5 - Pressure, Flow, and Resistance
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
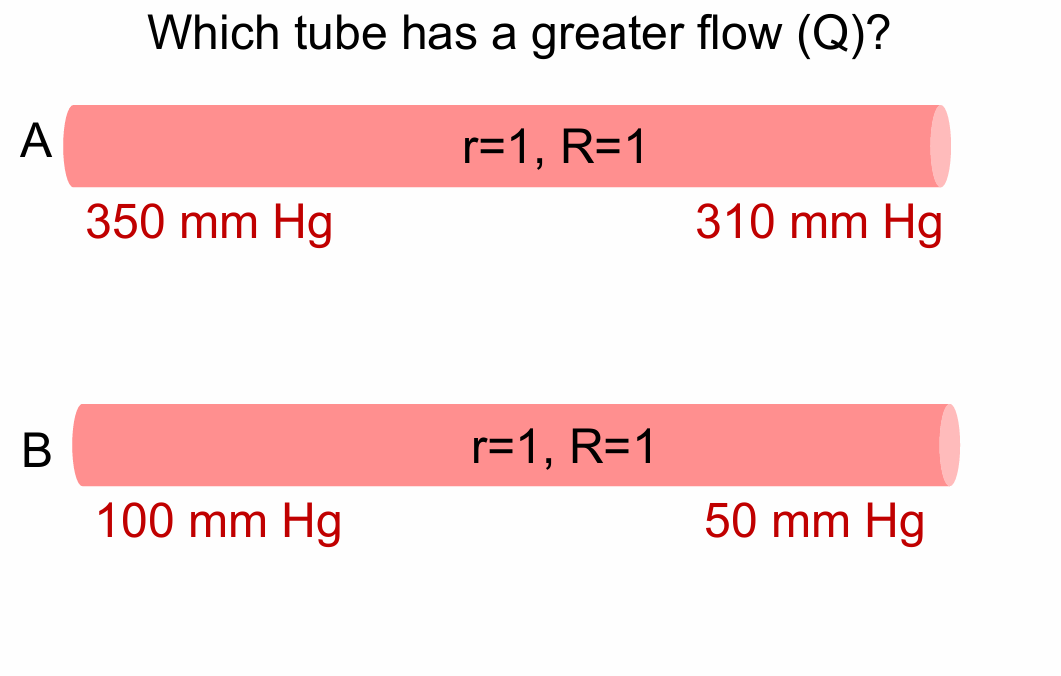
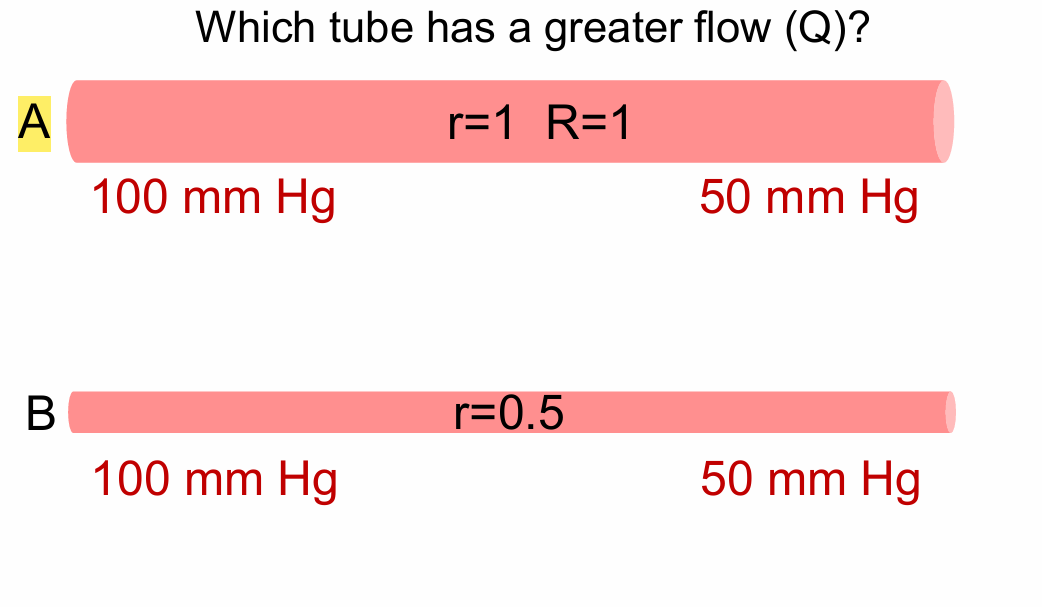
Which tube has a greater flow (Q)?
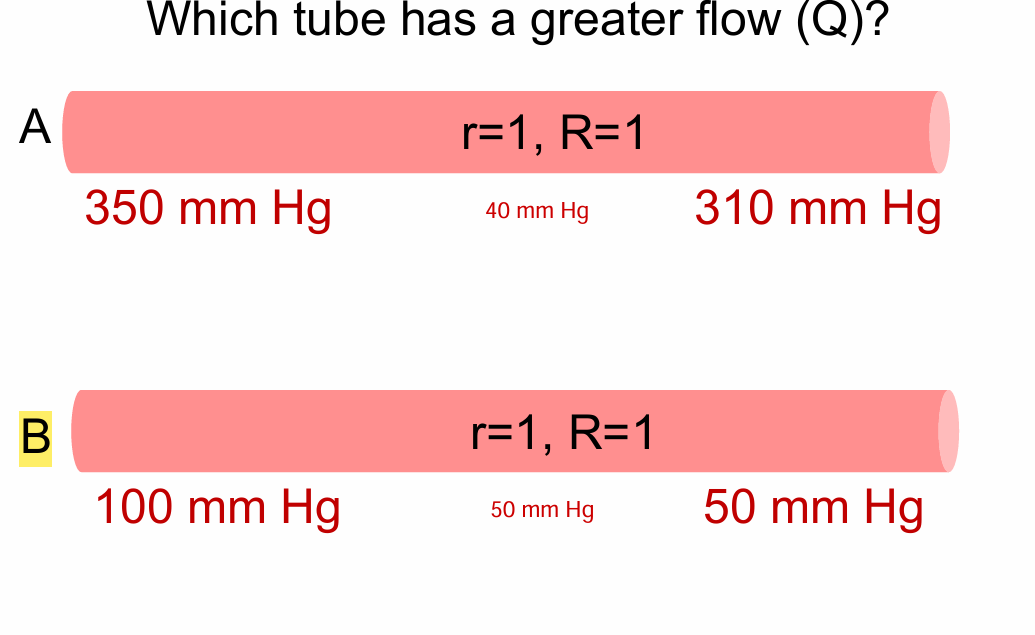
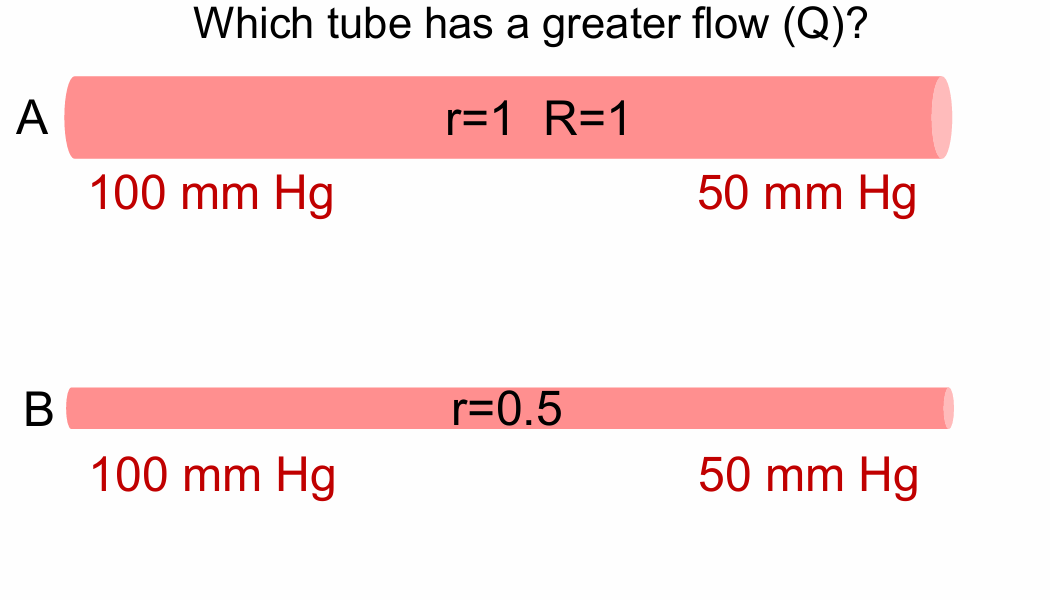
Which tube has a greater flow (Q)?
How does pressure change going from the aorta to the vena cava?
Arteries
Arterioles
Capillaries
Venules
Veins
Arteries - Pressure high in the large, elastic arteries
Arterioles - Pressure falls off dramatically in the arterioles
Capillaries - Continues to fall
Venules - Continues to fall
Veins - Pressure very low in veins
How does resistance (R) change from one group of vessels to the next?
Arteries
Arterioles
Veins
Arteries - Very low resistance
Arterioles- High resistance
Veins - Low resistance
What is compliance?
How easily a blood vessel can distend
Depends on the stiffness of the blood vessel wall
Compliance equation
Compliance = change in volume/ change in transmural pressure
How does compliance change from one group of vessels to the next?
Arteries
Arterioles
Veins
Arteries - high compliance
Arterioles - low compliance
Veins - very high compliance
What is the artery wall like?
Arteries are under much higher pressure, so have thicker walls and more muscle than veins
Structure of a large artery
Inner single layer of endothelial cells Aorta (endothelium)
Many layers of smooth muscle, elastic fibers and connective tissue
Outer layer of connective tissue
Identify what enables large arteries to have a low resistance and high compliance
A. Arterial wall contains a lot of elastic fibers
B. Arteries have a high pressure
C. Arteries have a large diameter or radius
Low resistance - C
High compliance - A and B
What is the function of arteries?
Rapid transit for passage of blood from the heart to organs
Pressure reservoir
Rapid transit for passage of blood from the heart to organs explained
Large diameter with low resistance
Called conductance vessels
Pressure reservoir explained
Driving force for blood during diastole
High compliance
Let’s look at what would happen during systole if the aorta was a rigid tube (not compliant)
Pressure increases from 80 mm Hg (during diastole) to 150 mm Hg (during systole)
Let’s look at what happens during systole when the aorta is a compliant tube (3)
Wall stretches (increases in surface area)
Limits the increase in systolic pressure
Maybe go from diastolic pressure of 80 to systolic pressure of 120
Another important thing that happens during systole: Some energy is stored
stored in the stretched wall
This energy can help maintain blood flow during diastole!
How blood continues to flow during systole? Diastole?
Systole:
70 mL goes in → 25 mL out
Dialated
Diastole:
0 mL goes in → 45 mL goes out
Contracts/ elastic recoil
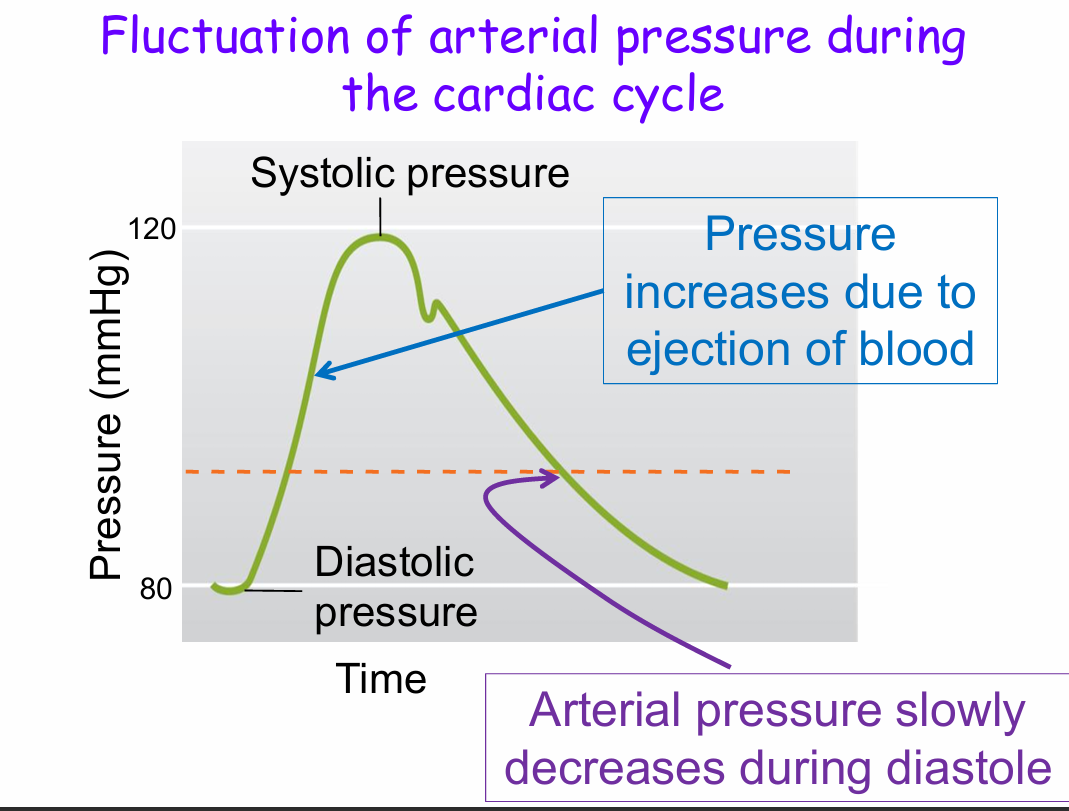
Fluctuation of arterial pressure during the cardiac cycle
Pressure increases due to ejection of blood - Reaches systolic pressure
Arterial pressure slowly decreases during diastole - Reaches diastolic pressure
What will happened to blood pressure if the large arteries become stiffer (ie less compliant or lose some of their elasticity)? Compared to ‘normal’:
A. Systolic pressure will be lower
B. Systolic pressure will be higher
C. Systolic pressure will be the same
A. Diastolic pressure will be lower
B. Diastolic pressure will be higher
C. Diastolic pressure will be the same
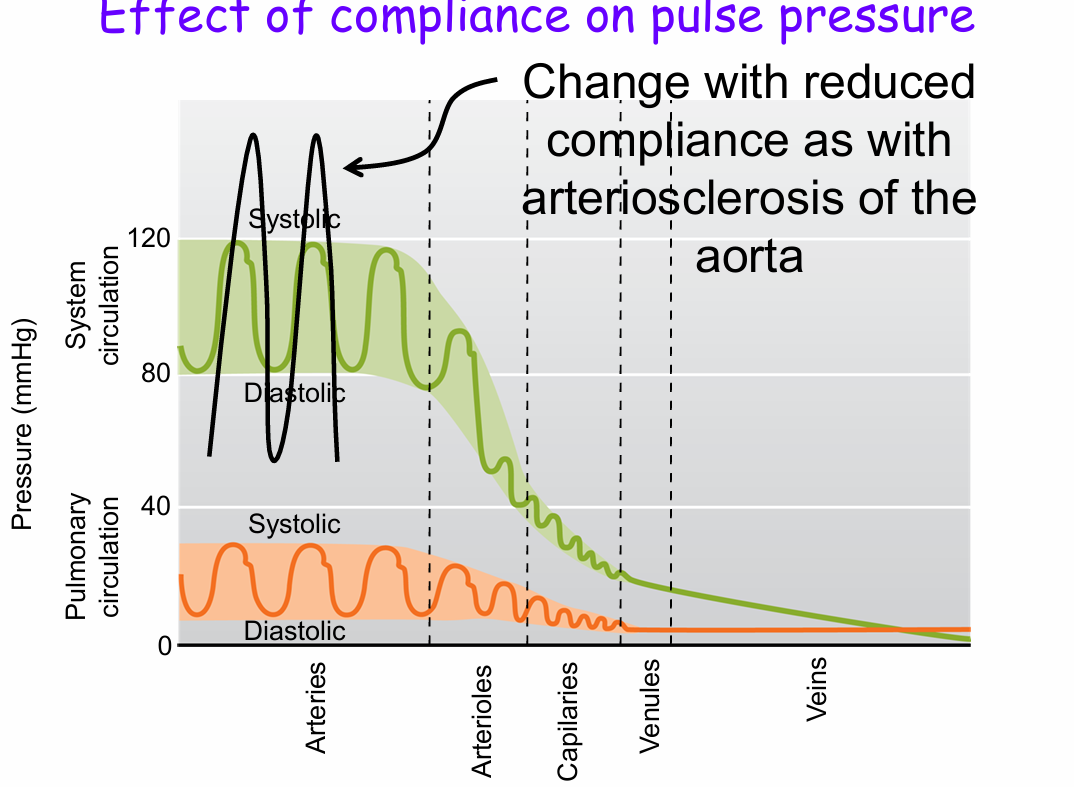
B. Systolic pressure will be higher - Won't stretch so will increase
A. Diastolic pressure will be lower - Wont contract so will decrease
What will happened to pulse pressure if the large arteries become stiffer (ie less compliant or loose some of their elasticity)?
Pulse pressure will increase
Pulse pressure equation
Pulse pressure = systolic - diastolic
Effect of compliance on pulse pressure
Change with reduced compliance as with arteriosclerosis of the aorta
What will most likely happen to mean arterial pressure if the large arteries become stiffer (ie less compliant or lose some of their elasticity)?
A. Mean arterial pressure will decrease
B. Mean arterial pressure will increase
C. Mean arterial pressure will not change
C. Mean arterial pressure will not change
Mean arterial pressure (MAP) definition
average pressure in the arteries during one cardiac cycle
It is not the arithmetic mean of systolic and diastolic pressure
The negative feedback response is for MAP
to stay constant
MAP Equation
MAP = DP + 1/3 (SP – DP)
MAP = 1/3 SP + 2/3 DP
Why is mean arterial pressure (MAP) important?
Tells you whether or not you are perfusing your organs (supplying organs with blood)
Why is pulse pressure important?
It is an important predictor of mortality
Better indicator of arteriosclerosis than MAP
Let’s summarize. What is the function of the aorta and other large elastic arteries?
Conduit for blood
Act as a ‘pressure reservoir’ during diastole
Limit the increase in systolic pressure and limit the decrease in diastolic pressure
What is the wall of an arteriole like?
Inner endothelium
Lumen
One to a couple of layer of smooth muscle cells
What is the function of arterioles? (3)
Transit for passage of blood from the large arteries to capillaries in an organ
Control the amount of blood delivered to those capillaries (or the tissue) at any given MAP
Help regulate arterial blood pressure or MAP
Change in P definition
Pressure reservoir - “arteries”(delta P is the same for all organs)
Variable-resistance definition
outflow tubes (“arterioles”)
How does the body ensure that a particular organ is supplied with sufficient blood to meet its metabolic demands?
A. By changing mean arterial pressure
B. By changing the resistance of the veins
C. By changing the resistance of the
arterioles that supply that organ
D. By changing the resistance of the large,
elastic arteries such as the aorta
E. By changing the resistance of the
capillaries in that organ
C. By changing the resistance of the
arterioles that supply that organ
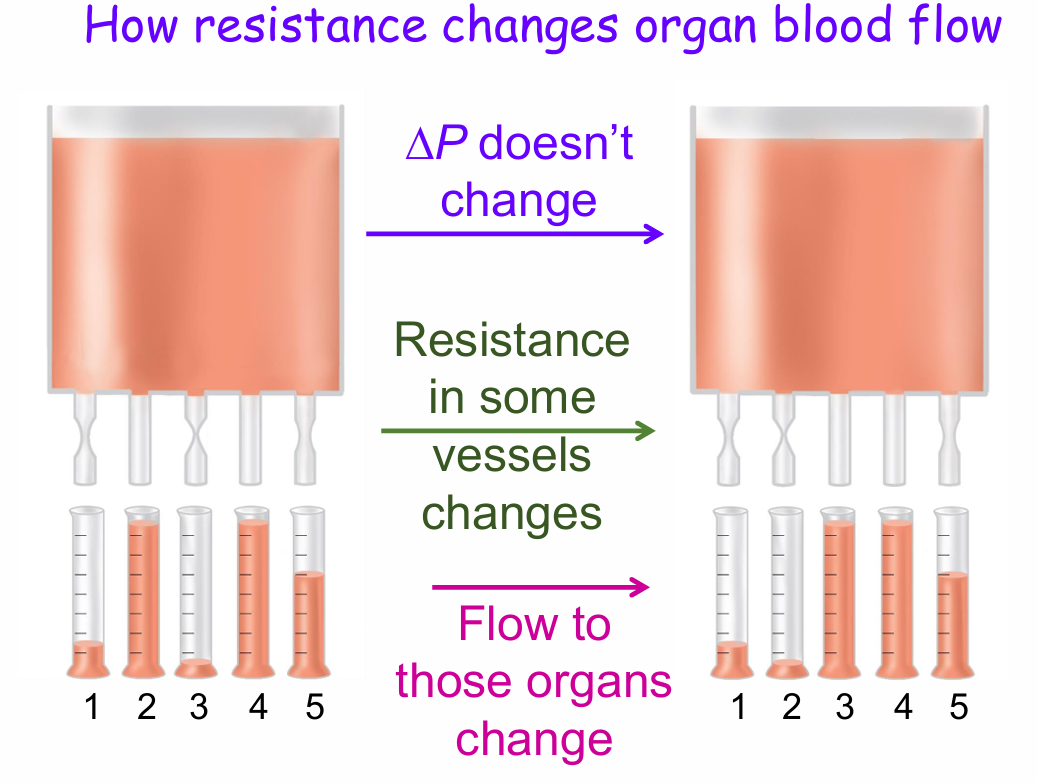
How resistance changes organ blood flow
Delta P doesn’t change
Resistance in some vessels changes
Flow to those organs change
What causes contraction or relaxation of arteriolar smooth muscle to change resistance and hence blood flow?
Arteriolar smooth muscle is tonically contracted (independent of neuronal or hormonal stimulation)
Local control
Extrinsic control (ANS and Hormones)
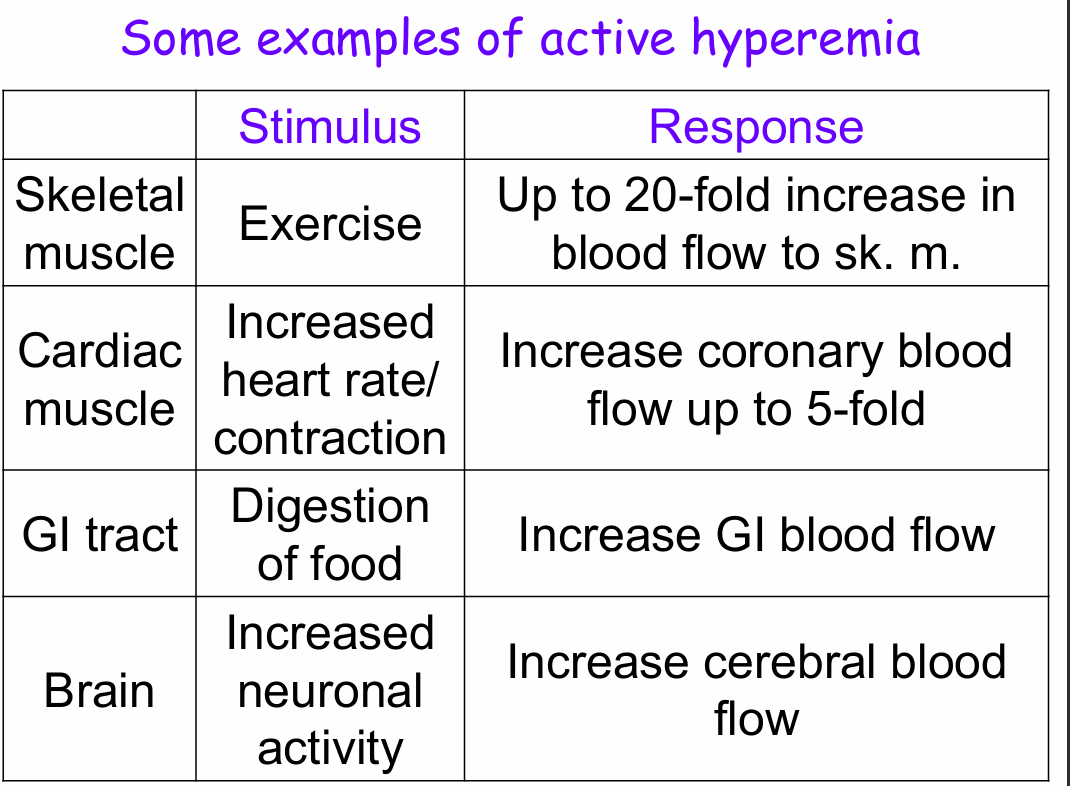
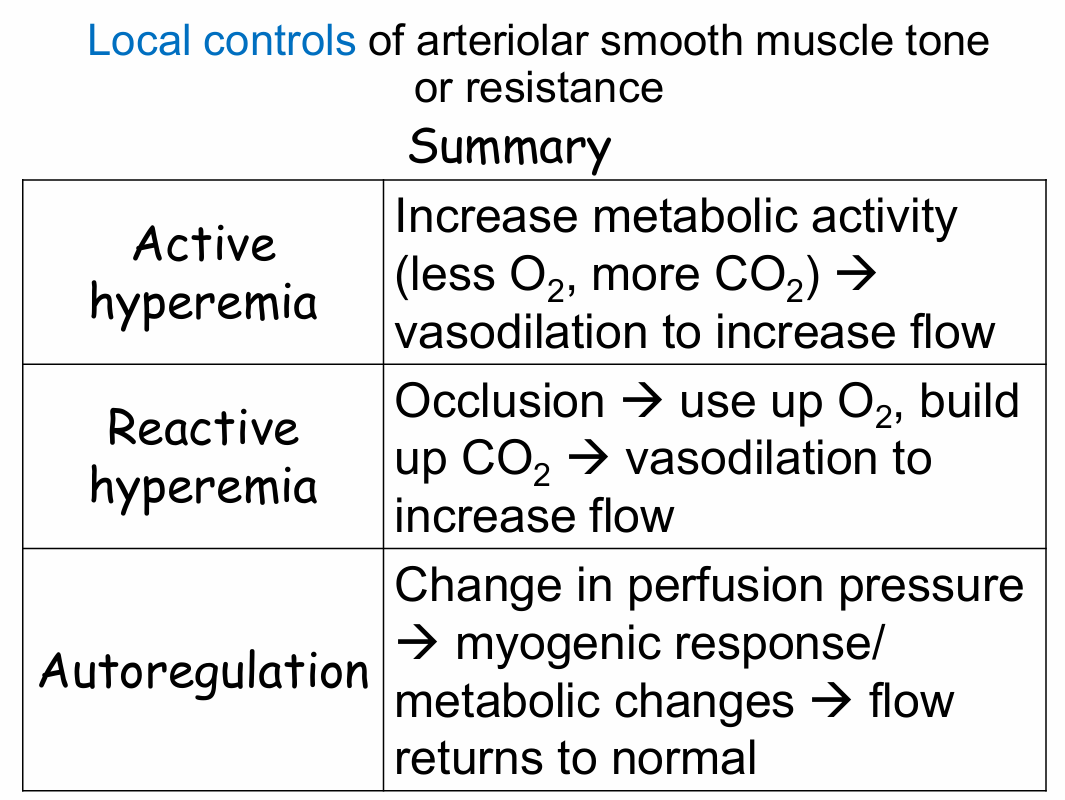
Local controls of arteriolar smooth muscle tone or resistance examples (3)
Active hyperemia
Reactive hyperemia
Autoregulation
Endothelium releases thromboxane A2
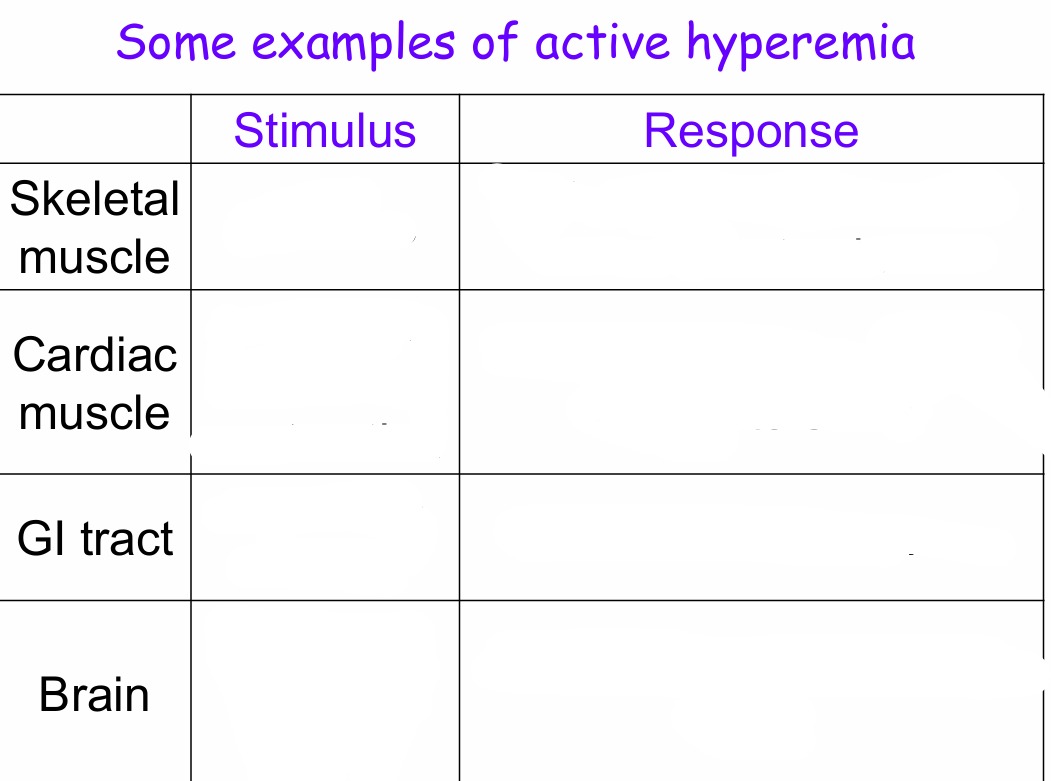
Active hyperemia
Blood flow response to increased tissue metabolic activity
Reactive hyperemia
Blood flow response to blood vessel occlusion
Autoregulation
Blood flow response to changes in perfusion pressure
Active hyperemia, When metabolic activity increases
blood flow to the tissue increases
How blood flow changes with active hyperemia
If a tissue increases its metabolic activity:
Uses more O2, nutrients (Decrease O2)
Generates more CO2, waste products (increase CO2)
Localized relaxation of arteriolar smooth muscle, vasodilation and increased blood flow
Flow autoregulation mechanism (4)
An organ experiences a change in perfusion pressure (Delta P) →
Blood flow to the organ changes →
Autoregulation →
Within few minutes blood flow returns to normal
Flow autoregulation example
Blood pressure decreases →
Blood flow to an organ (e.g. the brain) decreases →
Autoregulation →
Blood flow to the brain goes back to normal
Within a range of MAP, despite changes in perfusion or driving pressure
blood flow to the brain is constant
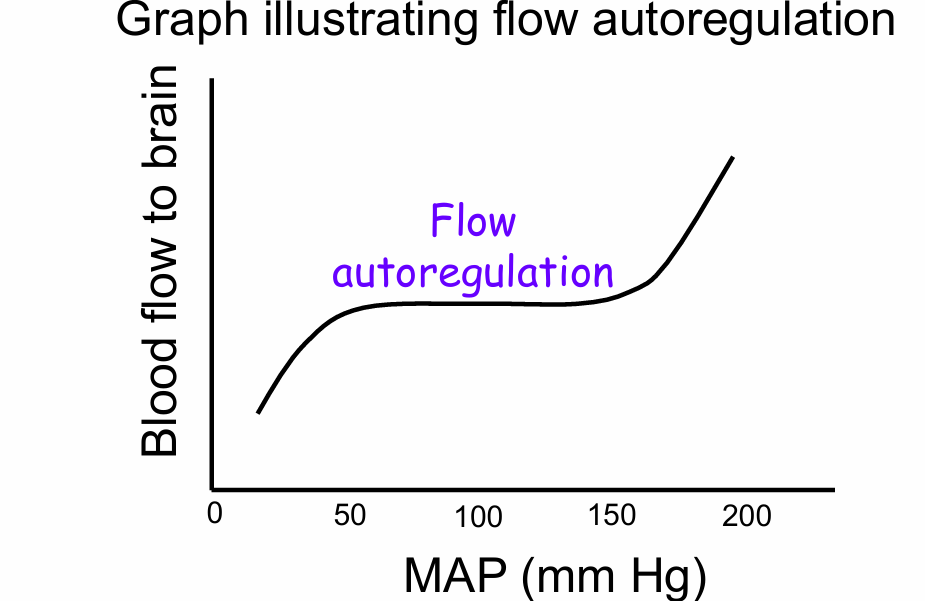
Autoregulation involves two mechanisms
The same metabolic factors as active hyperemia
The myogenic response → Some blood vessels act as stretch receptor
The myogenic response with flow autoregulation
Pressure is too high (too high a blood flow) →
Stretch the arteriole →
Vasoconstrict cerebral arterioles to reduce flow to the brain
And vise versa
A tourniquet is place on the arm. The arm starts turning blue. The tourniquet is removed. What happens to the arm?
C. Slowly goes back to its normal color
D. Turns bright red
E. Turns a darker blue
D. Turns bright red
Reactive hyperemia
Mechanism of reactive hyperemia
Loss of blood flow causes the tissues to:
Use up all of the O2, nutrients (Decreased O2)
Accumulate more CO2, waste products (Increase CO2)
Localized relaxation of arteriolar smooth muscle and vasodilation in the ischemic tissue
Extrinsic control of arteriolar vasodilation and vasoconstriction (2)
Sympathetic nervous system
Other Hormones
Extrinsic control of arteriolar vasodilation and vasoconstriction (SNS) (2)(1)(1)
A. Helps regulate blood pressure (or MAP)
Mostly postganglionic sympathetic neurons and NE
B. Involved with increasing or decreasing blood flow to select tissues
There is a differential distribution of alpha 1 and Beta 2 receptors on vasculature – EPI and NE
Extrinsic control of arteriolar vasodilation and vasoconstriction (Other hormones) (2)
Angiotensin II, Vasopressin, Atrial natriuretic peptide (ANP)
Are more involved with blood pressure (or MAP) regulation
What happens to blood vessels when you are cold? (5)(1)
Cold →
Activates SNS to release NE →
NE activates alpha 1 receptors on skin and gut→
Vasoconstriction to reduce heat loss
Can be shut off by the hypothalamus
Note: Smooth muscle on cutaneous arterioles contain predominantly alpha 1 receptors
When you exercise, there can be a very large increase in blood flow to skeletal muscle. How can that happen? (4)
Hot →
Active hyperemia + EPI from adrenal glands →
EPI activates Beta 2 receptors on skeletal muscle →
Vasodialation to increase heat loss
Let’s summarize. What is the function of the arterioles? (3)
Deliver blood to capillaries
Responsible for the relative blood flow to an organ at any given mean arterial pressure
Help to determine MAP