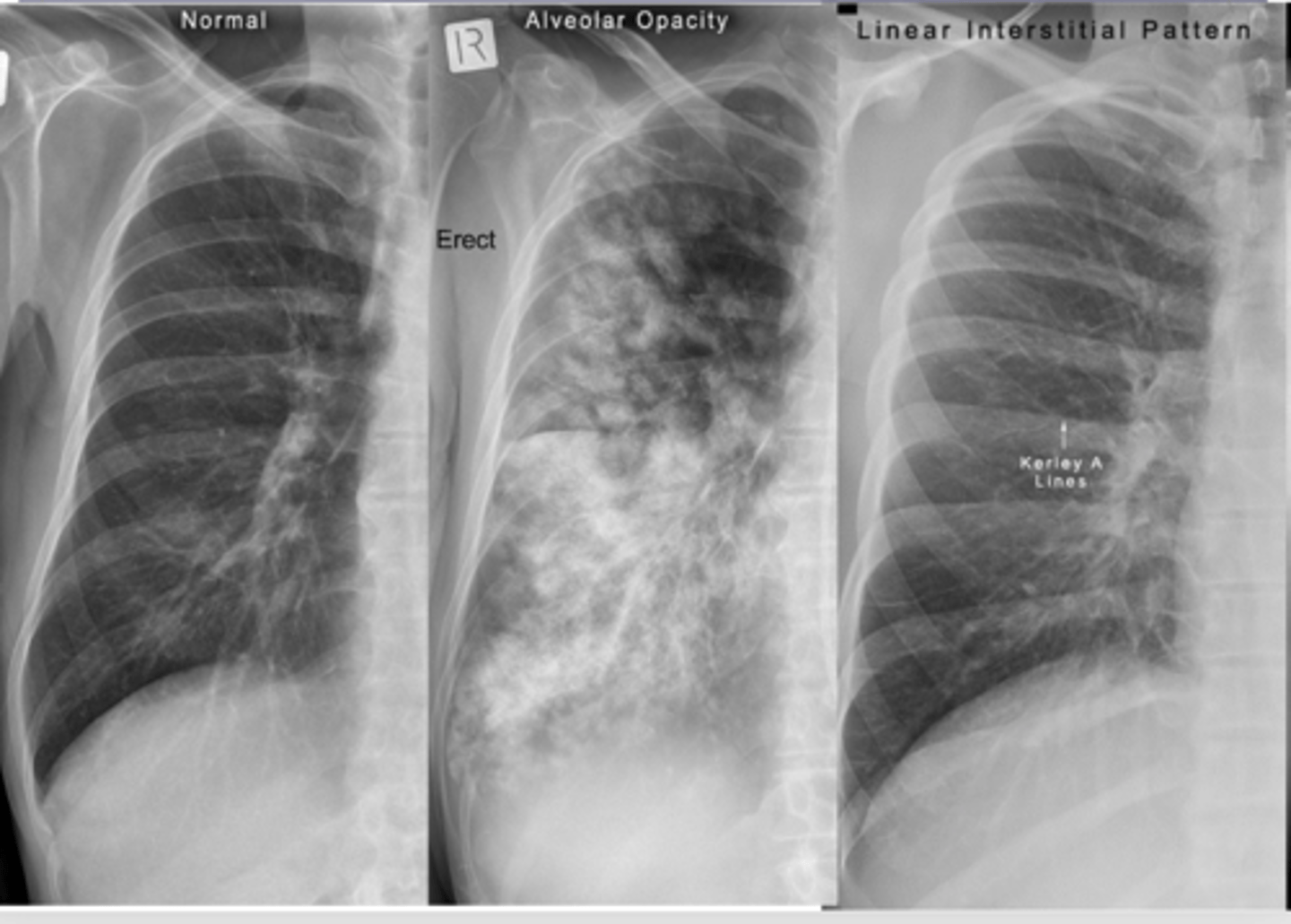
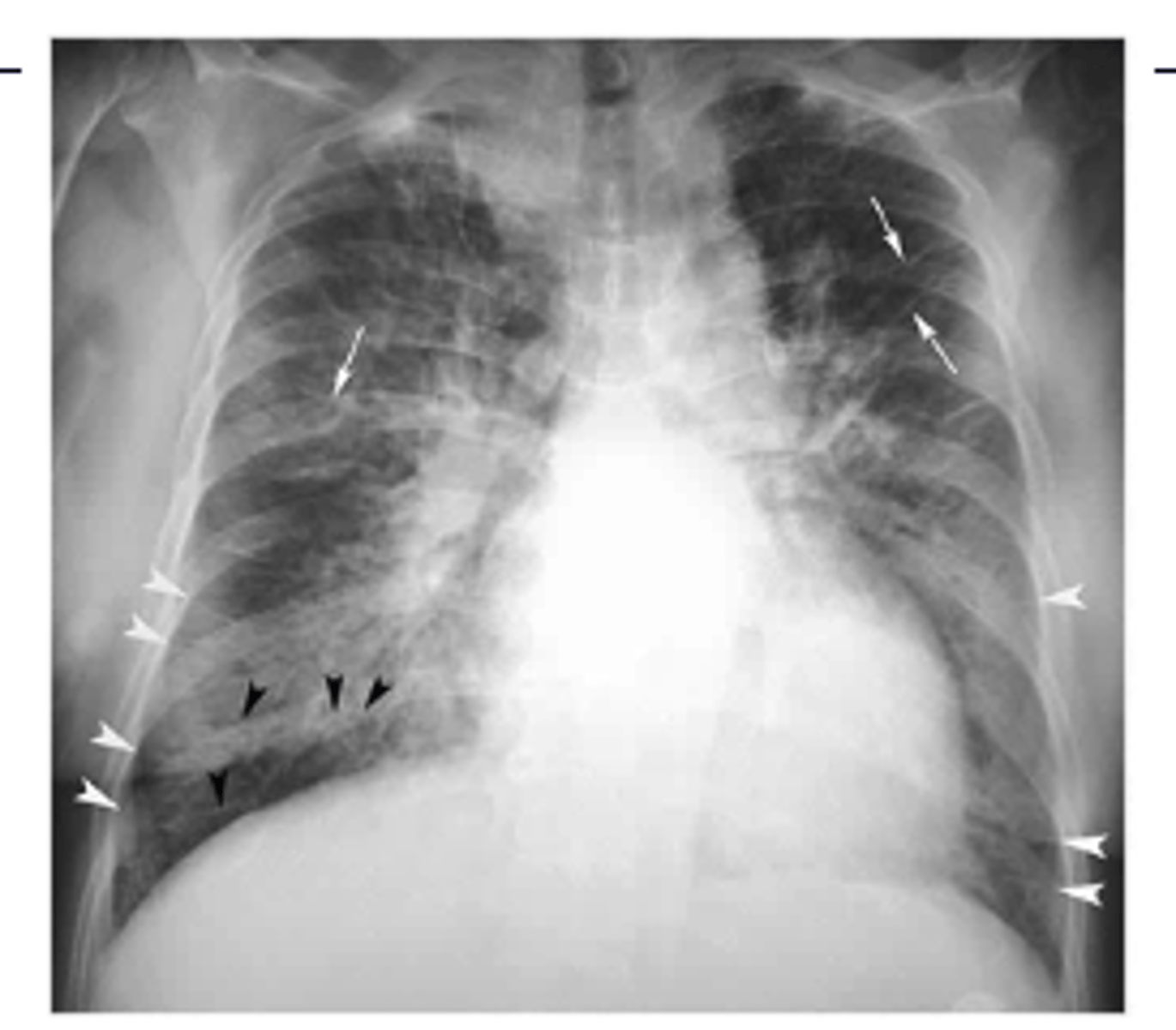
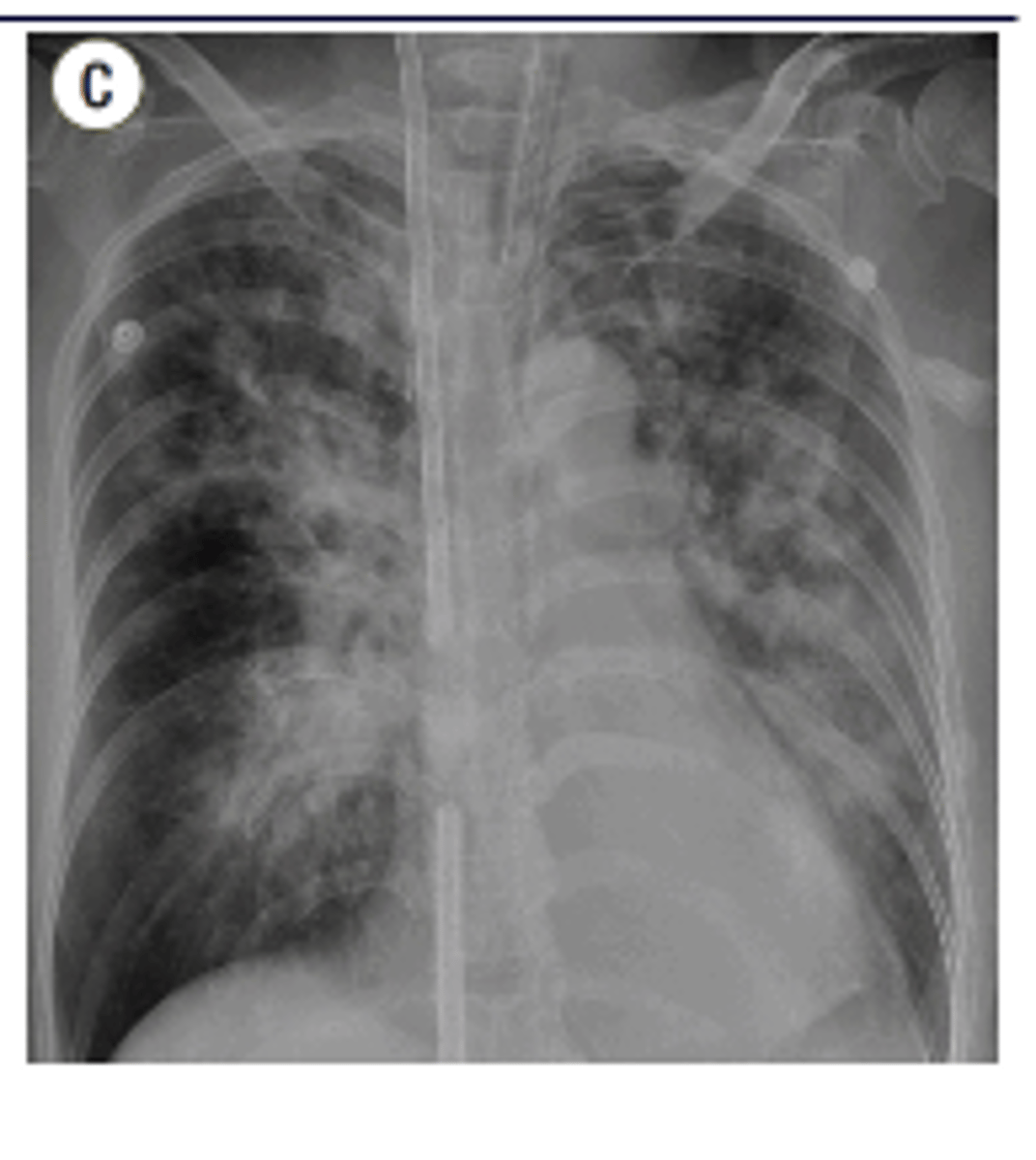
Mild vs moderate vs severe CHF x-ray findings
CXR changes are progressive - initially normal then redistribution of pulmonary vascular pattern and cardiomegaly.
Mild - equal pulmonary vasculature in upper and lower lobes (cephalization)
Moderate - Kerley B lines in lateral basilar regions
Severe - pulmonary edema - bilateral perihilar and basilar alveolar infiltrates
What finding indicates pulm edema in CHF?
kerley a and B lines
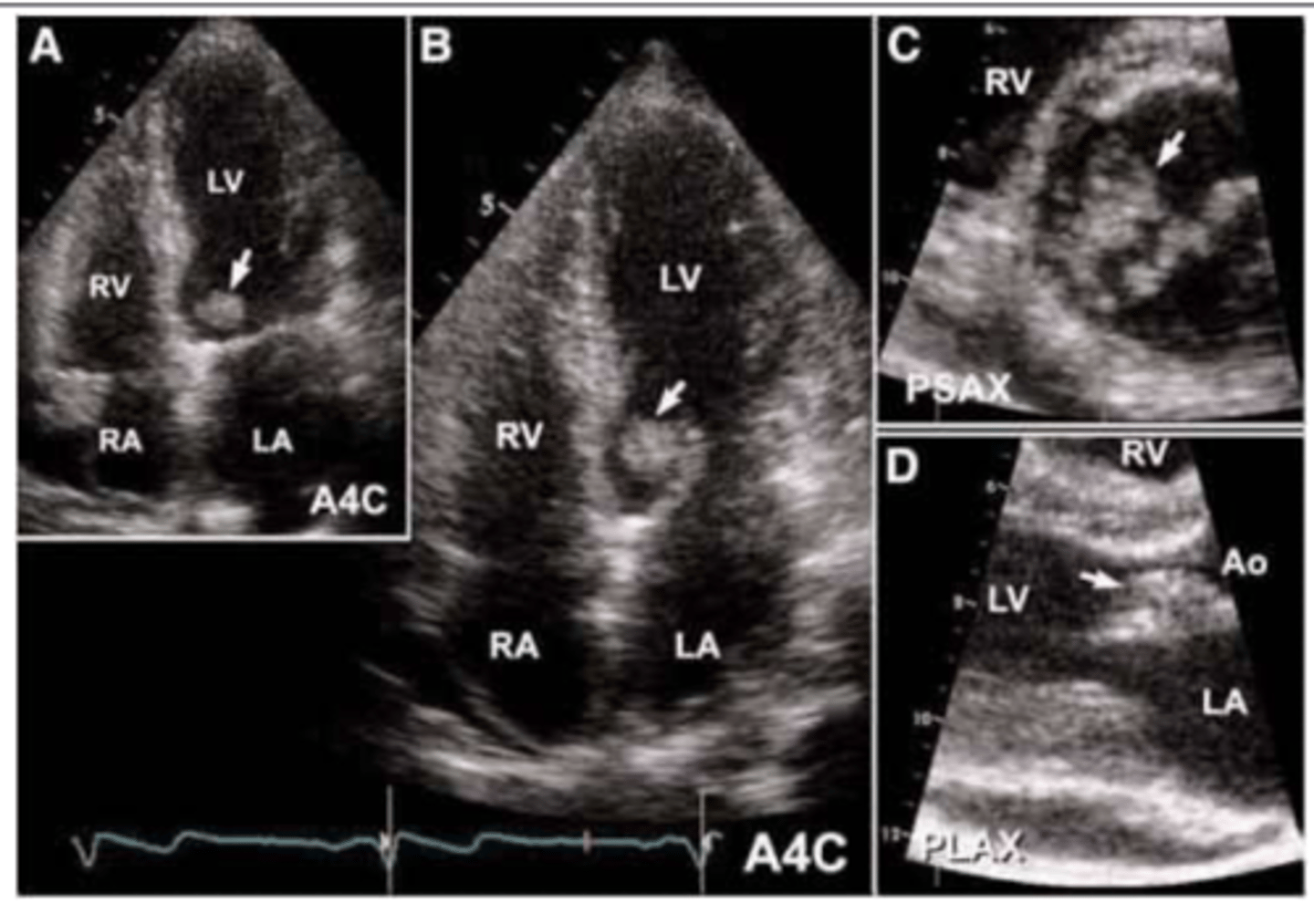
What should you order in order to evaluate cardiac fx?
you can order either an
echocardiogram or MUGA scan
Normal EF for older pt. WHen is angiogram indicated?
above 50%. angiogram may be indicated if EF , 35%
Pros and cons of Echo vs MUGA
ECHO
1. Very close in accuracy to MUGA in evaluating heart function
2. Can evaluate valves, heart size, clots in heart, wall size etc.
3. No radioactivity
4. cheaper
CONS:
-Poor in pts with lung Dz
MUGA
-most accurate in evaluating heart fx
-good for pt w lung dz
CONS
-radioactive
-needles
-$
What is the finding on the back of the card?
coarctation of aorta
Common causes of chamber enlargement
Left ventricular enlargement can be due to chronic HTN (most common), coronary artery disease, aortic stenosis or regurgitation, or ventricular aneurysm.
Best imaging to eval LV hypertrophy
Left ventricular hypertrophy (wall thickening) is best evaluated by echocardiogram.
What is endocarditis? Epidemiology
Endocarditis = infection of the heart valves
Usually occurs in patients with prior valvular disease or drug addiction.
Imaging used to eval endocarditis
Echocardiogram (usually transesophageal)
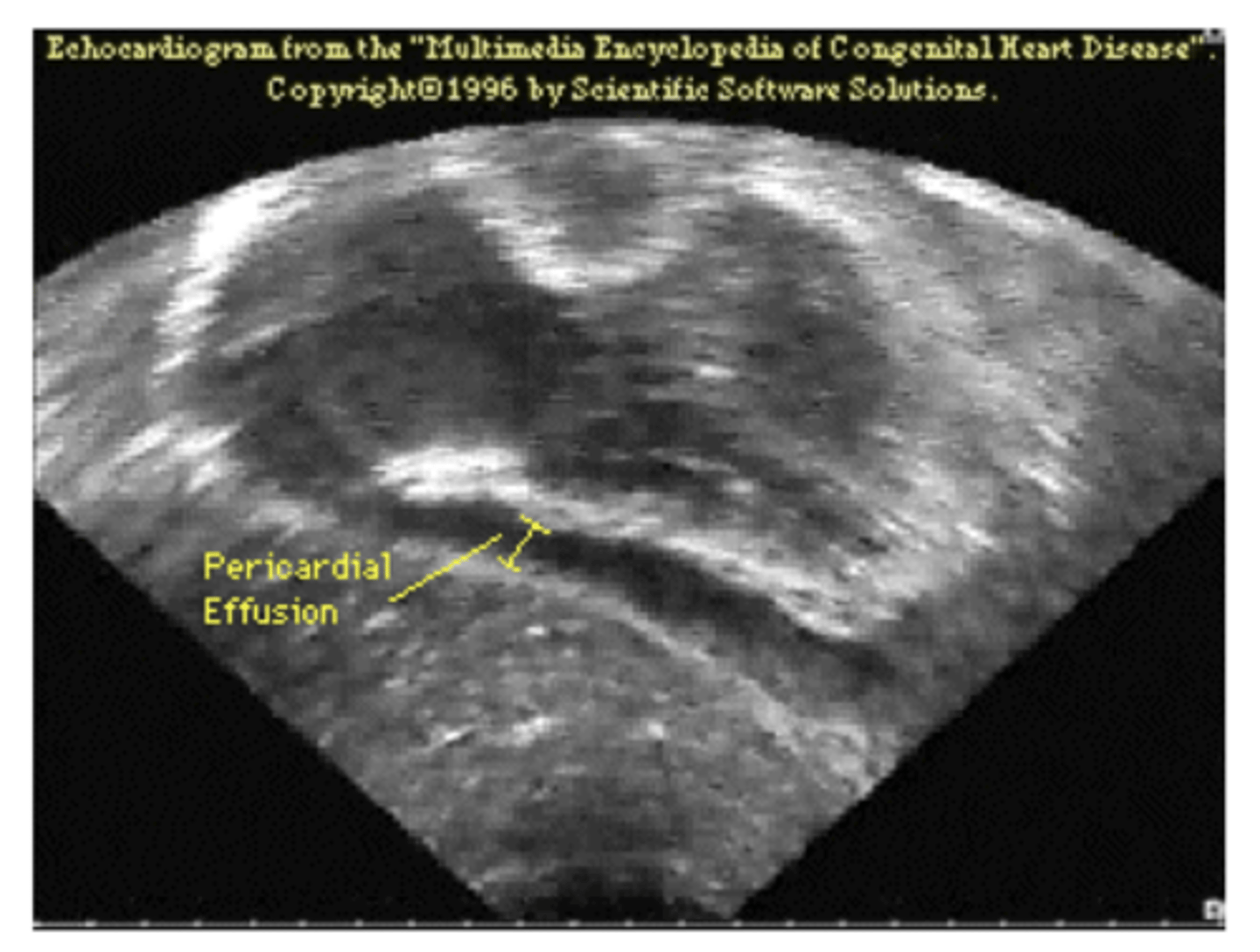
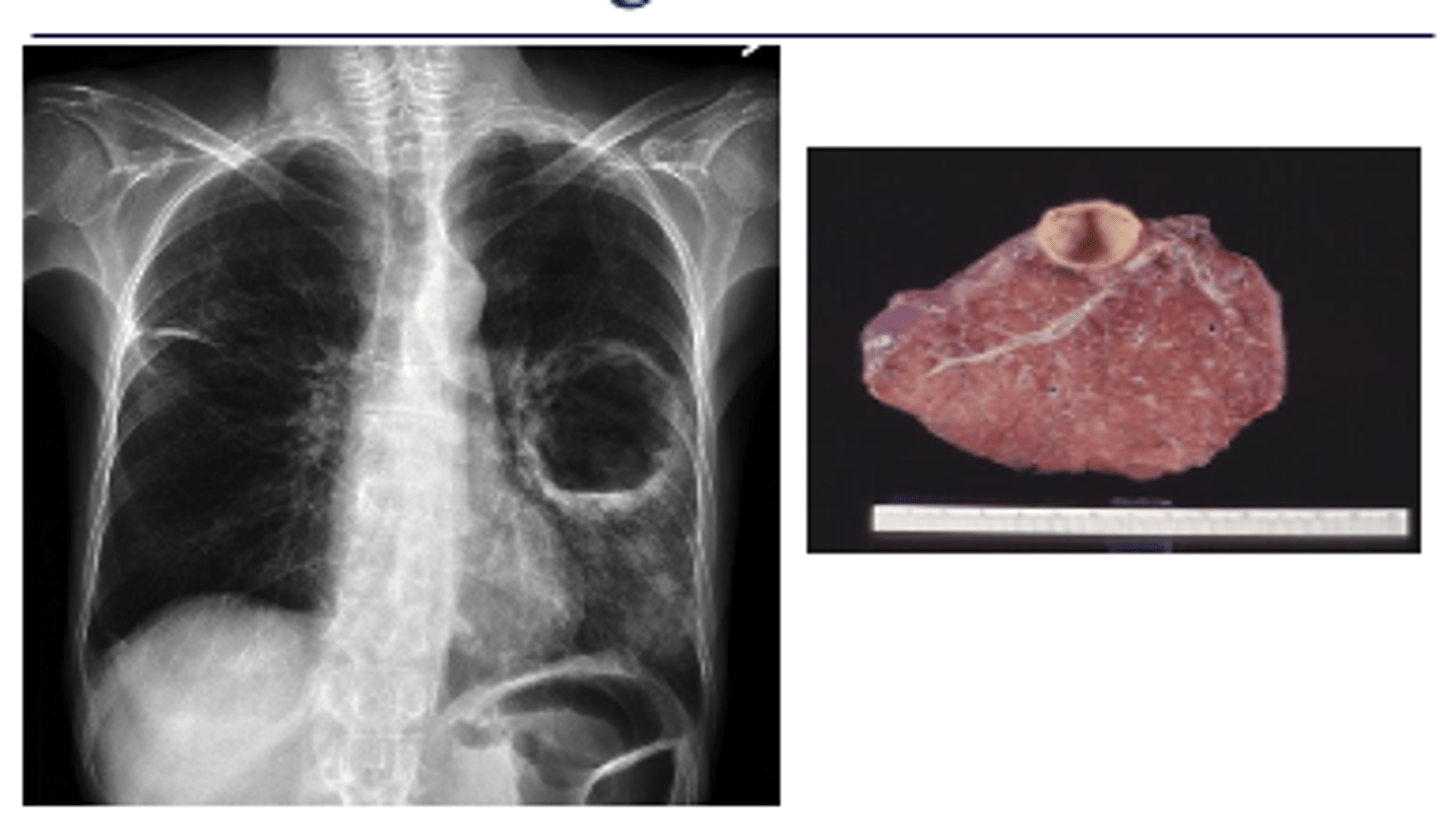
What is the typical appearance of pericardial effusion? Imaging of choice
Pericardial effusion causes an acute marked
enlargement with the heart appearing pendulous and very wide at the base – “water bag appearance.”
echocardiogram is imaging of choice (image here is x-ray)
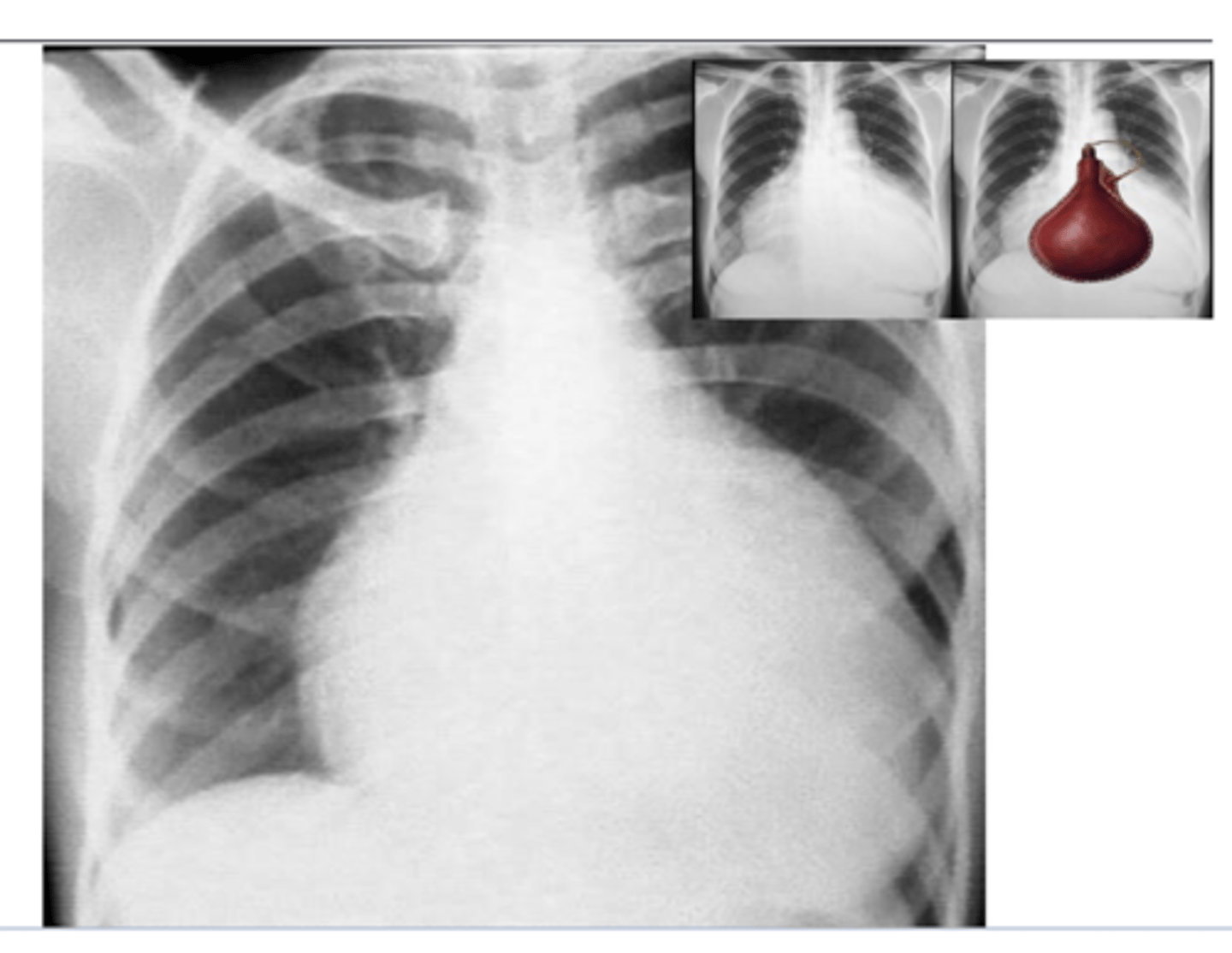
What does epicardial effusion look like on ECG?
area of darkness around heart
What is the most common congenital cardiac deformity in adults?
Atrial septal defect
-blood is going through an additional opening out of the atrium
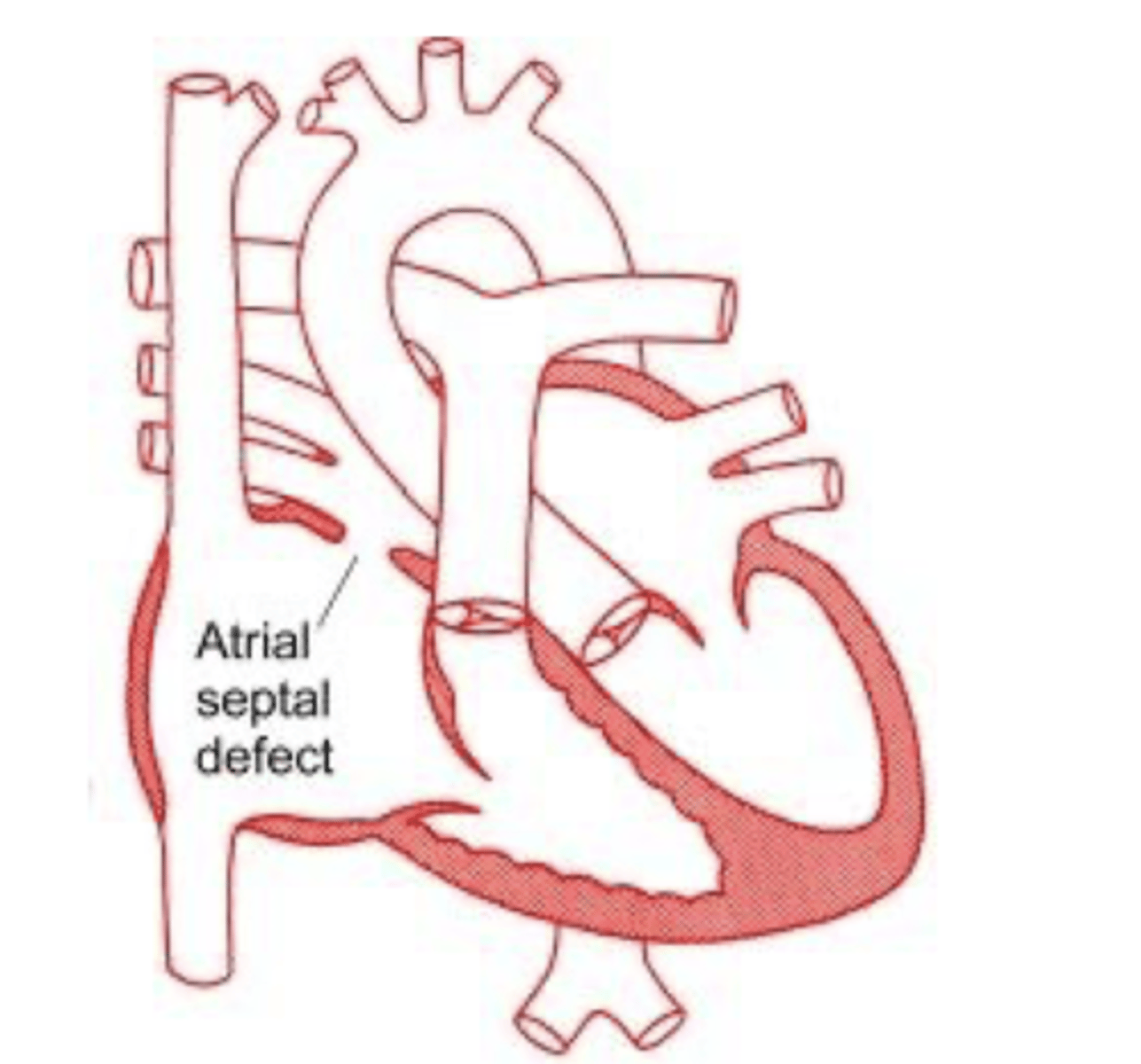
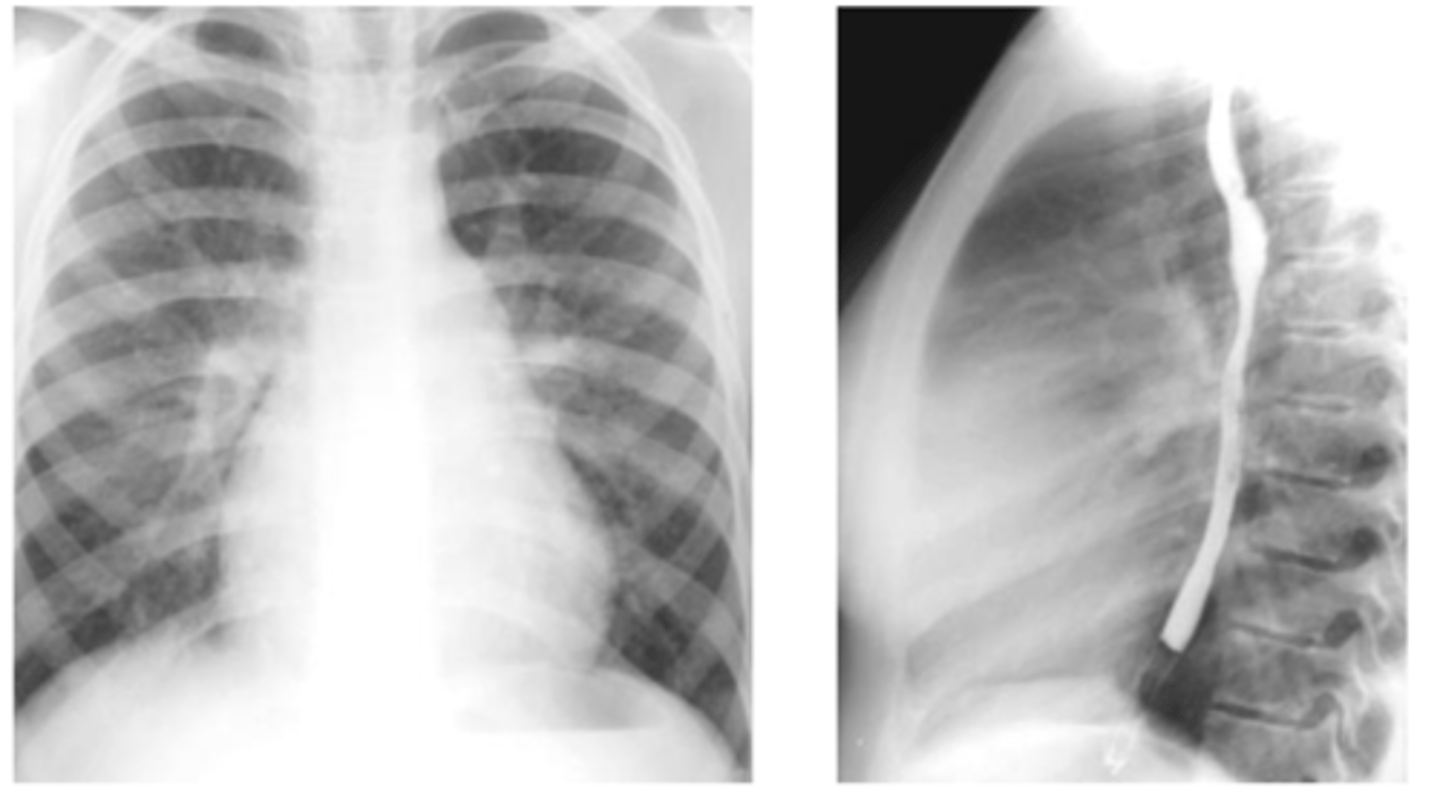
X-ray findings with atrial septal defect
-pulmonary artery
enlargement, right atrial and right ventricular enlargement.
-Film shows filling-in of retrosternal space and
increased size of the pulmonary artery.
What is hampton's hump?
Wedge shaped pleural based opacity --> indicative of pulmonary embolism
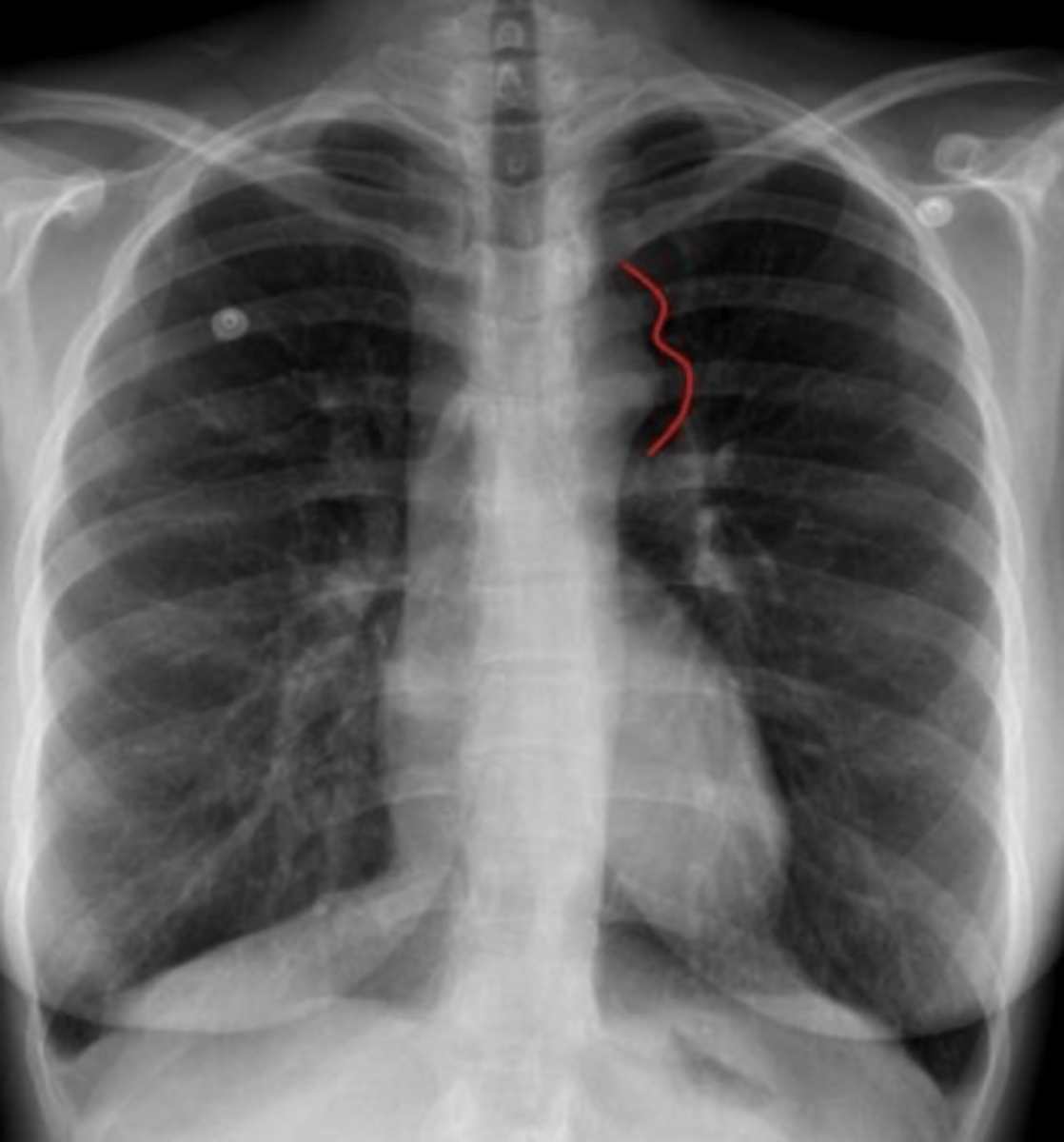
What is westermark's sign? What is it indicative of?
Westermark's sign - the
decreased distal vasculature creating the
appearance of a sharp cut off
*pulmonary embolism
what is the best initial study for suspected pulmonary embolism?
spiral CT with
contrast (CT
Angiography -
CTA)
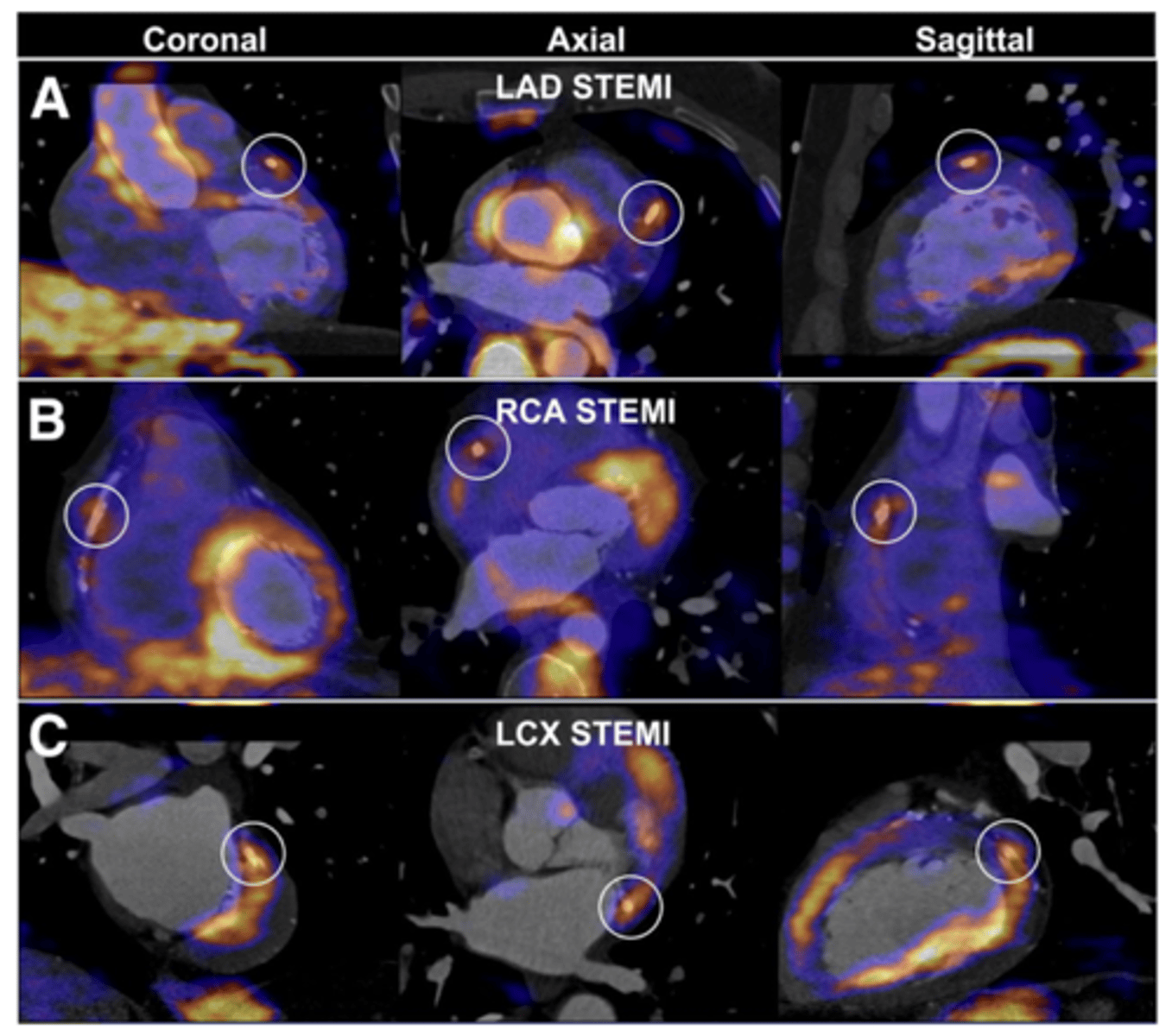
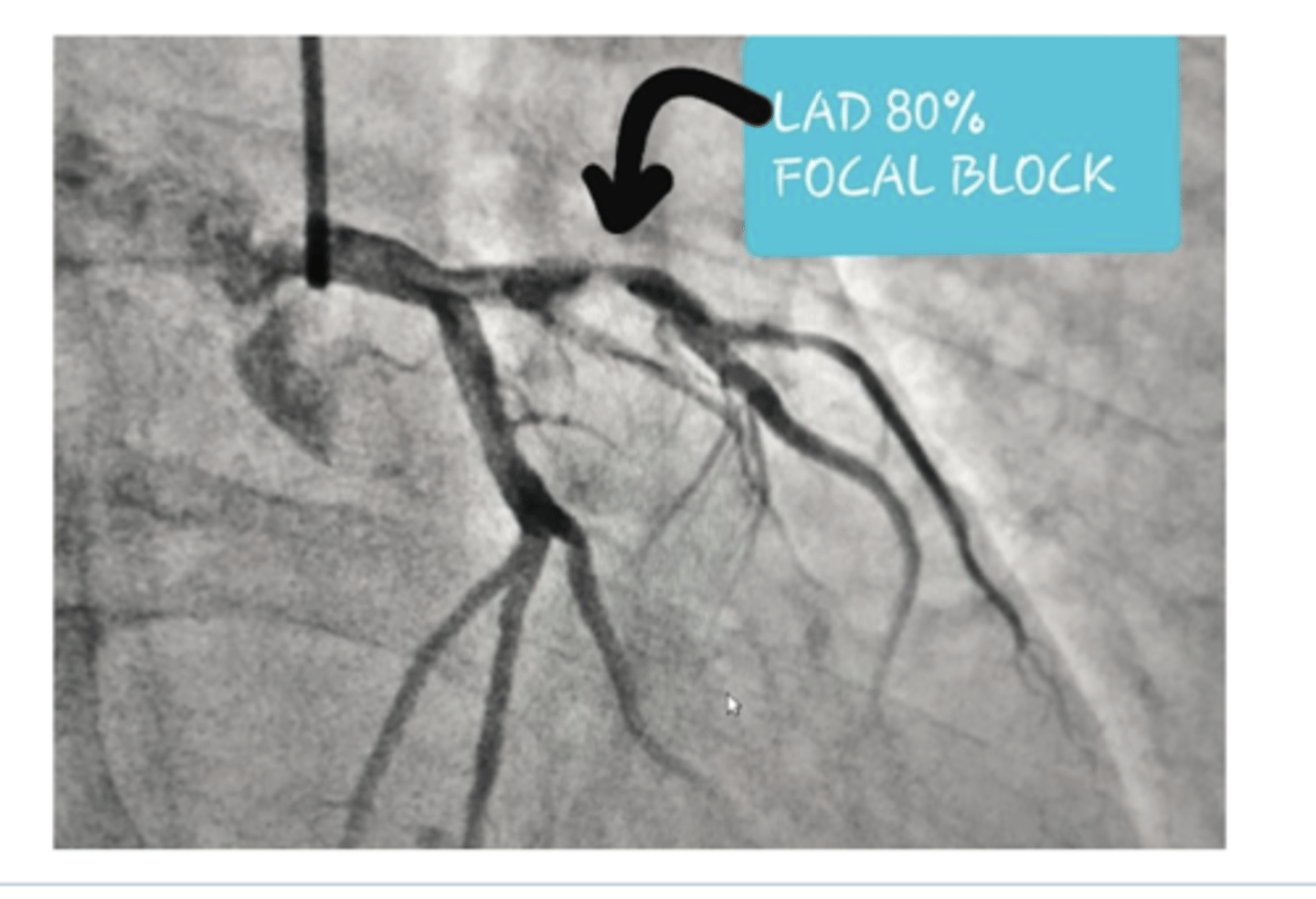
What imaging/tests can be used to eval coronary artery dz? What does each test look for?
◼ A thallium stress test evaluates the musculature of the
left ventricle during rest and under stress.
◼ The echocardiogram looks for regional wall motion abnormalities – can also be done with stress
◼ Coronary angiography (cardiac cath) is the best study to visualize the coronary arteries but is expensive, invasive and involves a high dose of radiation.
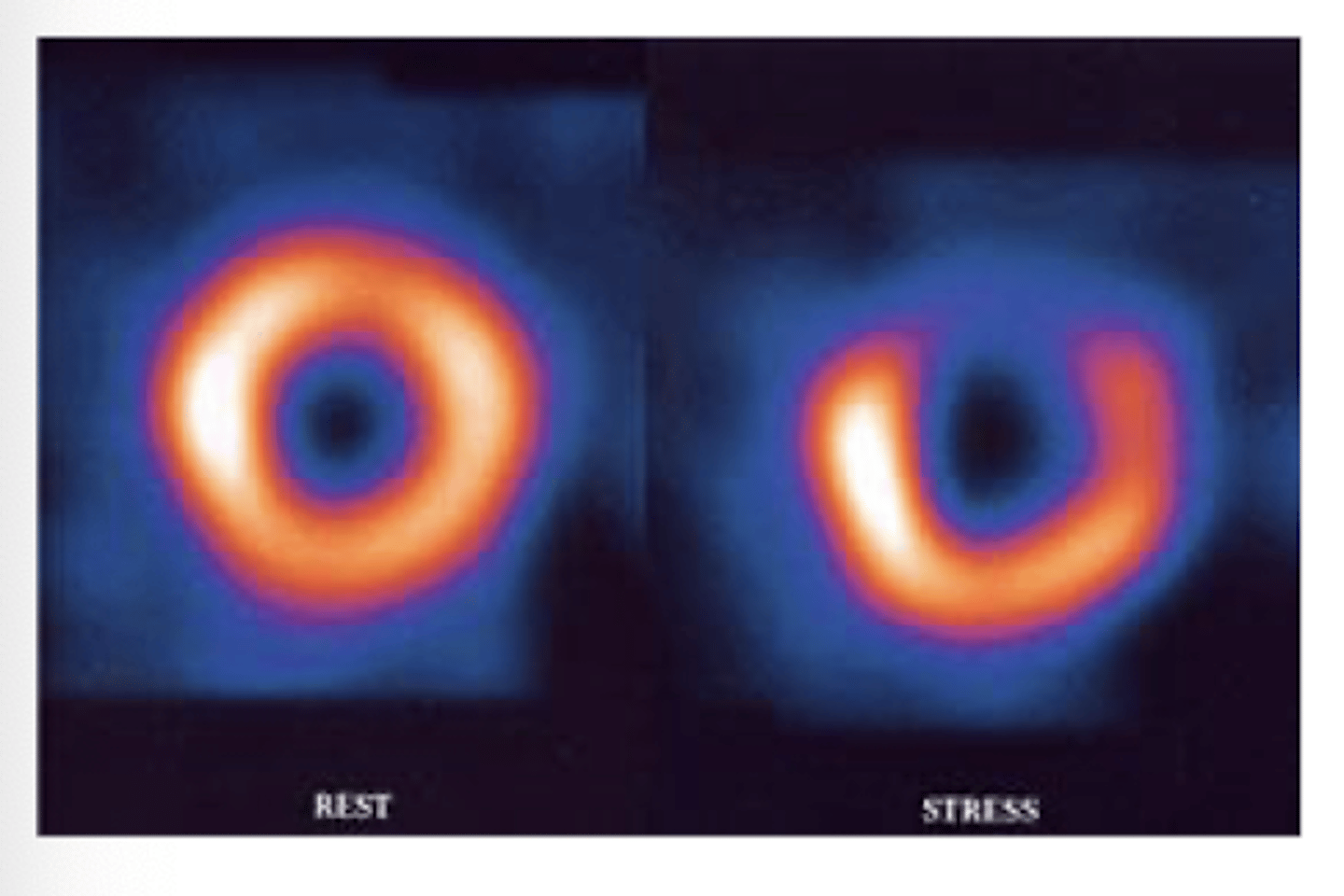
What would an abnormal thallium scan look like?
#1 test for evaluating stress -->.R image indicates void of uptake and dec blood supply
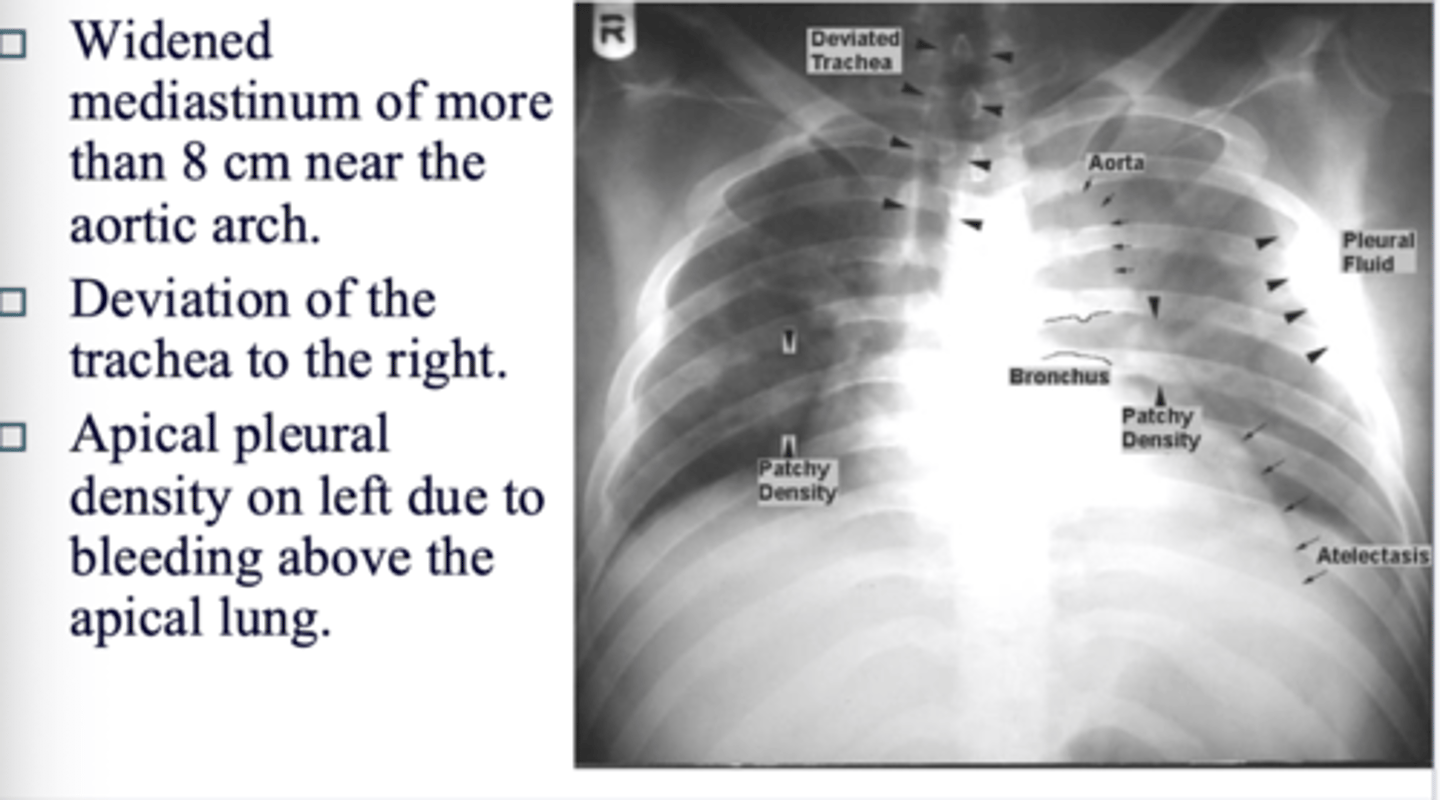
What cause sup to 40% of deaths in MVA's?
aortic tears or ruptures
What is the test of choice for initrial eval of aortic tear or rupture?
CT scan
What are the signs of a tear on CT?
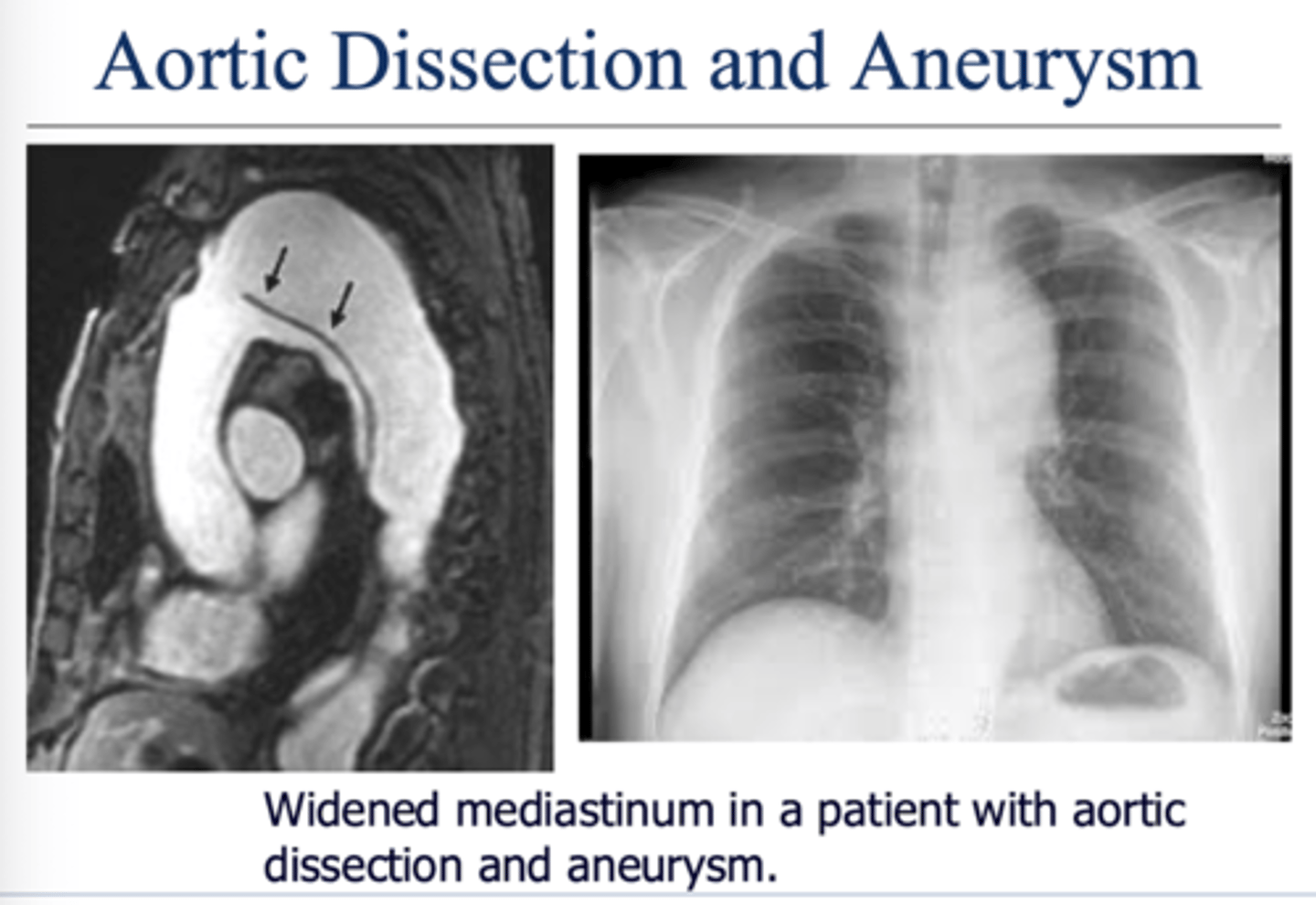
◼ Widened mediastinum of more than 8 cm near the aortic arch.
◼ Deviation of the trachea to the right.
◼ Apical pleural density on left due to bleeding above the apical lung.
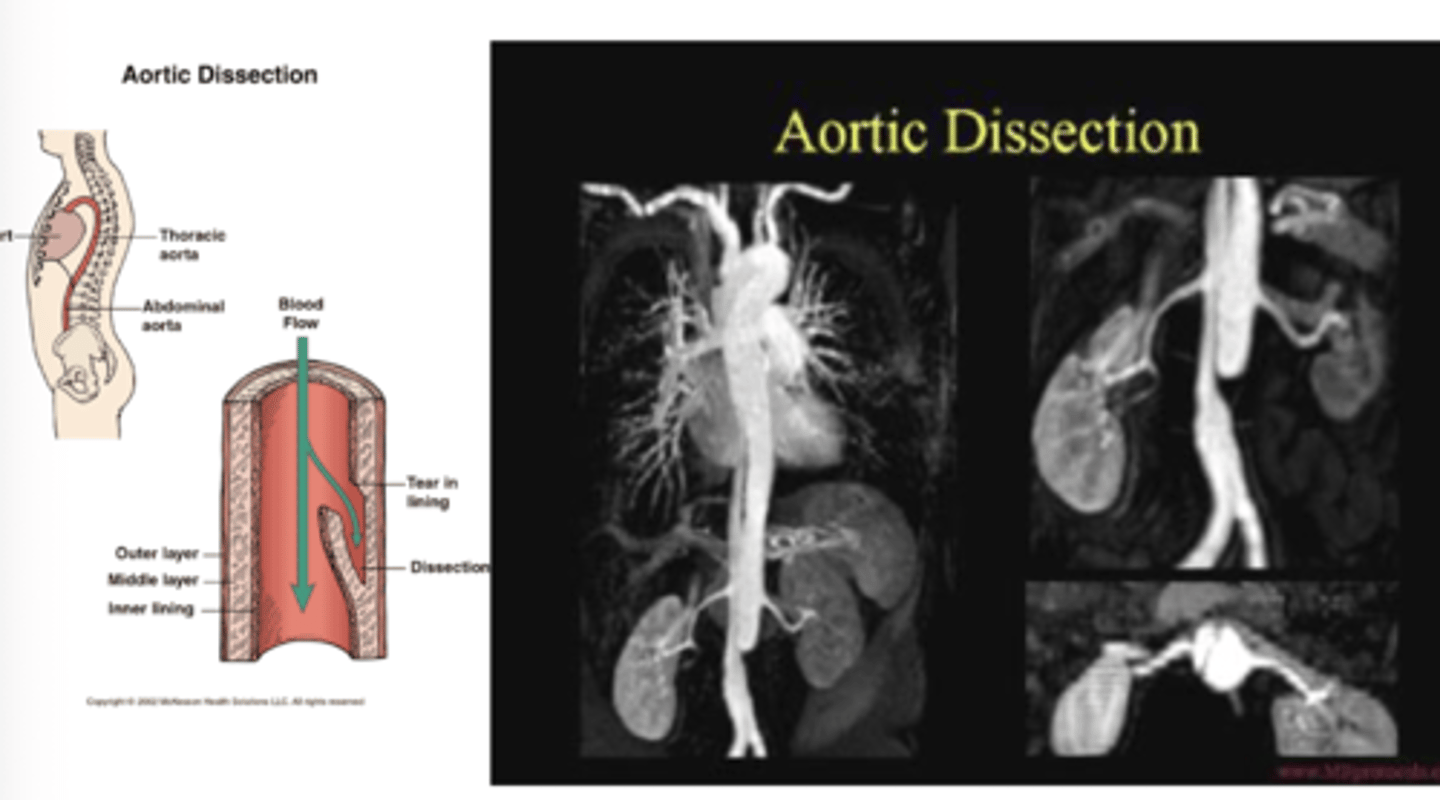
What is aortic dissection?
separation of the layers of the aortic walls allowing blood to flow between the layers of the aortic wall. Often associated with aortic
aneurysm.
What is test of choice with aortic dissection?
CT scan with contrast is test of choice
What is an aortic aneurysm? What is test of choice? At what point is there risk for rupture?
Dilation of the aorta with or without dissection of the aortic wall.
Widening of aorta greater than 5 cm is at risk for rupture
CT scan with contrast
What is the gold standard for evaluating vessels? what is the down side of this testing, and what is used as first line study instead?
contrast angiography - invasive and carries risk of harm to pt
duplex u/s is first line study for vascular dz. can eval anatomy plus direction and magnitude of flow
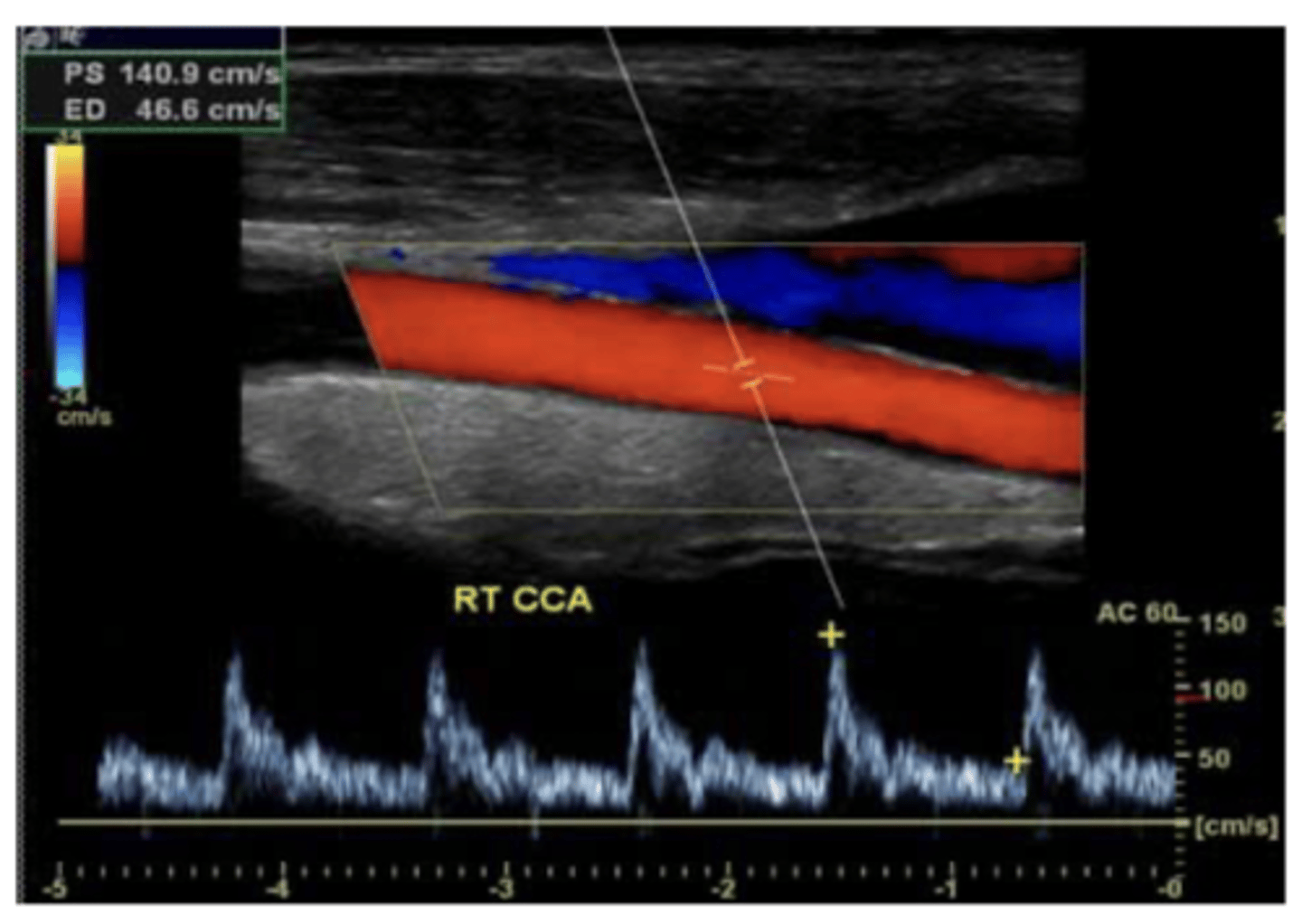
second line study for peripheral vessels
angiography

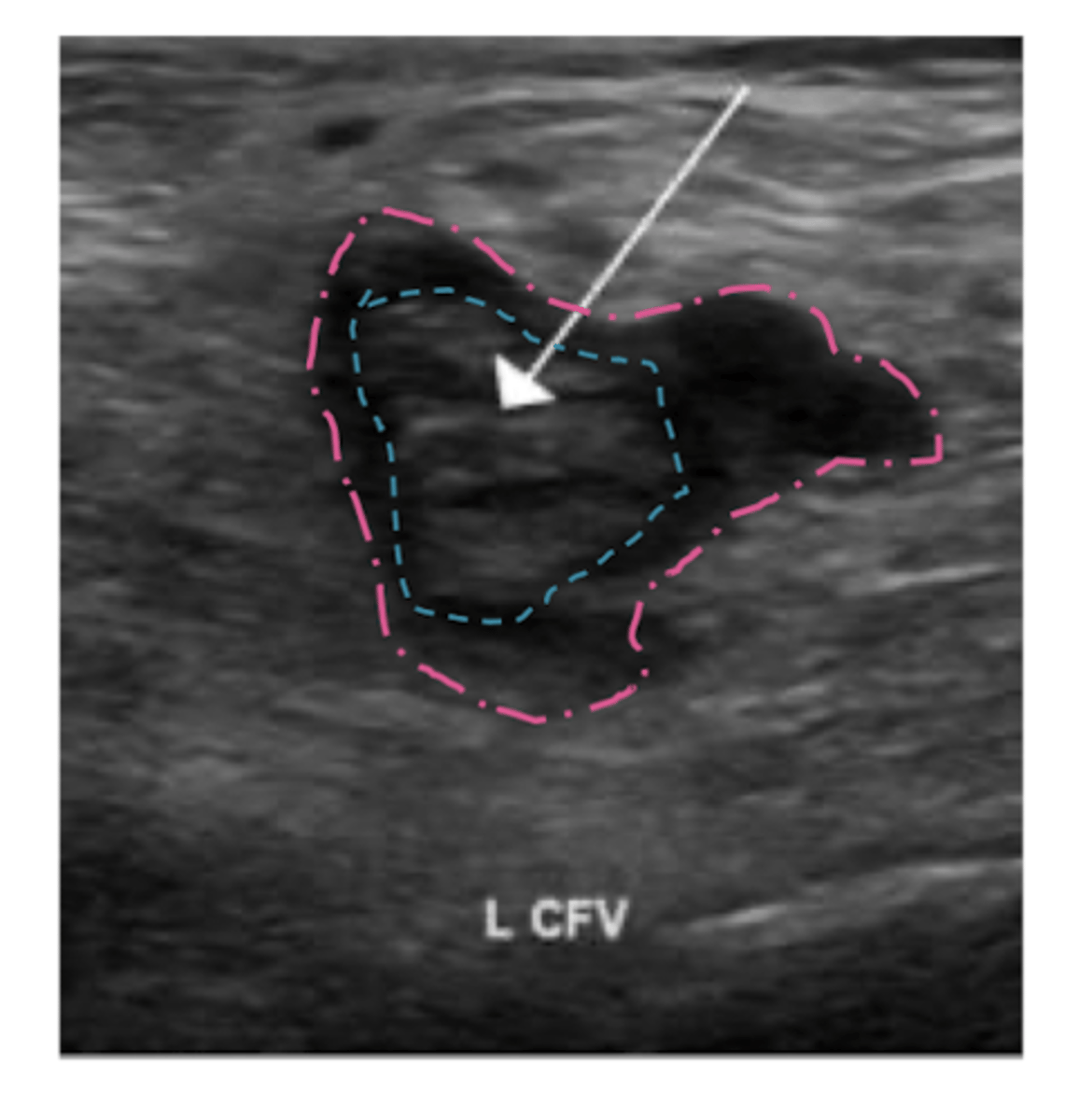
What is initial study of choice for DVT? second line?
duplex u/s of inguinal region, thigh, and popliteal area
second line: contrast venogram
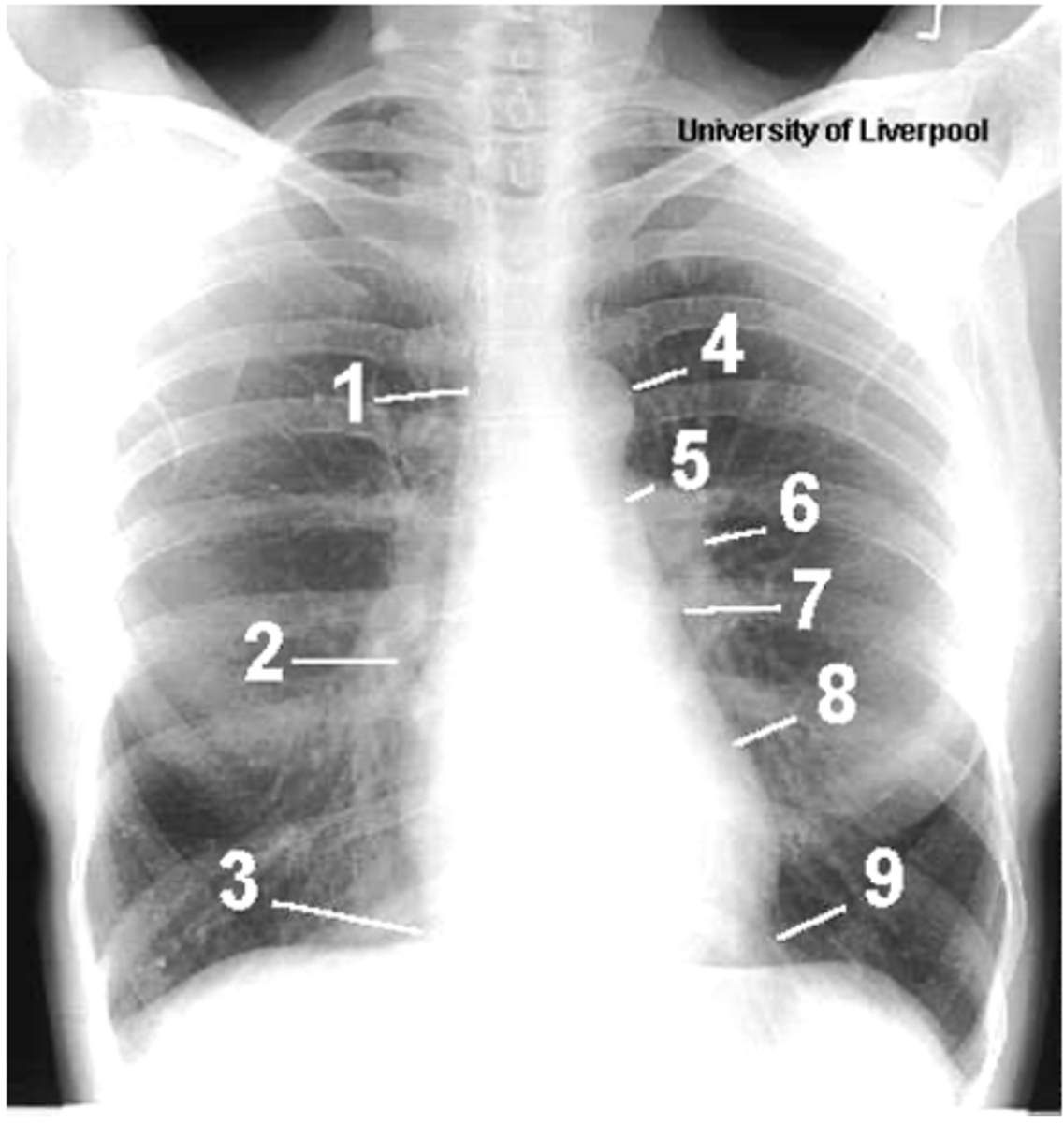
ID structures
1- superior vena cava
2- right atrium
3- inferior vena cava
4- aortic arch or knob
5- left pulmonary trunk
6- left pulmonary artery
7- left atrium
8- left ventricle
9- left cardiophrenic angle
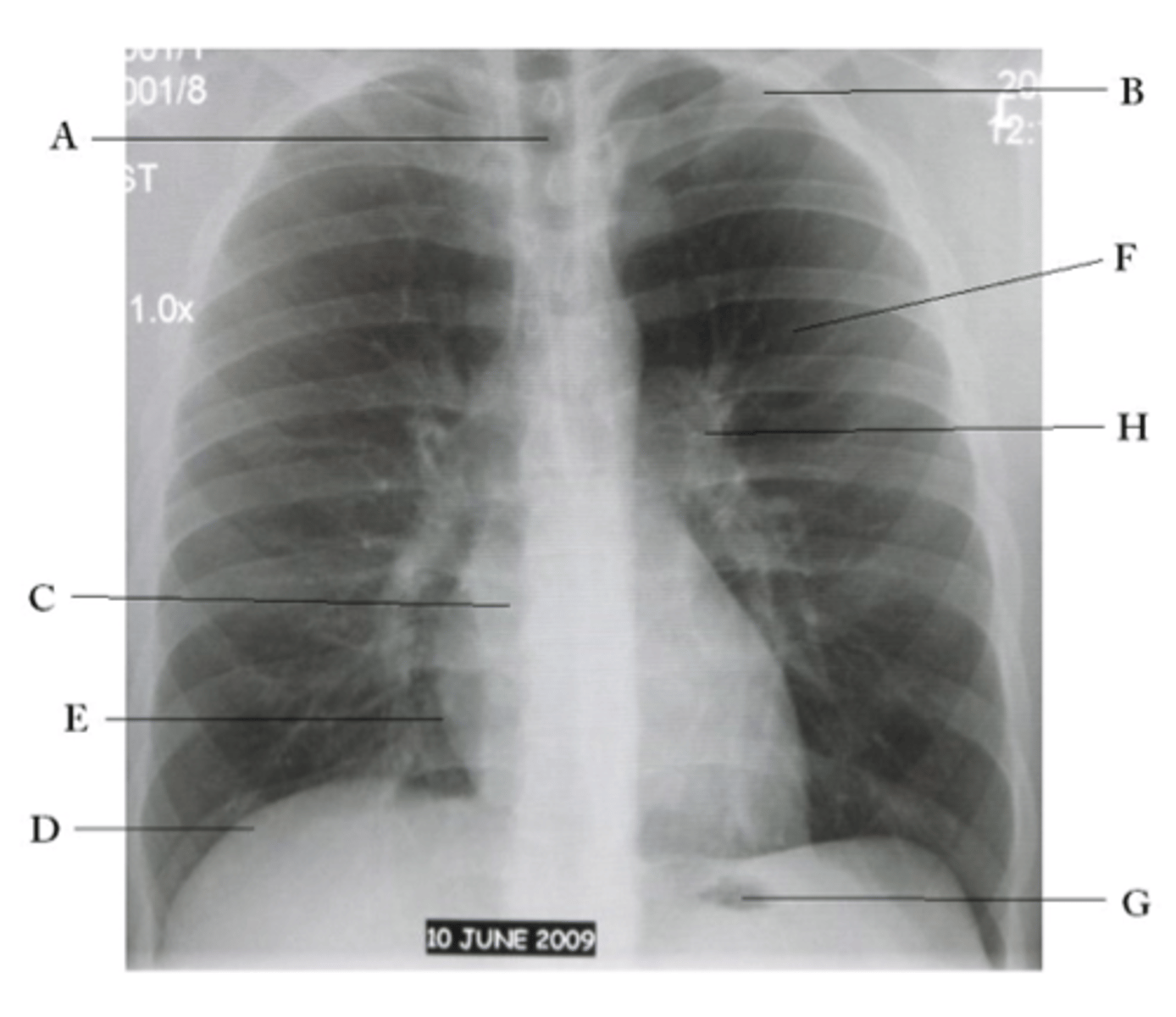
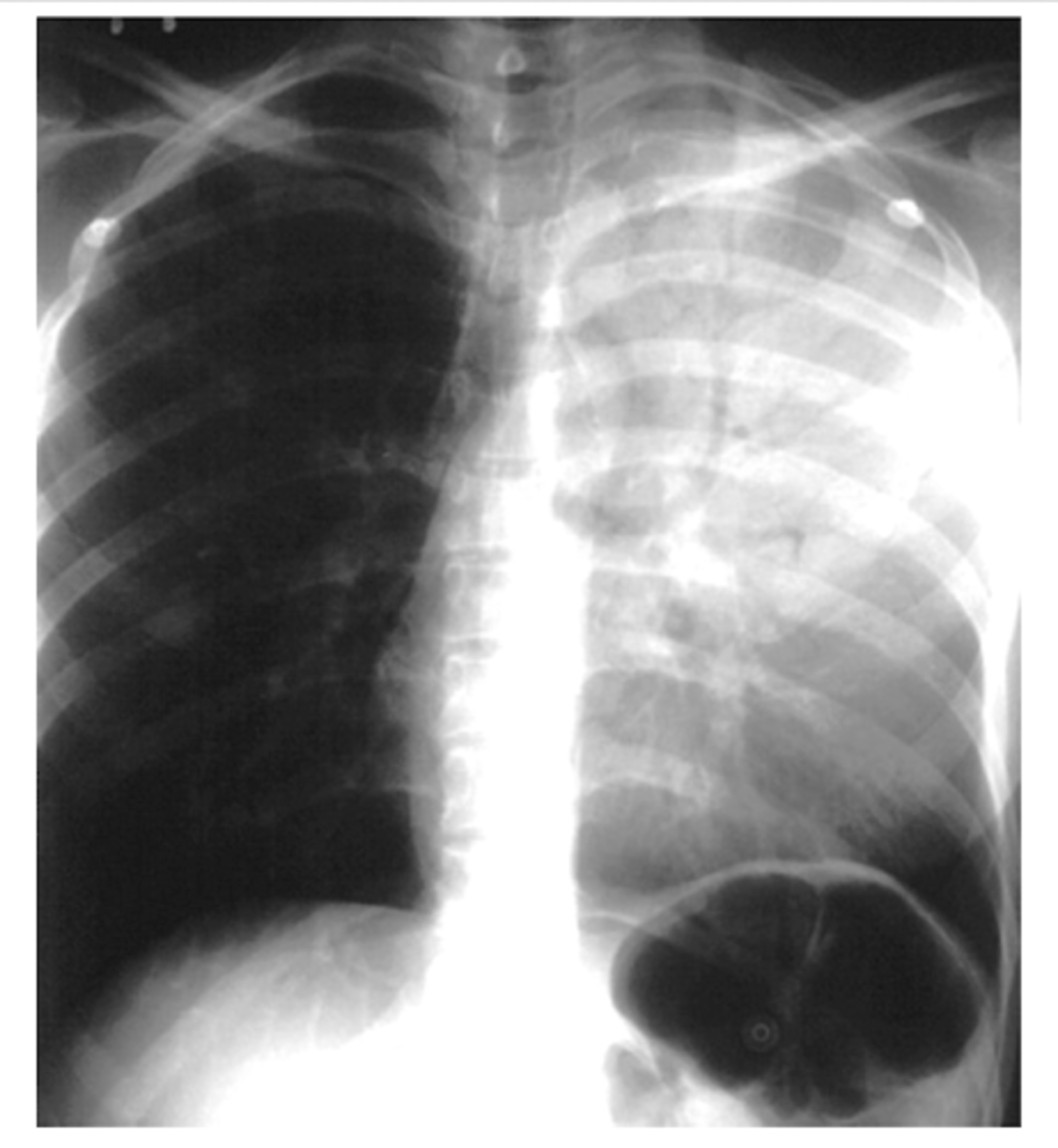
ID structures
oA - Trachea
oB - Clavicle
oC - Right Atrium
oD - Diaphragm
oE - Cardiophrenic angle (Costocardio)
oF - Left upper lobe
oG - Gastric Bubble
oH - Left Hilum
Define interstitial
tissue outside of the alveoli are affected. (diffuse)
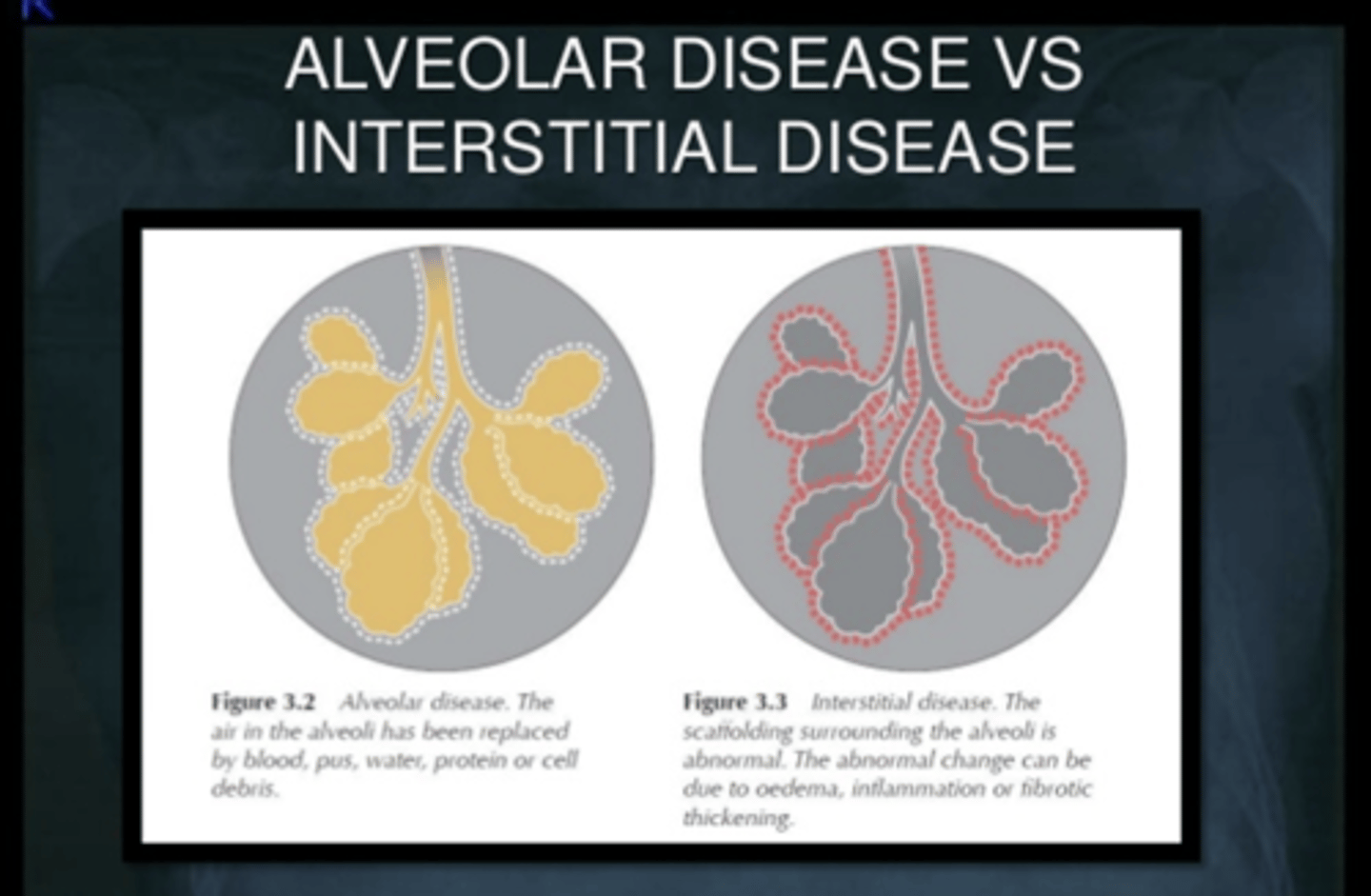
Define alveolar
o alveolar spaces are filled with some material such as blood, pus, fluid or cells (tends to be localized)
In a normal lung, what will bronchogram show?
Both the bronchi and the surrounding alveoli are filled with air, making the bronchi invisible on an X-ray.
What pathological processes can cause infiltrates?
- non specific....but CHF, pulmonary fibrosis, collagen vascular diseases, etc.
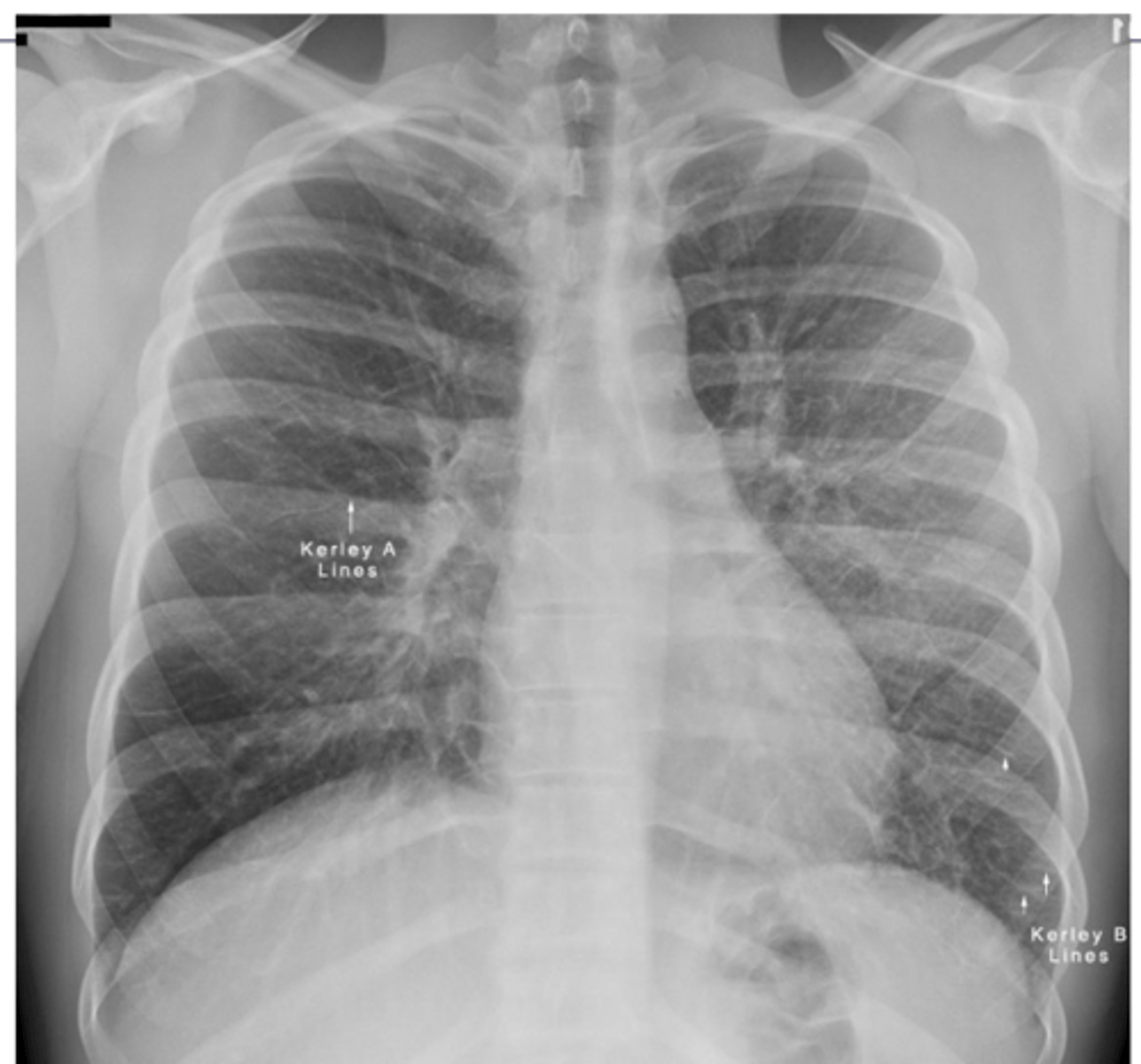
What are kerley A and B lines?
•Kerley A lines are linear opacities extending from the periphery to the hila caused by distention between peripheral and central lymphatics
•Kerley B lines are small, horizontal, peripheral straight lines demonstrated at the lung bases that represent thickened interlobular septa on CXR.
What does alveolar infiltrate look like?
alveolar infiltrate - looks "fluffy
Dx middle
lung fibrosis
What does an air bronchogram sign look like? What causes the abnormal appearance?
Alveoli are white but bronchi remain dark creating a visible pattern
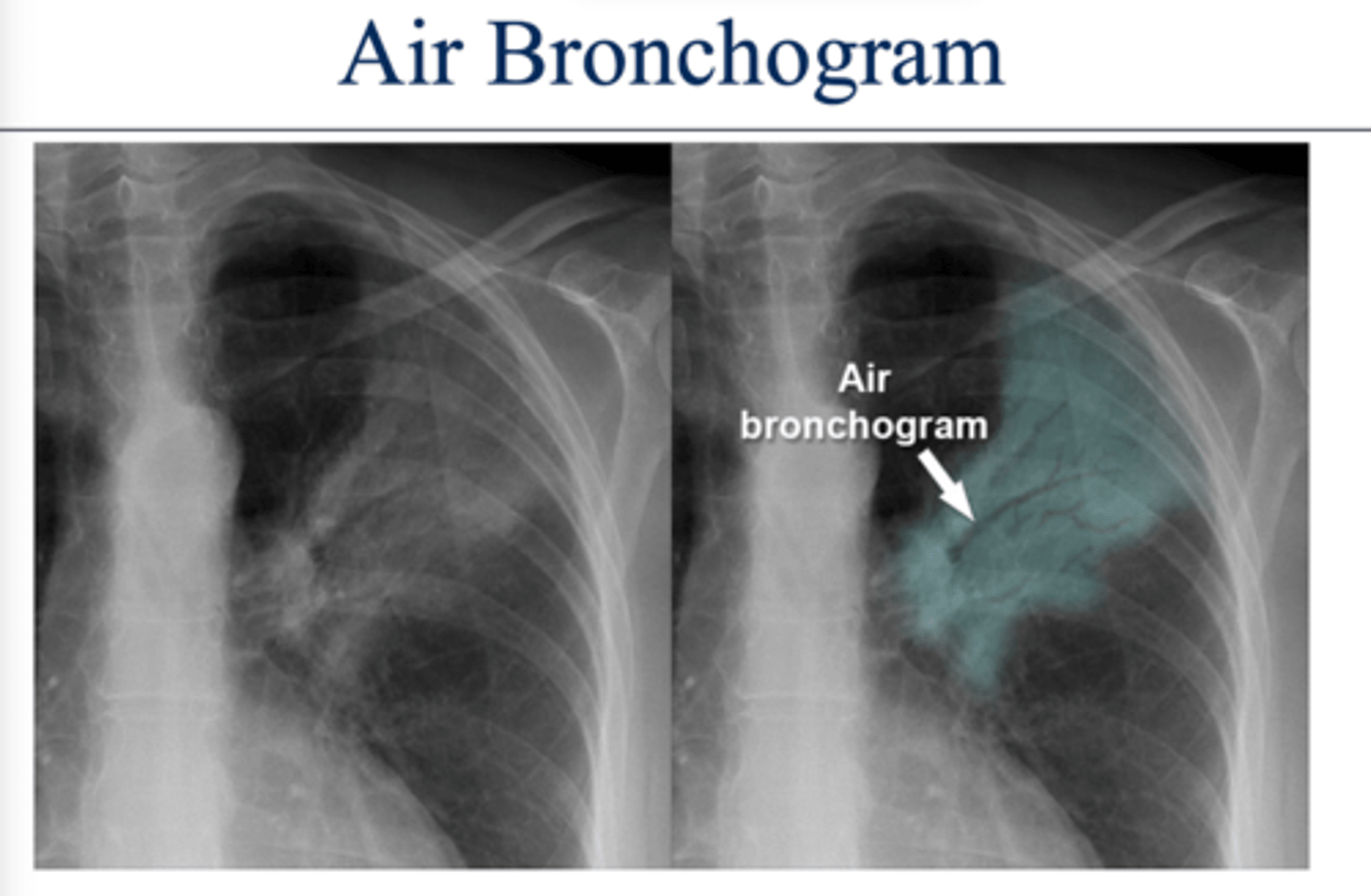
What dz would have an air bronchogram sign?
Pneumonia.
The infection causes the alveoli to fill with fluid.
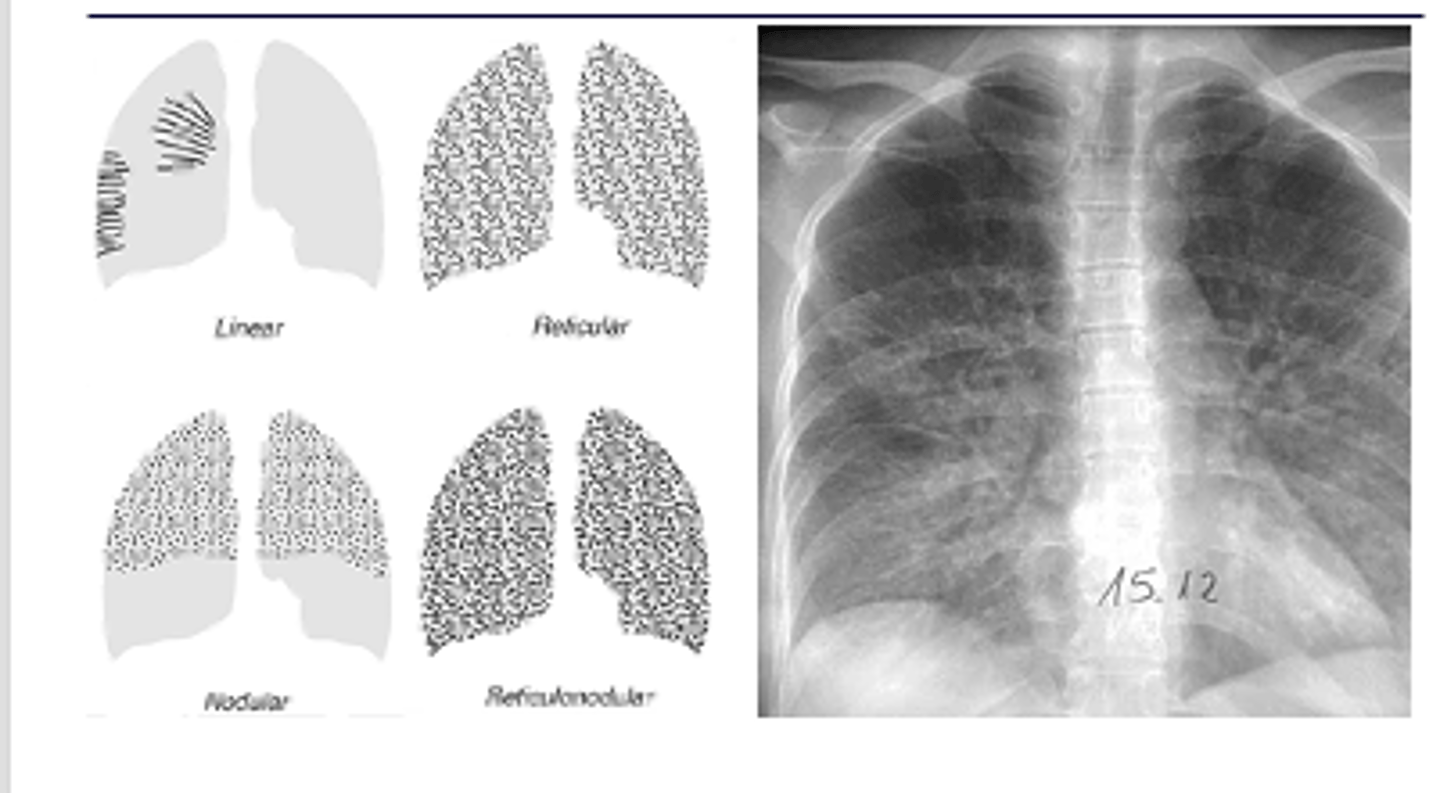
What do interstitial infiltrates look like and what are some causes? IS this sign specific or non specific?
caused by acute and chronic disease processes that affect the tissue outside of the alveoli.
Interstitial processes are usually diffuse & are seen as thin white lines. May appear honeycombed (reticular)
Interstitial infiltrates are nonspecific as they can be caused by many processes such as CHF, pulmonary fibrosis, collagen vascular diseases, etc.
What are linear interstitial infiltrates also called? What is this sign commonly associated with?
Kerley lines --> interstitial pulm edema
What is reticular opacity? What is this difference between fine and coarse?
Coarse - greatest width of opacity (fine on L and coarse on R)
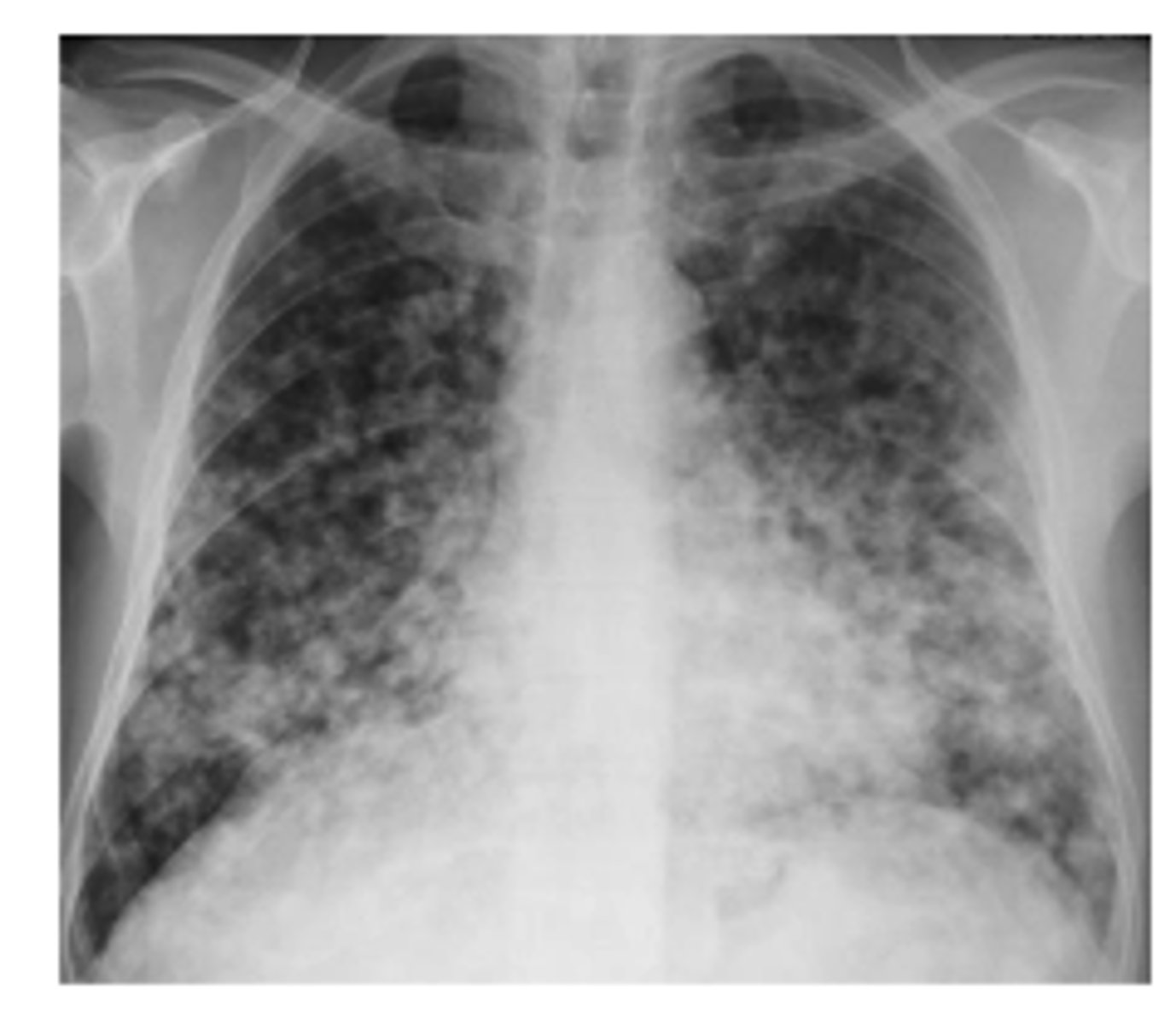
Describe nodular pattern interstitial infiltrate
Nodular
A nodular pattern consists of multiple round opacities, generally ranging in diameter from 1 mm to 1 cm
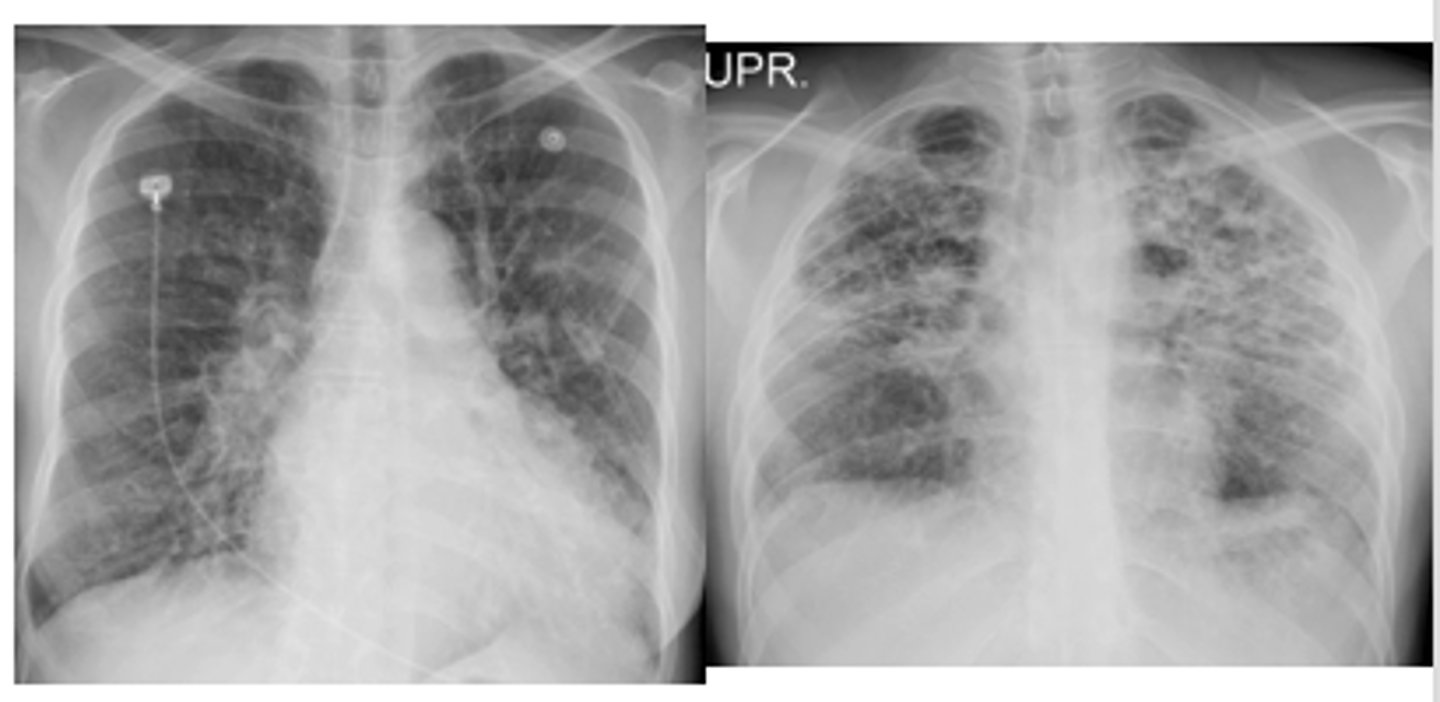
What 2 patterns can community acquired pneumonia appear as? Typical patterns of bacterial, viral, mycoplasma and conolidation
Alveolar or interstitial
oBacterial – usually alveolar and focal
oViral and mycoplasma– usually interstitial and diffuse
oA consolidation = severe alveolar infiltrate
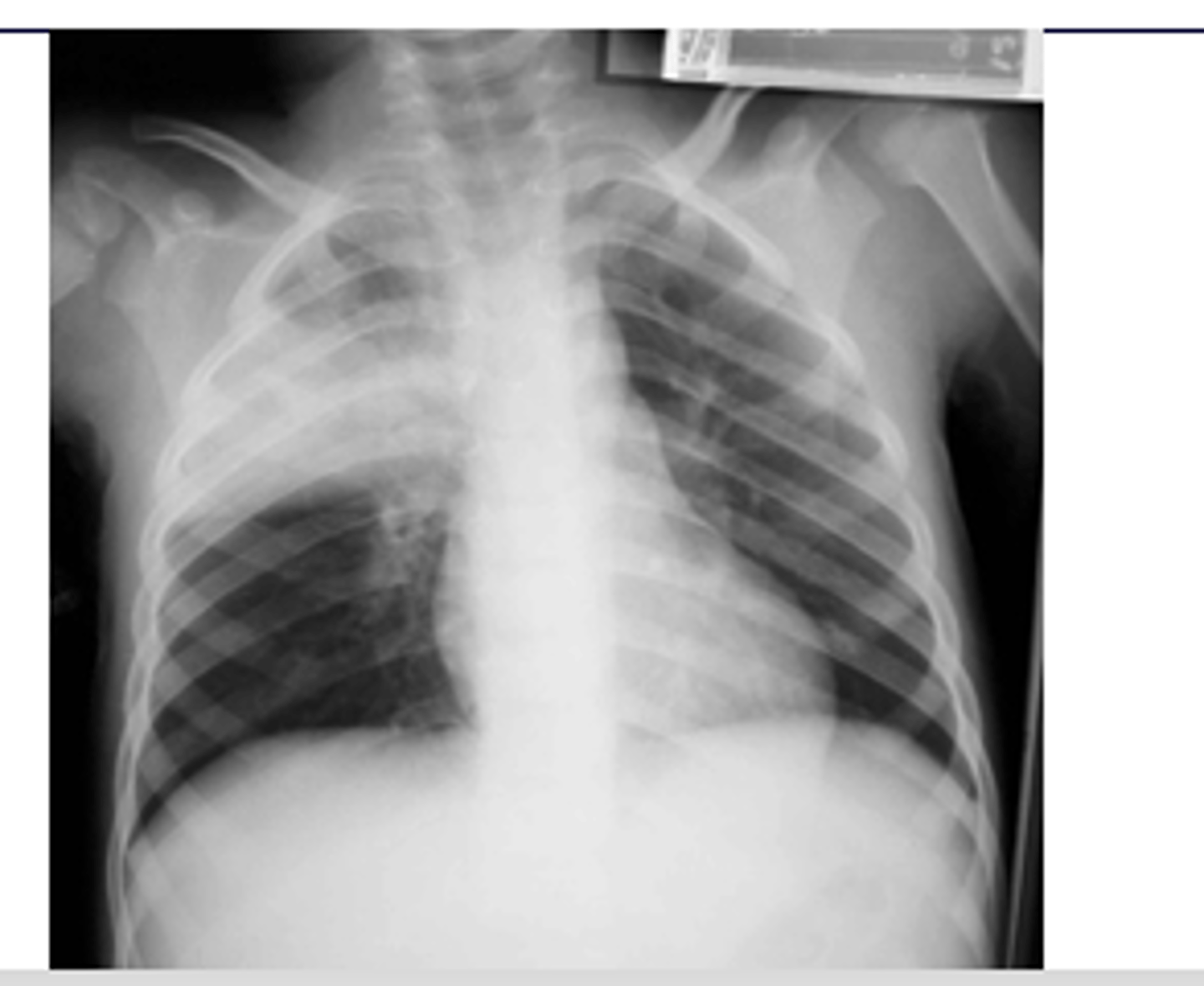
ID picture on back
LLL pneumonia
ID picture on back
RUL pneumonia with air bronchogram sign
What is the silhouette sign? What does it help determine?
oHelps determine the location of an abnormality in comparison to normal anatomy.
oLoss of a normal border and contour occurs if there is an abnormality contiguous with that structure (next to)
EX: if the R cardiac border is obscured, then the infiltrate must be in the medial segment of the R middle lobe.
(pic also has spine sign)
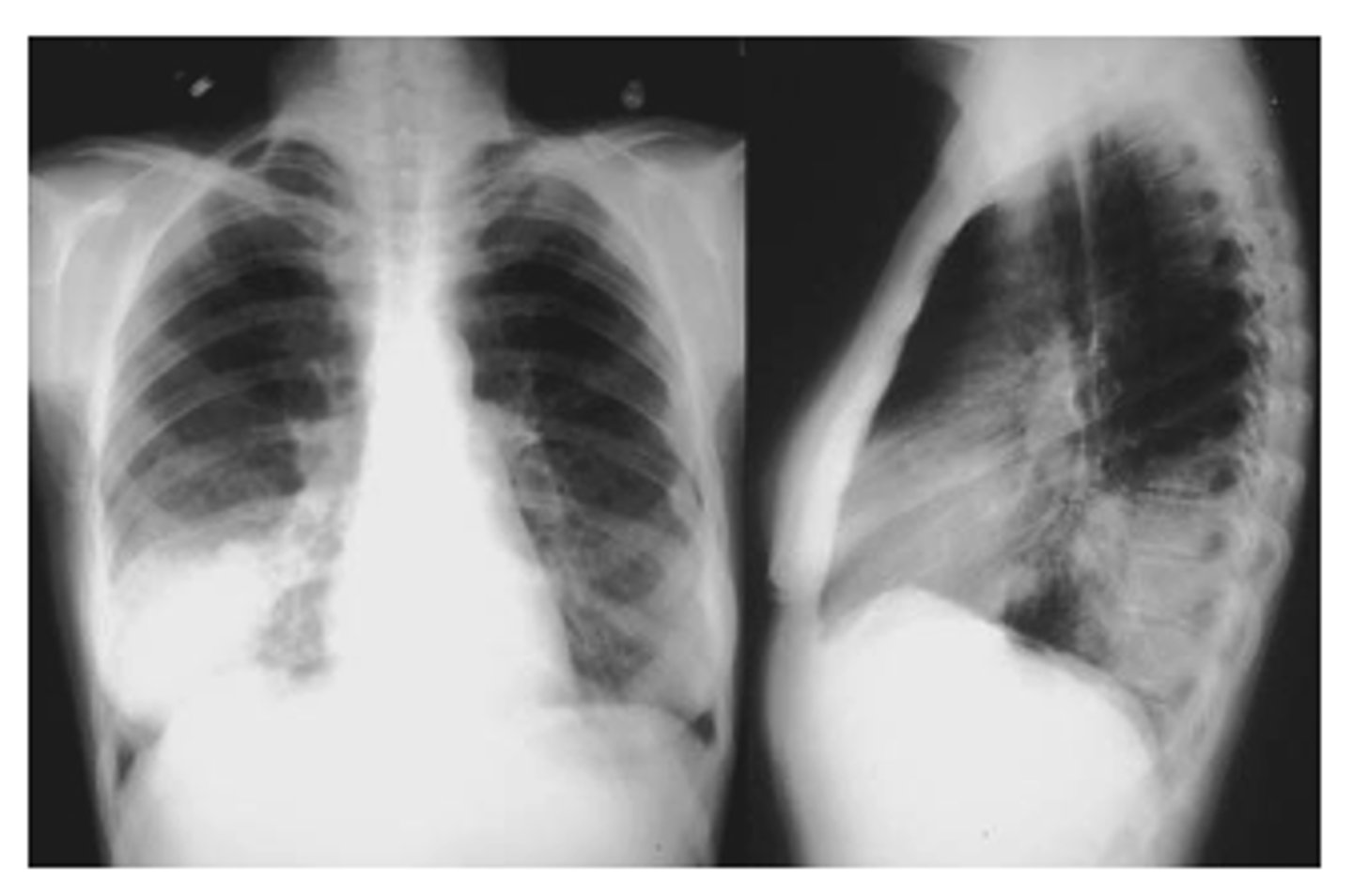
ID sign on back and finding
RML pneumonia obscuring the cardiac border but not the R hemidiaphragm. Note the triangular density on the lateral view.
What is spine sign?
oSpine sign = vertebral bodies are lighter (white) than normal
What x-ray findings indicate atypical pneumonias caused by mycoplasma, viruses or pneumocystis? Most common pathogen
Pneumonias that are interstitial and symmetrically diffuse in both lungs
Path: mycoplasma
What x-ray finding is indicative of CAP and is more common in children than adults? What can this be mistaken for?
Round pattern
oCan simulate a mass lesion such as a neoplasm.
What type of pneumonia is commonly find in immunocompromised pts? How will the x-ray pattern evolve with dz progression?
oPneumocystis jiroveci pneumonia (PJP) evolves from a normal CXR to an interstitial pattern (diffuse) to an alveolar pattern (localized).
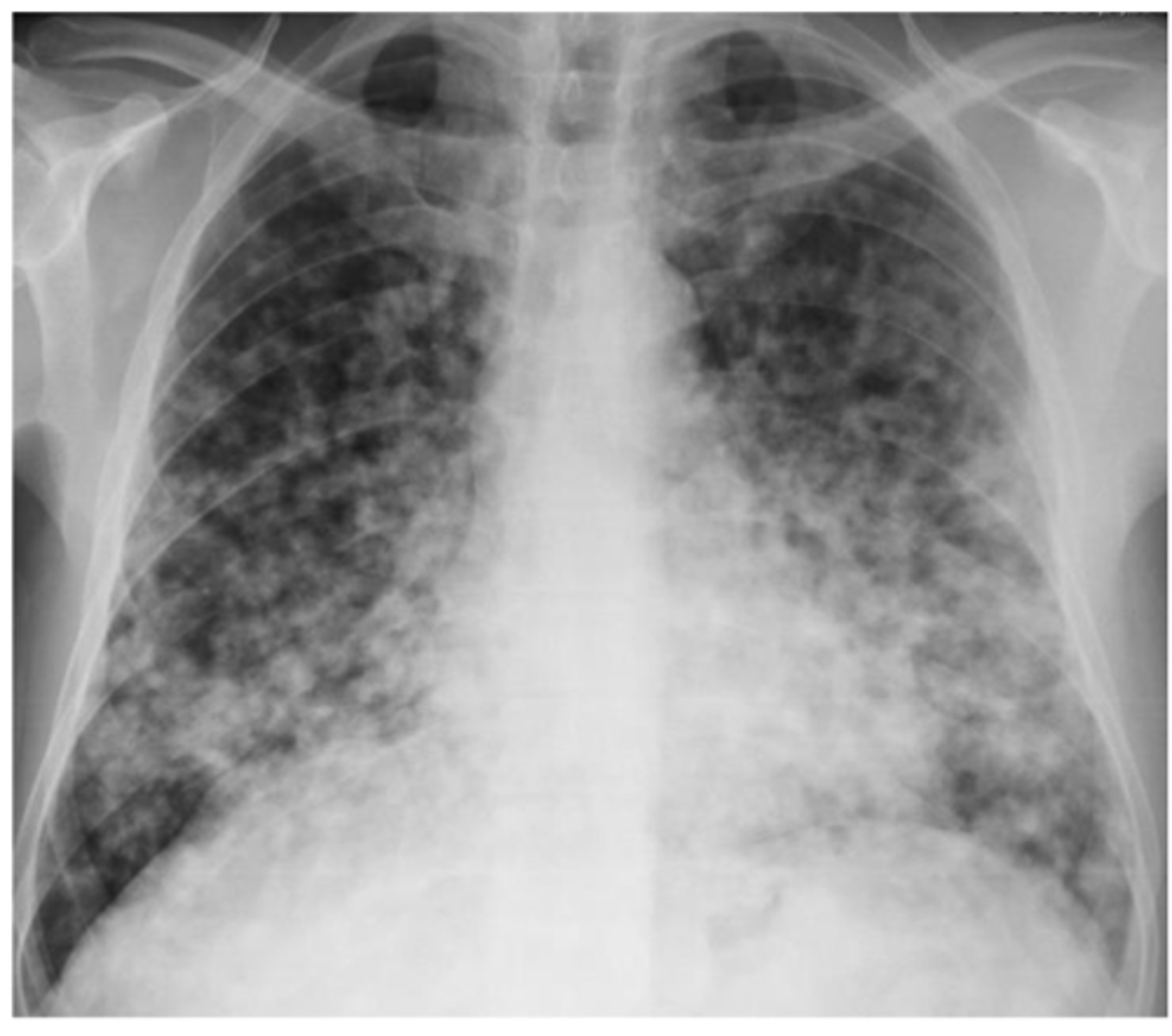
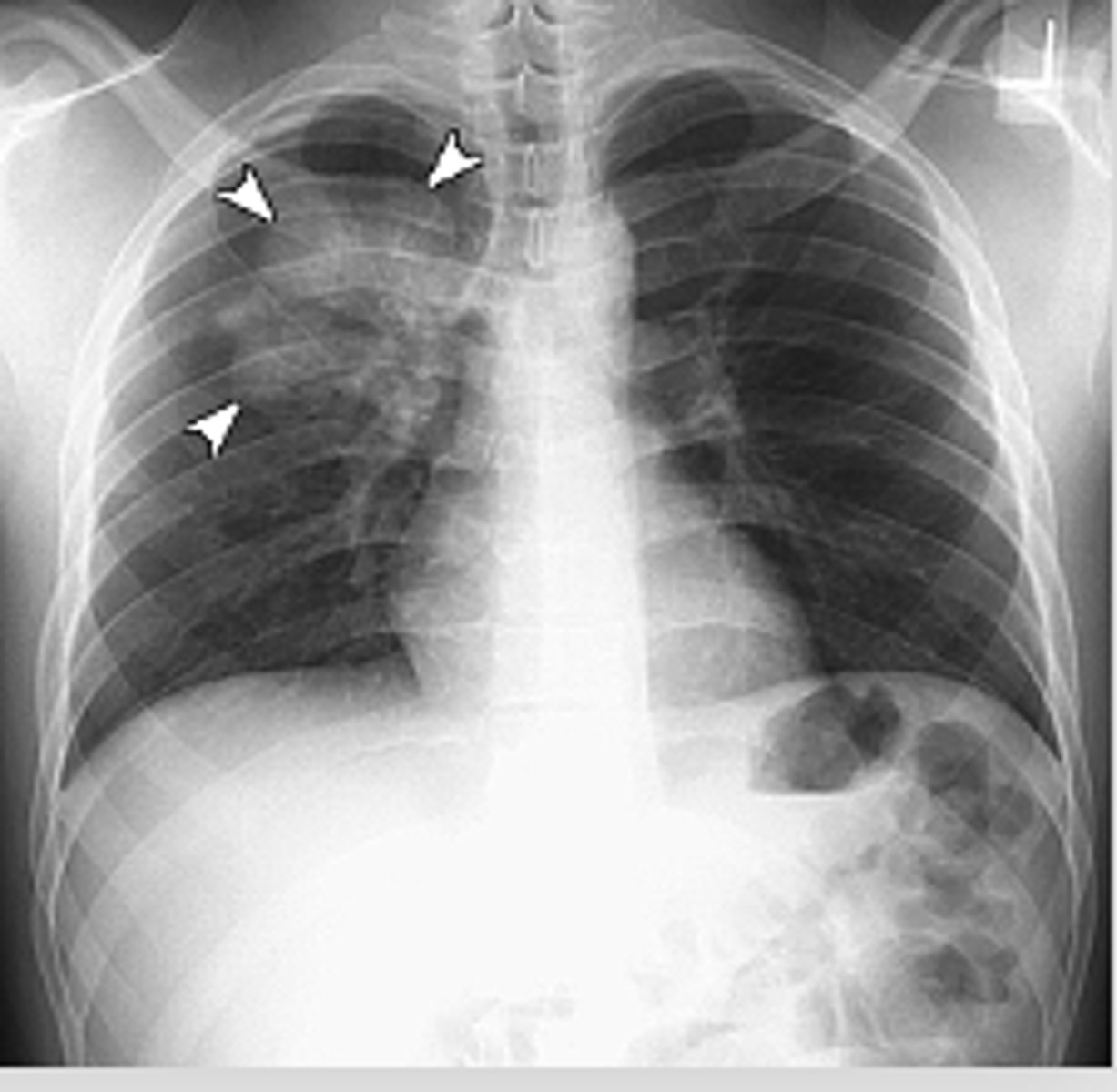
What is the pattern on the image of the back of the card?
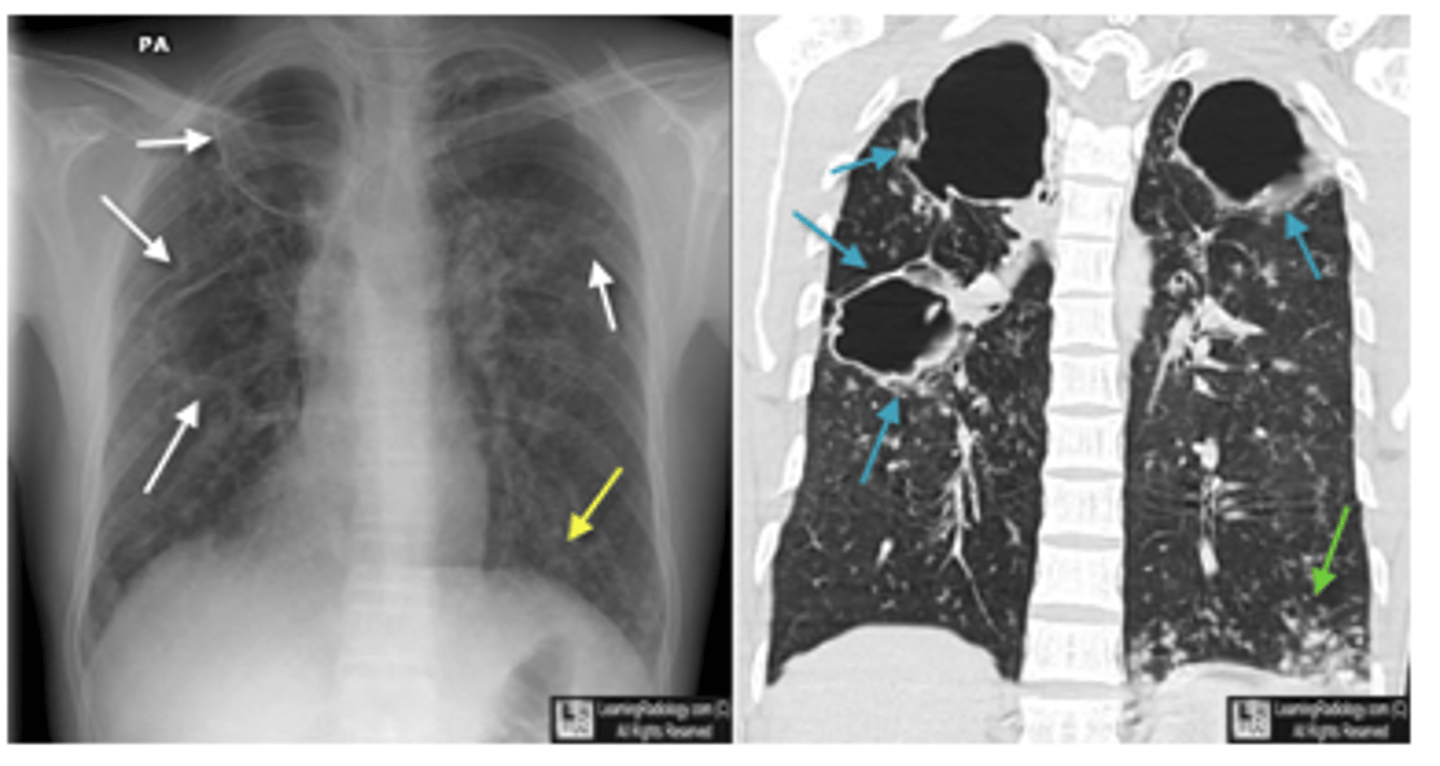
Cystic PJP - PA chest radiograph shows diffuse bilateral reticulonodular interstitial infiltrates

What is aspiration pneumonia? What x-ray finding will be seen?
Gastric contents or other bodily fluids can be aspirated into the lungs
patchy, alveolar infiltrate
Common x-ray finding of primary active TB
oEnlargement of hilar or mediastinal lymph nodes is present about 95% of the time in primary active TB.
oCalcification usually occurs at the site of infection or in the node or both.

Common x-ray finding of military TB. What makes military TB particularly deadly?
diffuse bilateral infiltrates with very small nodules
-late phase of TB: potentially fatal form of the disseminated disease due to the hematogenous spread of tubercle bacilli to the lungs, and other organs.

What is cavitary TB? What will X-ray look like?
oCavitary TB is also a late phase of TB.
oHealing leads to fibrososis and calcifications which may pull the hilum up on the affected side.
X-ray will have dark spots indicating holes/cavities
What are the key differences between ghon and ranke complexes?
Key Differences:
Stage of Disease:
1. Ghon complex: Represents the active or primary stage of TB infection.
2. Ranke complex: Indicates a healed or inactive stage of TB.
Calcification:
1. Ghon complex: May or may not be calcified.
2. Ranke complex: Is fully calcified.
Clinical Significance:
1. Ghon complex: Shows an active or recently acquired TB infection.
2. Ranke complex: Suggests the patient has had TB in the past, and the infection has resolved.
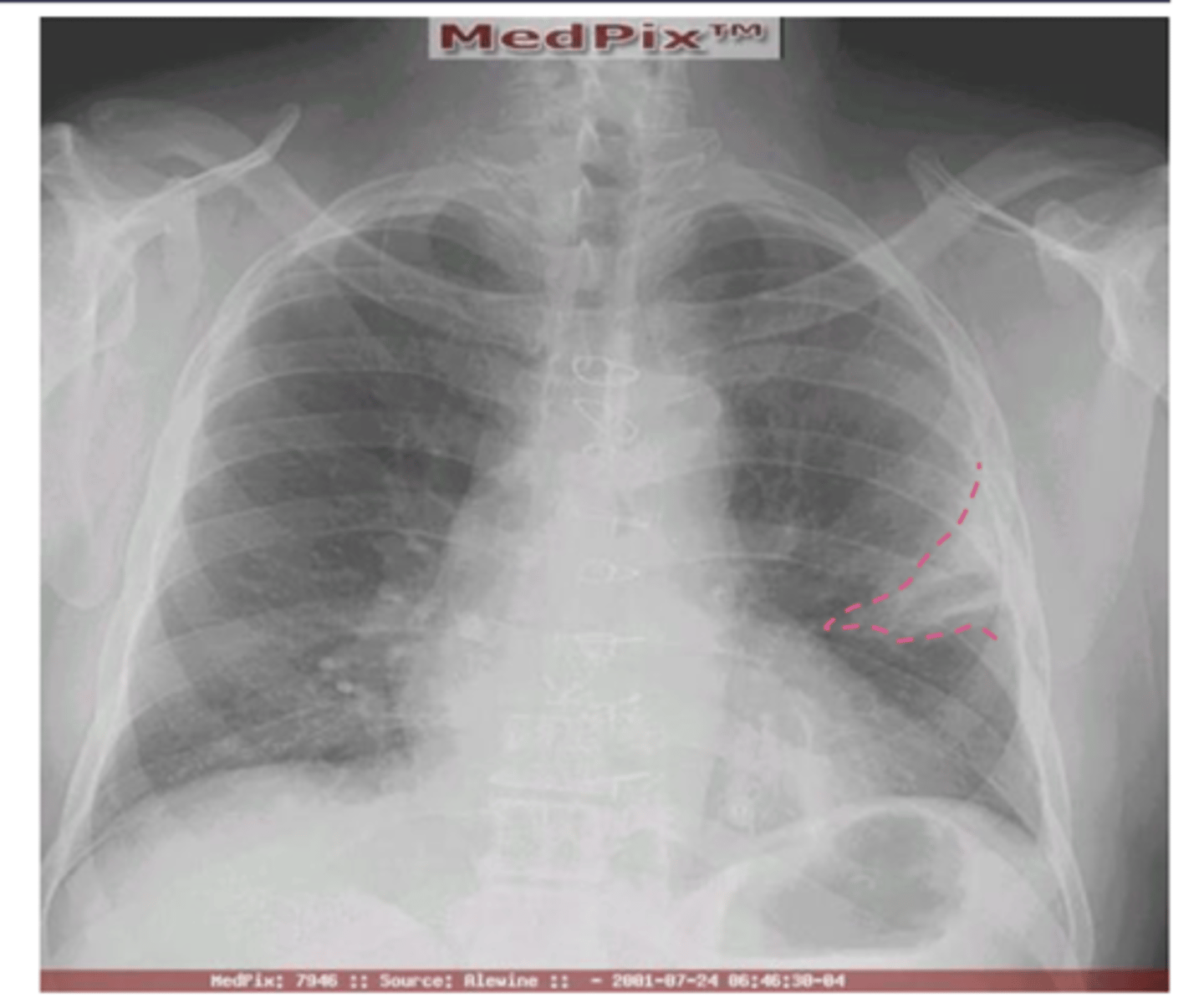
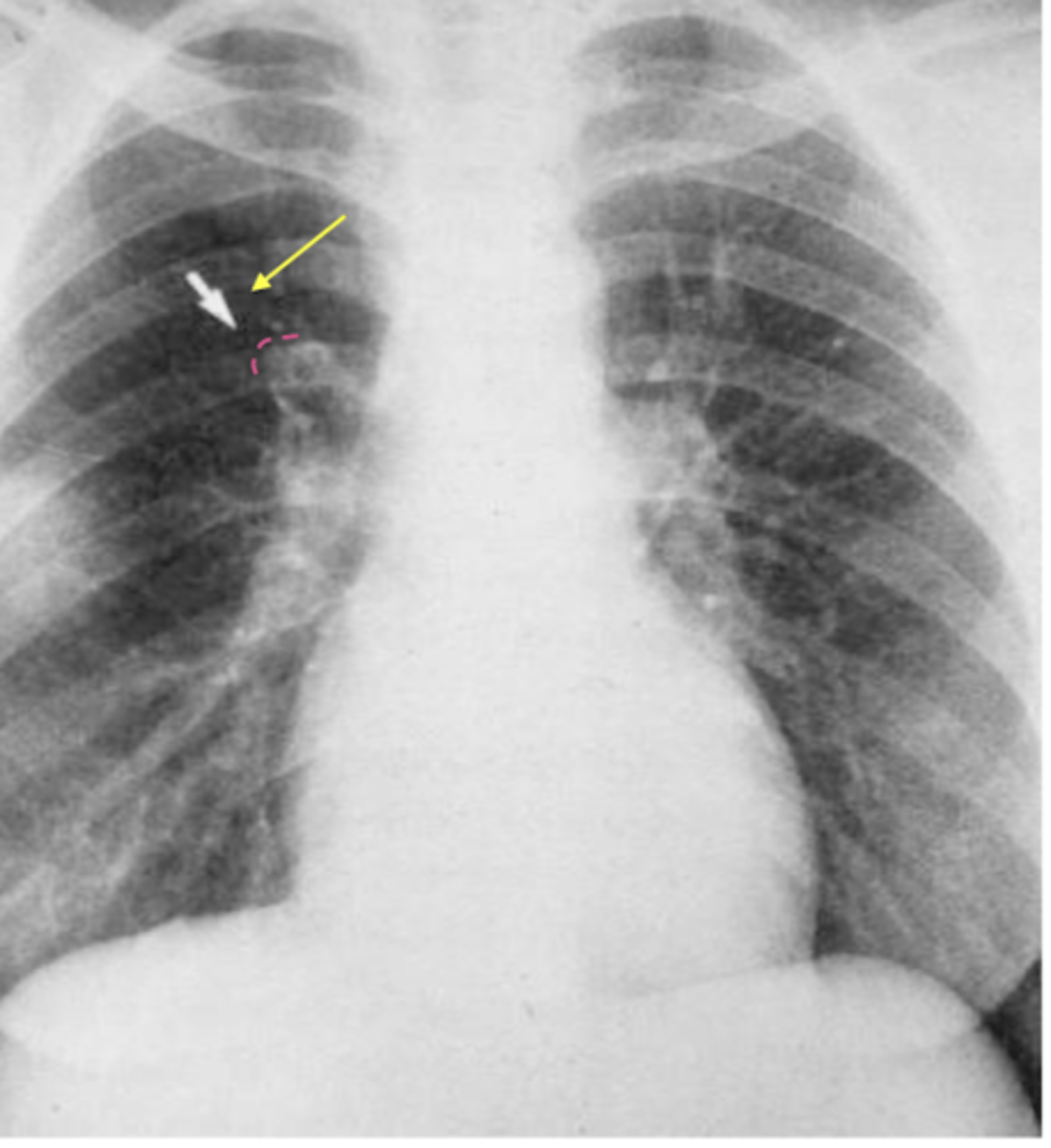
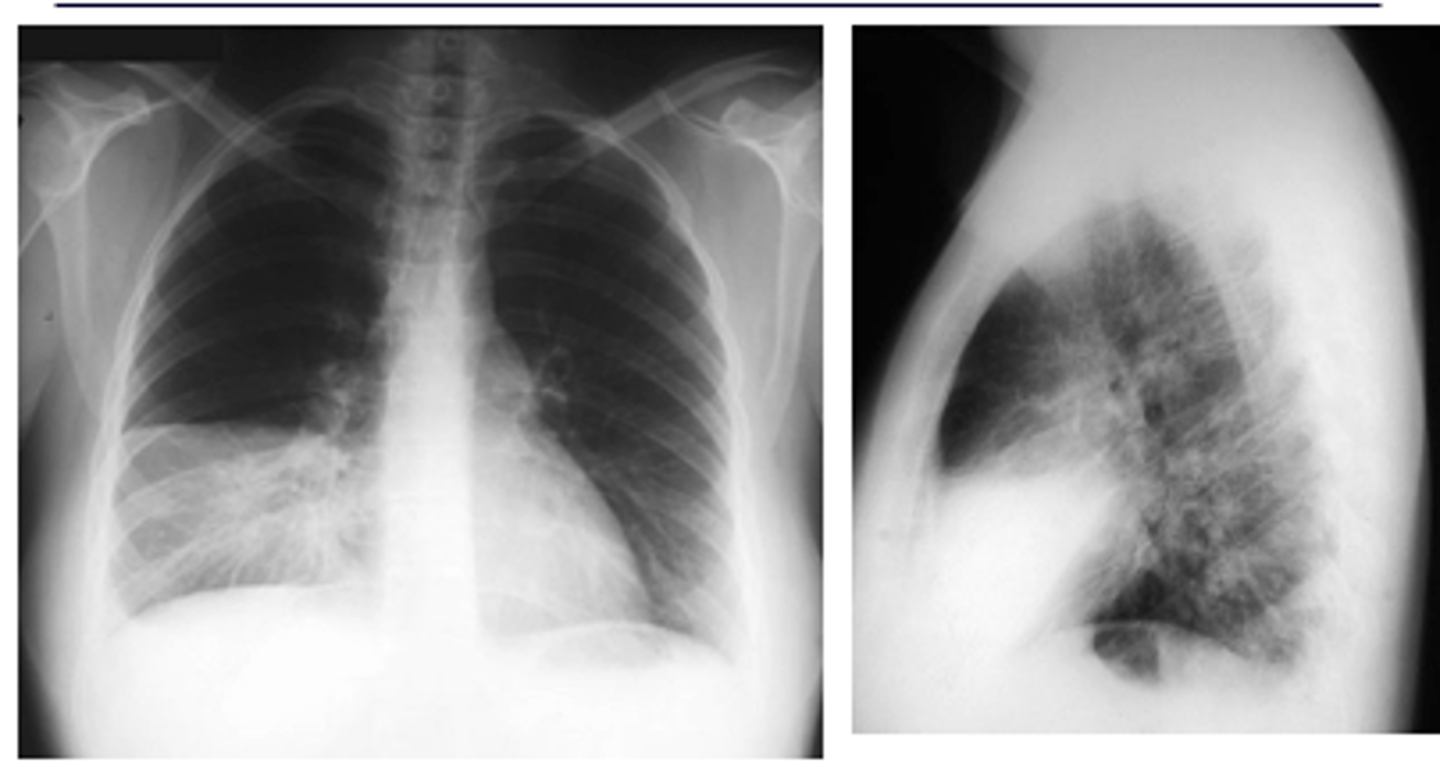
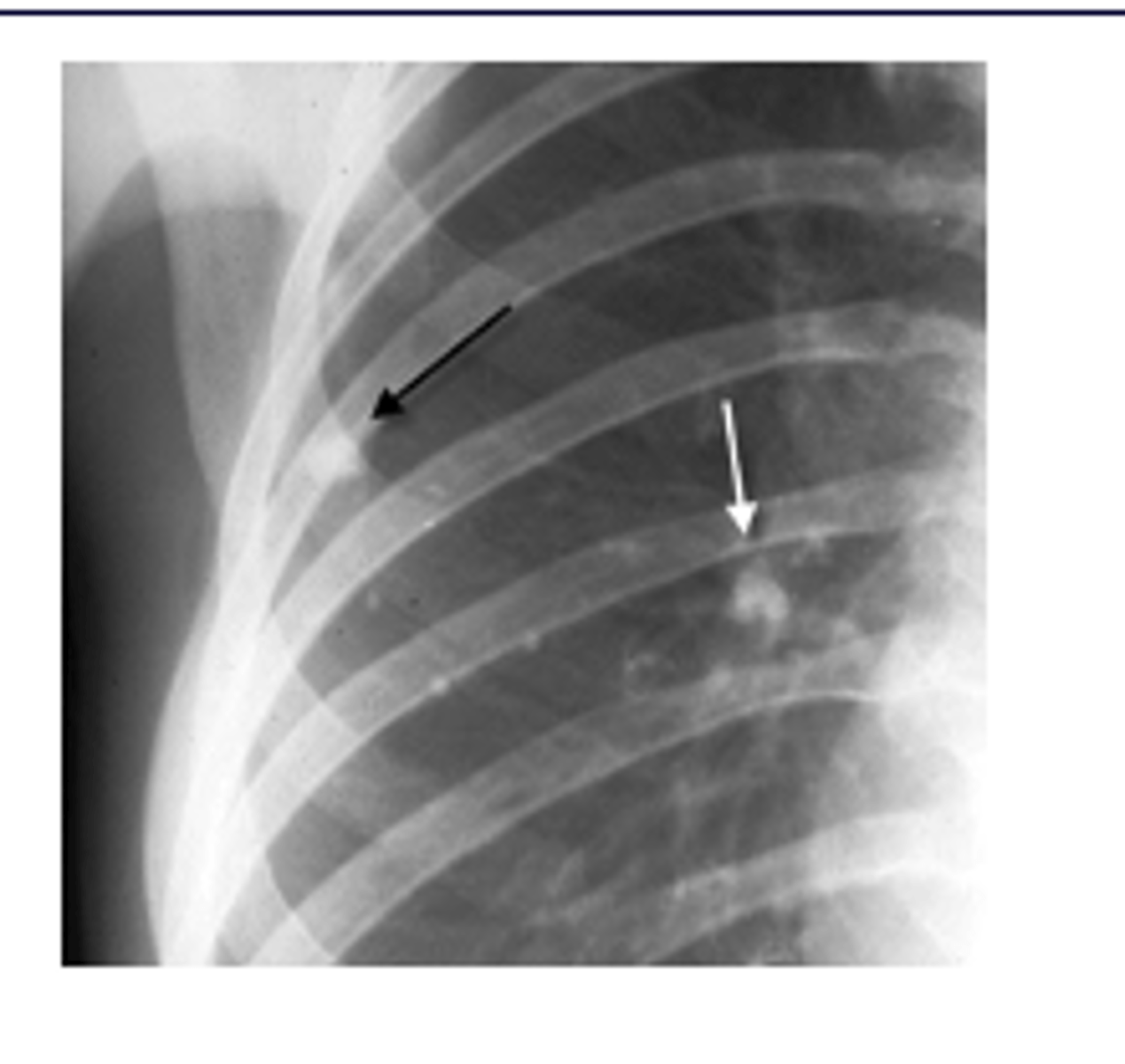
ID Ghon and Ranke complexes on xray
There is a combination of a calcified peripheral granuloma (black arrow) and a calcified hilar lymph node (white arrow) on the same side. Several other, small calcified granulomas are seen in the right mid-lung field - ranke complex
ranke typically more dense
What would a lung abscess look like on x-ray?
oMay appear solid or cavitary with an air fluid level and a thick wall.
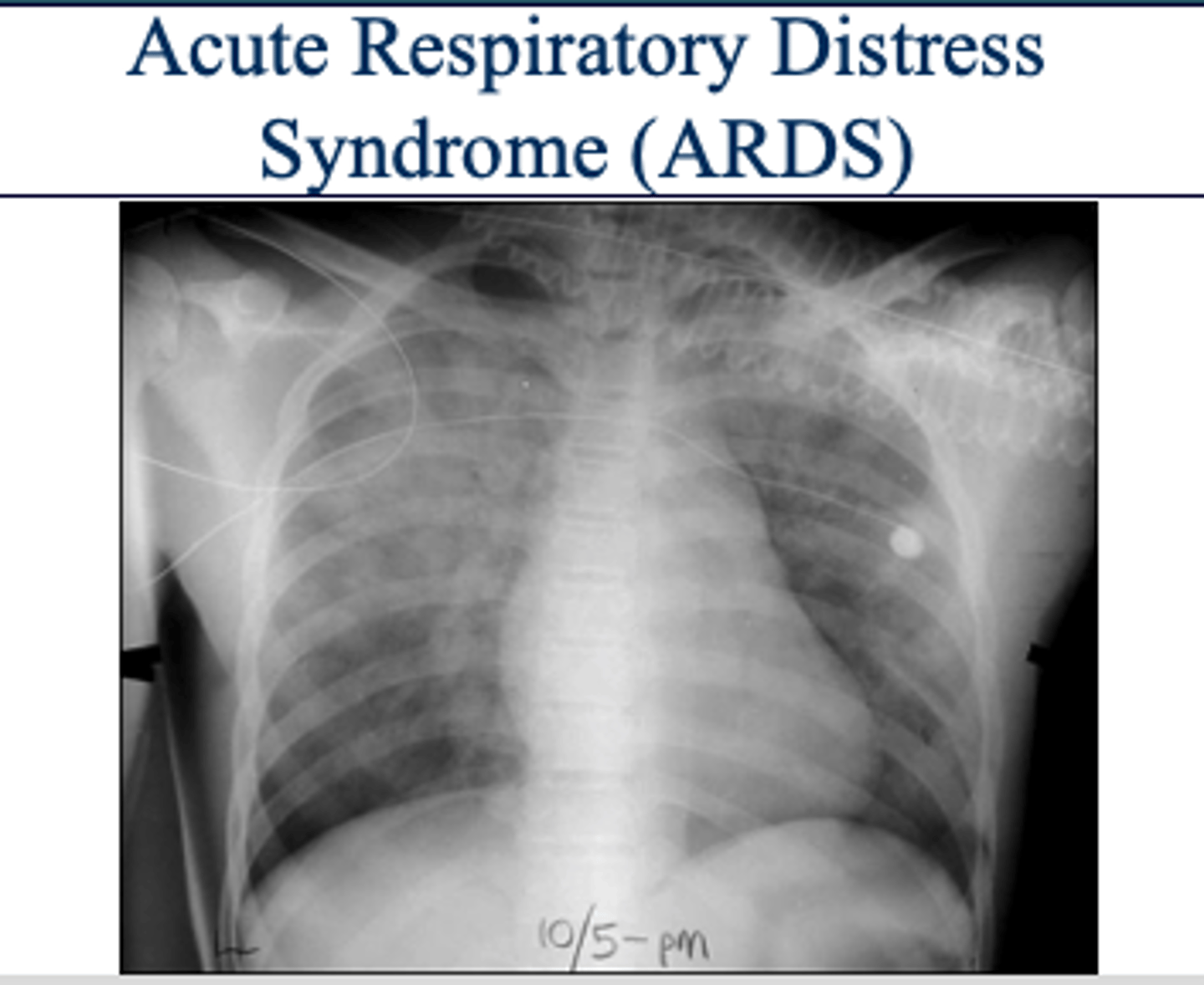
What is ARDS and what is the etiology?
oCapillaries are "leaky" and fluid shifts into the lungs from the blood supply through the capillaries - alveolar infiltrates.
oInitial insult to the alveoli usually caused by either alveolar or vascular damage.
oIncreases the permeability of the capillaries surrounding the alveoli and causes protein-rich fluid to fill the alveolar sacs.
ARDS x-ray appearance
"white out appearance" sometimes with sparing of costophrenic angles
What are pulmonary nodules? How do they appear on x-ray?
Small, round opacities within the lung parenchyma.CXR Findings:Solitary or multiple nodules. Well-defined or irregular borders.
Benign vs malignant pulm nodules
oBenign Nodule
Less than 3 cm
Calcified
Round, well-defined borders
Solid - no cavity
oMalignant Nodule
Greater than 3 cm
Not calcified
Irregular shape, poorly defined borders, ground glass
Cavitated
Growth in past 2 yrs
CT scan indications for lung mass
-New or larger lesion when compared to previous films.
-size greater than 3 cm in patient less than 35 yrs old.
-Any size in patient greater than 35 yrs old.
-Hilar enlargement